
1
Fifth stage
Pediatric
Lec-3
.د
رياض
28/3/2016
Infectious Diseases-1
Meningitis
Causes and clinical picture:
It is inflammation of meninges by bacteria, viruses or fungal. Most serious is bacterial M.
Bacterial men.is life treatening infection so it need rapid diagnosis and prompt antibiotic
therapy,any delay in suggestion and in antibiotic treatment will lead to serious mortality
and morbidity states.It is medical emergency. features ; headache,fever,
vomiting,irritability,seizures,neck stiffness,kerning sign and brudziniski sign are +ve.
Liumber puncture should be done to diagnose the CSF finding, and should be early
without delay for the start of antibiotics.fundoscopy should be done to exclude
papillodema.or CT SCAN OF BRAIN but here should take blood culture and give first dose
antibiotic before sending for CT scan.
Complications:
Bacterial meningitis is serious condition and if not treated rapidly; may have mortality by
30%. Delay in treatment may lead to meningoccemia, DIC
Multiorgans failure, or morbidity post meningitis problems as hydrocephalus, epilepsy
,cranial nerve palsy, subdural effusion,sensorineural hearing defect.
Some misdiagnosed cases may be partially treated by outpatient doctors by oral
antibiotics and lead to diagnostic confusion.
Lumber puncture:
Contraindicated in;
Increased intracranial pressure as indicated by focal neurological sign and bradycardia
and by papilloedema or persistent tense bulging fontanele in case of still open. or if the
patient is depressed in mentation or be cardiorespiratory compromise, or if has
infection at the lumber site
2
Treatment:
Should be rapid by conservative fluid therapy and antibiotics; Imperical therapy
combination of ceftriaxone+vancomycin+acyclovir if viral cause cannot excluded. Then
specific antibiotic according culture &sensitivity result can be choosed. Steroid usually
dexamethasone should be started soon; together or before the start of antibiotics to
get benefit from its anti-inflamatory effect and to reduce adhesions in the meninges.
Continue therapy for10-14 days.
Bacteria agent are; N.meningitis, H.influenza b.,pneumococcus; are most common
Partially treated meningitis:
Partially treated bacterial meningitis
It is due to wrongly antibiotics given before considering the real diagnosis in the patient
as erroneously some doctors miss the diagnosis and give oral or injectable antibiotics on
assumption of simple upper respiratory infection for at least 24 hours and so this will
mask the CSF findings. Usually CSF will show normal pressure and normal sugar,proteins
remain elevated for some days and cells may show lymphocytosis, and gram stain and
culture may be negative.Diagnosis for bacterial antigens by latex agglutination test for
CFS may detect positive finding for pneumococcus,meningococcus,or H,influenza
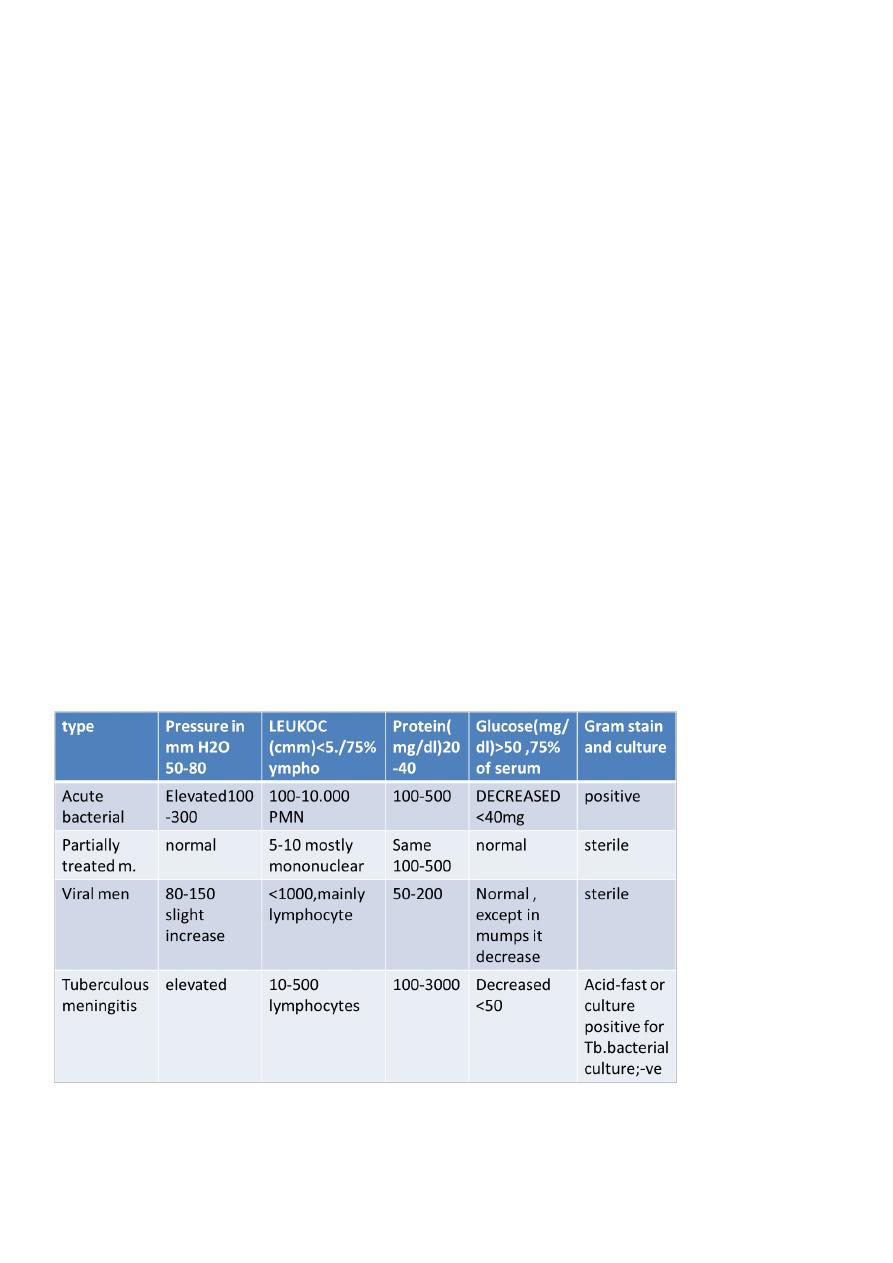
CSF finding in meningitis:

