
1
Third stage
Surgery
Lec-1
د
.نشوان
1/1/2016
Trauma
Trauma: Is cellular disruption caused by environmental energy that is beyond the body's
resilience.
Injury: Is the adverse effect of a physical force upon a person.
Trauma could be: accidents, self harm (suicide), assault (homicide), legal intervention, war,
and undetermined causes.
THE SCALE OF THE PROBLEM
Trauma is the leading cause of death and disability in the first four decades of life and
is the third most common cause of death overall.
It is estimated that more than 10 per cent of people will die from trauma.
Trauma is recognised as a serious public health problem
It cause:
1- Death
2- long term disability and profound change in lifestyle
3- costly medical expenses
4- It affects everyone who is involved in the injured person’s life.
Causes of injury
1-Mechanical trauma could be blunt, penetrating, or crush injury
Blunt like motor vehicle accident (MVA), motorcycle, fall from height, fight.
Penetrating injury like stab wound, bullet and blast .
Crush injury like industrial injury
2-Thermal injury like burn
3-Chemical
4-Radiation
5-Psycological
2
Trimodal distribution of death:
1- Immediate, 50 per cent of all deaths.
These are probably not possible to save.
They are usually the result of massive head injury or severe cardio-pulmonary insult.
2- Early, 30% within the first few hours. These will result from a failure of oxygenation of
tissue either because airway or breathing problem, or because the circulation filure.
3- Late, 20% of deaths. Usually from multiple organ failure and sepsis, influenced by
inadequate early resuscitation and care.
ATLS:
The steps in the Advanced Trauma Life Support (ATLS) philosophy
1-Primary survey with simultaneous resuscitation: identify and treat what is killing the
patient.
2- Secondary survey: proceed to identify all other injuries and treat them.
3-Definitive care: develop a definitive management plan and follow up
Primary survey
ABCDE of trauma care
A, Airway with cervical spine protection
B, Breathing and ventilation
C, Circulation with hemorrhage control
D, Disability: neurological status assessment.
E, Exposure: completely undress the patient and assess for other injuries.
PRIMARY SURVEY AND RESUSCITATION
1--Airway with cervical spine protection
In alert patient. Ensuring a patent airway may require simple measures, such as clearing
the mouth and suction, or maneuvers such as a jaw thrust or chin lift, nasopharyngeal or
Guedel airway may be used, provided that the patient will tolerate it.
In case of severe head trauma, where the patient is unconscious, with apnea and inability
to maintain oxygenation, then a definitive airway may be required (such as
cricothyroidotomy, endotracheal intubation or tracheostomy).
3
Patients in dangerous of air way obstruction:
1- Penetrating injuries to the neck with expanding hematoma.
2- Evidence of chemical or thermal injury to the mouth, nares, or hypo pharynx.
3- Extensive subcutaneous air in the neck.
4- Complex maxillofacial trauma.
5- Airway bleeding.
6- Patients who have an abnormal voice.
7- Abnormal breathing sounds.
8- Tachypnea
9- Altered mental status
Every patient who has had significant trauma (especially to the head) has a cervical spine
injury until proven otherwise.
Therefore, throughout the initial assessment, the cervical spine must be immobilized. This
is either performed manually, or with the traditional collar, sandbags and tape.
Life-saving surgery may need to be performed prior to transfer for other injuries.
This is called ‘damage control surgery
2--Breathing and ventilation
Oxygen should be administered to all trauma patients, using a high concentration mask
with a reservoir.
A check should be made for signs of surgical emphysema, dilatation of the neck veins,
asymmetry of the chest wall, excessive respiratory effort and abnormal rate.
The aim is to exclude and treat life threatening injury which are:
Tension pneumothorax.
Open pneumothorax
Flail chest with contusion
In tension pneumothorax, lung tear acts as a one-way valve, with each inhalation,
additional air accumulate in the pleural space. The normally negative intrapleural pressure
becomes positive, which depresses the ipsilateral hemidiaphragm and shifts the
mediastinal structures into the contralateral chest. Subsequently, the contralateral lung is
4
compressed and the heart rotates about the superior and inferior vena cava; this decreases
venous return and ultimately cardiac output, which results in cardiovascular collapse.
