
1
Third stage
Medicine
Lec-6
د
.
اسماعيل
1/1/2014
CRIMEAN-CONGO HAEMORRHAGIC FEVER (CCHF)
INTRODUCTION:
Haemorrhagic fever cover a wide field in medicine (infectious and
non infectious) that cause fever associated with fever. The term viral haemorrhagic fever is
restricted to some groups of RNA viruses in which the fever is associated with significant
bleeding tendency in addition to the other features. These groups and diseases caused by
them is shown in the table below.
Crimean-Congo haemorrhagic fever: Is the only type of viral haemorrhagic fever that was
present in Iraq (the early cases were reported in late seventies and subsequent cases were
reported in eighties and early nineties of last century, then disappeared till now), but
awareness of the presence of such a disease here and there in our country is still important.
HISTORY:
هذا المقطع لالطالع فق
ط
During the summers of 1944 and 1945 over 200 cases of a severe, acute, febrile illness with
marked hemorrhagic manifestations occurred in the USSR in the Western Crimea. Many of
the cases were among troops of the Soviet Union. Virus was isolated from blood samples of
patients with acute disease and from the tick Hyalomma. It was later realized that a similar
disease had been known for many years in other areas of the USSR, particularly Central Asian
republics, and the same syndrome has since been described in areas bordering the Black and
Caspian Seas and Bulgaria and former Yugoslavia. In 1969, it was shown that the virus
causing CCHF was identical to the virus named Congo which had been isolated in 1956 from
the blood of a febrile child in Zaire. This virus is widely spread in East and West Africa. More
recently, CCHF or antibody to it, has been shown to have appeared in Dubai, Iraq, South
Africa, Pakistan, Greece, Turkey, Albania, Afghanistan, and India. Geographical variation in
virulence has been observed, for example, the disease in Africa, where haemorrhagic
phenomena and deaths are only rarely reported, does not seem to be as virulent as in Asia.
Probably because CCIHF is associated with severe haemorrhagic features, secondary cases
are relatively common. In an outbreak in Saudi Arabia, one case resuscitated in an accident
and emergency unit gave rise to seven secondary cases. In 1967, five laboratory-acquired
cases were recognized. Hospital-associated outbreaks were described in Pakistan in 1976 and
in Dubai in 1980. In November 1996, 15 cases of CCHF were confirmed in South Africa. All of
the patients worked in the slaughtering unit of the same ostrich farm. Ostriches, like other
birds, are thought to be fairly resistant to infection with CCHF, but they undoubtedly suffer
heavy burdens of Hyalomma spp., which could be vectors of the disease.
VIROLOGY
• Name: CCHF VIRUS
• Genus: Nairovirus
• Family: Bunya virus (bunyaviridae)
• Type: RNA virus
• Vector: Tick
• Zoonosis: Transmitted from animals to human being.

2
CCHF RESERVOIRS AND VECTORS
The CCHF virus may infect a wide range of domestic and wild animals. Many birds are
resistant to infection, but ostriches are susceptible and may show a high prevalence of
infection in endemic areas. Animals become infected with CCHF from the bite of
infected ticks.
A number of tick genera are capable of becoming infected with CCHF virus, but the most
efficient and common vectors for CCHF appear to be members of the Hyalomma genus.
Trans-ovarial (transmission of the virus from infected female ticks to offspring via eggs) and
venereal transmission have been demonstrated amongst some vector species, indicating one
mechanism which may contribute to maintaining the circulation of the virus in nature.
Once infected, the tick remains infected through its developmental stages, and the
mature tick may transmit the infection to large vertebrates, such as livestock. Domestic
ruminant animals, such as cattle, sheep and goats, are viraemic (virus circulating in the
bloodstream) for around one week after becoming infected.
The animals develop (little or no symptoms).