3
Pertussis Syndrome
ETIOLOGY
The pertussis is MOSTLY disease caused by Bordetella pertussis )a gram-negative
pleomorphic bacillus ( . Vaccine for this available DPT
Bordetella parapertussis, which causes a similar but milder illness that is not affected by
B. pertussis vaccination
Adenoviruses have been associated with the pertussis syndrome.
EPIDEMIOLOGY
The mean incubation period is7-10 days , range 4-21 days.
pertussis is very common and important to know this illness.It is called one( month
cough disease).
Patients are most infectious during the catarrhal stage till after 3 weeks of coughing
stage.Three stages each 2wks durations catarrhal,paroxysmal,convalescent
CLINICAL MANIFESTATIONS
pertussis is the syndrome seen in most infants 1-month to school age. The progression of
the disease is divided into:
1. The catarrhal stage is marked by nonspecific signs (upper respiratory tract infection
as running nose, sneezing and low-grade fever) that last 1wk.
2. The paroxysmal stage :coughing stage; is the most distinctive classic stage of
pertussis. Coughing occurs in paroxysms (episodes) during expiration, causing young
children above 6 months to lose their breath and even apnea followed by high pitch
inspiratory sound –whoop
The forceful inhalation against a narrowed glottis that follows this paroxysm of cough
produces the characteristic whoop .
Post-tussive emesis should raise the suspicion of pertussis .Facial congestion and
cyanosis may be seen in the attack. This stage lasts 2- weeks. Pertussis may produce
anoxic brain damage and even encephalopathy.
3. The convalescent stage is marked by gradual resolution of symptoms over 1 to 2
weeks. Coughing becomes less severe, residual cough may persist for months
Infants below 3 months and neonates may get the illness due to lack of maternal
immunity,may not give the classic pertussis syndrome; the first signs may be
episodes of repetitive coughing and some may develops apnea.. Adolescents and
4
adults with pertussis usually present with a prolonged cough without whoops many
weeks to months. Physical examination is nonspecific
LABORATORY AND IMAGING STUDIES
1. Culture of nasopharyngeal swabs.
2. Direct fluorescent antibody staining of the swab from nasopharynx.
3. PCR is useful .
4. Leukocytosis (15,000–30,000 cells/mm3) due to absolute lymphocytosis.
5. Radiological X-R ; not specific, It may show segmental lung atelectasis to develop
during pertussis, especially during the paroxysmal stage. Perihilar infiltrates are
common and are similar to what is seen in viral pneumonia. Secondary bacterial
pneumonia may develop.
DIFFERENTIAL DIAGNOSIS
1. Respiratory viruses such as RSV, parainfluenza virus, and Chlamydia pneumoniae can
produce bronchitic illnesses among infants.
2. In older children and young adults, Mycoplasma pneumoniae may produce a prolonged
bronchitic illness that is not distinguished easily from pertussis in this age group.
TREATMENT
Erythromycin,, or Azithromycin if given early in the course of illness it eradicates organisms
within first 3 to 4 days in (catarrhal stage), and it abort and stop the course of infection.
Treatment is indicated during the first 3 weeks of whooping cough stage illness to reduce
the severity and infectivity, but it does not treat the the coughing. Antibiotics reduce the
risk of infectivity to contacts when given for full 5 days course during the infectivity period
(first 3 wks of coughing illness). It also should be given to contacts members regardless of
their vaccination. When given to neonates pt. younger than 4 weeks old, clarythromycin or
erythromycin may rarely been associated with pyloric stenosis, but treatment is still
recommended because of the seriousness of pertussis in this age. Azithromycin has less
such side effect and is drug of choice for neonates for 5 days.
COMPLICATIONS
1. Hypoxia
2. Apnoea specially in young infants.
3. Pneumonia : caused by B. pertussis itself or resulting from secondary bacterial infection

