1
Fifth stage
Gynecology
Lec-4
.د
اسماء
13/4/2016
Malignant disease of the body of the uterus
Endometrial cancer may sometimes be referred to as uterine cancer. However,
different cancers may develop not only from the endometrium itself but also from
other tissues of the uterus, including cervical cancer, sarcoma of the myometrium, and
trophoblastic disease.
Corpus cancer accounts for 3% of cancer in females.
1.Endometrial carcinoma which arise from the lining of the uterus.
0r 2.Sarcoma arise from the stroma of endometrium or from myometrium.
The incidence is at 60 years & more ,75% of cases usually occur in the post menopausal
period
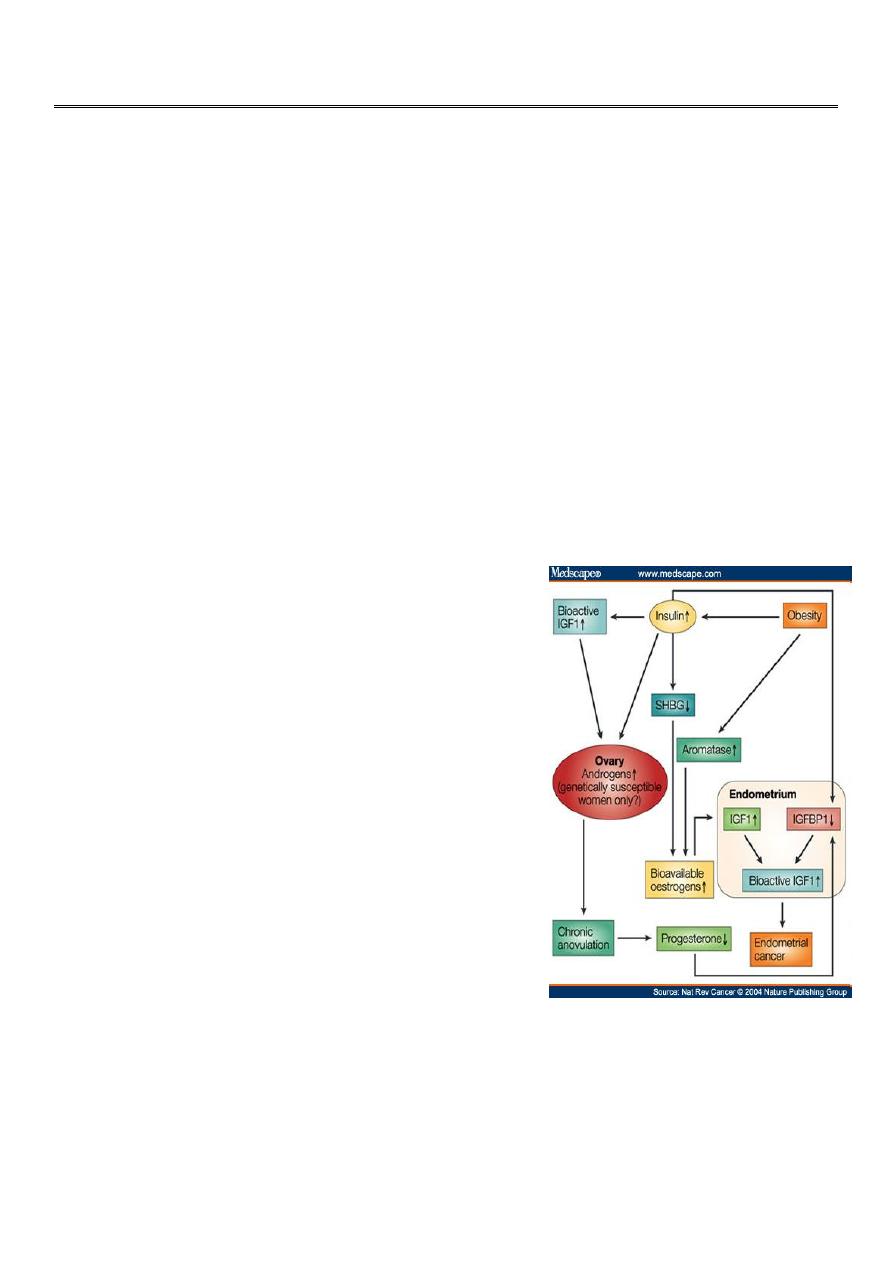
Risk factors for Endometrial Cancer:
high levels of estrogen
endometrial hyperplasia
obesity
hypertension
polycystic ovary syndrome[citation needed]
nulliparity (never having carried a pregnancy)
infertility (inability to become pregnant)
early menarche (onset of menstruation)
late menopause (cessation of menstruation)
endometrial polyps or other benign growths of the
uterine lining
diabetes
Tamoxifen
high intake of animal fat[citation needed]
pelvic radiation therapy
breast cancer
ovarian cancer
heavy daily alcohol consumption (possibly a risk factor)

2
Factors reduce risk of endometrial carcinoma:
oral contraception.
progestogens.