TRANSMISSION:
Humans who become infected with CCHF acquire the virus from
direct contact with blood or other infected tissues from livestock during this time, or
they may become infected from a tick bite. The majority of cases have occurred in those
involved with the livestock industry, such as agricultural workers, slaughterhouse
workers, butchers and veterinarians.
CLINICAL MANIFESTATION
1. The incubation period is about 2 - 7 days, and has not been recorded as longer than 12
days. The disease is more common in adult and older children than the small children (more
exposure to the source in adult). The disease is fatal during pregnancy. It occurs mainly
during hot seasons starting in late spring, summer, and early autum, and rare during cold
seasons like winter. This is because the life cycle of tick and the virus life cycle in tick are
affected by temperature variation.
2. Prodromal stage: Illness begins abruptly with
• High fever,
• Myalgia,
• Headache,
• Vomiting
• Pain in the epigastrium, lower back and thighs.
• Loose stools, dry cough, tachycardia, although relative bradycardia may be present.
3. Haemorrhagic manifestation: Some patients recover quite suddenly after seven or eight
days, but up to 75% begin to show haemorrhagic features after 3 - 5 days.
• Petechial rashs often appears in the mucous members and skin
• Ecchymosis ( blue and black patches) in skin
• Haematemesis and melaena
• Epistaxis
• Conjunctival injection and haemorrhages
• Haematuria.
Despite high viraemia, there is often a marked neutrophilia.
4. Other features and complications:

3
• The liver is enlarged and tender, liver and tissue transaminases are elevated and
• disseminated intravascular coagulation (DIC) may follow.
• Death may occur (30 -50% of cases) on the seventh to ninth day, following a period of
shock, oliguria and, sometimes, respiratory distress syndrome.
• Leucopenia and thrombocytopenia
5. Convalescence: The patient may recover gradually, starting on day 10 onwards. The skin
rashes (petechia and ecchymosis) fade, bleeding stops and fever subsides. The recovery is
usually complete, although some describe a type of neuritis and asthenia which may remain
for some time. The patient is usually less infectious and even in late days of this stage is non
infectious, and his serum can be used for prophylaxis (passive immunity) for contacts in
future. The immunity is permanent for all strains of CCHF viruses. The patient remains in
hospital for an average of 20 days.
Causes of bleeding in CCHF
1. Generalized capillary damage is the major cause.
2. Rarely DIC may occur in severe conditions, late in the disease; may play a role as
indicated by prolonged PT, PTT and increase in fibrin degradation products (FDP).
3. Thrombocytopenia is usually mild and usually not plays an important role in bleeding.
Causes of shock in CCHF
1. Bleeding is the major cause
2. Dehydration due to vomiting and diarrhea
3. Occasionally immunological causes (Ag-Ab complex) leading to release of mediators.
Causes of death in CCHF
1. Shock is the most important cause
2. Multiple organ failure
3. Renal failure
4. Secondary bacterial infection
5. Intra cranial haemorrhage
6. Respiratory distress syndrome
CONFIRMING THE DIAGNOSIS:
Early diagnosis is possible using
1. Antigen detection by immunofluorescence techniques. Some laboratories use reverse
transcriptase PCR methods.
2. Antibody detection: by using immunofluorescence test and ELIZA test
IgM antibodies are often detectable after the first five to seven days of fever, but their
concentration diminishes significantly after about 10 days, and is replaced by rising IgG
levels.
3.The virus is readily cultured in commonly-available cell lines such as monkey kidney
cells.

