1
Fifth stage
Gynecology
Lec-3
د.براء
17/4/2014
Common gynecological procedures
Myomectomy
A myomectomy is an operation to remove fibroids while preserving the uterus.
For women who have fibroid symptoms and want to have children in the future,
myomectomy is the best treatment option.
Myomectomy is very effective, but fibroids can re-grow )recurrence). The younger the
patient is and the more fibroids she has at the time of myomectomy, the more likely is
the recurrence in the future.
Indications
1. Abnormal uterine bleeding, causing anemia
2. Severe pelvic pain
3. Large or multiple (Palpable per Abdomen)
4. Pressure Symptoms (Urinary tract symptoms)
5. Postmenopausal or rapid growth
6. Obscuring evaluation of adnexa
7. Indications in Infertility:
Deformity of Endometrial Cavity
Distortion of Fallopian Tubes
Fibroid associated with Unexplained Infertility
Approach:
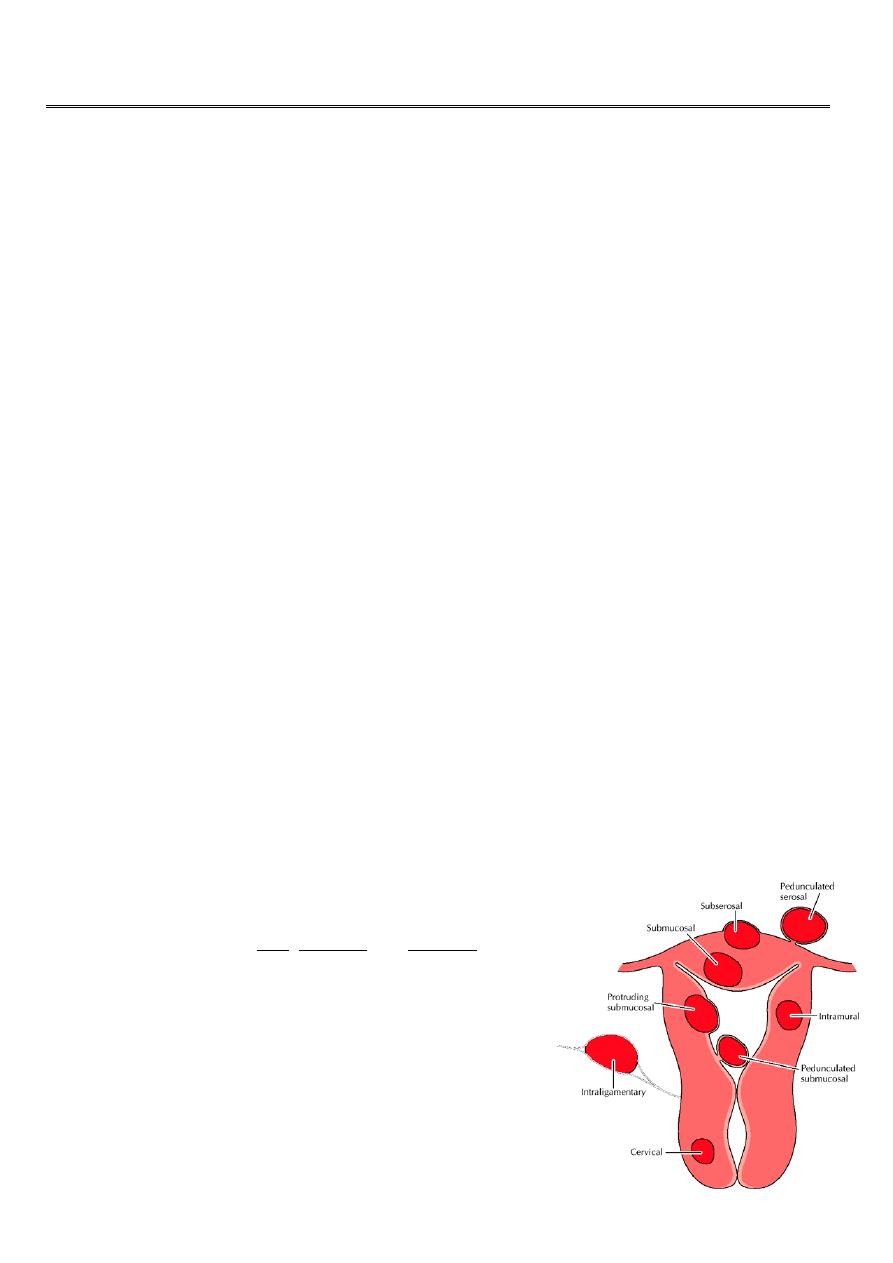
A myomectomy can be performed in several different
ways depending on the size, number and location of the
fibroids:
Abdominally (open)
Laparoscopic
Hysteroscopic
o Primarily for submucosal fibroids
Vaginal
o Primarily for pedunculated submucous fibroids
2
Abdominal Myomectomy
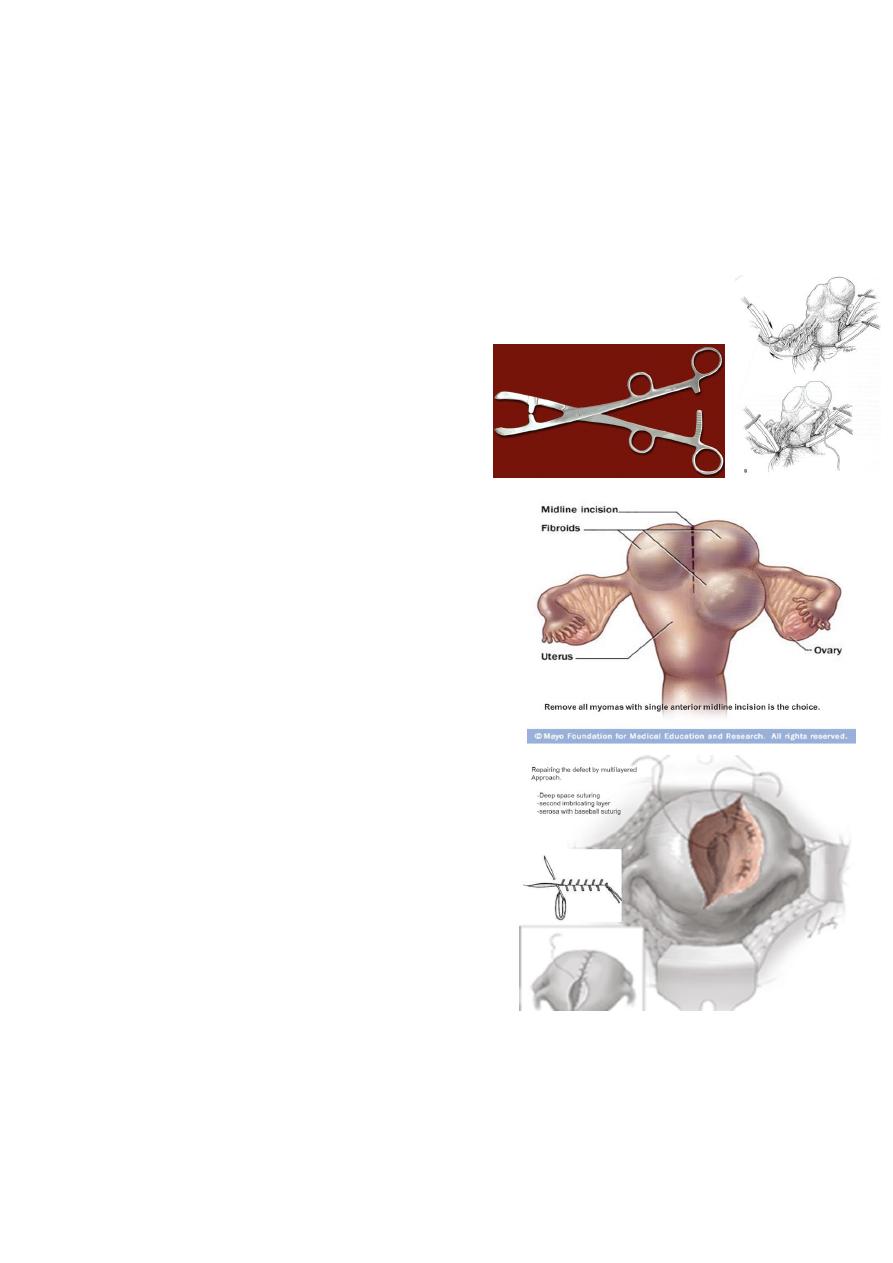
Technique:
1. Localization of myoma.
2. Non- crushing clamp or Torniquet.
3. Anterior midline incision.
4. enucleation.
