Dr. Ahmed Saleem
FICMS
TUCOM / 2015
SURGICAL HISTORY TAKING – GENERAL FORMULA
1. Introduction and demographics
2. Presenting complaint
3. History of presenting complaint
a) The story
b) Details of complaint
c) Review of relevant system
d) Relevant medical history
4. Past medical and surgical history
5. Medication and allergies
6. Social history
7. Family history
8. Full review of non-relevant systems
9. Summary
Taking a surgical history
Taking a relevant, concise and accurate history is an essential skill for a surgeon because it is during
the history that you will be able to make most diagnoses. Once you have this basic structure you will
find you can usually ‘fine tune’ it to a specific situation. It is especially important to have a basic
structure to rely on in the stressful situation of the exam.
1. Introductions and demographics
Introduce yourself and explain what you are doing. Check who they are, their relationship with
anyone they may have bought with them, how old they are and what they do for a living.
‘Hello, I’m Ali, a medical student ... Are you Mr. Hardy?’ (Smile and shake hands with the patient, do
not make assumptions – this can be very embarrassing if you are wrong – instead ask an open
question such as... ‘According to the letter I have here from your GP you are 70 and used to work as
a receptionist in the hospital. Is that correct?’
2. Presenting complaint
In order to determine a ‘presenting complaint’ such as ‘change in bowel habit for 6 months’ or ‘right
loin pain for 2 hours’ you need to initially ask them an open question such as ‘What has caused you to
come to the hospital?’ If they list a vast array of concerns and you remain slightly unclear as to the
main problem, ask them ‘What is the thing that’s bothering you most at the moment?’ Try and illicit
the duration of the problem. Again, if they are a bit vague, asking them when they were last well can
help. ‘When did this all start?’ or ‘When were you last well?’
3. History of presenting complaint
This is the story of the complaint as they describe it from when they were last well. ‘Tell me what’s
being happening?’ Gather details of the presenting complaint. For example, if it is pain, a systematic
way to approach this is using SIROD CASP:
Site: ‘Where is the pain?’
Intensity: ‘Can you rate the pain on a scale from 1 to 10. 1 being no pain and 10 the worst pain
ever,’ (this is subjective and it is more important to know how it affects their life, i.e. ‘Does it keep
you off work?’, ‘Does it wake you at night?’
Radiation: ‘Does the pain move anywhere else?’
Onset: ‘Does the pain come on suddenly or gradually?’
Duration: ‘How long does the pain last?’
Character: ‘What is the pain like?’ (If they require prompting, ask if it is sharp, dull, burning, or
colicky?)
Alleviating and exacerbating factors: ‘Does anything make the pain better, or worse?’
Symptoms associated with the pain: ‘Do you notice anything else when you get the pain?’ (e.g.
Jaundice, vomiting, change in bowels)
Previous episodes: ‘Have you had a pain like this before?’ (If yes...) ‘What did you do then?’
*If the complaint is not pain, you can still ask sensible, specific questions targeted to their problem.
Review the relevant system/s: for the example of abdominal pain this may include a GI, gynecological
and urological history but not the other systems unaffected by the presenting complaint. This requires
direct questioning about every aspect of that system and recording of the positives and negatives.
Relevant medical history: for instance with abdominal pain this would include any previous episodes
of pain, any abdominal surgery or investigations.
4. Past medical and surgical history
All the previous medical history of illnesses, operations, investigations not mentioned as relevant to
the history of the presenting complaint.
5. Medication and allergies
List of all drugs taken, doses and timings of these. List allergies and the nature of the reaction. Ask
directly about medications that may have to be stopped pre-operatively such as the oral
contraceptive pill, antiplatelet medications e.g. aspirin or clopidogrel, and warfarin.
6. Social history
• Smoking – current, ex or never and how many per day for how long.
• Alcohol – current, ex heavy drinker or teetotal and number of units per week.
• Recreational drug use (if appropriate).
• Where they live (nursing home, residential home, sheltered accommodation or own home.
• Who they live with – are they a carer for someone else?
• Who cares for them and whether they have social service input.
7. Family history
Any relevant family history not ascertained earlier, for instance a family history of diabetes in a
patient with an abscess.
8. Full review of non-relevant systems
This includes all systems not relevant to the presenting complaint. Depending on the time you have
left, you may be able to do a quick systems review. You should have already thoroughly reviewed the
systems relevant to the presenting complaint in the history of the presenting complaint section earlier
on. There might be an important fact to pick up on that the examiners want you to find.
