1
Third stage
Medicine
Lec-4
د
.
وائل
1/1/2014
Fat soluble vitamins
Vitamin A
Deficiency:
Globally, the most important consequence of vitamin A deficiency is blindness. Each year,
approximately 500 000 new cases of blindness occur in young children, mostly in Asia.
Adults are not usually at risk because liver stores can supply vitamin A when foods
containing vitamin A are unavailable.
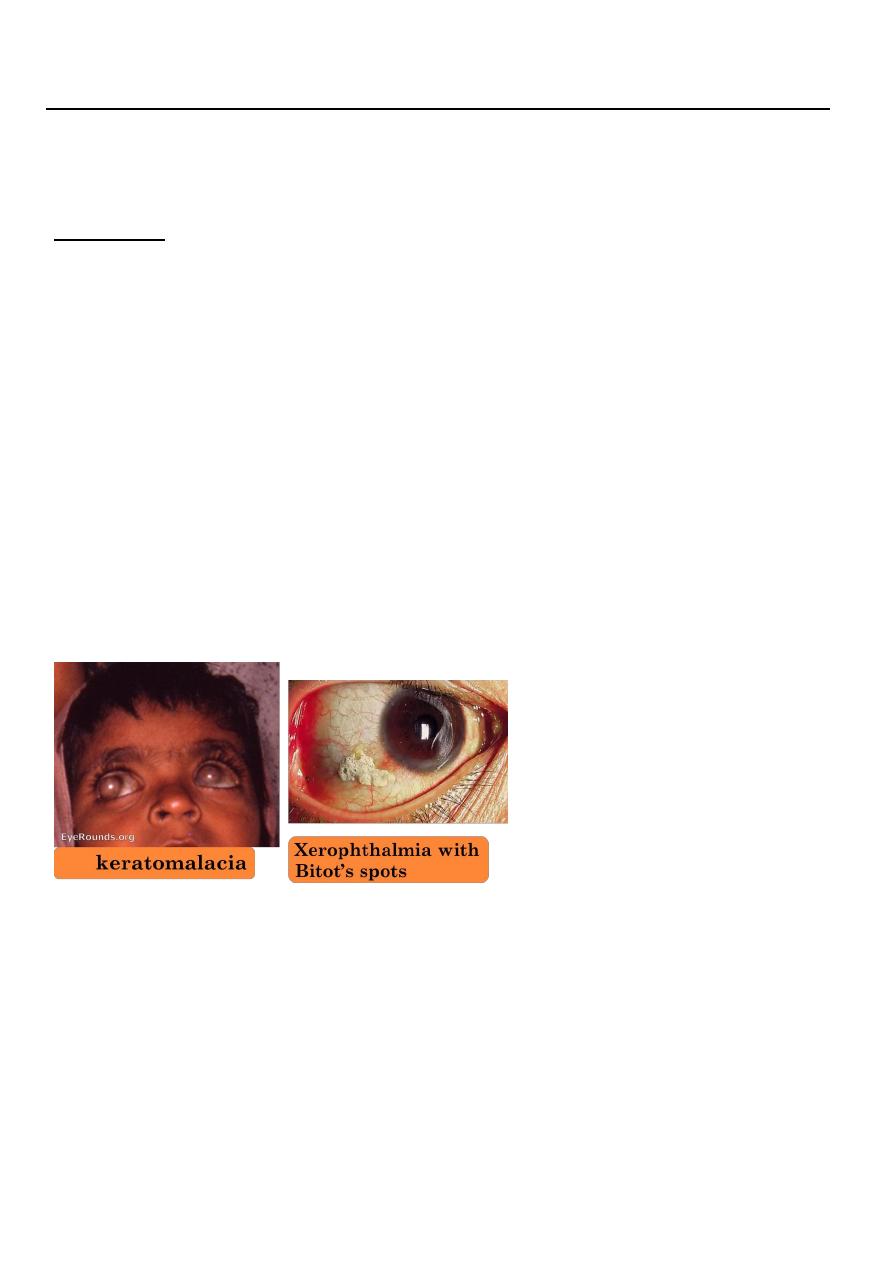
Early deficiency causes impaired adaptation to the dark (night blindness). Keratinisation of
the cornea (xerophthalmia) causes characteristic Bitot's spots, which progresses to
keratomalacia, with corneal ulceration, scarring and irreversible blindness.