Smoking.
Pathology:
The histopathology of endometrial cancers is highly diverse. The most common finding is a
well-differentiated endometrioid adenocarcinoma, which is composed of numerous, small,
crowded glands with varying degrees of nuclear atypia, mitotic activity, and stratification.
This often appears on a background of endometrial hyperplasia.
Lymphatic spread occurs later and is less frequent than in cases of cervical carcinoma.
Remote metastases in lungs, bones or else-where are not common but occur more often
than with cervical carcinoma
Clinical presentation:
Symptoms
1. The classic symptom is bleeding
A. Post menopausal bleeding in 75-80 %.
This symptom should be assumed to be caused by carcinoma of endometrium until proved
otherwise. Women with post menopausal bleeding in women not taking hormone
replacement therapy has 10% risk of having a genital tract cancer
B. In premenopausal women may present as:
* intermenstrual bleeding
*menorrhagia.
2. Watery or purulent vaginal discharge (blood stained).
3. Pain is a late symptom and denotes extensive spread of disease.
4. Abnormal screening test.
Signs
A full general and systematic examination is indicated.
Enlarged lymph nodes in the groin or supraclavicular fossa may be found.
3
Breast should be palpated.
Uterine enlargement can be palpated.
Pelvic examination:
Bleeding through cervix.
Secondary metastasis in vagina, urethra.
Investigations:
A Pap smear may be either normal or show abnormal cellular changes.
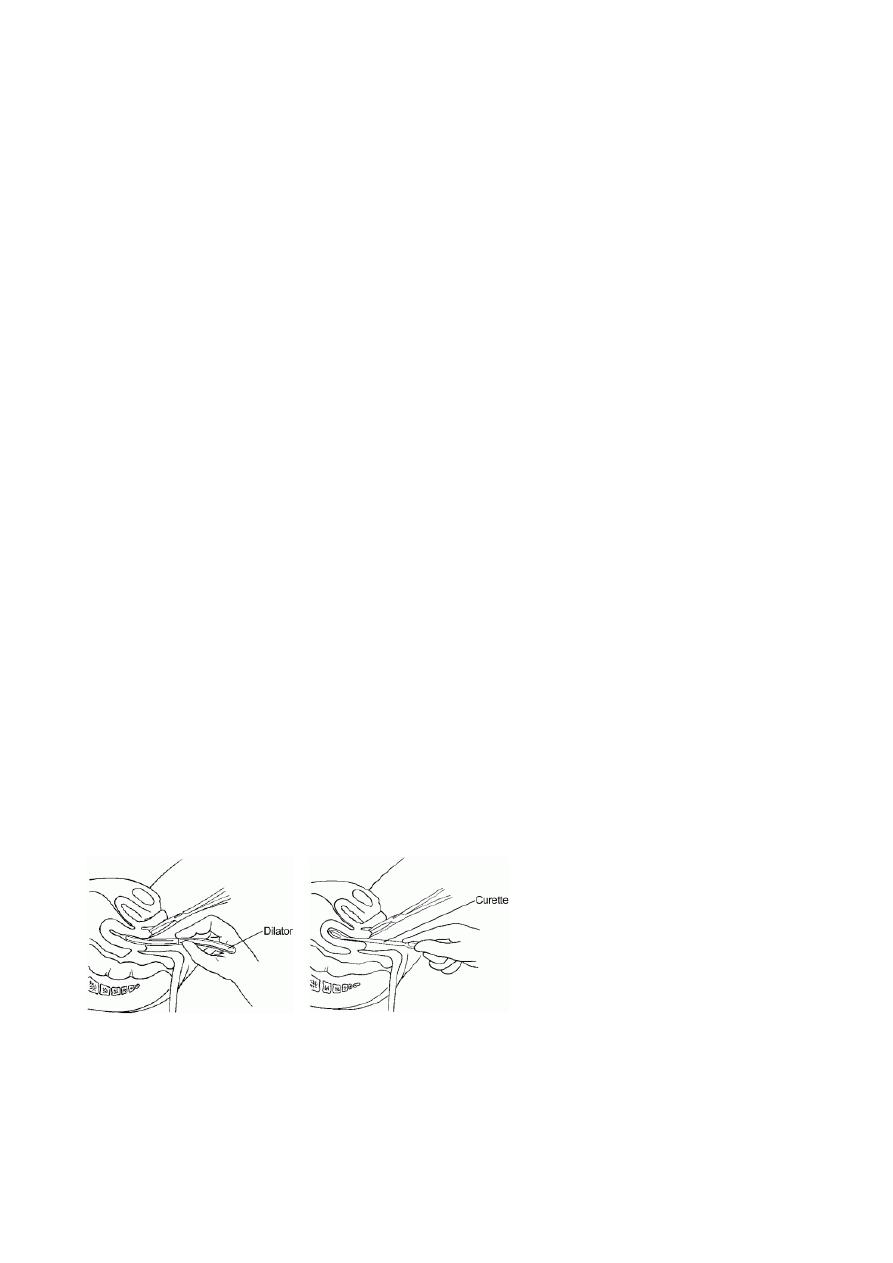
Endometrial curettage is the traditional diagnostic method. Both endometrial and
endocervical material should be sampled.
