
Dr. Ahmed Saleem
FICMS
TUCOM / 2015
GENERAL EXAMINATION
Setting:
The room should be private, warm and well lighted
The position of the examiner and the patient
Equipment
Wash/gel your hands
Handshake and introduction
Permission and sensitively, but adequately, expose the areas to be examined
General mental state and level of consciousness
Facial expression and hair
General demeanor
Normal, wasted, overweight, or have some skeletal or sexual characteristics that look
out of proportion.
IV access/Drains/Monitors
Complexion/Skin changes
Pallor
Cyanosis/Polycythemia
Jaundice
Hydration
Pigmentation/Tattoos
Excoriation/pruritus
Face, Eye, Mouth, LN
Hands and radial pulse (Nails, Temperature, Moisture, Color)
Operation Site/Dressing
Legs for edema/DVT
BP/RR/Temperature
Thank and cover the patient
* Baseline examination sequence
After introducing yourself and taking permission, stand on the right and start by inspection; then you
may say “The patient conscious, oriented and look well, no abnormal discoloration or pigmentation
+/- (IV access/Drains/Monitors) attached” then show the following while explaining to the examiner:
The eye for jaundice and pallor
The lips and mouth for cyanosis, pallor and hydration
Hands and radial pulse (Nails, Temperature, Moisture, Color)
Operation Site/Dressing
Legs for edema/DVT
BP/RR/Temperature
Thank and cover the patient
GENERAL EXAMINATION
Setting:
The room should be private, warm and well lighted
The position of the examiner and the patient
Equipment
Wash/gel your hands
Handshake and introduction
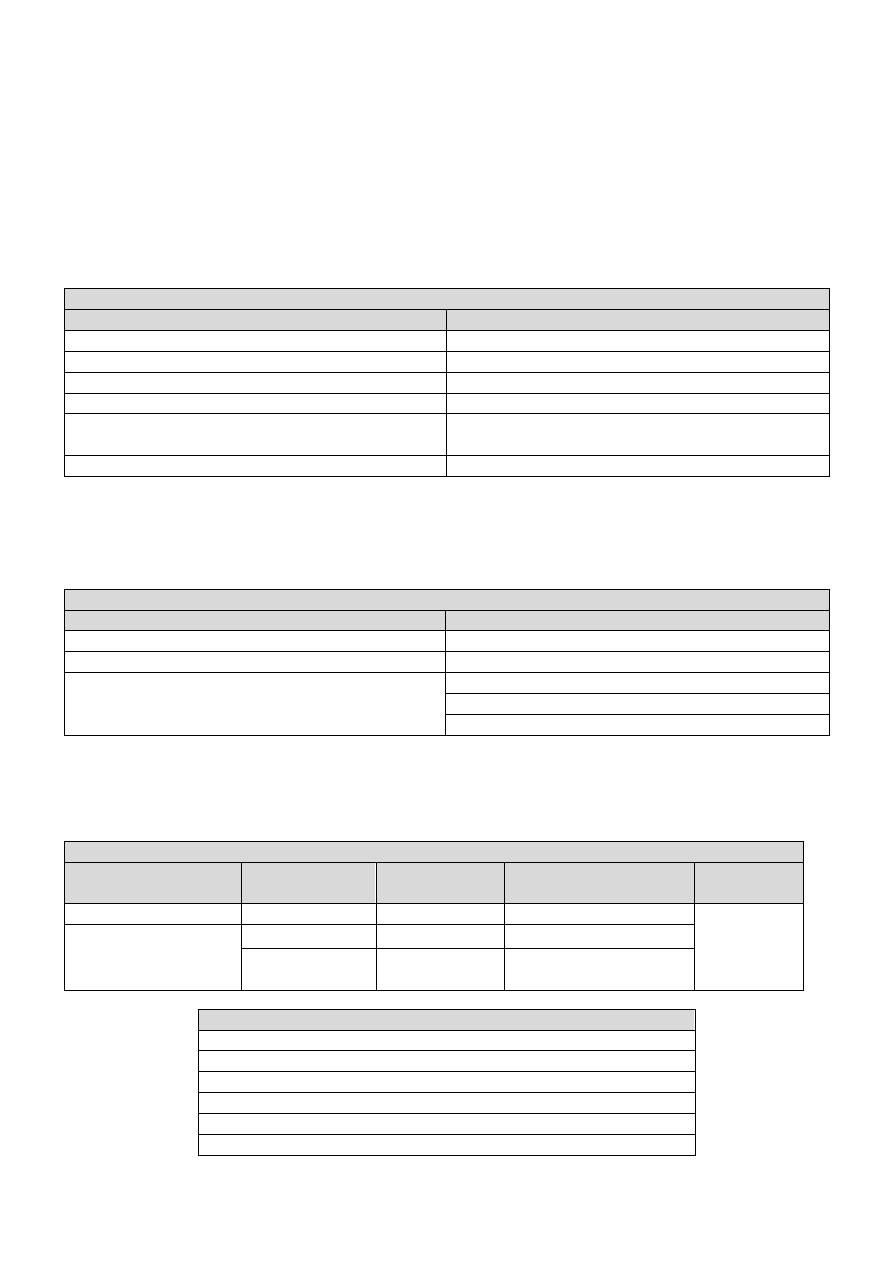
Information from a handshake
Features
Diagnosis
Cold, sweaty hands
Anxiety
Hot, sweaty hands
Hyperthyroidism
Cold, dry hands
Raynaud's phenomenon
Large, fleshy, sweaty hands
Acromegaly
Dry, coarse skin
Hypothyroidism
Manual occupation
Deformed hands/fingers
Dupuytren's contracture, Rheumatoid arthritis
Permission and sensitively, but adequately, expose the areas to be examined
General mental state and level of consciousness
Facial expression and hair
The common causes of hair loss
Local
General
Male balding
Hypothyroidism
Alopecia areata
Cytotoxic drugs
Skin infections
Hypopituitarism
Iron deficiency
Sever illness
General demeanor
Normal, wasted, overweight, or have some skeletal or sexual characteristics that look
out of proportion.
The common causes of wasting
In children
In young adults
In middle age
In old age
All age
groups
Severe gastroenteritis
Tuberculosis
Diabetes
Carcinoma
Starvation
Malabsorption
syndromes
Reticuloses
Thyrotoxicosis
Senility
Anorexia nervosa Carcinoma
Gross cardiorespiratory
disease
The common causes of an increase in weight
Obesity
Pregnancy
Interstitial fluid retention (renal, cardiac or hepatic failure)
Localized fluid retention (massive ovarian cysts, ascites)
Myxedema
Cushing’s syndrome
IV access/Drains/Monitors
Complexion/Skin and Discoloration
Pallor
Look at the color of the conjunctiva on the inner side of the lower eyelid, Look at
the color of the buccal mucous membrane, Stretch the skin of the palm and look at
the color of the palmar creases.
