1
Third stage
Medicine
Lec-5
د
.
اسماعيل
1/1/2014
Amoebiasis
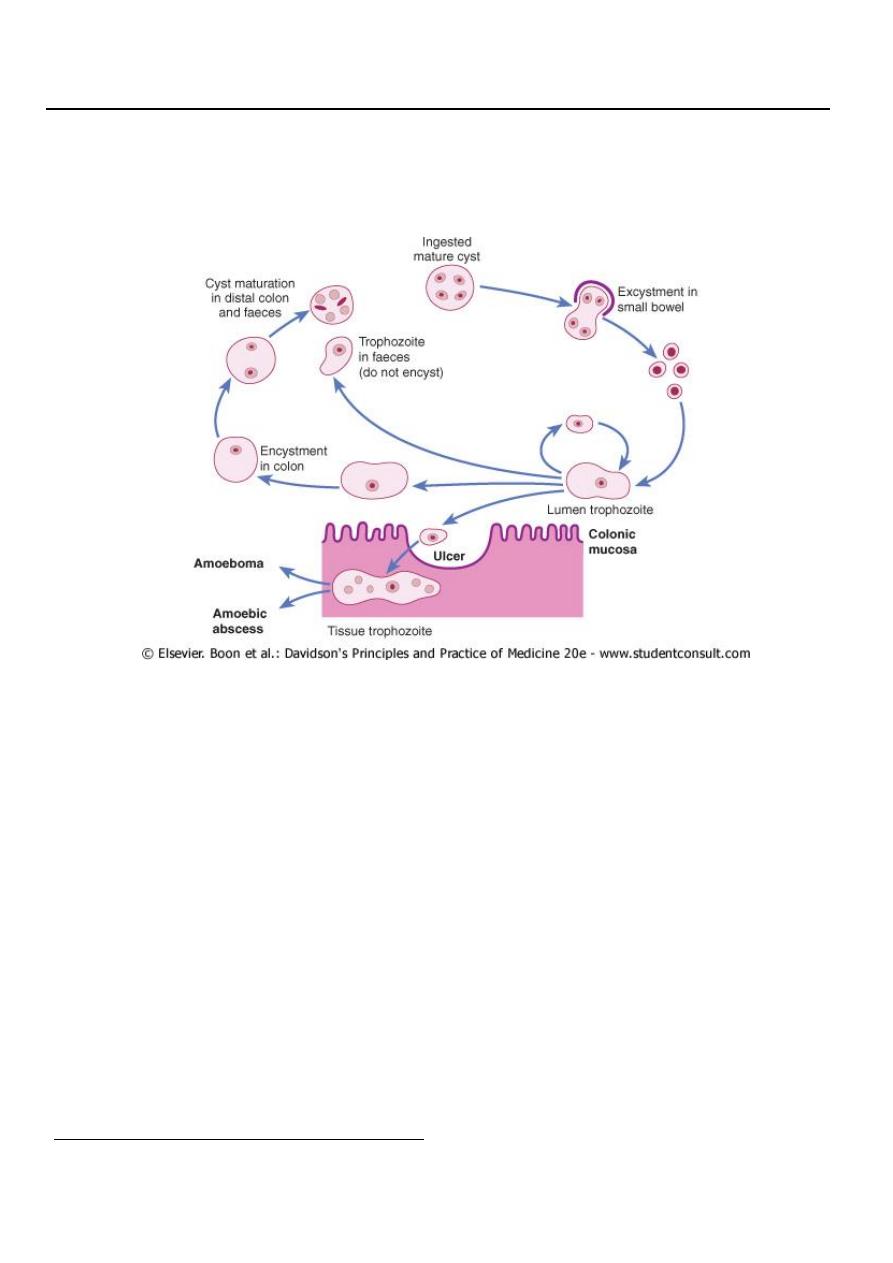
Amoebiasis is caused by Entamoeba histolytica, which is spread between humans by its
cysts. It is common throughout the tropics. E. histolytica can give rise to amoebic dysentery
or extraintestinal amoebiasis, e.g. amoebic liver abscess through invasion by trophozoit.
Pathology:
Cysts of E. histolytica are ingested in water or uncooked food contaminated by human
faeces. Vegetables are a common vehicle of infection.
In the colon vegetative trophozoite forms emerge from the cysts and may invade the
mucous membrane of the large bowel, producing lesions that are maximal in the caecum
but found as far down as the anal canal. These are flask-shaped ulcers varying greatly in size
and surrounded by healthy mucosa. A localised granuloma (amoeboma), presenting as a
palpable mass in the rectum or a filling defect in the colon on radiography, is a rare
complication. This responds well to anti-amoebic treatment so should be differentiated
from colonic carcinoma.