5. Repairing the defect.
Place non crushing clamp across the ovarian
and uterine arteries to minimise blood loss
or use a tourniquet.
Attempt to remove all fibroids through a
single midline incision if possible (Avoids
vascular structures laterally. An anterior
incision is preferred to minimize the risk of later
adhesion of bowel & retroversion. ).
Tissue surrounding the fibroid is compressed
tightly forming a pseudocapsule
o No vascular bundle enters the myoma
o Identification of and dissection along this
plane will minimize blood loss
o Cleavage planes may be altered in those who
have been pretreated with GnRH analogue.
o Palpate the uterus for any remaining
fibroids.
Repairing defect
o Multi layered approach
Deep sutures to close dead space
Second imbricating layer
Close serosa with a “baseball stitch”
o May require removal of excess myometrial
tissue to allow adequate closure
Apply a sheet of adhesive barrier over the
incision line to avoids adhesion formation.

3
Morbidity
Intra operative:
Haemorrhage
Visceral Damage
Need for Hysterectomy
Post operative:
Myoma Fever – 33%
Sequelae:
Recurrence / Retreatment – 4-27%
Adhesions
Uterine Rupture in Labour (Rare)
Biggest complication is blood loss
Why Is Myomectomy Not Preferred?
Reputation as “bloody” operation
Fibroid recurrence is possible risk
Adhesion formation
“Hysterectomy usually is a simpler procedure than multiple myomectomy, as well as
the procedure to which most gynecologists are more accustomed” (Te Linde:
Operative Gynecology, Seventh Edition)
However, hysterectomy risks include:
Ureteral injury (0.1 - 0.5%)
Changes in libido (25-33%) and orgasm
Depression
Decreased time to ovarian failure
Laparoscopic Myomectomy
Limitations of laparoscopic myomectomy:
Special Equipment & Special skill required
Difficult in:
o Broad Ligament / Cervical/ deeply embedded
o Size >8cm
4
o Number >3 fibroids
Separate incisions needed
Closure of dead space & haemostasis difficult
Weaker scar
Increased Operating Time & Blood Loss
Inherent Complications of Laparoscopic surgery
Hysterectomy
A hysterectomy is an operation to remove a woman's uterus.
A woman may have a hysterectomy for different reasons, including:
Uterine fibroids that cause pain, bleeding, or other problems
Uterine prolapse,
Cancer of the uterus, cervix, or ovaries
Severe and intractable endometriosis and/or adenomyosis after pharmaceutical or
other surgical options have been exhausted.
Abnormal vaginal bleeding that persists despite treatment