4
MANAGEMENT
1. SPECIFIC TREATMENT
There is evidence that CCHF responds to treatment with ribavirin amelioration of fever and
lessening or avoidance of haemorrhagic features. The use of ribavirin is complicated in these
patients by its tendency to cause significant anaemia, mainly due to haemolysis. (also can
be given to contacts)
2. INTENSIVE SUPPORTIVE MANAGEMENT
is required at an early stage and sometimes for prolonged periods by cases of CCHF. The
intensive Supportive management includes:
1. Correction of dehydration, electrolytes, and blood transfusion.
2. Monitoring of the patient and follow up chart.
3. Treatment of DIC.
4. Routine steroid and antibiotics are not indicated.
5. Management of other complications if present.
3. OTHER MEASURES AND PROTECTING AGAINST HOSPITAL – ACQUIRED CASES
1. Isolation of the patient in a single room in hospital
2. Decrease the number visitors and medical personnel to the patient
3. Provision of adequate disposable equipment and protection clothing.
4. Notification of the disease to health authorities within 24 hours.
5. Good staff training and supervision
6. Regular observation of all contacts for any symptom; samples of blood may be taken
from them for serology.
6. Send samples of blood for serological, CBC, blood group and Rh; Labeling them as a
“Highly infectious samples” to avoid Lab. Personnel’s contamination.
7. Bone marrow examination may be needed sometimes to exclude blood diseases like
leukaemia.
8. A vaccine is not available for CCHF at time being.
DECONTAMINATION: The virus is killed by common disinfectants, solvents, and dry heat
(56°C, 30 min.). The vectors (ticks of the genus Hyalomma) also need to be controlled with
acaricides and possible animal reservoirs will need to be monitored.
DIFFERENTIAL DIAGNOSIS:
هذا
المقطع
لالطالع
فقط
1. Other non infectious diseases or conditions that need to be eliminated like