An important determinant of skin color is the relative amount of oxyhemoglobin and
deoxyhemoglobin. Oxyhemoglobin is a bright red pigment. An increase in its flow
beneath thinned facial skin causes the characteristic plethora of Cushing’s syndrome,
whereas a decrease in flow causes pallor.
Pallor can have many causes. It may be:
temporary, due to shock, hemorrhage or intense emotion
persistent, due to anemia or peripheral vasoconstriction.
Vasoconstriction is seen in patients with severe atopy – an inherited susceptibility to
asthma, eczema and hay fever. Pallor is a feature of anemia, but not all pale persons
are anemic; conjunctival and mucosal color is a better indication of anemia than skin
color. A pale skin resulting from diminished pigment occurs with hypopituitarism and
hypogonadism.
Cyanosis/Polycythemia
As blood passes through the capillary bed, oxygen is given up to metabolizing tissues to
produce deoxyhemoglobin. This has a darker, less red, more bluish pigment and its
presence in peripheral blood vessels in increased amounts causes the clinical sign of
cyanosis. There are two physiological types of cyanosis: peripheral and central.
Peripheral cyanosis is associated with increased extraction of oxygen from capillaries
when peripheral blood flow is slowed, often due to vasospasm caused by cold, heart
failure or anxiety. The cyanosed extremity is usually cold and the tongue is
unaffected. Any condition causing slowing of the peripheral circulation may lead to
peripheral cyanosis as there is more time for oxygen extraction. Central cyanosis is
caused by inadequate oxygenation of blood, in turn due to heart failure, serious
respiratory disease or mixing of venous and arterial blood across a right to left cardiac
shunt. In the latter situation, blood passes directly from the right to the left side of the
heart, without passing through the pulmonary circulation, thereby failing to become
oxygenated. Central cyanosis is generalized and the peripheries are often warm. At
least 5 g/dl of reduced hemoglobin is necessary to produce central cyanosis, and it is
therefore less marked in anemic patients. The cyanosis of heart failure is often due to
both peripheral and central causes. The presence of central cyanosis is best
appreciated at the lips, mucous membranes and conjunctivae, where the keratinized
skin is thinnest.
An excess of circulating red blood cells gives the patient a purple-red, florid
appearance. This may be mistaken for cyanosis. It differs from cyanosis in that it
heightens the color of all the skin, especially the cheeks, neck and backs of hands and
feet. The discoloration of cyanosis is usually limited to the tips of the hands, feet and
nose.

Jaundice
Hold the patient upper eyelid with one hand and ask the patient to follow your
finger of other hand downward to reveal the upper sclera, compare both sides.
Jaundice is a yellowish discoloration of the skin, sclerae and mucous membranes due to
hyperbilirubinemia. The yellow colour is first visible against the white background of
the sclera, but as the jaundice increases, the whole skin turns yellow. Bilirubin, a
breakdown product of the porphyrin ring of heme-containing proteins, is found in the
blood in two fractions—conjugated and unconjugated. The unconjugated fraction, also
termed the indirect fraction, is insoluble in water and is bound to albumin in the blood.
The conjugated (direct) bilirubin fraction is water soluble and can therefore be
excreted by the kidney. When measured by the original van den Bergh method, the
normal total serum bilirubin concentration is 17 μmol/L (1 mg/dL). Up to 30%, or 5.1
μmol/L (0.3 mg/dL), of the total is direct-reacting (or conjugated) bilirubin. Levels of
bilirubin >50 μmol/l are needed for clinical detection in good light. Unconjugated
bilirubin is insoluble and transported in plasma bound to albumin; it is therefore not
filtered by the renal glomeruli. In jaundice due to unconjugated hyperbilirubinemia, the
urine is normal in color (acholuric jaundice. In the liver, bilirubin is conjugated to form
bilirubin diglucuronide and excreted, giving bile its characteristic green color. In
conjugated hyperbilirubinemia, the urine is dark brown in color due to the presence of
bilirubin diglucuronide. In the colon, conjugated bilirubin is metabolized by bacterial
flora to stercobilinogen and stercobilin which are excreted in the stool, contributing to
the brown color of stool. Stercobilinogen is absorbed from the bowel and excreted in
the urine as urobilinogen, a colorless, water-soluble compound.
Prehepatic jaundice In hemolytic disorders the accompanying anemic pallor combined
with jaundice may produce a pale lemon complexion. The stools and urine are normal
in color. Gilbert's syndrome is common and causes unconjugated hyperbilirubinemia.
Serum liver enzyme concentrations are normal and jaundice is mild (plasma bilirubin
<100 μmol/l) but increases during prolonged fasting or intercurrent febrile illness.
Hepatic jaundice Hepatocellular disease causes hyperbilirubinemia that is both
unconjugated and conjugated. Urine will be dark and stools normal in color.
Post-hepatic jaundice In biliary obstruction, conjugated bilirubin in the bile does not
reach the intestine, so the stools are pale. Conjugated bilirubin is soluble and filtered
by the kidney, so the urine is dark brown. Obstructive jaundice may be accompanied by
generalized itch (pruritus) due to skin deposition of bile salts. Obstructive jaundice with
abdominal pain is usually due to gallstones; if fever or rigors also occur (Charcot's
triad), ascending cholangitis is likely. Painless obstructive jaundice suggests malignant
biliary obstruction, e.g. cholangiocarcinoma or cancer of the head of the pancreas.
Obstructive jaundice can be hepatic as well as post-hepatic intrahepatic cholestasis,
e.g. primary biliary cirrhosis.
Hydration
Assess the state of hydration by looking for sunken orbits and dry mucous membranes.
If severe dehydration seems likely, test skin turgor. Gently pinch a fold of skin on the
neck or anterior chest wall, hold it for a few seconds and then release. Well-hydrated
skin springs back into position immediately, whereas dehydrated skin subsides
abnormally slowly.
Pigmentation/Tattoos
Excoriation/pruritus

Face, Eye, Mouth, LN
Hands and radial pulse (Nails, Temperature, Moisture, Color)
The majority of patients with finger clubbing have thoracic disease but it is also associated
with gastrointestinal disorders and can be familial. Rarely, clubbing develops relatively quickly
over several weeks, in empyema. Clubbing requires:
loss of the normal angle between the nail and nail bed
increased nail bed fluctuation
increased nail curvature in later stages
increased bulk of the soft tissues over the terminal phalanges.
