
1
Third stage
Medicine
Lec-3
د
.
زين
العابدين
1/1/2014
Immunosuppressive Therapy
Objectives of the lecture
1. To define what is the immune suppression and immunocompromised status.
2. To know the indications of immunosuppressive agents
3. To study from clinical point of view the different immunosuppressive agents
4. To understand the basis and indications of immunotherapy
Immunosuppressive Therapy
Immunosuppression involves an act that reduces the activation of the immune system.
Deliberately induced immunosuppression is used for:
1. Hypersensitivity disorders
2. Autoimmune diseases
3. Solid organ transplantation including GvHD
Immunocompromised
Immunocompromised individual is the person who is undergoing
- immunosuppression (deliberate)
- or whose immune system is weak for reasons (non-deliberate) such as:
chemotherapy,
radiation,
HIV
lupus.
Types of immunosuppressive drugs/agents
There are several groups of immunosuppressive drugs/agents including:
1. Glucocorticosteroids
2. Antiproliferative drugs
2
3. Calcineurine inhibitors
4. Biological agents
Glucocorticosteroids
Glucocorticosteroid drugs such as cortisone, hydrocortisone, prednisone, and prednisolone
are the most commonly used steroids as an immunosuppressive medication. They have also
potent anti-inflammatory effects.
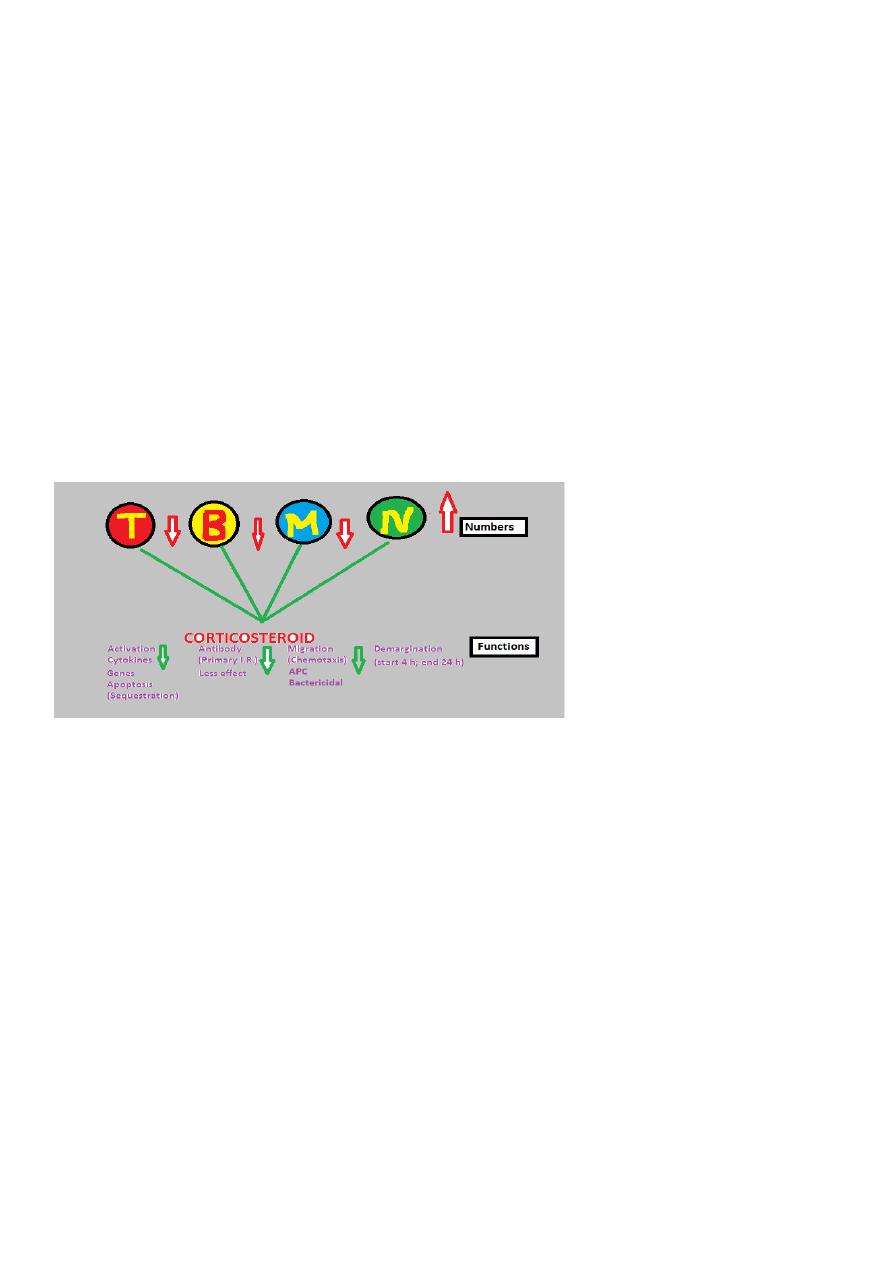
I. The immunosuppressive effects on the immune system are more prominent on the
cellular immunity than on antibody production according to the following mechanisms (See
Figure 1):
Figure 1: Immunosuppressive action of glucocorticosteroid drugs
On T-cells:
Decreased numbers of peripheral blood lymphocytes (lymphopenia) and in lymphoid
tissues in particular CD4 T cells due to apoptosis in the bone marrow (sequestration) and
inhibition of activation and proliferation due to blockade of cytokines production mainly IL-
2 and INF-gamma by interfering with their gene expression.
On Neutrophils:
Increased numbers in the peripheral blood due to interference with their migration
(chemotaxis) to tissues (demargination).
On monocytes/macrophages:
Decreased numbers of monocytes in the blood, and inhibition of the proinflammatory
cytokines production (IL-1, IL-6, and TNF-alpha), antigen presentation, and bactericidal
activity.

3
On B cells: Decrease antibody production in primary immune response and no effect on