Clinical features:
Intestinal amoebiasis or amoebic dysentery The incubation period of amoebiasis ranges
from 2 weeks to many years, followed by a chronic course with abdominal pains and two or
more unformed stools a day. Diarrhoea alternating with constipation is common, as is
2
mucus, sometimes with streaks of blood; the stools often have an offensive odour. There
may be tenderness along the line of the colon, especially over the caecum (which may
simulate acute appendicitis) and pelvic colon. Acute bowel symptoms, with very frequent
motions and the passage of much blood and mucus, simulating bacillary dysentery or
ulcerative colitis, occur particularly in older people, in the puerperium and with superadded
pyogenic infection of the ulcers.
Diagnosis:
Any exudate should be examined at once under the microscope for motile trophozoites
containing red blood cells. Movements cease rapidly as the stool preparation cools.
Sigmoidoscopy may reveal typical flask-shaped ulcers, which should be scraped and
examined immediately for E. histolytica. Several stools may need to be examined in chronic
amoebiasis before cysts are found. In endemic areas one-third of the population are
symptomless passers of amoebic cysts.
Antibodies are detectable by immunofluorescence in over 95% of patients with hepatic
amoebiasis and intestinal amoeboma but in only about 60% of dysenteric amoebiasis
Treatment and Prevention:
Intestinal amoebiasis responds quickly to oral metronidazole (800 mg 8-hourly for 5 days)
or tinidazole (2 g daily for 3 days). Diloxanide furoate 500 mg should be given orally 8-
hourly for 10 days after treatment to eliminate luminal cysts.
Prevention Personal precautions against contracting amoebiasis consist of not eating fresh
uncooked vegetables or drinking unboiled water.
AMOEBIC LIVER ABSCESS:
This often occurs without a history of recent diarrhoea.
Amoebic trophozoites emerge from the vegetative cyst form in the colon and may invade
the bowel mucosa. They may enter a portal venous radicle and be carried to the liver where
they multiply rapidly and destroy the parenchyma, causing an amoebic abscess. The liquid
contents at first have a characteristic pinkish colour which may later change to chocolate
brown.
Clinical features The abscess is usually found in the right hepatic lobe. Early symptoms may
be local discomfort only and malaise; later, a swinging temperature and sweating may
develop. An enlarged, tender liver, cough and pain in the right shoulder are characteristic,
but symptoms may remain vague and signs minimal . The absence of toxicity in the
presence of a high swinging fever is noticeable. The less common abscess in the left lobe is
difficult to diagnose. There is usually neutrophil leucocytosis and a raised diaphragm, with
diminished movement on the right side. A large abscess may penetrate the diaphragm and
rupture into the lung, from where its contents may be coughed up. Rupture into the pleural
cavity, the peritoneal cavity or pericardial sac is less common but more serious.
3
Investigations An amoebic abscess of the liver is suspected from the clinical and
radiographic appearances and confirmed by ultrasonic scanning. Aspirated pus from an
amoebic abscess has the characteristic appearance described above but only rarely
contains free amoebae. Antibodies are detectable by immunofluorescence in over 95% of
patients with hepatic amoebiasis
Management
Early hepatic amoebiasis responds promptly to treatment with metronidazole (800 mg 8-
hourly for 5 days) or tinidazole (2 g daily for 3 days) as above. The luminal amoebicide
diloxanide furoate (500 mg 8-hourly for 10 days) is given to eliminate the intestinal
infection. If the abscess is large or threatens to burst, or if the response to chemotherapy is
not prompt, aspiration is required and repeated if necessary. Rupture of an abscess into the
pleural cavity, pericardial sac or peritoneal cavity necessitates immediate aspiration or
surgical drainage. Small serous effusions resolve without drainage.
GIARDIASIS
Infection with Giardia intestinalis, also known as G. lamblia, is found world-wide and is
common in the tropics. It particularly affects children, tourists and immunosuppressed
individuals. The cysts remain viable in water for up to 3 months and infection usually occurs
by ingesting contaminated water. The parasites attach to the duodenal and jejunal mucosa,
causing inflammation.
Clinical features
After an incubation period of 1-3 weeks, there is diarrhoea, abdominal pain, weakness,
anorexia, nausea and vomiting. On examination there may be abdominal distension and
tenderness. Stools obtained at 2-3-day intervals should be examined for cysts. Duodenal or
jejunal fluid gives a higher diagnostic yield. Thus if endoscopy is being performed, giardiasis
should be considered and juice aspirated for microscopic examination. On jejunal biopsy
fresh mucus examination may show Giardia on the epithelial surface.
Management
Treatment is with a single dose of tinidazole 2 g, or metronidazole 2 g once daily for 3 days
or 400 mg 8-hourly for 10 days.