Clinically: hypotension, tracheal deviation away from the affected side, lack of breath
sounds and subcutaneous emphysema on the affected side, distended neck veins due to
impedance of the superior vena cava.
Urgent maneuver
Immediate needle thoracostomy decompression with a 14-gauge in the second intercostal
space in the midclavicular line, then Tube thoracostomy in the ED before a chest radiograph
is obtained.
An open pneumothorax or "sucking chest wound" occurs with full-thickness loss of the
chest wall, permitting free communication between the pleural space and the atmosphere .
This compromises ventilation due to equilibration of atmospheric and pleural pressures,
which prevents lung inflation and alveolar ventilation, and results in hypoxia and
hypercarbia.
Definitive treatment requires closure of the chest wall defect and tube thoracostomy
remote from the wound.
Flail chest occurs when three or more contiguous ribs are fractured in at least two
locations.
Paradoxical movement of this free-floating segment of chest wall sufficient to compromise
ventilation.
Immediate stabilization should be done followed by definitive fixation
3--Circulation and control of bleeding
bleeding can occur in:
one on the floor and 4 more
1- external bleeding
2- chest cavity
3- Abdominal cavity
4- pelvis and bones fracture
5- intracranial
Assessment includes
Check pulse and blood pressure.
Secure two large-bore cannulae

5
Take blood sample for blood group and cross match
Commence fluid resuscitation
Emergency maneuver to stop external bleeding
Classic signs and symptoms of shock are tachycardia, hypotension, tachypnea, mental
status changes, sweating, and pallor .
The goal of fluid resuscitation is to re-establish tissue perfusion.
Fluid resuscitation begins with a 2 L (adult) or 20 mL/kg (child) IV bolus of Ringer's lactate.
Then blood should be given according to the need.
Urine output is a quantitative, reliable indicator of organ perfusion. Adequate urine output
is 0.5 mL/kg per hour in an adult, 1 mL/kg per hour in a child, and 2 mL/kg per hour in an
infant
During the circulation section of the primary survey, four life-threatening injuries that must
be identified and treated:
(a) massive hemothorax,
(b) cardiac tamponade,
(c) massive hemoperitoneum,
(d) mechanically unstable pelvic fractures.
A massive hemothorax (life-threatening injury number one) is defined as >1500 mL of blood
inside the chest
Causes in blunt trauma:
1- multiple rib fractures with severed intercostal arteries.
2- lacerated lung parenchyma.
Causes in penetrating trauma:
pulmonary hilar vessel injury.
A massive hemothorax is an indication for thoracotomy, but tube thoracostomy is critical to
facilitate lung re-expansion, which may provide some degree of tamponade.
Cardiac tamponade (life-threatening injury number two) occurs most commonly after
penetrating thoracic injuries, although blunt rupture of the heart, particularly the atrial
appendage occasionally seen.
Only <100 mL of pericardial blood may cause pericardial tamponade.
The classic diagnostic Beck's triad: dilated neck veins, muffled heart sound and a decline in
arterial pressure. This will result in:
6
This will result in
1- Impairment of right atrial filling and right ventricular preload.
2- Impedes myocardial blood flow, which leads to subendocardial ischemia and a further
reduction in cardiac output.