leukaemia, and aplastic anaemia.
2. Other infectious diseases that may be associated with haemorrhagic
manifestations like:
• Leptospirosis (spirochaetal disease)
• Listeriosis Bacterial infections
• Meningococcal septicaemia
• Q fever
5
• Other viral hemorrhagic fevers: Usually these are not present in our country but may
be present in other countries. These are also caused by RNA viruses (look to the table
below) and include:
– Argentinian hemorrhagic fever
– Bolivian hemorrhagic fever
– Dengue fever
– Ebola hemorrhagic fever
– Hemorrhagic fever with renal syndrome
– Lassa fever
– Marburg fever
– Rift valley fever
– Yellow fever
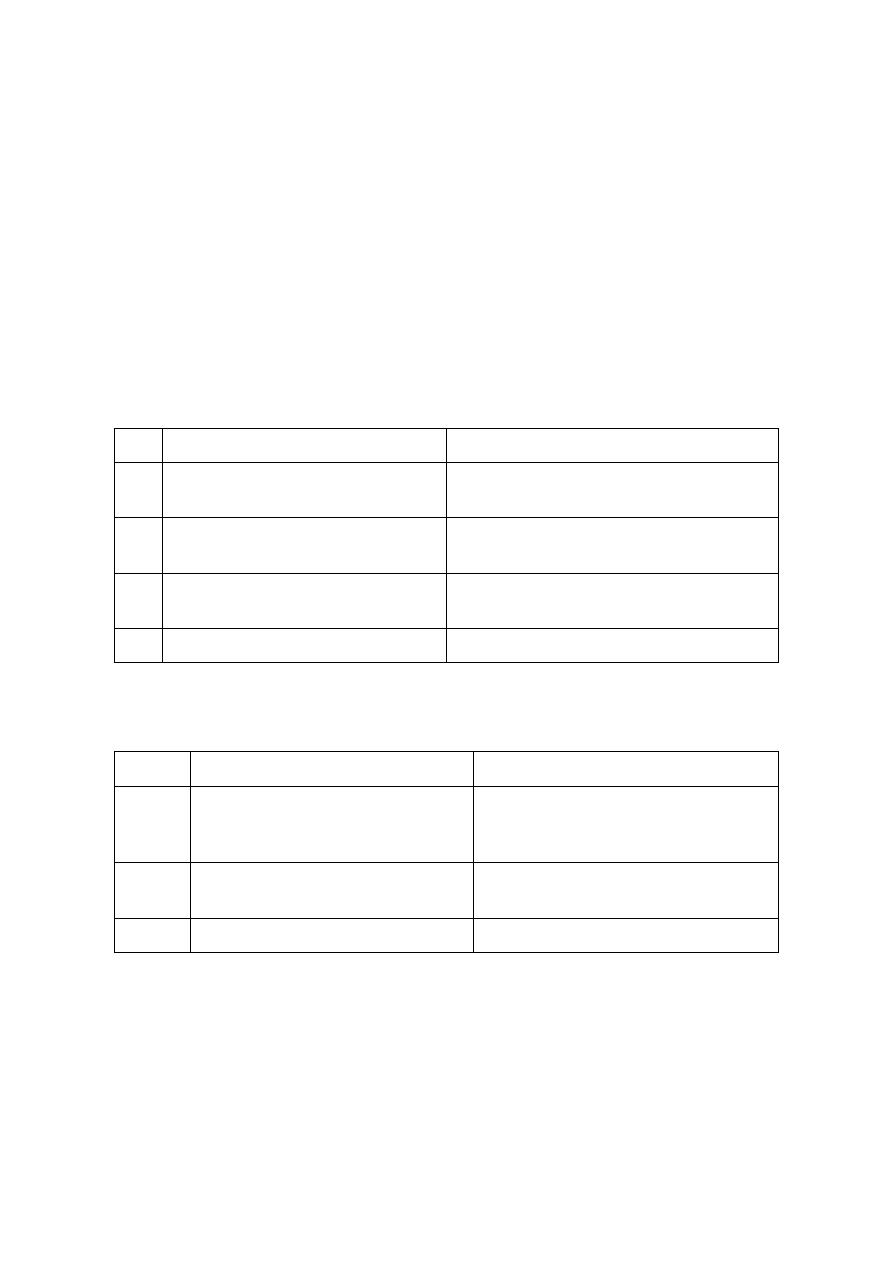
Table 1: Shows different groups of RNA viruses that cause haemorrhagic fever:
هذه
الجداول
ل
الطالع
فقط
No
Viral group
Examples of the diseases
1
Flaviviridae
Yellow fever, dengue fever, Omask
HF, Kyasanar HF
2
Bunyaviridae
Crimean-Congo HF, HF with renal
syndrome, rift valley HF
3
Arenaviridae
Lassa fever, Argentinean and Bolivian
HF
4
Filoviridae
Murburge-Ebola HF
Table 2: Shows vector groups that are responsible for disease transmission in different types
of viral haemohhagic fever:
No
Vectors
Examples of Diseases
1
ARBO (Arthropod born)
Mosquito (Yellow fever, Dengue
fever,and Rift-valley fever). Tick
(CCHF, Omask HF, Kyassar HF)
2
ROBA (Rodent born)
HF with renal syndrome, like
Argentina and Bolivian HF
3
Unknown vector
Murburge- Ebola Hf
تعليمات
دفن
الموتى
بمرض
الحمى
النزفية
( :
لالطالع
فقط
)
لغرض
منع
انتشار
الوباء
لالخرين
من
المستحسن
اجراء
ما
يلي
عند
الدفن
:
1.
ان
يكون
القبر
بعمق
مناسب
(
2
م
او
اكثر
)
2.
ان
توضع
الجثة
في
تابوت
محكم
المنافذ
ويستحسن
ان
يكون
مصنوعا
من
حديد
3.
ان
ترش
على
الجثة
مادة
معقمة
وقاتلة
للمكروبات
4.
من
االفضل
عدم
السماح
بنقل
الجثة
من
مكان
الى
اخر
(
من
مدينة
الى
اخرى
)
اال
بعد
مرور
فترة
زمنية
مناتسبة
5.
ان
تدفن
الجثة
تحت
اشراف
السلطات
الصحية
6.
تحرق
الشراشف
والمالبس
المستخدمة
من
قبل
المريض
في
المستشفى