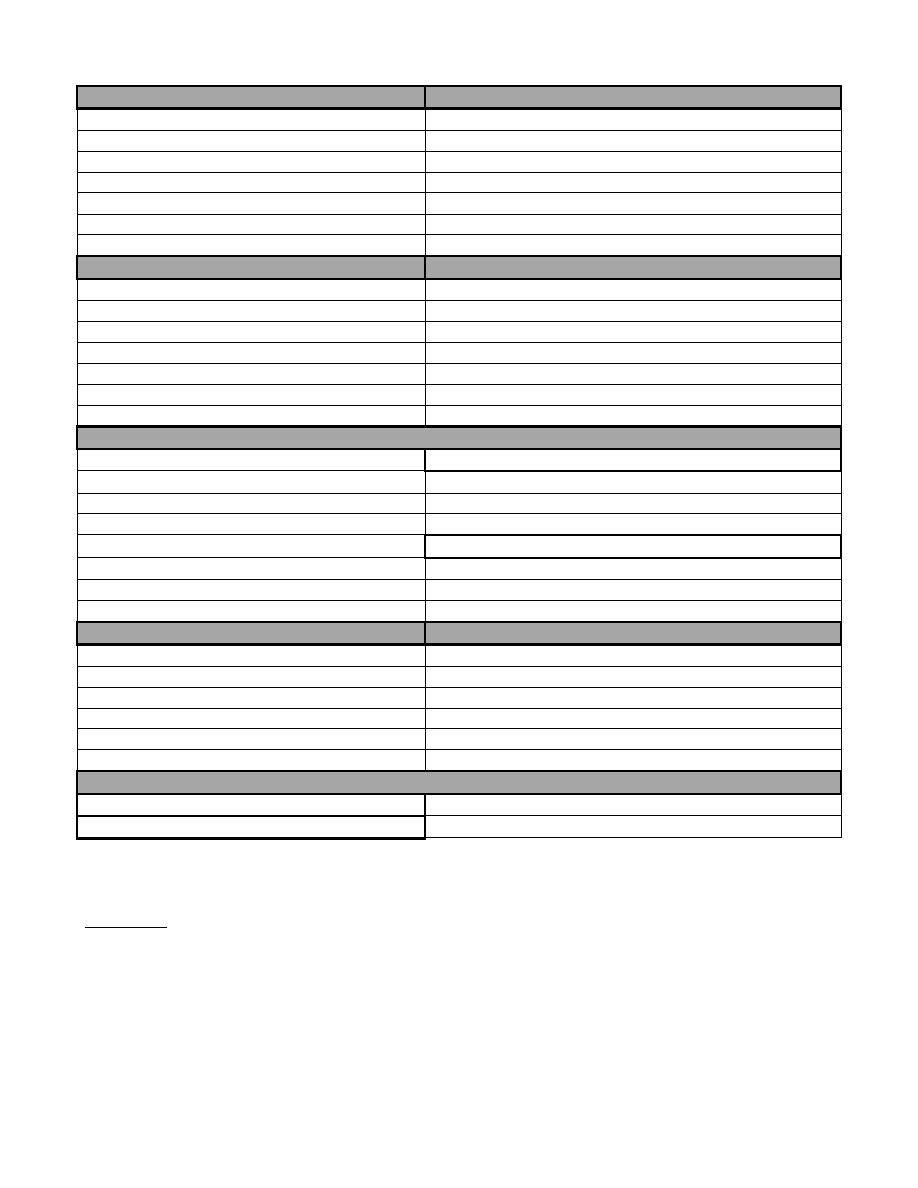
Cardiovascular:
Respiratory:
Chest pain
Cough
Dyspnea
Sputum
Palpitations
Shortness of breath
Paroxysmal nocturnal dyspnea
Exercise tolerance
Orthopnea
Hemoptysis
Ankle edema
Wheeze
Claudication
GI tract:
BOWELS:
Appetite
Frequency
Weight loss
Blood/slime
Dysphagia
Diarrhea/constipation
Indigestion
Melaena
Abdominal pain
Tenesmus
Hematemesis
Urgency
Incontinence
Genitourinary:
Incontinence
Men:
Dysuria
Prostatic signs: dribbling, hesitancy, flow rates
Hematuria
Impotence
Nocturia
Urethral discharge
Frequency
Women:
LMP/menopause
Pregnant?
Discharge
Neurological:
Locomotor:
Headaches
Pain
Fits
Stiffness
Faints
Function
Weakness
Swelling
Hearing
Vision
Thyroid:
Hyper:
Hot, sweaty, diarrhea, tremor, weight loss, palpitations
Hypo:
Cold, depressed, tired, constipated, deep voice
9. Summary
A summary allows you to check you have understood what the patient has been telling you and ensure that
you have not missed anything essential.
‘So, Mr. Hardy, you have said you have had 3 months of bleeding from the back passage. You also noticed
that you have lost some weight during this time and your appetite is not as good as it used to be. Are there
any other problems that I have missed?’