Operation Site/Dressing
Legs for edema/DVT
Inspect the legs for obvious edema and examine for pitting edema. Press firmly but gently
for around 20 – 30 seconds behind the medial malleolus, over the dorsum of the foot and on
the shin. If edema is present, a depression/concavity will form.
The cardinal sign of subcutaneous edema is pitting of superficial tissues. Pitting on pressure
may not be demonstrable until body weight has increased by 10-15% and may be only
demonstrable on sacrum in bedridden patients. Day-to-day alterations in body weight are
usually the most reliable index of changes in body water. Hypothyroidism is characterized by
mucinous infiltration of tissues (myxedema). In contrast to edema, myxedema and chronic
lymphedema do not pit on pressure.
BP/RR/Temperature
Body temperature may be recorded in the mouth, axilla, ear or rectum. A ‘normal’ mouth
temperature is 35.8-37.2 °C. Those in the ear and rectum are 0.5°C higher and in the axilla
0.5°C lower. There is a diurnal variation in temperature; the lowest values are recorded in the
early morning with a maximum between 6 and 10 pm. In women, ovulation is associated with
a 0.5°C rise in temperature.
Thank and cover the patient

EXAMINATION OF THE ABDOMEN
Setting: …
Inspection:
General …
End of bed: Asymmetry/Distension
Umbilicus
Visible peristalsis
Lump: Physical signs
Patient reaction and lump changes with Respiration/Coughing
Striae, Scars, sinuses or fistulae, pigmentation
Dilated surface veins
Palpation:
Technique …
Ask about pain and its site
Light palpation for tenderness.
Deep palpation for tenderness.
Mild tenderness, Sever tenderness (Guarding), Rebound tenderness, Rigidity
If mass found; assess its physical characteristics
Palpation of the normal solid viscera
Liver
Gallbladder
Spleen
Right Kidney
Left Kidney
Urinary Bladder
Percussion:
General percussion
Defining the boundaries of abdominal organs and masses
Liver, spleen, urinary bladder, other masses
Detection of ascites
Auscultation:
Bowel sounds and vascular bruits
Never forget to examine:
Supraclavicular lymph glands
Hernia orifices and femoral pulses
Genitalia
Anal canal and rectum
Thank and cover the patient

EXAMINATION OF THE ABDOMEN
Setting: …
Stand on right side and the patient lie supine on a hard couch and head raised by 15–20° and
the arms by his side. The full extent of the abdomen must be visible and, ideally, patients
should be uncovered from nipples to knees. Many find this embarrassing and a compromise is
to cover the lower abdomen with a sheet or blanket while palpating the abdomen, but never
forget to examine the genitalia and the hernial orifices.
Inspection:
General …
End of bed: Asymmetry/Distension
Is the abdomen of normal contour and fullness, or distended? Is it scaphoid (sunken)?
Generalized fullness or distension may be due to fat, fluid, flatus, feces or fetus. Localized
distension may be symmetrical and centered around the umbilicus as in the case of small
bowel obstruction, or asymmetrical as in gross enlargement of the spleen, liver or ovary.
Make a mental note of the site of any such swelling or distension; think of the anatomical
structures in that region and note if there is any movement of the swelling, either with or
independent of respiration. Remember that chronic urinary retention may cause palpable
enlargement in the lower abdomen.
Umbilicus
Normally the umbilicus is slightly retracted and inverted. If it is everted, then an umbilical
hernia may be present and this can be confirmed by feeling an expansile impulse on
palpation of the swelling when the patient coughs. The hernial sac may contain omentum,
bowel or fluid. A common finding in the umbilicus of elderly obese people is a
concentration of inspissated desquamated epithelium and other debris (omphalolith).
Visible peristalsis
Seen in 3: Pyloric obstruction, Distal small bowel obstruction, Paralytic ileus.
Lump: Physical signs
Patient reaction and lump changes with Respiration/Coughing
Striae, Scars, sinuses or fistulae, pigmentation
In marked abdominal distension, the skin is smooth and shiny. Striae atrophica or
gravidarum are white or pink wrinkled linear marks on the abdominal skin. They are
produced by gross stretching of the skin with rupture of the elastic fibers and indicate a
recent change in size of the abdomen, such as is found in pregnancy, ascites, wasting
diseases and severe dieting. Wide purple striae are characteristic of Cushing’s syndrome
and excessive steroid treatment. Note any scars present, their site, whether they are old
(white) or recent (red or pink), linear or stretched (and therefore likely to be weak and
contain an incisional hernia). Pigmentation of the abdominal wall may be seen in the
midline below the umbilicus, where it forms the linea nigra and is a sign of pregnancy.
Erythema ab igne is a brown mottled pigmentation produced by constant application of
heat, usually a hot water bottle or heat pad, on the skin of the abdominal wall. It is a sign
that the patient is experiencing severe ongoing pain such as from chronic pancreatitis.

Dilated surface veins
Look for prominent superficial veins, which may be apparent in three situations: thin veins
over the costal margin, usually of no significance; occlusion of the inferior vena cava; and
venous anastomoses in portal hypertension. Inferior vena caval obstruction not only
causes edema of the limbs, buttocks and groins but, in time, distended veins on the
abdominal wall and chest wall appear. These represent dilated anastomotic channels
between the superficial epigastric and circumflex iliac veins below, and the lateral thoracic
veins above, conveying the diverted blood from the long saphenous vein to the axillary
vein; the direction of flow is therefore upwards. If the veins are prominent enough, try to
detect the direction in which the blood is flowing by occluding a vein, emptying it by
massage and then looking for the direction of refill. Distended veins around the umbilicus
(caput medusae) are uncommon but signify portal hypertension, other signs of which may
include splenomegaly and ascites. These distended veins represent the opening up of
anastomoses between portal and systemic veins and occur in other sites, such as
esophageal and rectal varices.
Palpation:
Technique
Palpation forms the most important part of the abdominal examination. Tell the patient to
relax as best he can and to breathe quietly, and assure him that you will be as gentle as
possible. Enquire about the site of any pain and come to this region last. These points,
together with unhurried palpation with a warm hand, will give the patient confidence and
allow the maximum amount of information to be obtained. When palpating, the wrist and
forearm should be in the same horizontal plane where possible, even if this means
bending down or kneeling by the patient’s side. The best palpation technique involves
moulding the relaxed right hand to the abdominal wall, not to hold it rigid. The best
movement is gentle but with firm pressure, with the fingers held almost straight but with
slight flexion at the metacarpophalangeal joints and certainly avoiding sudden poking with
the fingertips
Ask about pain and its site
Light palpation for tenderness.