5
4. seizures, encephalopathy
5. failure to thrive.
6. Atelectasis may develop
7. The force of the paroxysm may rupture alveoli and produce pneumothorax,
8. epistaxis; and retinal and subconjunctival hemorrhages, hernia
9. Otitis media and sinusitis may occur.
Infants <4 mo of age account for 90% of cases of fatal pertussis
PREVENTION
Active immunity can be induced with acellular pertussis vaccine, given in combination with
the toxoids of tetanus and diphtheria (DTaP). Pertussis vaccine has an efficacy of 70% .the
efficacy declines if fewer vaccinations given.
Compared with older, whole cell pertussis vaccines, acellular vaccines have fewer adverse
effects and local reactions .
Patient who have pertussis produce life long immunity.
Erythromycin is effective in preventing disease in contacts exposed to pertussis. Close
contacts younger than 7 years old who have received four doses of vaccine should receive a
booster dose of DTaP.They also should be given erythromycin. Close contacts older than
age 7 should receive only prophylactic erythromycin 5 days, but not the vaccine.
Immune deficiency status
Immunity depend on humoral antibodies produced by B-lymphocytes ,and complements.
While cellular immunity depends on T-lymphocytes, and neutrophils.
Humoral antibodies is mainly to bacterial infection .
Cellular T-CELL mainly to viral and fungal infection.
May be primary due to genetic defects or inherited or may be secondary causes like AIDS or
malignancy or drugs.
PRESENTATIONS OF IMMUNE DEFICIENCY
Recurrent bacterial infections.
Severe bscterial infections; like meningitis and sepsis.
Infections with unexpected opportunistic m.o.

6
Extensive candidiasis.
Abscesses any where in the body skin or internal organs.
Delayed separation of umbilical cord in newborn.
HIV infection AIDS
Route of infection is mother to child by transplacental or during delivery or by breast
feeding from infected mother. To children may be by blood products or unsterile needles.
Diagnostic tests
Less than 18 months born to infected mother is by HIV DNA- PCR.
For older than 18 m.is by antibodies and antigens of HIV .
Clinical features of AIDS
May remain sublinical for 1yr in infants and for many months for children untill symptoms
appears ; as prolonged fever PUO, faiure to thrive. chronic diarrhea, candidiasis TB,
lymphadenitis,hepatosplenomegaly, serious infections.
ROSEOLA INFANTUM
Epidemiology
caused by human herpesvirus (HHV) type 6 (HHV-6) for<2yrs old 80% of cases; and less
frequent in
10-30% of cases by HHV-7 in older than 2 yr.
Are DNA viruses, which are of the herpesvirus family
HHV-6 is a major cause of acute febrile illnesses in infants and may be responsible for
20% of visits to the emergency department for children 6 to 18 months old.
Clinical Manifestations
Roseola is characterized by high fever (often ≥40°C) lasting 3 to 4 days followed by
maculopapular, rose-colored pruritic rash that appears with the remission of fever.
The rash usually lasts 1 to 2 days but may fade rapidly
Roseola is associated with approximately one third of febrile seizures

