
1
Third stage
Surgery
Lec-2
.د
محمد صالح
1/1/2016
Post-operative care
Post-operative care:
The aim of postoperative care is to provide the patient with as quick, painless and safe a
recovery from surgery as possible
Patient recovery
Once patients are fully conscious and comfortable and their vital functions are stable they are
transferred to the general ward;
however, patients who are at high risk may be transferred to a high-dependency or intensive
care unit.
POSTOPERATIVE CARE OF THE PATIENT
After the operation the patient should be safely transferred to the bed from the operating
table, under the supervision of the anesthetist and surgeon.
A clear operative note should be written immediately. This should include instructions on the
postoperative care, including the thresholds for calling back the surgeon.
The following details should be included in the operative
note:
1 - Patient’s details – full name, date of birth, hospital number, address, ward.
2 - Date (and start/finish time) of operation.
3 - Operating room.
4 - Name of operation.
5 - Surgeon, assistant, anesthetist.
6 - Anesthetic type.
7 - Patient positioning and set-up.
8 - Was a tourniquet used, were antibiotics given, was the patient catheterised, type of skin
preparation, method of draping.
9 - Tourniquet time, if applicable.

2
10 - Operative details including:
• Incision;
• Approach;
• Findings;
• Procedure (appropriate illustration, if appropriate);
• Complications, untoward events;
• Implants used;
• Closure, including suture material used;
• Dressing;
• Postoperative state (e.g. distal neurovascular status);
• Type of dressing used.
11 - Postoperative instructions relevant to surgery:
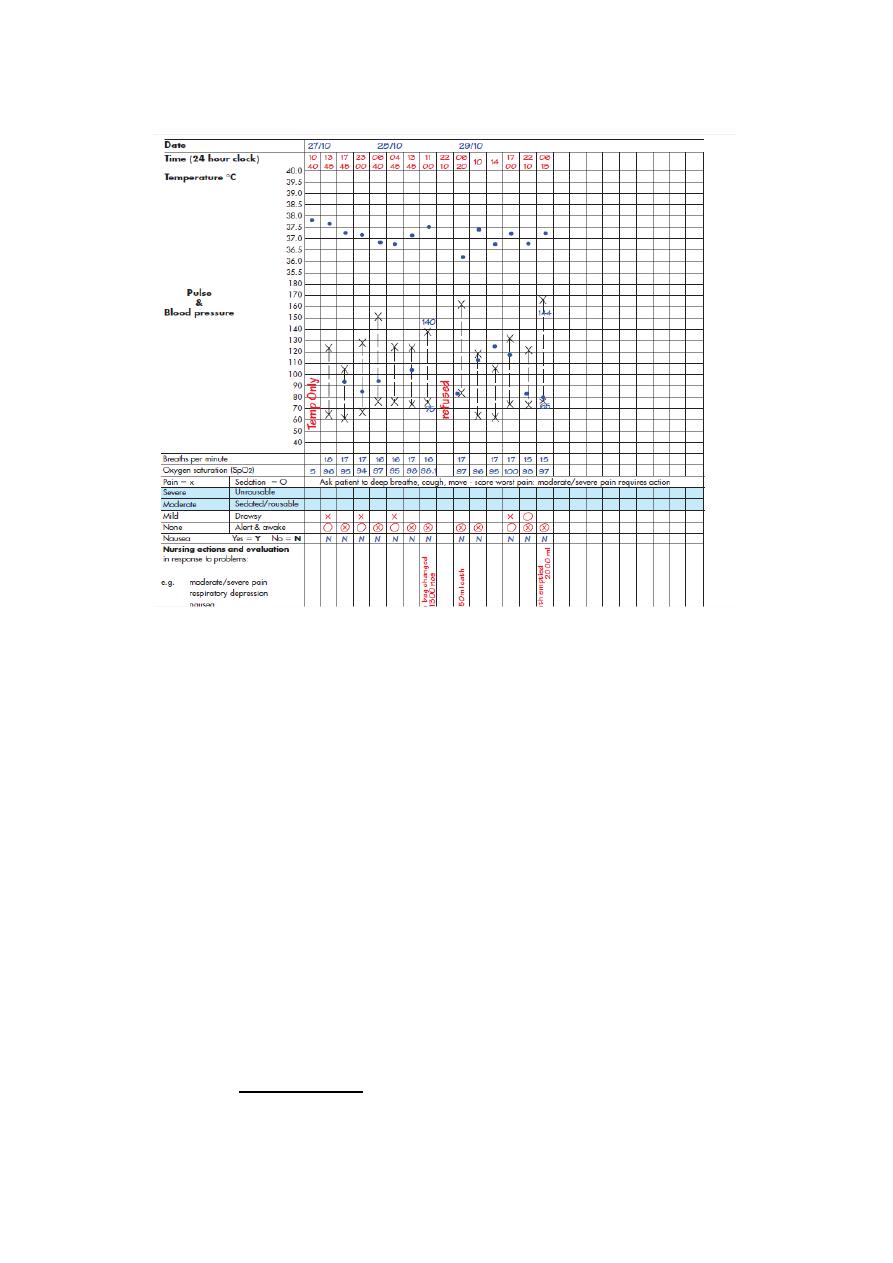
• Observations required and frequency, e.g. 4-hourly pulse and blood pressure measurements
for 24 hours
• possible complications and action to be taken if complications occur, e.g. if blood loss
exceeds 500 ml in a drain call the surgeon
• treatment, e.g. intravenous fluids;
• time lines for patient recovery, e.g. when to mobilise, when to resume normal oral intake,
the need for physiotherapy, allowable movements, dressing changes.