Gently resting a hand on the abdomen and pressing lightly and systematically moved over
the whole of the abdomen, starting in left iliac fossa and move round in an anti-clockwise
direction to finish in the right iliac fossa.
Deep palpation for tenderness.
When no pain is elicited by systematic light palpation over the whole abdomen, repeat the
process, pressing more firmly and deeply to see if there is any deep tenderness.
Mild tenderness, Sever tenderness (Guarding), Rebound tenderness, Rigidity
If mass found; assess its physical characteristics
Palpation of the normal solid viscera
The liver
Start in the right iliac fossa. Place your hand flat on the abdomen with your fingers
pointing upwards and sensing fingers (index and middle) lateral to the rectus muscle,
so that your fingertips lie parallel to rectus sheath. Keep your hand stationary. Ask the
patient to breathe in deeply through the mouth. Feel for the liver edge as it descends
on inspiration. Move your hand progressively up the abdomen, 1 cm at a time,
between each breath the patient takes, until you reach the costal margin or detect the
liver edge. Another commonly employed though less accurate method of feeling for an
enlarged liver is to place the right hand below and parallel to the right subcostal
margin. The liver edge will then be felt against the radial border of the index finger. The
liver is often palpable in normal patients without being enlarged. The lower edge of the
liver can be clarified by percussion, as can the upper border in order to determine
overall size: a palpable liver edge can be due to enlargement or displacement
downwards by lung pathology. Hepatomegaly conventionally is measured in
centimeters palpable below the right costal margin, which should be determined with a
ruler if possible. Try to make out the character of its surface (i.e. whether it is soft,
smooth and tender as in heart failure, very firm and regular as in obstructive jaundice
and cirrhosis, or hard, irregular, painless and sometimes nodular as in advanced
secondary carcinoma). In tricuspid regurgitation, the liver may be felt to pulsate.
Occasionally a congenital variant of the right lobe projects down lateral to the
gallbladder as a tongue-shaped process, called Riedel’s lobe. Though uncommon, it is
important to be aware of this because it may be mistaken either for the gallbladder
itself or for the right kidney.
The upper and lower borders of the right lobe of the liver can be mapped out
accurately by percussion. Start anteriorly, at the fourth intercostal space, where the
note will be resonant over the lungs, and work vertically downwards. Over a normal
liver, percussion will detect the upper border, which is found at about the fifth
intercostal space (just below the right nipple in men). The dullness extends down to the
lower border at or just below the right subcostal margin, giving a normal liver vertical
height of 12-15 cm. The normal dullness over the upper part of the liver is reduced in
severe emphysema, in the presence of a large right pneumothorax and after
laparotomy or laparoscopy.
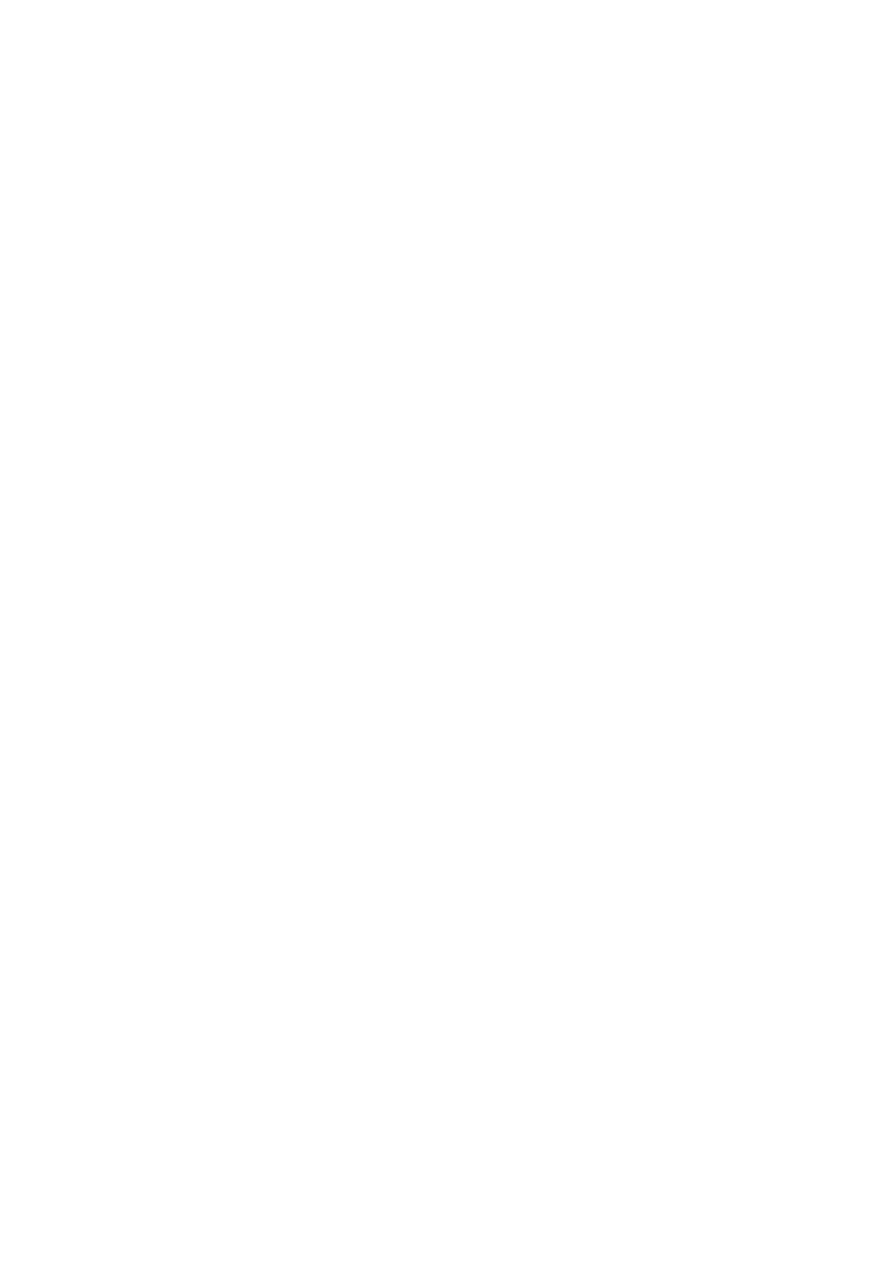
Causes of hepatomegaly
Chronic parenchymal
liver disease
Infectious
Malignancy
Haematological
disorders
Rarities
Alcoholic liver disease
Viral hepatitis
Primary hepatocellular
cancer
Lymphoma
Amyloidosis
Hepatic steatosis
Hydatid disease
Secondary metastatic
cancer
Leukaemia
Budd-Chiari
syndrome
Autoimmune hepatitis
Myelofibrosis
Sarcoidosis
Primary biliary cirrhosis
Polycythaemia
Right heart failure

Gallbladder
The gallbladder is palpated in the same way as the liver. The normal gallbladder cannot
be felt. When it is distended, however, it forms an important sign and may be palpated
as a firm, smooth, or globular swelling with distinct borders, just lateral to the edge of
the rectus abdominis near the tip of the ninth costal cartilage. It moves with
respiration. Its upper border merges with the lower border of the right lobe of the
liver, or disappears beneath the costal margin and therefore can never be felt. When
the liver is enlarged or the gallbladder grossly distended, the latter may be felt not in
the hypochondrium, but in the right lumbar or even as low down as the right iliac
region. The ease of definition of the rounded borders of the gallbladder, its
comparative mobility on respiration, the fact that it is not normally bimanually
palpable and that it seems to lie just beneath the abdominal wall helps to identify
such a swelling as gallbladder rather than a palpable right kidney. A painless
gallbladder can usually be palpated in the following clinical situations:
1-In a jaundiced patient with carcinoma of the head of the pancreas or other malignant
causes of obstruction of the common bile duct (below the entry of the cystic duct), the
ducts above the obstruction become dilated, as does the gallbladder (see Courvoisier’s
law, below).