3- Cardiac arrhythmia
Urgent intervention
Pericardiocentesis is successful in decompressing tamponade in approximately 80% of
cases; the majority of failures are due to the presence of clotted blood within the
pericardium. Definitive treatment by thoracotomy
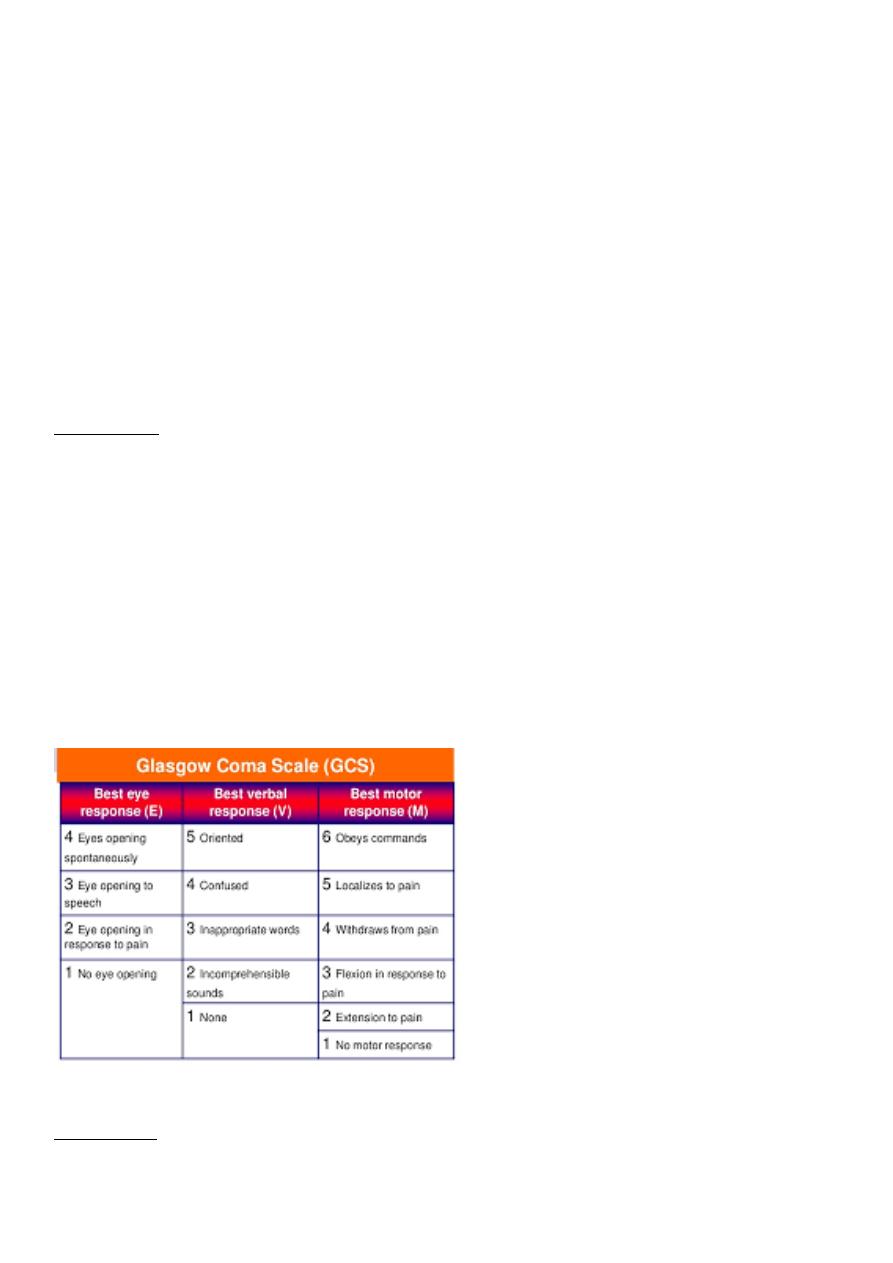
4--Disability
The neurological status of the patient should be rapidly assessed and repeated regularly by
using GCS
(Glasgow coma scale).
The pupils are monitored for size and reactivity.
Deferential diagnosis of altered level of consciousness include: hypovolaemia,
hypoglycaemia, alcohol and drug abuse.
GCS is calculated by adding the scores of the best motor response, best verbal response,
and eye opening. Scores range from 3 (the lowest) to 15 (normal).
Scores of 13 to 14 indicate mild head injury, 9 to 12 moderate injury, and 4 to 8 as sever
head injury
5--Exposure
The patient must be fully exposed and examined front and back using a carefully controlled
log roll.

7
Spinal alignment must be maintained during this procedure
Hypothermia can be rapid following trauma, and warming air blankets are vitally important
in the resuscitative phase.