memory cells (secondary immune response).
II. The anti-inflammatory effect is through the inhibition of phosphlipase A2 and cyclo-
oxygenase enzymes of arachidonic acid metabolites (inflammatory mediators).
Clinical uses of glucocoticosteroids The clinical uses are mentioned above; with special
attention to allergic diseases, in combination with other immunosuppressive agents to
prevent solid transplants rejection, including bone marrow transplantation to prevent
GvHD, high doses of I.V. methylprednisolone are used to treat acute rejection episodes, and
for treatment of different autoimmune diseases.
Side effects some of which are serious in nature (see Figure 2), so the doses should be
minimized as much as possible and tapered gradually before stop after prolonged use to
avoid adrenal insufficiency.
Antiproliferative drugs (cytotoxic and anti- metabolites)
The anti-proliferative drugs affect the cell division of actively dividing cells including
immune cells and cancer cells. They are used primarily for cancer chemotherapy, but also
useful as immunosuppressive agents. The major side effects of these agents are myelo-
suppression (bone marrow suppression/ leucopenia), infection and hepatotoxicity. The
commonly used agents for immune suppression are:
1. Azathioprine
It is a purine analogue that inhibits purine synthesis consequently blocking DNA synthesis
after it is metabolized in the liver to an active drug form which is 6-mercaptopurine (6MP).
It is used to prevent graft rejection and treatment of many autoimmune diseases.
4
2. Mycophenolate mofitil (MMF
It is also a purine analogue which has a similar action to azathioprine but more powerful
with less myelotoxicity.
3. Cyclophosphamide
It is an alkylating agent that inhibits DNA synthesis. It is used in the treatment of many
autoimmune diseases such as SLE and vasculitis (e.g. Wegener’s granulomatosis). It may
cause haemorrhagic cystitis.
4. Methotrexate (MTX)
It is a folic acid antagonist and blocks both DNA and RNA synthesis. It is commonly used in
the treatment of rheumatoid arthritis and sometimes in the treatment of psoriasis.
Calcineurin inhibitors & proliferation signal inhibitors
Calcineurin inhibitor (Cyclosporin and Tacrolimus) inhibit IL-2 production that leads to
inhibition of T lymphocytes activation and proliferation.