2-In mucocele of the gallbladder, a gallstone becomes impacted in the neck of a
collapsed, empty, uninfected gallbladder and mucus continues to be secreted into its
lumen. Eventually, the uninfected gallbladder is so distended that it becomes palpable.
In this case, the bile ducts are normal and the patient is not jaundiced.
3-In carcinoma of the gallbladder, the gallbladder may be felt as a stony, hard, irregular
swelling, unlike the firm, regular swelling of the two above-mentioned conditions.
* Murphy’s sign
In acute inflammation of the gallbladder (acute cholecystitis), severe pain is present.
Often an exquisitely tender but indefinite mass can be palpated; this represents the
underlying acutely inflamed gallbladder walled off by greater omentum. Ask the
patient to breathe in deeply, and palpate for the gallbladder in the normal way; at the
height of inspiration, the breathing stops with a gasp as the mass is felt. This represents
Murphy’s sign. The sign is not found in chronic cholecystitis or uncomplicated cases of
gallstones.
* Courvoisier’s law
This states that in the presence of jaundice, a palpable gallbladder makes gallstone
obstruction of the common bile duct an unlikely cause (because it is likely that the
patient will have had gallbladder stones for some time and these will have rendered
the wall of the gallbladder relatively fibrotic and therefore non-distensible). However,
the converse is not true, because the gallbladder is not palpable in many patients who
do turn out to have malignant bile duct obstruction.
Spleen
An enlarged spleen appears below the tip of the tenth rib along a line heading
towards the umbilicus and, if really large, may extend into the right iliac fossa. A
normal spleen is not palpable.
To feel the spleen, place the fingertips of your right hand on the right iliac fossa just
below the umbilicus. Ask the patient to take a deep breath. If nothing abnormal is
felt, move your hand in stages towards the tip of the left tenth rib. When the costal
margin is reached, place your left hand around the lower left rib cage and lift the
lower ribs and the spleen forwards as the patient inspires. This manoeuvre
occasionally lifts a slightly enlarged spleen far enough forward to make it palpable.
Where considerable splenomegaly is present, its typical characteristics include a
firm swelling appearing beneath the left subcostal margin in the left upper
quadrant of the abdomen, which is dull to percussion, moves downwards on
inspiration, is not bimanually palpable, whose upper border cannot be felt (i.e. one
cannot ‘get above it’) and in which a notch can often, though not invariably, be
felt in the lower medial border. The last three features distinguish the enlarged
spleen from an enlarged kidney; in addition, there is usually a band of colonic
resonance anterior to an enlarged kidney.
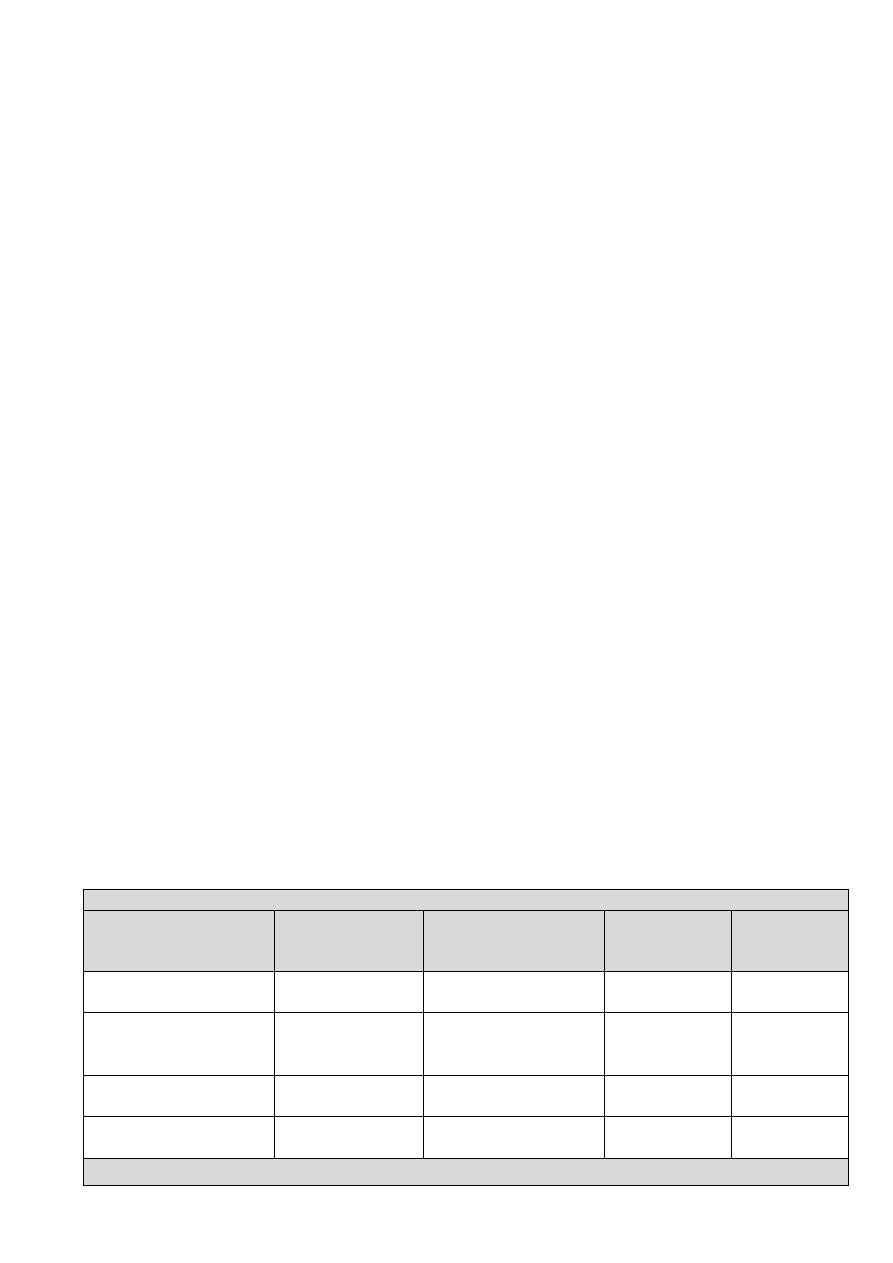
Causes of splenomegaly
Infections
Rheumatological conditions
Hematological disorders
Rarities
Glandular fever
Rheumatoid arthritis (Felty's
syndrome)
Lymphoma and lymphatic
leukemias
Sarcoidosis
Malaria, kala azar
(leishmaniasis)
Systemic lupus erythematosus Myeloproliferative diseases,
polycythemia rubra vera and
myelofibrosis
Amyloidosis
Brucellosis, tuberculosis,
salmonellosis
Hemolytic anemia, congenital
spherocytosis
Glycogen storage
disorders
Bacterial endocarditis
Portal hypertension
Causes of hepatosplenomegaly
Lymphoma
Myeloproliferative diseases
Cirrhosis with portal hypertension
Amyloidosis, sarcoidosis, glycogen storage disease
Right Kidney
Place the right hand horizontally in the right lumbar region anteriorly with the left hand
placed posteriorly in the right loin. Push forwards with the left hand, press the right
hand inward and upward and ask the patient to take a deep breath in. The lower pole
of the right kidney, unlike the left, is commonly palpable in thin patients and is felt as a
smooth, rounded swelling which descends on inspiration and is bimanually palpable
and may be ‘ballotted’.

Left Kidney
The right hand is placed anteriorly in the left lumbar region while the left hand is
placed posteriorly in the left loin. Ask the patient to take a deep breath in, press the
left hand forward and the right hand backward, upward and inward. The left kidney is
not usually palpable unless either low in position or enlarged. Its lower pole, when
palpable, is felt as a rounded firm swelling between both right and left hands (i.e.