In countries where vitamin A deficiency is endemic, pregnant women should be advised to
eat dark green leafy vegetables and yellow fruits (to build up stores of retinol in the fetal
liver), and infants should be fed the same.
WHO is giving high priority to prevention in communities where xerophthalmia occurs, with
single prophylactic oral doses of 60 mg retinyl palmitate (providing 200 000 U retinol) given
to pre-school children. This also reduces mortality from gastroenteritis and respiratory
infections.
Toxicity:
Repeated moderate or high doses of retinol can cause liver damage, hyperostosis and
teratogenicity. Women in countries where deficiency is not endemic are therefore advised
not to take vitamin A supplements in pregnancy. Retinol intake may also be restricted in
those at risk of osteoporosis. Acute overdose leads to nausea and headache, increased
intracranial pressure and skin desquamation. Excessive intake of carotene can cause
pigmentation of the skin (hypercarotenosis); this gradually fades when intake is reduced.

2
Vitamin D:
The most common cause is lack of sunlight exposure since maintenance of normal
levels of vitamin D depends on UV sunlight exposure to catalyse synthesis of
cholecalciferol from 7-dehydrocholesterol in the skin .
Dietary deficiency can also play a role, but vitamin D occurs in only small quantities in
most foods, except oily fish, so the amount present in average diets is insufficient to
meet requirements.
Lack of cholecalciferol results in reduced hepatic production of 25(OH)D3 and thus
reduced renal production of the biologically active metabolite 1,25(OH)2 D3. The lack
of 1,25(OH)2 D3 impairs intestinal calcium absorption and lowers serum calcium,
which stimulates PTH secretion. This causes phosphate wasting and increased bone
resorption in an attempt to maintain serum calcium levels within the normal range,
causing progressive demineralisation of bone.
Clinical features of deficiency:
Vitamin D deficiency in children causes delayed development, muscle hypotonia,
craniotabes (small unossified areas in membranous bones of the skull that yield to
finger pressure with a cracking feeling), bossing of the frontal and parietal bones and
delayed anterior fontanelle closure, enlargement of epiphyses at the lower end of
the radius, and swelling of the rib costochondral junctions ('rickety rosary').
Osteomalacia in adults presents insidiously. Mild osteomalacia can be
asymptomatic or present with fractures and mimic osteoporosis. More severe
osteomalacia presents with muscle and bone pain, general malaise and fragility
fractures. Proximal muscle weakness is prominent and the patient may walk with a
waddling gait and struggle to climb stairs or get out of a chair. There may be bone
and muscle tenderness on pressure and focal bone pain can occur due to fissure
fractures of the ribs and pelvis.
Investigations
The diagnosis can usually be made on a routine biochemical screen with measurement of
serum 25(OH)D and PTH. Typically, serum alkaline phosphatase levels are raised, 25(OH)D
levels are low or undetectable, and PTH is elevated. Serum calcium and phosphate levels
may also be low but normal values do not exclude the diagnosis.
Osteomalacia and rickets respond promptly to treatment with ergocalciferol (250-1000 μg
daily), showing rapid clinical improvement, an elevation in 25(OH)D and a reduction in PTH.
Serum alkaline phosphatase levels sometimes rise initially as mineralisation of bone
increases, but eventually fall to within the normal range as the bone disease heals.
After 3-4 months, treatment can generally be stopped or the dose of vitamin D reduced to a
maintenance level of 10-20 μg cholecalciferol daily, except in patients with underlying
disease such as malabsorption, in whom higher doses may be required.
3
Vitamin D-resistant rickets (VDRR)
This term describes osteomalacia and rickets caused by:
1-Inactivating mutations in the 25-hydroxyvitamin D-1-alpha-hydroxylase (CYP27B1)
enzyme which converts 25(OH)D to the active metabolite 1,25(OH)2 D3 (type I VDRR)
2-Inactivating mutations in the vitamin D receptor which impair its ability to activate
transcription (type II VDRR).
Clinical features are similar to those of infantile rickets and the diagnosis is usually first
suspected when the patient fails to respond to vitamin D supplementation.
Since both are recessive disorders, consanguinity is common but there may or may not be a
positive family history.