Chronic pelvic pain, after pharmaceutical or other surgical options have been
exhausted.
Postpartum to remove either a severe case of placenta praevia or placenta percreta, as
well as a last resort in case of excessive obstetrical haemorrhage
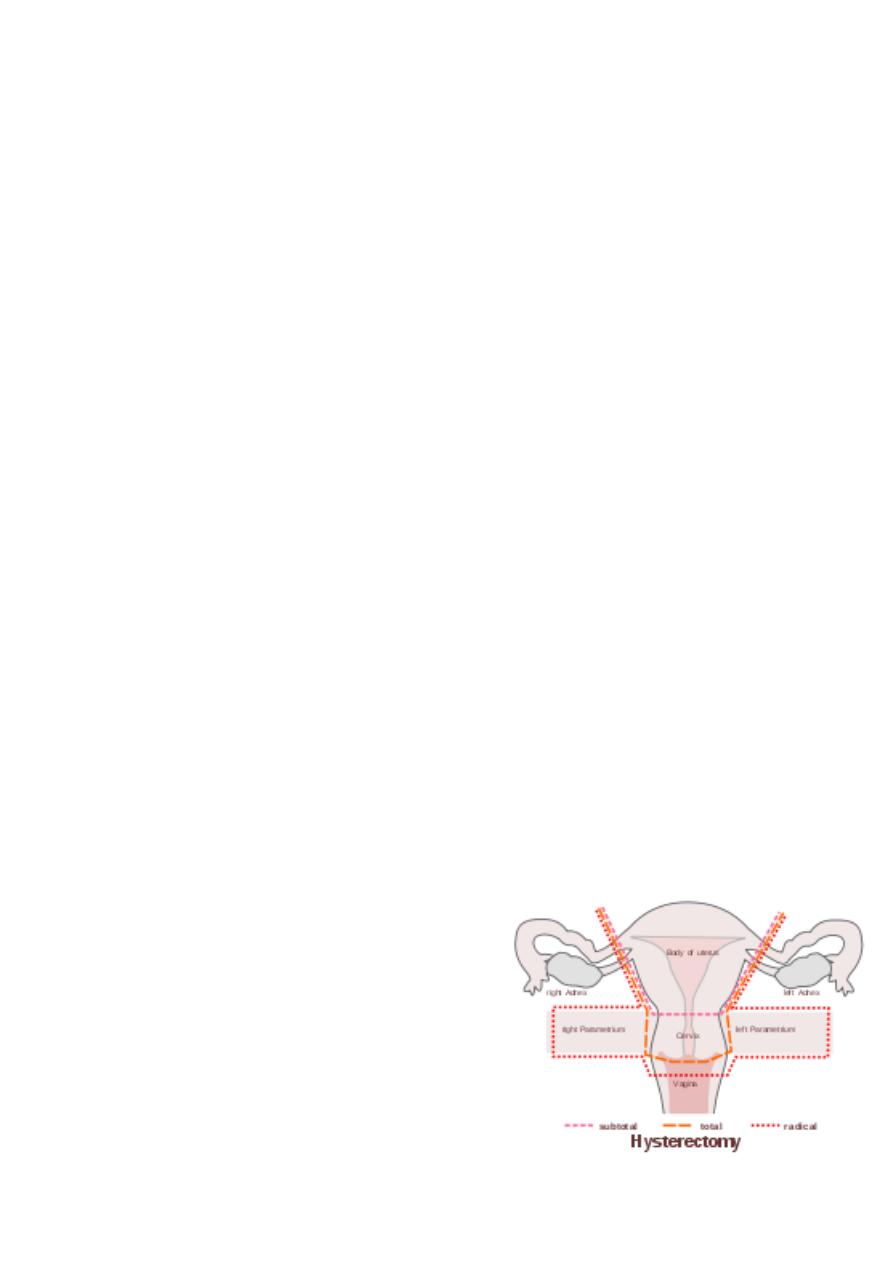
Types of hysterectomy:
Hysterectomy, in the literal sense of the word, means merely removal of the uterus.
However other organs such as ovaries, fallopian tubes and the cervix are very frequently
removed as part of the surgery.
Radical hysterectomy or Wertheim’s
hysterectomy : complete removal of the
uterus, cervix, upper vagina, and parametrium.
Indicated for cancer. Lymph nodes, ovaries and
fallopian tubes are also usually removed in this
situation.
Total hysterectomy : Complete removal of the
uterus and cervix.
Subtotal hysterectomy : removal of the uterus,
leaving the cervix in situ.

5
Despite speculation that there might be different sexual outcomes depending on
whether hysterectomy was subtotal, or total abdominal, this difference has
not been supported by recent studies
It is obvious that supracervical hysterectomy does not eliminate the possibility of
having cervical cancer since the cervix itself is left intact. Those who have undergone
this procedure must still have regular Pap smears to check for cervical dysplasia or
cancer
Approach:
There are several approaches that can be used for hysterectomy:
Abdominal hysterectomy
Vaginal hysterectomy
Laparoscopic-assisted vaginal hysterectomy: Using laparoscopic surgical tools, a
surgeon removes the uterus through an incision in the vagina.
Robot-assisted laparoscopic hysterectomy: This procedure is similar to a laparoscopic
hysterectomy, but the surgeon controls a sophisticated robotic system of surgical tools
from outside the body. Advanced technology allows the surgeon to use natural wrist
movements and view the hysterectomy on a three-dimensional screen.
Vaginal hysterectomy:
The main indication is second or third degree uterine prolapse.
There is trend nowadays to prefer vaginal to abdominal hysterectomy because the
morbidity &postoperative discomfort are less.
The contraindications:
1. Presence of genital tract malignancy
2. A uterus larger than 14 weeks in size
3. Narrow subpubic arch
4. Previous abdominal procedures where 5.bowel may be adherent to uterus or tubes
5. Uncertain ovarian pathology
The epithelium around the cervix is circumscribed ,the bladder freed &dissected upwards
&the uterovesical peritoneal pouch is entered .