bimanually palpable) and it can be pushed from one hand to the other, in an action
which is called ‘ballotting’.
Urinary Bladder
Normally the urinary bladder is not palpable. When it is full and the patient cannot
empty it (retention of urine), a smooth firm regular oval-shaped swelling will be
palpated in the suprapubic region and its dome (upper border) may reach as far as the
umbilicus. The lateral and upper borders can be readily made out, but it is not possible
to feel its lower border (i.e. the swelling is ‘arising out of the pelvis’). The fact that this
swelling is symmetrically placed in the suprapubic region beneath the umbilicus, that
it is dull to percussion and that pressure on it gives the patient a desire to micturate,
together with the signs above, confirm such a swelling as the bladder. In women,
however, a mass that is thought to be a palpable bladder has to be differentiated from
a gravid uterus (firmer, mobile side to side and vaginal signs different), a fibroid uterus
(may be bosselated, firmer and vaginal signs different) and an ovarian cyst (usually
eccentrically placed to left or right side).
Percussion:
The technique of percussion was probably developed as a way of ascertaining how much
fluid remained in barrels of wine or other liquids. Effective percussion is a knack that
requires consistent practice; do so upon yourself or on willing colleagues, as percussion
can be uncomfortable for patients if performed repeatedly and inexpertly. The middle
finger of the left hand is placed on the part to be percussed and pressed firmly against it,
with slight hyperextension of the distal interphalangeal joint. The back of this joint is then
struck with the tip of the middle finger of the right hand (vice versa if you are left-handed).
The movement should be at the wrist rather than at the elbow. The percussing finger is
bent so that its terminal phalanx is at right angles and it strikes the other finger
perpendicularly. As soon as the blow has been given, the striking finger is raised: the action
is a tapping movement. The two most common mistakes made by the beginner are, first,
failing to ensure that the finger of the left hand is applied flatly and firmly and, second,
striking the percussion blow from the elbow rather than from the wrist.
General percussion over the abdomen: A dull area may draw your attention to a mass
that was missed on palpation and indicate a more detailed and careful palpation of the
area of dullness.
Defining the boundaries of abdominal organs and masses
Liver, spleen, urinary bladder, other masses
Detection of ascites: The use of ultrasound to detect ascites has shown that quite a lot
needs to be present to be detected clinically, probably more than 2 liters. It is unwise
and unreliable to diagnose ascites unless there is sufficient free fluid present to give
generalized enlargement of the abdomen.

The cardinal sign created by ascites is shifting dullness. A fluid thrill may also be present
but it would be unwise to diagnose ascites based on this sign without the presence of
shifting dullness.
Shifting dullness: With the patient supine, percuss from the midline out to the flanks.
Note any change from resonant to dull, along with the areas of dullness and resonance.
Keep your finger on the site of dullness in the flank and ask the patient to turn on to his
opposite side. Pause for at least 10 seconds to allow any ascites to gravitate, then
percuss again. If the area of dullness is now resonant, shifting dullness is present,
indicating ascites.
Fluid thrill: If the abdomen is tensely distended and you are not certain whether ascites
is present, look for the presence of a fluid thrill. Place the palm of your left hand flat
against the left side of the abdomen and flick a finger of your right hand against the
right side of the abdomen. If you feel a ripple against your left hand, ask an assistant to
place the edge of their hand on the midline of the abdomen. This prevents
transmission of the impulse via the skin rather than through the ascites. If you still feel
a ripple against your left hand, a fluid thrill is present (only detected in gross ascites).
Auscultation:
Bowel sounds and vascular bruits
With the patient lying on his back, place the stethoscope diaphragm to the right of the
umbilicus and do not move it. Bowel sounds are gurgling noises from the normal peristaltic
activity of the gut. They normally occur every 5-10 seconds, but the frequency varies.