PRESENTING A SURGICAL HISTORY – GENERAL FORMULA
1. Introductory Sentence
2. Presenting complaint
3. History of presenting complaint
a) The story
Background to the illness
When last well
What exactly happened? (including timescale)
Treatment given/GP seen
b) Details of complaint
c) Review of relevant system
d) Relevant medical history
4. past medical and surgical history
A. Operations
B. Hospital admissions
C. Major illnesses
D. Question directly about:
Diabetes, Heart attack, Stroke, Hypertension, Epilepsy, Asthma, Bronchitis, Tuberculosis,
Rheumatic fever, Childbirth (women!), PE/DVT
5. Medication and allergies
6. Social history
A. Smoking/drinking
B. Home
7. Family history
8. Full review of non-relevant systems
9. Summary
Presenting a surgical history
It is important to practice presenting histories, either to your consultant/other colleagues at work,
friends or family. By doing this, your presentation will become precise and accurate.
The presentation to the consultant should follow a logical structure, contain appropriate clinical
language, pick out the key points and should cover the information obtained thoroughly but
succinctly.
Questions you may be asked:
• What differential diagnosis would you suggest at this stage based on the history you have taken?
• What signs would you specifically look for when examining this patient?
• What investigations would you request for this patient?
When presenting, make sure that you are sitting up straight, looking the examiner in the eye and
speaking in a clear, measured voice.
1. Introductory Sentence
Name, age, sex and occupation.
‘I would like to present Matthew Hardy, a 47-year-old male, chemistry teacher.’
2. Presenting Complaint
In one or two words state the MAIN COMPLAINT that has caused the patient to be referred to the
hospital and the time that they have been suffering from it. ‘His presenting complaint is a 3-month
history of weight loss and bloody diarrhea.’
3. History of the Presenting Complaint
A. The story:
Background to the illness
When last well
What exactly happened? (Including timescale)
Treatment given/GP seen
‘The history of the presenting complaint: Mr. Hardy is a gentleman who was fit and well until 3
months ago. The first thing he noticed was that he started to open his bowels three to four times
per day, having previously only opened them once a day. He initially thought it might pass, but it
continued and he became worried when he noticed what looked like blood mixed in with the loose
stool. During the last 2 weeks he’s been experiencing some lower abdominal pain. He’s lost about a
stone in weight during this time and when his symptoms didn’t settle he went to see his GP.’
B. Details of the complaint
If it’s a pain – SIROD CASP
‘The pain was described as a gradual-onset, intermittent, colicky ache specific to his left iliac fossa.
At worst he scored it 8/10 and it is normally aggravated when opening his bowels and relieved by
taking codamol. The pain lasted up to 3 hours and had made him nauseous. He hasn’t experienced
a pain similar to this before.’
C. Review of the relevant system (GI tract in this case)
‘In addition to his weight loss, Mr. Hardy has noticed a decrease in his appetite. He has no problems
with swallowing and doesn’t suffer from indigestion. Although he has had increased frequency of
his motions he doesn’t complain of tenesmus.’
D. Relevant medical history
‘Mr. Hardy has had no previous problems with his bowels apart from having occasional trouble
from hemorrhoids.’
4. Past Medical and Surgical History
A. Operations
B. Hospital admissions
C. Major illnesses
D. Question directly about:
Diabetes, Heart attack, Stroke, Hypertension, Epilepsy, Asthma, Bronchitis, Tuberculosis, Rheumatic
fever, Childbirth (women!), PE/DVT
‘Apart from an appendectomy performed 5 years ago, Mr. Hardy has never been in hospital.’
5. Medication/Allergies
List all the tablets the patient is currently taking. You may have to remind women about the pill or
HRT, which they often don’t include as medication.
‘Mr. Hardy does not take any regular medication and has no known allergies.’
6. Social History
A. Smoking/drinking
‘Mr. Hardy used to smoke 30 cigarettes a day, but gave up five years ago. He only drinks a few pints
of beer at the weekend.’
B. Home
‘Mr. Hardy lives with his wife and one daughter, aged 5.’
7. Family History
‘Apart from his father’s bowel cancer, there is no other family history of note.’
8. Review of Non-relevant Systems
‘There is nothing of note on review of his cardiovascular, respiratory or other systems.’
9. Summarize
Summarize the main points of the history in one short sentence.
‘In summary, Mr. Hardy is a 47-year-old man, normally fit and well, who presents with a 3-month
history of increased frequency of bowel motions, rectal bleeding and significant weight loss.’
HISTORY FORMULA OF A LUMP OR AN ULCER
1. Duration
When it was first noticed?
2. First symptom
What brought it to the patient notice?
3. Other symptoms
What symptoms does it cause?
4. Progression
How has it changed since it was first noticed?
5. Persistence
Has it ever disappeared or healed?
6. Multiplicity
Has (or had) the patient any other lumps or ulcers?
7. Cause
What does the patient think caused it?