Biochemical features of type I disease are similar to vitamin D deficiency, except that levels
of 25(OH)D are normal. In type II disease, 25(OH)D is normal but PTH and 1,25(OH)2D3
values are raised. Type I can be treated with the active vitamin D metabolites, 1-alpha
hydroxyvitamin D (1-2 μg daily orally) or 1,25 dihydroxyvitamin D (0.25-1.5 μg daily orally),
with or without calcium supplements, depending upon the patient's diet. Type II VDRR is
extremely difficult to treat but sometimes responds partially to very high doses of active
vitamin D metabolites and calcium and phosphate supplements
Renal rickets and osteomalacia
Osteomalacia and rickets occur in patients with chronic renal failure due to defects in
synthesis of renal 1,25(OH)
2
D
3
or due to over-aggressive treatment with oral phosphate
binders.
Hypophosphataemic rickets and osteomalacia
Rickets and osteomalacia can occur as the result of inherited or acquired defects in renal
tubular phosphate reabsorption, and rarely in patients with tumours that secrete
phosphaturic substances .
Clinical features and diagnosis
The hereditary disorders usually present in childhood with rickets. The diagnosis is made on
the basis of the early age at onset and presence of hypophosphataemia with renal
phosphate wasting in the absence of vitamin D deficiency. Molecular diagnosis can define
the causal mutation. Tumour-induced hypophosphataemic osteomalacia presents with
severe, rapidly progessive symptoms in patients with no obvious predisposing factor for
osteomalacia. Strenuous efforts should be made to identify the underlying, usually occult
tumour. This often requires whole-body MRI or CT.
Management
Treatment is with phosphate supplements (1-4 g daily) and active metabolites of vitamin D
(1-alpha hydroxyvitamin D 1-2 μg daily or 1,25 dihydroxyvitamin D 0.25-1.5 μg daily) to
promote intestinal calcium and phosphate absorption. The aim is to ameliorate symptoms,
restore normal growth, maintain serum phosphate levels within the normal range and
4
normalise alkaline phosphatase levels. Levels of calcium, phosphate and alkaline
phosphatase, along with renal function, should be monitored.
Tumour-induced osteomalacia can be managed in the same way but surgical excision of the
tumour is curative.
Vitamin E:
Human deficiency is rare and has only been described in premature infants and in
malabsorption. It can cause a mild haemolytic anaemia, ataxia and visual scotomas. Vitamin
E intakes are considered safe up to 3200 mg/day (1000-fold greater than recommended
intakes). Diets rich in vitamin E are consumed in countries with lower rates of coronary
heart disease. However, randomised controlled trials have not demonstrated
cardioprotective effects of vitamin E or other antioxidants.
Vitamin K:
Vitamin K deficiency leads to delayed coagulation and bleeding. In obstructive jaundice,
dietary vitamin K is not absorbed and it is essential to administer the vitamin in parenteral
form before surgery. Warfarin and related anticoagulants act by antagonising vitamin K.
Vitamin K is given routinely to newborn babies to prevent haemorrhagic disease. Symptoms
of excess have been reported only in infants, with synthetic preparations linked to
haemolysis and liver damage.
Water-soluble vitamins
Thiamin (vitamin B1 )
Thiamin is widely distributed in foods of both vegetable and animal origin.
Thiamin pyrophosphate (TPP) is a co-factor for enzyme reactions involved in the
metabolism of macronutrients (carbohydrate, fat and alcohol)
In thiamin deficiency, cells cannot metabolise glucose aerobically to generate energy as
ATP.
Neuronal cells are most vulnerable, since they depend almost exclusively on glucose
for energy requirements.
Impaired glucose oxidation also causes an accumulation of pyruvic and lactic acids,
which produce vasodilatation and increased cardiac output.
Thiamin (vitamin B1 ) Deficiency – beri-beri
In the developed world, thiamin deficiency is mainly encountered in chronic alcoholics.
Poor diet, impaired absorption, storage and phosphorylation of thiamin in the liver,
and the increased requirements for thiamin to metabolise ethanol all contribute.
5
In the developing world, deficiency usually arises as a consequence of a diet based on
polished rice.
The body has very limited stores of thiamin, so deficiency is manifest after only 1 month
on a thiamin-free diet. There are two forms of the:
1. Dry (or neurological) beri-beri manifests with chronic peripheral neuropathy and with
wrist and/or foot drop, and may cause Korsakoff’s psychosis and Wernicke’s
encephalopathy .