1. Cyclosporine: It is a fungal derived peptide which is used to prevent graft rejection. Its
main side effects are increased susceptibility to infections, nephrotoxicity (problem ),
hypertension, hirsutism and gingival hypertrophy (Figure 4).
2. Tacrolimus: It is more potent than cyclosporine, but is diabetogenic and less likely to
cause hirsutism (hypertrichosis).
Proliferation signal inhibitors (Sirolimus) Sirolimus acts on T-cells at the level of post-
activation events in the nucleus. Its major advantage over calcineurin inhibitors is that it is
not nephrotoxic.
Biological agents
These agents (mainly polyclonal or chimeric/ monoclonal antibodies) target antigens on the
lymphocytes or cytokines and cytokine receptors.
1. Polyclonal antibodies: Antithymocyte globulin (ATG) is a horse antibody that can deplete
the long-lived peripheral T lymphocytes. It is used in the treatment of acute rejection
episodes and GvHD in combination with other immunosuppressive agents. As well as in the
treatment of aplastic anaemia. The main side effects are serum sickness-like reaction.
2. Chimeric/ monoclonal antibodies (MAb): The most important examples are (see Figure 3
about rheumatoid arthritis as a clinical example):
Anti-TNF-alpha blockers: MAb: Infliximab (Remicade), adalimumab, and certolizumab; OR
circulating receptor fusion protein: Etanercept (Enbrel); for RA, Crohn’s disease

5
Anti-CD80/CD28 (costimulatory pair): Abatacept; for RA
Anti-IL-1: Anakinra; for RA
Anti-IL-6: Tocilizumab; for RA
Anti-IL-2/receptor (CD25): Basilizumab, Daclizumab; for prevention of acute transplant
rejection
Anti-B cells (CD20): Rituximab; for NHL, RA, multiple sclerosis
Anti-CD3: Muromonab; for graft rejection
Anti-IgE: Omalizumab; for asthma
Anti-CD11a (LFA-1/ICAM-1): Efalizumab; for Psoriasis
Immunotherapy
Immunotherapy is a new term used instead hypo/desensitization. Its mechanism of action
is poorly understood, but the following mechanisms could explain it:
1. Induction the formation of IgG blocking antibodies in the extracellular fluid that can catch
the allergens before reaching the basophiles/mast cells.
2. Induction of some changes in the T-cell regulatory mechanism
3. Induction of tolerance (state of a specific unresponsiveness)
The immunotherapy is done by:
Subcutaneous injections of the sensitizing allergen once or twice weekly in increasing
doses pattern, until a maintenance dose is reached based on the clinical improvement
showed by the patient.
6
Indications for immunotherapy
1. Severe allergic rhinitis poorly responding to drug therapy and in whom allergen
avoidance is not possible
2. Allergic asthma not responding to drug therapy; this rather less certain indication for
immunotherapy
3. IgE-mediated allergy to drugs such as penicillin, or insulin. A short course of
immunotherapy can be prescribed.
4. Anaphylaxis to insect venom; it is an effective therapy to prevent the development of
systemic anaphylaxis to insect venom (e.g. bees, wasp).
Summary of the lecture
1. Immunosuppression reduces the activation of the immune system;
Immunocompromised whose immune system is weak
2. Groups of immunosuppressive agents are: Glucocorticosteroids, Antiproliferative drugs,
Calcineurine inhibitors, and Biological agents
3. Glucocorticosteroids: Act on T-, B- Macrophages, and Neutrophils
4. Antiproliferative drugs: affect the cell division of actively dividing cells
5. Calcineurin inhibitors: affect IL-2 production that leads to inhibition of T lymphocytes
6. Biological agents: (polyclonal or chimeric/ monoclonal antibodies) target antigens on the
lymphocytes or cytokines and cytokine receptors. A clinical application is given about
rheumatoid arthritis
7. Immunotherapy induces the formation of IgG blocking antibodies , changes in the T-cell
regulatory mechanism , and tolerance. It is indicated for management of severe allergic
rhinitis, allergic asthma, IgE-mediated allergy to drugs, and anaphylaxis to insect venom