Listen for up to 2 minutes before concluding that bowel sounds are absent. Absence of
bowel sounds implies paralytic ileus or peritonitis. In intestinal obstruction, bowel sounds
occur with increased frequency, volume and pitch, and have a high-pitched, tinkling
quality.
Listen above the umbilicus over the aorta for arterial bruits, which suggest an
atheromatous or aneurysmal aorta or superior mesenteric artery stenosis.
Now place the stethoscope 2-3 cm above and lateral to the umbilicus and listen for renal
artery bruits from renal artery stenosis.
Listen over the liver for bruits due to hepatoma or acute alcoholic hepatitis. A friction rub,
which sounds like rubbing your dry fingers together, may be heard over the liver
(perihepatitis) or spleen (perisplenitis).
A succussion splash sounds like a half-filled water bottle being shaken. Explain the
procedure to the patient then shake the abdomen by lifting him with both hands under the
pelvis. An audible splash more than 4 hours after the patient has eaten or drunk anything
indicates delayed gastric emptying, e.g. pyloric stenosis.
Never forget to examine:
Supraclavicular lymph glands
Hernia orifices and femoral pulses
Genitalia
Anal canal and rectum
Thank and cover the patient
ANO-RECTAL EXAMINATION
Setting …
Uncover the patient
from the waist to the middle of the thighs.
The patient should lie in the left lateral position
with the neck and shoulders rounded so that the
chin rests on the chest, hips flexed to 90° or more,
but knees
flexed to slightly less than 90°. Ask the patient to move towards you so that his buttocks are up to the edge of
the bed. This makes inspection easier and tips the abdominal contents forwards, which helps the bimanual
examination.
Inspection:
Lift up the uppermost buttock with your left hand so that you can see the anus, peri-anal skin
and perineum clearly. Look for:
skin rashes and excoriation,
fecal soiling, blood or mucus,
scarring, or the opening of a fistula,
lumps and bumps (e.g. polyps, a peri-anal hematoma, prolapsed piles, or even a
carcinoma),
ulcers, especially fissures.
Palpation:
Before carrying out a digital examination, particularly if there is a history of pain on defecation,
place your fingers on either side of the anus and gently stretch the anal orifice. This is to see if
there is any spasm associated with a fissure, which may be visible. If there is spasm or a
fissure, in no circumstances carry out any instrumentation as this could cause severe pain.
Place the pulp of your gloved right index finger on the center of the anus, with the finger
parallel to the skin of the perineum and in the mid-line. Then press gently into the anal canal,
but at the same time press backwards against the skin of the posterior wall of the anal canal
and the underlying sling of the puborectalis muscle. This overcomes most of the tone in the
anal sphincter and allows the finger to straighten and slip into the rectum. Never thrust the tip
of your finger straight in.
The anal canal
As the finger goes through the anal canal, note:
The tone of the sphincter
Pain or tenderness
Thickening or masses.
The rectum
Feel all around the rectum as high as possible, and
Note the texture of the wall of the rectum and the presence of any masses or
ulcers. If you feel a mass, try to decide if it is within or outside the wall of the
rectum by testing the mobility of the mucosa over it. This is a most important
distinction.
Do not forget to feel the lower rectum, just above the anal canal. Posteriorly, the
rectum turns away at a right-angle, and it is easy to miss a small swelling in this
area.

Note the contents of the rectum. The rectum may be full of feces (hard or soft),
empty and collapsed, or empty but ‘ballooned out’. Feces may feel like a tumor but
are indentable, the only rectal mass that is.
If you can just detect a possible abnormality at your fingertip, ask the patient to
strain or push down. This will often move the mass down 1 or 2 cm or so and bring
it within your reach.
The recto-vesical/recto-uterine pouch
Turn your finger round so that the pulp feels forwards and can detect any masses
outside the rectum in the peritoneal pouch between the rectum and the bladder or
uterus. It takes practice to be able to tell the normal prostate and cervix from an
abnormal mass. Do not be downhearted if you get it wrong at first: experience and
confidence are needed.
Bimanual examination
The examination of the contents of the pelvis is helped if you place your left hand
on the abdomen and feel bimanually. This gives you a much better idea of the size,
shape and nature of any pelvic mass. You will find this method of examination
much more difficult in an obese patient.
The cervix and uterus
These structures are easy to feel per rectum and, with the help of bimanual
palpation; you should be able to define the shape and size of the uterus and any
adnexal masses. Do not call the hard mass that you can feel in the anterior rectal
wall a carcinoma until you are sure that it is neither the cervix nor a tampon.
The prostate and seminal vesicles
The normal prostate gland is firm, rubbery, bilobed and 2–3 cm across. Its surface
should be smooth, with a shallow central sulcus, and the rectal mucosa should
move freely over it. The seminal vesicles may occasionally be palpable just above
the upper lateral edges of the gland.
Benign hypertrophy of the prostate causes enlargement of the whole gland, which
bulges backwards into the rectum. However, the central sulcus is usually still there
unless the gland is very large. The gland may feel lobulated. The overlying rectal
mucosa remains uninvolved and mobile.
Carcinoma of the prostate may cause an irregular, hard enlargement which is often
unilateral. The edge of the enlarged area is indistinct. If the tumor has spread out
into the floor of the pelvis, you will feel thickening either side of the gland, which
can sometimes encircle the rectum. This lateral thickening is sometimes described
as ‘winging’ of the prostate. The central sulcus may be distorted or obliterated at
an early stage of the disease and the rectal mucosa fixed to the underlying gland.
Look at your finger, when you remove it from the rectum, to note the color of the feces
and the presence of blood or mucus.
Thank and cover the patient

EXAMINATION OF INGUINAL HERNIA
Setting …
*
Ask the patient to stand up
*
Always examine both inguinal regions.
Inspection:
Look at the lump from in front and assess:
the exact site and shape of the lump.
whether the lump extends down into the scrotum, if there are any other scrotal
swelling
any swelling on the ‘normal’ side.
Palpation:
Feel from the front
Examine the scrotum and its contents.
In men, first decide if the lump is a hernia or a true scrotal lump by examining its
upper edge.
Feel from the side
Having examined the scrotal contents and decided that you cannot get above the
lump, you can make a provisional diagnosis of inguinal hernia and proceed to
examine the lump itself. Stand at the side of the patient, on the same side as the
hernia. Place one hand in the small of the patient’s back to support him and your
examining hand on the lump with your fingers and arm roughly parallel to the
inguinal ligament and ascertain the physical characteristics of the lump.