2. Wet (or cardiac) beri-beri causes generalised oedema due to biventricular heart failure
with pulmonary congestion.
In dry beri-beri, response to thiamin administration is not uniformly good. However,
multivitamin therapy seems to produce some improvement, suggesting that other
vitamin deficiencies may be involved.
Wernicke’s encephalopathy and wet beri-beri should be treated without delay with
intravenous vitamin B
and C mixture .
Korsakoff’s psychosis is irreversible and does not respond to thiamin treatment.
Riboflavin (vitamin B2 )
Deficiency is rare in developed countries.
It mainly affects the tongue and lips and manifests as glossitis, angular stomatitis and
cheilosis.
The genitals may be affected, as well as the skin areas rich in sebaceous glands, causing
nasolabial or facial dyssebacea.
Rapid recovery usually follows administration of riboflavin 10 mg daily by mouth.
Niacin (vitamin B3 )
Niacin include nicotinic acid and nicotinamide.
Nicotinamide is an essential part of the two pyridine nucleotides, nicotinamide adenine
dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate(NADP), which
play a key role as hydrogen acceptors and donors for many enzymes.
Niacin can be synthesised in the body in limited amounts from the amino acid
tryptophan.
Niacin deficiency: Pellagra
Pellagra was formerly endemic among poor people who depend chiefly on maize,
which contains niacytin, a form of niacin that the body is unable to utilise.
Pellagra can develop in only 8 weeks in individuals eating diets that are very deficient in
niacin and tryptophan.
6
It remains a problem in parts of Africa, and is occasionally seen in alcoholics and in
patients with chronic small intestinal disease in developed countries.
Pellagra can occur in Hartnup’s disease, a genetic disorder characterised by impaired
absorption of several amino acids, including tryptophan.
It is also seen occasionally in carcinoid syndrome when tryptophan is consumed in the
excessive production of 5-hydroxytryptamine (5-HT).
Pellagra has been called the disease of the
three Ds: • Dermatitis. • Diarrhoea. • Dementia.
Treatment is with nicotinamide, given in a dose orally or parenterally.
The response is usually rapid. Within 24 hours, the erythema diminishes, the diarrhoea
ceases and a striking improvement occurs in the patient’s mental state.
Nicotinic acid is a lipid-lowering agent.
Pyridoxine (vitamin B6 )
Pyridoxine, pyridoxal and pyridoxamine are different forms of vitamin B6 that undergo
phosphorylation to produce pyridoxal 5-phosphate (PLP).
PLP is the co-factor for a large number of enzymes involved in the metabolism of
amino acids.
Deficiency is rare, although certain drugs, such as isoniazid and penicillamine, act as
chemical antagonists to pyridoxine.
Pyridoxine administration is effective in isoniazid-induced peripheral neuropathy and
some cases of sideroblastic anaemia.
Large doses of vitamin B6 have an antiemetic effect in radiotherapy-induced nausea.
Although vitamin B6 supplements have become popular in the treatment of nausea in
pregnancy, carpal tunnel syndrome and premenstrual syndrome, there is no convincing
evidence of benefit. polyneuropathy.
Biotin
Biotin is a co-enzyme in the synthesis of fatty acids, isoleucine and valine and is also
involved in gluconeogenesis.
Deficiency results from consuming very large quantities of raw egg whites and It may
also be seen after long periods of total parenteral nutrition.
The clinical features of deficiency include scaly dermatitis, alopecia and paraesthesia.