If endometrial curettage does not yield sufficient diagnostic material, a dilation and
curettage (D&C) is necessary for diagnosing the cancer.
Hysteroscopy allows the direct visualization of the uterine cavity and can be used to
detect the presence of lesions or tumours. It also permits the doctor to obtain cell
samples with minimal damage to the endometrial lining (unlike blind D&C).
Endometrial biopsy or aspiration may assist the diagnosis.
Transvaginal ultrasound to evaluate the endometrial thickness in women with
postmenopausal bleeding is increasingly being used to evaluate for endometrial
cancer.
An endometrial thickness exceeding 4 to 5 mm on ultrasound is suggestive of
endometrial pathology in such women.
Sonohysterography:
It may improve delineation of endometrial polyps.
both D&C and Pipelle biopsy curettage give 65-70% positive predictive value. But most
important of these is hysteroscopy which gives 90-95% positive predictive value.
Recently, a new method of testing has been introduced called the TruTest, offered
through Gynecor. It uses the small flexible Tao Brush to brush the entire lining of the
uterus. This method is less painful than a pipelle biopsy and has a larger likelihood of
procuring enough tissue for testing. Since it is simpler and less invasive, the TruTest can
be performed as often, and at the same time as, a routine Pap smear, thus allowing for
early detection and treatment
4
Magnetic resonance imaging (MRI):
It is expensive and not practical to screen all women.
It used for evaluation of endometrial thickness and to predict myometrial invasion.
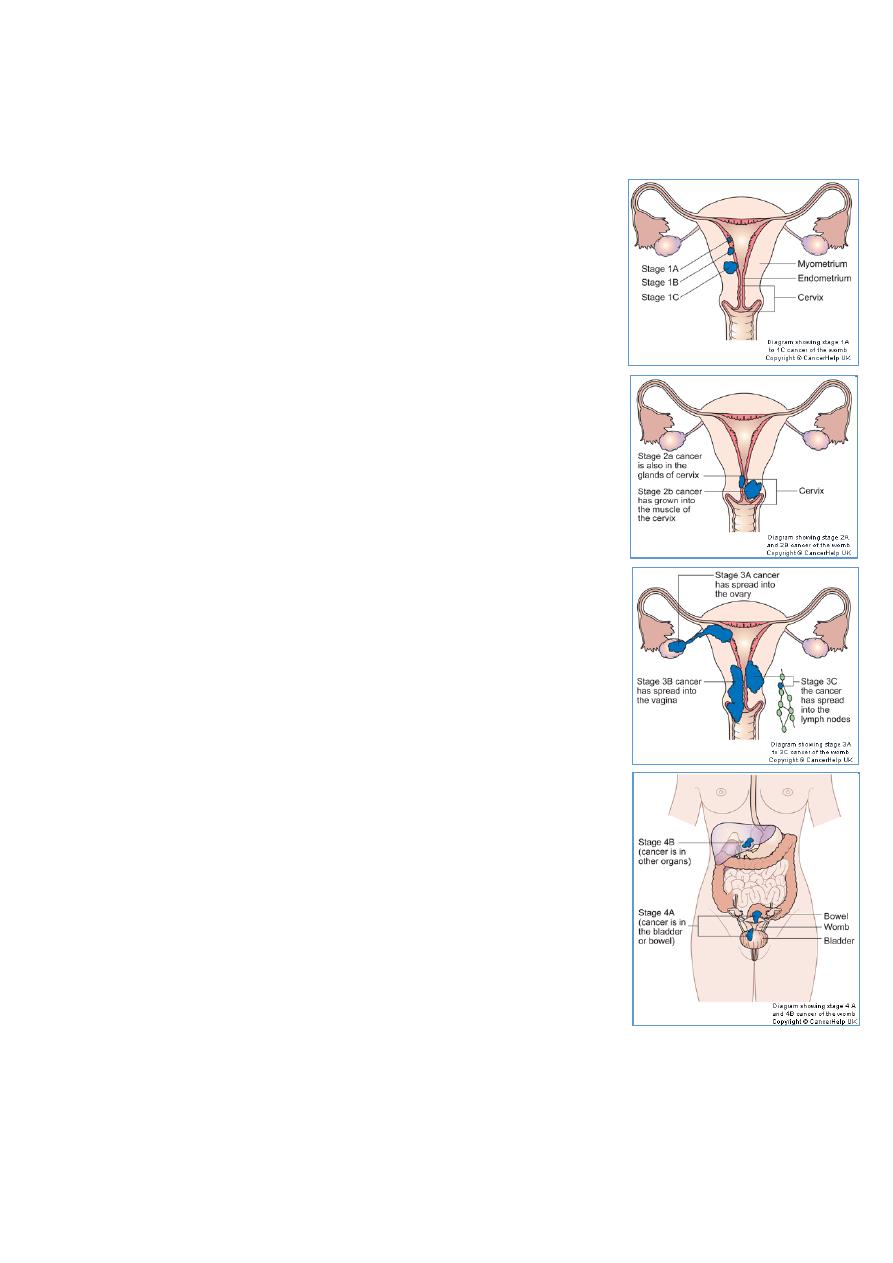
Staging of Endometrial Cancer:
—
I: Confined to uterine corpus
◦ IA: limited to endometrium
◦ IB: invades less than ½ of myometrium
◦ IC: invades more than ½ of myometrium
—