Expansile cough impulse
Compress the lump firmly with your fingers, then ask the patient to turn his head
towards the opposite side, and then to cough. If the swelling becomes tense and
expands with coughing, it has a ‘cough impulse’. Movement of the swelling without
expansion or an increase in tension is not a cough impulse. The presence of an
expansile cough impulse is diagnostic of a hernia, but its absence does not exclude
the diagnosis.
Is the swelling reducible?
The main reason for standing at the side of the patient is to be able to place your
hand in exactly the same position as the patient places his own hand when he is
reducing or supporting the hernia. He puts his hand on the lump and lifts it
upwards and backwards. You must do the same. You can only do this if your arm
comes from a position above and behind the hernia. First, press firmly to reduce
the tension of the lump. Then gently compress the lower part of the swelling. As
the lump gets softer, lift it up towards the external ring. Once it has all passed in
through this point, slide your fingers upwards and laterally towards the internal
ring to see if the hernia can be controlled (kept inside) by pressure at this point. If
the lump reduces into or through the abdominal wall at a point above and medial
to the pubic tubercle, it is an inguinal hernia. If the point of reduction is below and
lateral to the pubic tubercle, it is a femoral hernia.
Note that this method of differentiation refers to the point where the lump
reduces, not the position of the unreduced hernia, because once a hernia reaches
the subcutaneous tissue it can expand and spread in any direction. If the hernia can
be held reduced only by pressure over the external inguinal ring, it is a direct
inguinal hernia. If it can be controlled by pressure over the internal ring, it is an
indirect inguinal hernia. If there is any difficulty in reducing the hernia, ask the
patient to lie down and try again. This will also allow you to examine the abdomen.
Remove your hand and watch the hernia reappear
The direction of movement of the swelling and the way in which it reappears will
help to confirm your deductions about its site of origin. A reappearing indirect
hernia will seem to slide obliquely downwards along the line of the canal,
whereas
a direct hernia will project directly forwards.
Percuss and auscultate the lump
Feel the other side
Examine the abdomen
Thank and cover the patient
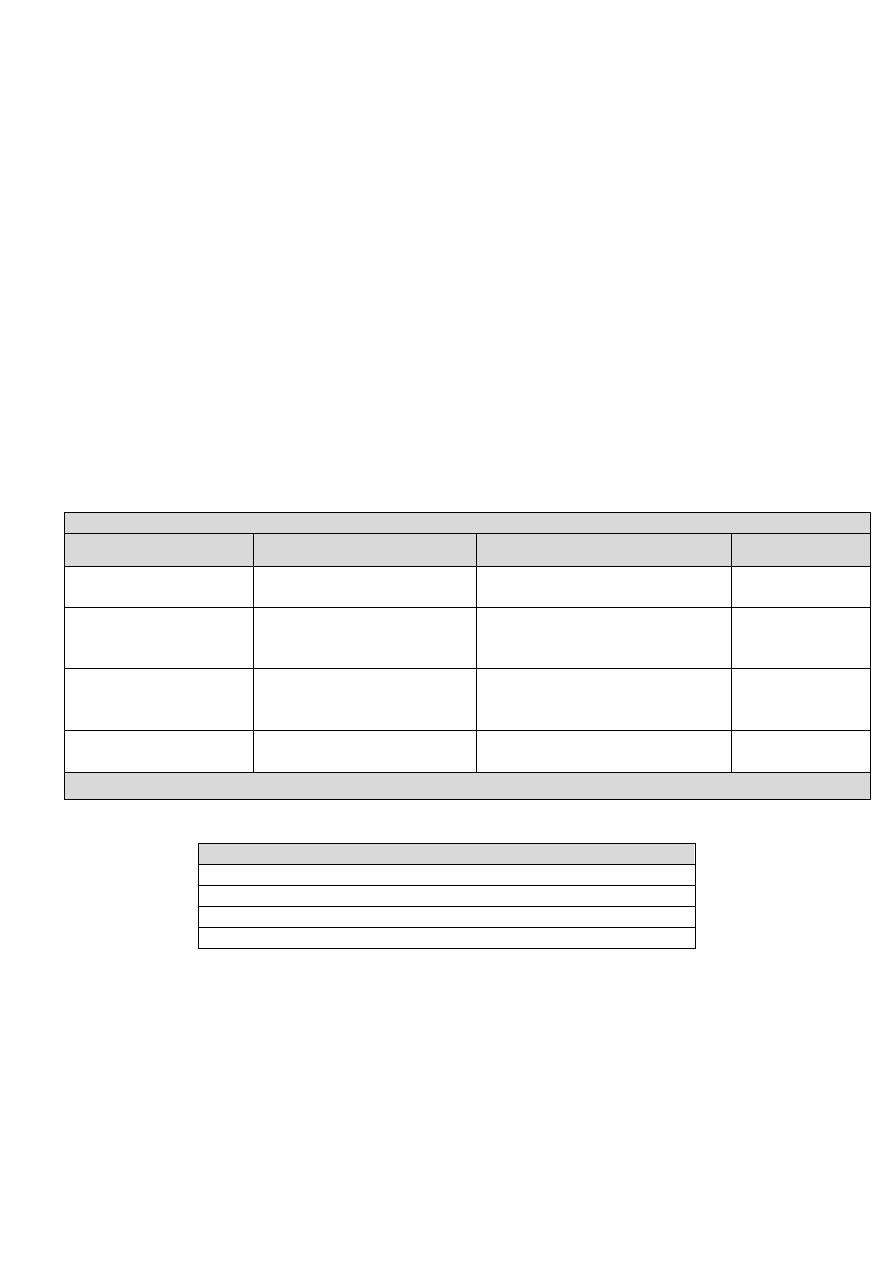
EXAMINATION OF A LUMP
Local examination
Site
Size
Shape
Surface
Depth
Color
Temperature
Tenderness
Edge
Composition:
consistence
fluctuation
fluid thrill
translucence
resonance
Solid, fluid or gas
pulsatility
compressibility
bruit
Vascular
Reducibility
Relations to surrounding structures - mobility/fixity
Regional lymph glands
State of local tissues:
arteries
nerves
bones and joints
General examination
EXAMINATION OF AN ULCER
Local examination
Site
Size
Shape
Base (Granulation tissue)
Depth
Edge
Sloping
Punched-out
Undermined
Rolled
Everted
Discharge
Temperature
Tenderness
Relations to surrounding structures - mobility/fixity
Regional lymph glands
State of local tissues:
arteries
nerves
bones and joints
General examination