The cervix is lifted forwards &peritoneum of the rectouterine pouch of Douglas identified &
opened, the uterosacral ligaments are ligated.
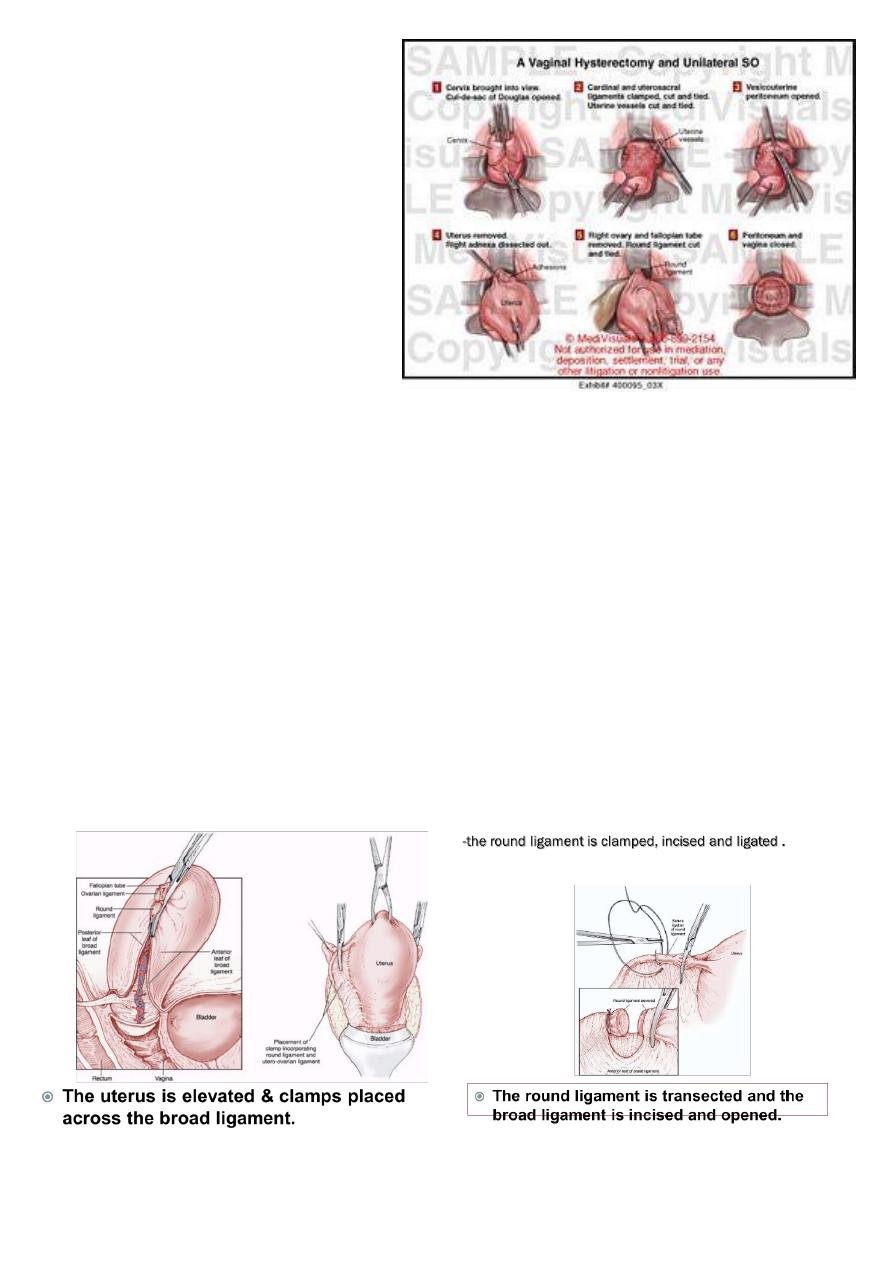
6
Next the uterine artery &cardinal
ligaments are identified & ligated.
Finally the ovarian pedicles are
similarly identified & ligated.
The uterus is removed & associated
anterior or posterior vaginal wall
prolapse are repaired &the vault
closed.