7
Treatment
There is no specific therapy for roseola. Routine supportive care includes maintaining
adequate hydration and antipyretics
ERYTHEMA INFECTIOSUM (FIFTH DISEASE)
Epidemiology
caused by the human parvovirus B19
Single stranded DNA virus.
Benign self-limited illness affecting any age mostly 5-15 yrs old and even adults .
Incubation period average 15-17 days .It is transmitted by respiratory secretions
airborne route.
it an important cause of aplastic crisis in patients with hemolytic anemias like
thalassemia, sickle anemia,& spheroytosis. Parvovirus B19 also causes severe fetal
anemia and even hydrops fetalis after primary infection during pregnancy
Clinical Manifestations
1. usually begin with a mild prodromal nonspecific illness characterized by low grade fever,
malaise, myalgias, and headache.
2. This illness is followed by the characteristic rash within few days (Erythema Infectiosum).
The rash appears in two stages
A. erythematous cheeks, appearing as a "slapped cheek" rash
B. After 1-4 days an erythematous symmetric, maculopapular, involves trunk and limbs
rash appears, later central clearing takes place in the rash, giving a distinctive lacy,
reticulated rash مشبكthat lasts few days to even 1-3 weeks. This rash may be pruritic, does
not desquamate – and it waxes and wanes with exposure to sunlight, heat, exercise and
stress.
3.Arthralgia .
4.Main abnormalities occur in CBC with parvovirus infection, includes low reticulocyte
count and anemia due to low RBCs production by bone marrow; which may be mild anemia
or may be severe called : aquired pure red cell anemia, or in pregnancy ; fetal anemia and
hydrops fetalis.

8
Investigations
Includes CBC showing; Low RBC count and; Low Reticulocyte count; and
Parvovirus B19 can be detected by PCR .
Treatment
There is no specific therapy.
Routine supportive care.
Transfusions may be required for ; transient aplastic crisis in pt. with hemolytic
diseases or in ; aquired pure red cell anemia.
Intrauterine transfusion has been performed for hydrops fetalis associated with fetal
parvovirus B19 infection.
VARICELLA-ZOSTER VIRUS INFECTION
Chickenpox
DNA virus that is a member of the herpesvirus family
Humans are the only natural host.
VZV (chickenpox) is highly communicable among susceptible individuals.
It is mild disease in young children but may be severe in adult and in
immunocompromised children
Chickenpox pt. and pt with zoster lesion (shingles) infect susceptible child leading to
chicken pox illness.
the period of infectivity to others; ranges from 2 days before to 7 days after the onset
of the rash till when all lesions are crusted and dried.
Epidemiology
the peak age of 5 to 10 yr.
peak seasonal infection in late winter and spring
Transmission is airborne route by inhalation of the virus; by direct contact with the
lesions before dried or crusted, or by air droplet from sneezing or coughing of the
patient in the catarrhal stage.
Clinical Manifestations
The incubation period of varicella is generally 14 to 16 days

9
Prodromal symptoms of fever, malaise, and anorexia, running nose may precede the
rash by 1 day
The characteristic rash appears initially as small red papules that rapidly progress to
oval, "teardrop" vesicles on an erythematous base and in crops (different lesions) of
lesions: papules and vesicles. The fluid progresses from clear to cloudy, and the vesicles
ulcerate, crusted, and dried and heal.
New crops appear in 3 to 4 days, usually beginning on the trunk followed by the head,
the face, and, less commonly, the extremities., with all stages of lesions being present
at the same time(crop). Pruritus is universal.
Periods of illness is about 1-2 weeks .
Shingles(herpes zoster) is recurrence of VZV infection in previously infected child.
Congenital varicella
Fetal varicella during first 6 months of pregnancy includes followings pathological
effects: low birth wt, cortical brain atrophy, mental retardation, cataract, microcephaly,
cicatrical scarring of body and limbs with aplasia of fingers and toes .
Treatment
Symptomatic therapy of varicella includes nonaspirin antipyretics, cool baths, and
careful hygiene.
ANTIVIRAL(acyclovir) THERAPY indicated ;IN infected :
1.immunocompromised persons,
2.adult above 15 yrs
3.neonates less than 28 days old of un- immunized mother, and in premature baby
whatever the mother immunity; because the baby will not receive immunity from
mother and his illness will be severe
Complications
Varicella is a more severe disease for neonates, adults, and immunocompromised
persons.
Secondary infection of skin lesions by streptococci or staphylococci is the most
common complication
hemorrhagic lesions may occur, known as varicella gangrenosa
Pneumonia is uncommon in healthy children, but may occurs in 15% to 20% of healthy
adults and in immunecompromised persons .
Reye syndrome when aspirin used .
Encephalitis and postinfectious cerecbellar ataxia , Guillain-Barrie syndrome

10
Prevention
Varicella vaccine is live attenuated , is recommended for routine administration to
children with 2 doses: at 12 mo and at 4–6 yr of age.
Passive immunity can be provided by VZIG, which is indicated within72 hours of
exposure to infected pt. in those individuals at increased risk for severe illness,
including:
1.immunocompromised persons,
2. neonates of infected mothers who had onset of chickenpox within 5 days before
delivery or 48 hours after delivery to prevents getting infection because it will be
severe and may be fatal.
3.Newborn of un-imunized mother and premature baby.
Newborn of mother with previous imunity, will be protected and no needs for VZIG if
exposed to pt.
4.Adult and ages 15 yr and older, who are exposed to infection.