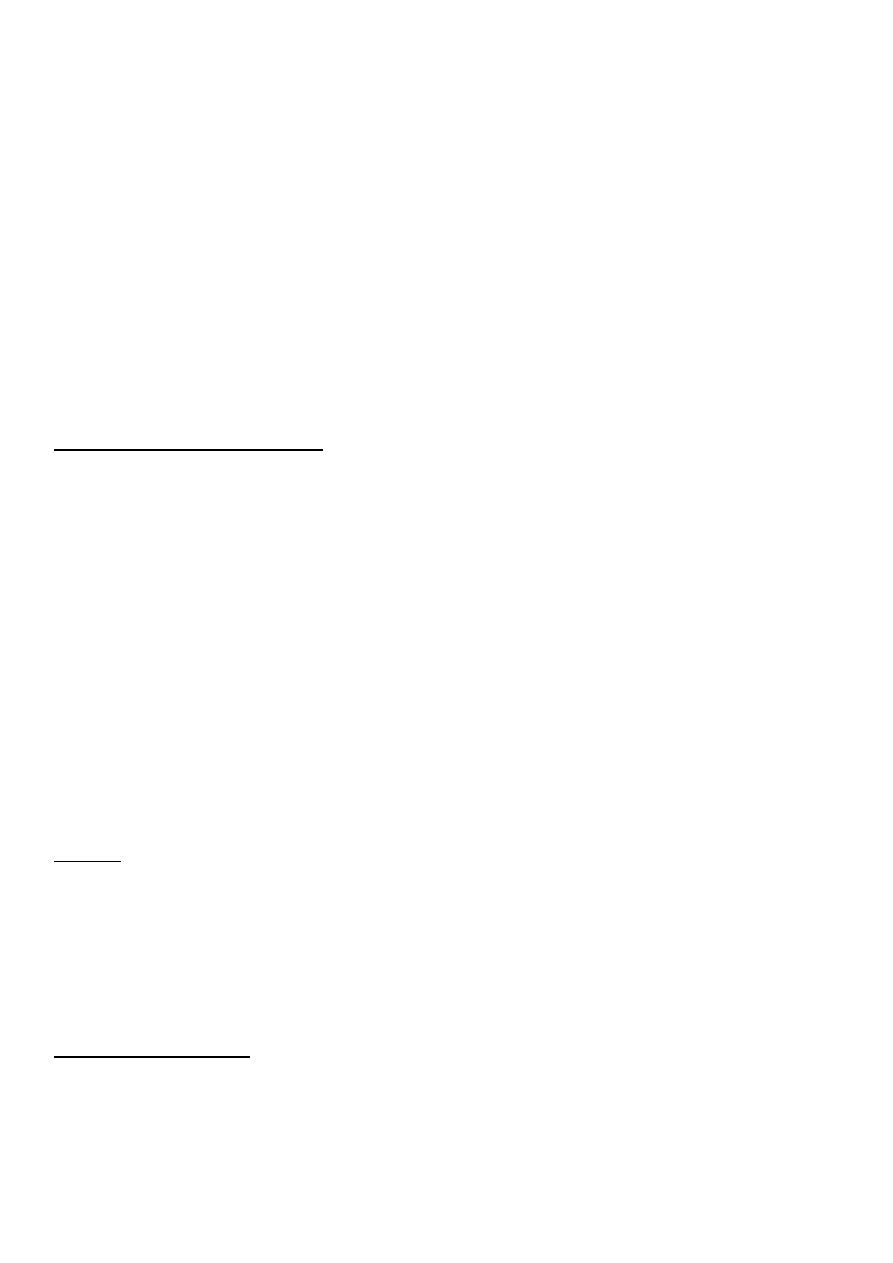
Folate (Folic acid)
Folates exist in many forms. The main circulating form is 5-methyltetrahydrofolate.
Folic acid is the stable synthetic form.
Folate works as a methyl donor for cellular methylation and protein synthesis. It is
directly involved in DNA and RNA synthesis, and requirements increase during
embryonic development.
7
Folate deficiency may cause three major birth defects (spina bifida, anencephaly and
encephalocele).
All women planning a pregnancy are advised to include good sources of folate in their
diet, and to take folate supplements throughout the first trimester.
Folate deficiency has also been associated with heart disease, dementia and cancer.
Hydroxycobolamin(vitamin B12)
Vitamin B12 is a co-factor in folate co-enzyme recycling and nerve myelination. Vitamin
B12 and folate are particularly important in DNA synthesis in red blood cells.
The haematological disorders (macrocytic ormegaloblastic anaemias) due to their
deficiency .
Vitamin B12, but not folate, is needed for the integrity of myelin, so that vitamin B12
deficiency is also associated with neurological disease
Neurological consequences of vitamin B12 deficiency
In older people and chronic alcoholics, vitamin B12 deficiency arises from insufficient
intake and/or from malabsorption.
Several drugs, including neomycin, can render vitamin B12 inactive.
In severe deficiency there is insidious, diffuse and uneven demyelination.