Abdominal hysterectomy:
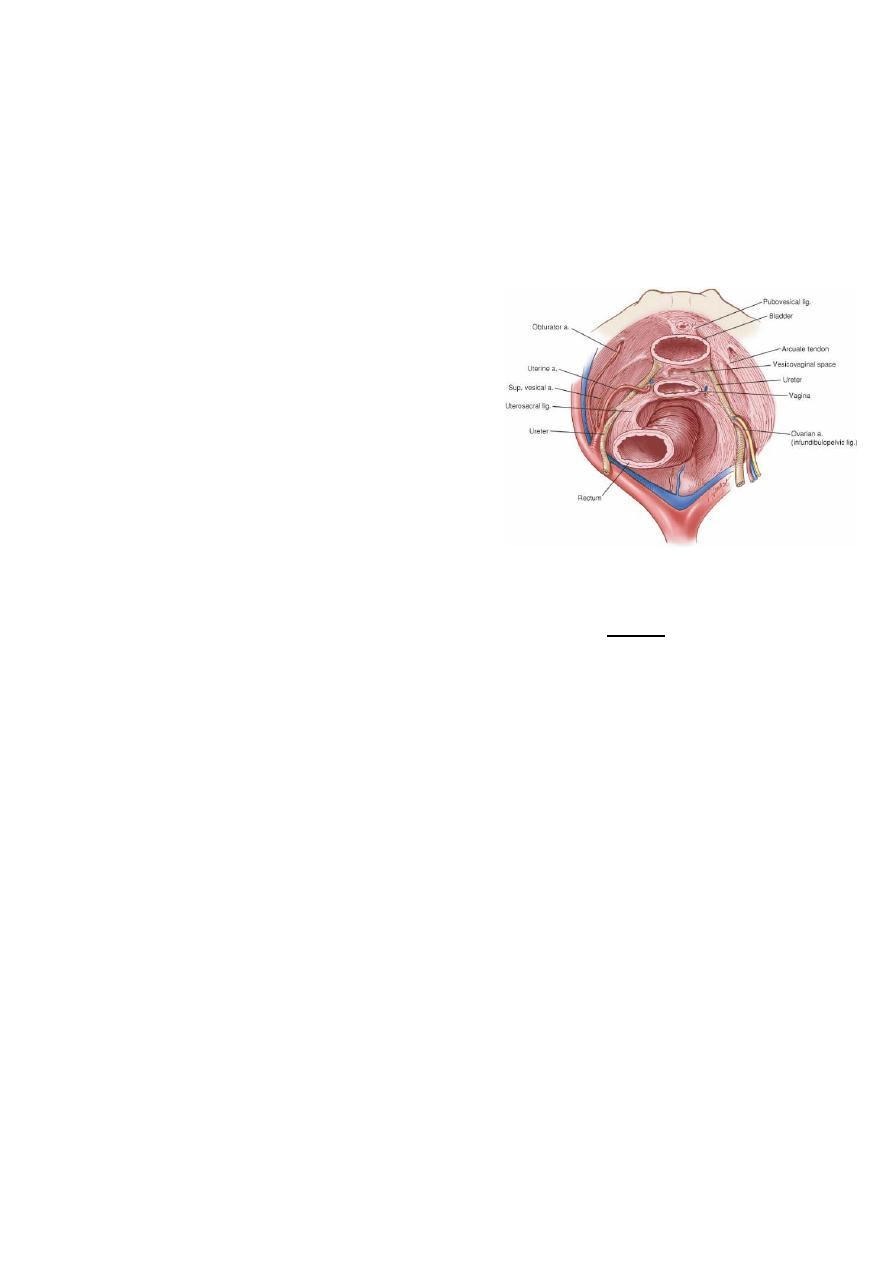
The same pedicles as in vaginal hysterectomy are clamped but in reverse order i.e. ovarian
followed by uterine, followed by cardinal ligaments.
Technique of abdominal hysterectomy:
-patient is supine under GA.
-skin incision:
• transverse lower abdominal incision.
• vertical incision.