Adjuncts to the primary survey
Blood tests – full blood count, urea and electrolytes, clotting screen, glucose,
toxicology, cross-match
ECG, pulse oximetry, arterial blood gas (ABG)
Two wide-bore cannulae for intravenous fluids
Urinary and gastric catheters
Radiographs of the cervical spine, chest and pelvis
SECONDARY SURVEY
The secondary survey does not begin until after the primary survey has been completed,
and all potentially life-threatening injuries have been dealt with.
The purpose of the secondary survey are
1- Identify all other injuries and perform a ‘head to toe’ examination.
2- Here that the patient’s history is reviewed.
Review of patient’s history (AMPLE)
■ Allergy ■ Medication, including tetanus status ■ Past medical history ■ Last meal ■ Events
of the incident
Secondary survey physical examination
Head and face.
Evaluate the head for penetrating injuries and depressed fractures, and any evidence of
bleeding or discharge from the nose or ears suggestive of a basal skull fracture. .
Check the face for maxillofacial fractures and ocular injury.
Inspect the mouth, mandible, zygoma, nose and ears. Exclude midfacial injury and
potential airway compromise
Neck
Inspect and palpate the cervical spine for haematomas, crepitus, tenderness and evidence
of steps on palpation.
8
The spine is held immobilized until formally cleared clinically and radiographically.
Chest
Review the primary survey and perform full palpation and auscultation of the chest wall.
Palpate the entire chest wall including the clavicle, sternum and ribs.
Abdomen and pelvis
Inspect for distension, bruising or penetrating wounds.
Inspect and palpate for tenderness and signs of peritonism.
Palpate the iliac crests for pain which might indicate pelvic instability, resulting from ring
fractures.
Inspect the perineum for evidence of ecchymosis or bleeding.
A rectal examination is needed to assess tone, prostate level and to look for bleeding.
Vaginal examination with a speculum also should be performed in women with pelvic
fractures to exclude an open fracture.
Urethral injuries are suspected if examination reveals blood at the meatus, scrotal or
perineal hematomas
Blunt abdominal trauma initially is evaluated by FAST in most major trauma centers.
(Focused Assessment with Sonography in Trauma
The benefits of the FAST includes:
1- Decreases the time to diagnosis.
2- Helps accurately diagnose
3- Asses hemoperitoneum
4- Is noninvasive.
5- Can be integrated into the primary or secondary survey
6- Can be performed quickly, without removing patients from the clinical arena
7- Can be repeated.
8- Is safe in pregnant patients and children, as it requires less radiation than CT
Abdominal stab wounds should be explored under local anesthesia.
Injuries that do not penetrate the peritoneal cavity do not require further evaluation.
Patients with fascial penetration must be further evaluated for intra-abdominal injury, by,
diagnostic peritoneal lavage (DPL), or CT scanning.

9
Minimal evaluation is required before laparotomy for gunshot or shotgun wounds that
penetrate the peritoneal cavity, because over 90% of patients have significant internal
injuries.
Extremities
Examine the vascularity, nerve, bone, joints, and tendons.
Deformed limbs should be manipulated into as near anatomical alignment as possible,
remembering to document the distal neurovascular status before and after the
intervention.
Adjuncts to the secondary survey
Selective radiography and laboratory tests are done early in the evaluation after the
primary survey.
For patients with severe blunt trauma, lateral cervical spine, chest, and pelvic radiographs
should be obtained, often termed the big three.
Blood samples for a routine trauma panel (complete blood count, blood chemistries,
coagulation studies, lactate level, and arterial blood gas analysis) should be sent to the
laboratory.
Definitive care and transfer or the third survey
A careful and complete examination followed by serial assessments help recognize missed
injuries and related problems.
Early transfer to an appropriate care facility is the most important contributor to successful
outcome.
When it becomes mandatory to transfer the patient from the initial receiving hospital, the
patient must be haemodynamically and cardiovascularly stable.
An experienced anesthetist should accompany the patient, the airway should be secured as
necessary.