It may be clinically manifest as peripheral neuropathy or spinal cord degeneration
affecting both posterior and lateralcolumns (‘subacute combined degeneration of the
spinalcord), or there may be cerebral manifestations (resembling dementia) or optic
atrophy. Vitamin B12 therapy improves symptoms in most cases.
Vitamin C (ascorbic acid)
Deficiency – scurvy
Vitamin C deficiency causes defective formation of collagen with impaired healing of
wounds, capillary haemorrhage and reduced platelet adhesiveness (normal platelets
are rich in ascorbate).
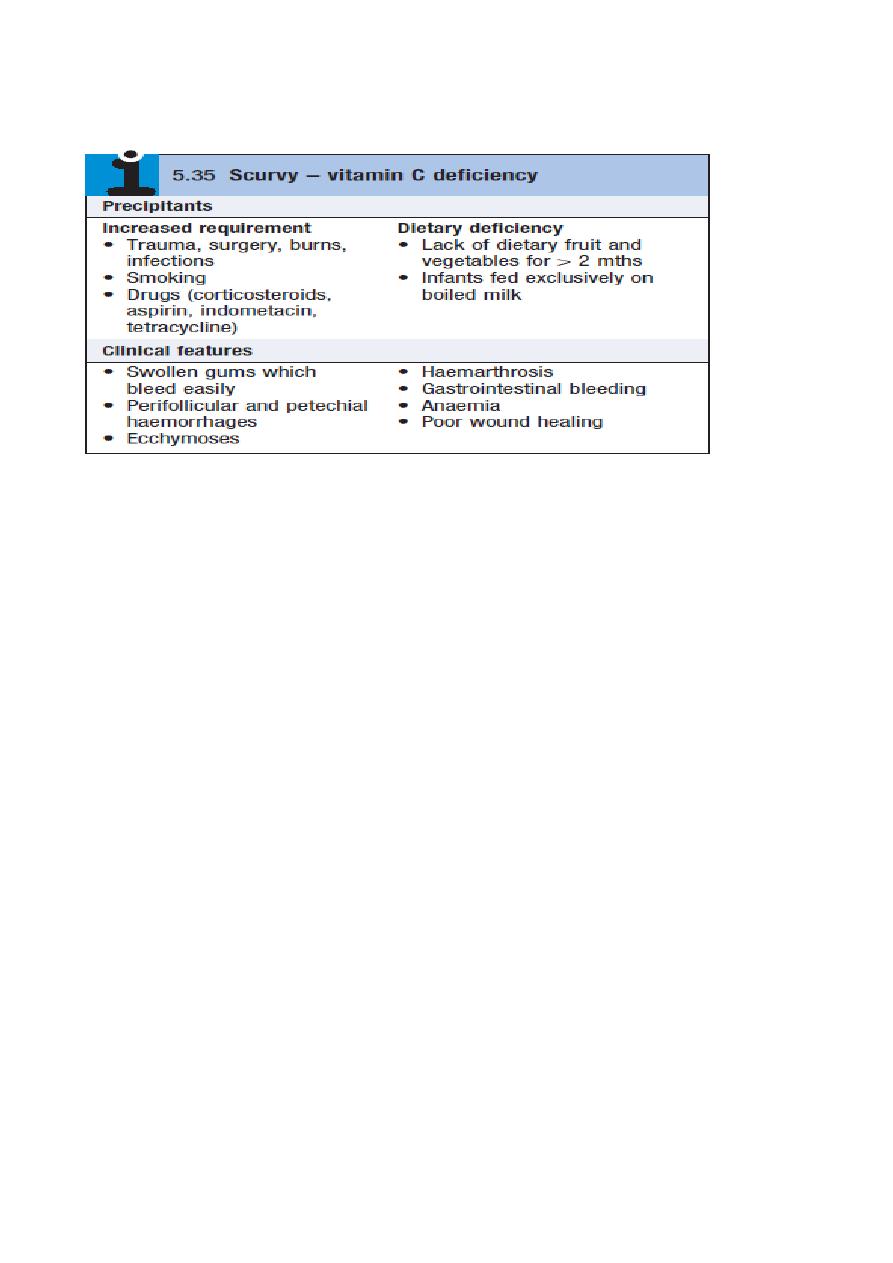
8
A dose of 250 mg vitamin C 3 times daily by mouth should saturate the tissues quickly.
Daily intakes of more than 1 g/day have been reported to cause diarrhoea and the
formation of renal oxalate stones.