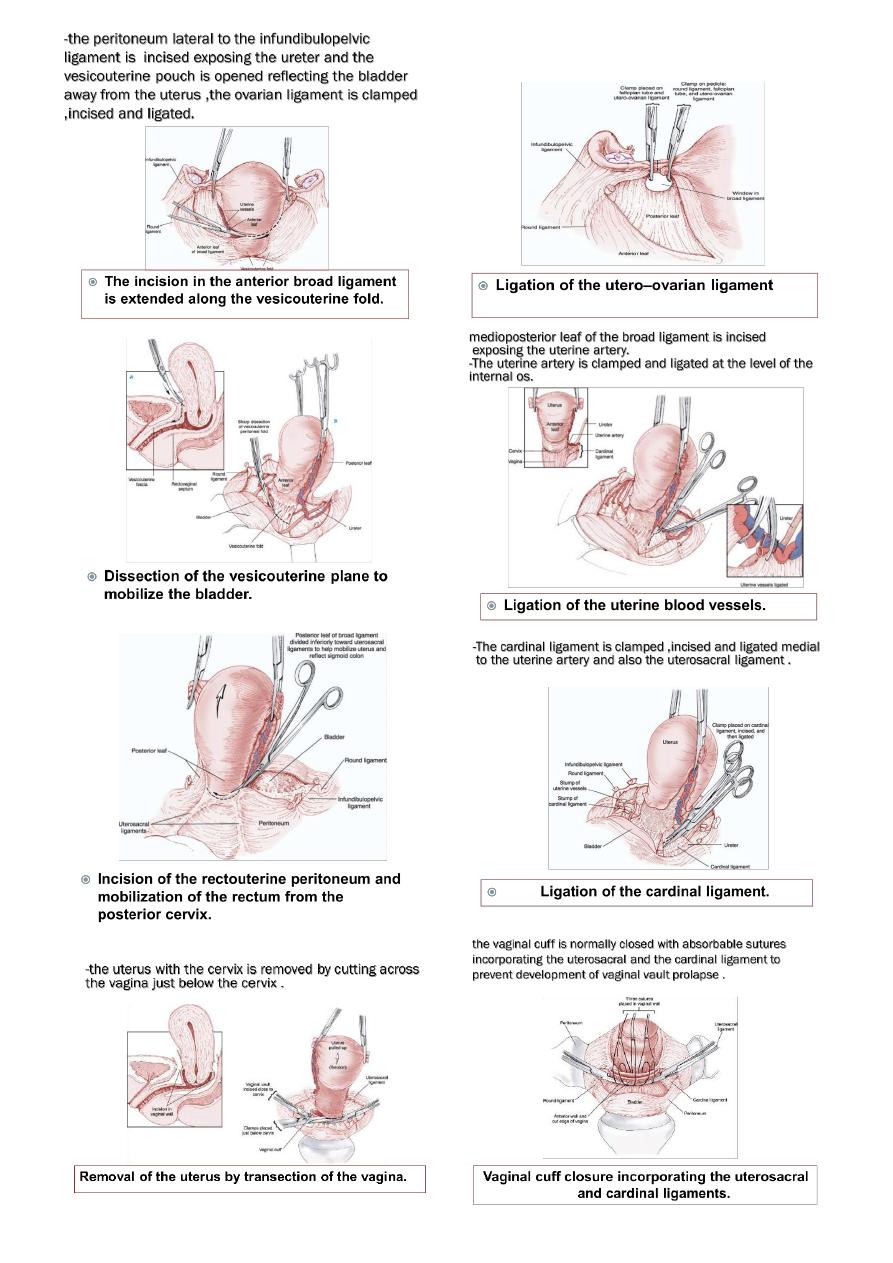
7
8
Complications
1. Anaesthesia complications
2. Primary haemorrhage due to slip ligature
3. Secondary haemorrhage due to infection
4. Damage to ureter ,bladder,or bowel
5. Infection with pelvic abscess
6. Late ;adhesion with intestinal obstruction.
-There is three points in the procedure presents
particular risk to injure the ureter:
o As the infundibulopelvic ligament are clamped
incised and clamped.
o As the uterine vessels are ligated.
o As the cardinal ligament is ligated if the
bladder is not reflected inferiorly enough.
Ovarian Cystectomy
Enucleation of a cyst from the overy is frequently carried out for benign cyst in women
below 40 years of age.
o The incision into the ovarian capsule must be made very carefully to prevent rupture of
the cyst.
o Once the cyst is enucleated,the ovary is carefully recostructed with meticulous
hemostasis to avoid ovarian hematoma.