II: invades cervix but not beyond uterus
◦ IIA: endocervical gland involvement only
◦ IIB: cervical stroma involvement
—
III: local and/or regional spread
◦ IIIA: invades serosa/adnexa, or positive cytology
◦ IIIB: vaginal metastasis
◦ IIIC: metastasis to pelvic or para-aortic lymph nodes
—
IVA: invades bladder/bowel mucosa
—
IVB: distant metastasis
Five Year Survival:
—
Stage I: 81-91%
72% diagnosed at this stage
—
Stage II: 71-78%
—
Stage III: 52-60%
—
Stage IV: 14-17%
3% diagnosed at this stage

5
Spread Patterns:
Direct extension
◦ most common
Transtubal
Lymphatic
◦ Pelvic usually first, then para-aortic
Hematogenous
◦ Lung most common
◦ Liver, brain, bone
Treatment:
Stage IB or less: total hyst/BSO/PPALND, cytology
Stage IC to IIB: total hyst/BSO/PPALND, cytology, adjuvant pelvic XRT
Stage III: total hyst/BSO/PPALND, cytology, adjuvant chemotherapy
Stage IV: palliative XRT and chemotherapy
Methods of Endometrial Cancer Treatment:
The treatment of endometrial carcinoma is usually:
* surgical.
* Radiotherapy
* Hormone therapy: Progestogens inhibit the rate of growth and spread of
endometrial carcinoma.
Other Types of Uterine Cancer:
Leiomyosarcoma
o Rapidly growing fibroid should be evaluated
Stromal sarcoma
Carcinosarcoma (MMMT)
Uterine Sarcomas:
Account for fewer than 10% of all corpus cancers.
Types:

6
( Carcinosarcoma, leiomyosarcoma, Endometrial stromal sarcoma, adenosarcoma)
Exposure to radiation may enhance the development of pelvic sarcomas
Abnormal vaginal bleeding most frequent presenting symptom for all histologic types.
No specific staging system (commonly use staging of endometrial carcinoma)
Management of Uterine Sarcomas:
Surgery is the hallmark of treatment with total abdominal hysterectomy and bilateral
salpingo-oopherectomy (TAH/BSO) being the standard procedure.