12 - Discharge and follow-up details; instruction for sutures, splints, casts
SOAP
Subjective
Objective
Assessment
Plan
- Subjective
Ask the patient how he is.
- Objective
Check the patient’s charts for temperature, pulse and respiration
(TPR), fluid balance
Specific examinations also need to be recorded, such as
- Bowel sounds after abdominal surgery or
- Distal neurovascular status after orthopedic procedures.
- Regularly review nutritional status in those patients who may
b
e in negative nitrogen
balance.
3
- Review all laboratory results and investigations.
- Review the drug chart to ensure that drugs are not being continued unnecessarily.
- Record all relevant findings (both negative and positive) clearly in the notes
Assessment
Review all of the information obtained under S and O and list the
problems that the patient is now facing
Plan
Formulate and agree a plan with the patient and the staff and
record that plan in the notes.
This includes anticipating when discharge from hospital might occur and ensuring that
everything is in place (e.g. social services) to prevent any unnecessary delay.
This is the minimum set of notes required on each patient every day.
These notes should be dated, signed and legible.
Pain management
Optimal management of acute postoperative pain requires planning,
patient and staff education and tailoring of the regimen to
the type of surgery and the needs of the individual patient.
) in their requirement for analgesia, even after identical
up to eightfold
Patients vary greatly (
surgical procedures.
Under treatment results in unacceptable levels of pain with tachycardia
hypertension, vasoconstriction .

4
Painful abdominal and thoracic wounds restrict inspiration, leading
to tachypnoea, small tidal
volumes and inhibition of effective
coughing and mobilisation.
This predisposes to chest infection
delayed mobilisation, deep venous thrombosis, muscle
wasting
and pressure sores
pain, the fifth vital sign’
requires regular pain measurement, with staff to be alerted in the
event of high scores .
The joint working party report also encouraged
the use of combined ‘multimodal’ analgesia
comprising local anaesthesia and simple analgesics such as paracetamol (acetaminophen)
and non-steroidal anti-inflammatory drugs (NSAIDs)
with opioid drugs
Simple analgesic agents
In minor surgery and when the patient is able to eat after surgery,
NSAIDs and paracetamol may be sufficient
- Codeine phosphate is commonly favoured after intracranial surgery
because of its intermediate respiratory depressant effect; however,
it should not be given intravenously as it can then cause profound
hypotension. Constipation is also not uncommon with codeine
- Rectal and intravenous diclofenac or intravenous ketorolac are commonly used NSAIDs in
the perioperative period.
Stronger analgesic agents
With adjuvant analgesics in combination, regular intramuscular
morphine injection can provide effective treatment for the majority of surgical patients
Techniques for postoperative pain relief
■ Regular intramuscular injections – may get pain breakthrough
■ Local anaesthetic block – ideal if it works
■ Indwelling epidural – good pain control -opioids may depress respiration
■ Continuous infusions – reduce oscillations in pain relief but risk overdose
■ Patient-controlled analgesia – pain relief titrated to patient’s needs
5
Fluid, electrolyte management
1- Give daily requirement
2- Add fluid lost by bleeding, NGT, drains
SPECIFIC POSTOPERATIVE
COMPLICATIONS
Respiratory complications
Shortness of breath
The commonest cause of postoperative dyspnoea (shortness of breath) and rapid shallow
breathing is alveolar collapse or atelectasis.
The diagnosis is confirmed by clinical examination and radiography). Atelectasis usually
responds to chest Physiotherapy
Causes of acute postoperative shortness of breath
■ Myocardial infarction and heart failure
■ Pulmonary embolism
■ Chest infection
■ Exacerbation of asthma or chronic obstructive airway Disease
Cyanosis
In patients whose airway is clear but who develop cyanosis the problem may be in the lungs
or in the circulation.
Common problems in the lung may be acute bronchospasm
Cardiovascular complications
Hypotension
Whatever the cause of hypotension, the emergency treatment
requires an increase in the fluid input with administration of high-flow oxygen
Low blood pressure postoperatively
6
■ dehydration
■ anaesthetic
■ blood loss
■ morphine
■ myocardial infarct
Hypertension
High blood pressure may be dangerous in patients with ischaemi heart disease or
cerebrovascular disease as it may precipitate infarction or stroke.
Most causes of hypertension relate to inadequate pain relief or anxiety and usually settle with
appropriate analgesia.
Deep vein thrombosis
There are several risk factors for deep vein thrombosis (DVT).
Most patients with postoperative DVT show no physical signs;
however, they may present with calf pain, swelling, warmth, redness and engorged veins.
On palpation the muscle may be tender and there is a positive Homans’ sign (calf pain on
dorsiflexion of the foot); however, it must be emphasised that this sign is neither specific nor
sensitive
Gastrointestinal complications
Postoperative nausea and vomiting
This is a common problem
Urinary complications
Urine output (oliguria/anuria)
Oliguria may be defined as urine output less than the minimum obligatory volume (0.5 ml
kg–1h–1).
The commonest cause of oliguria postoperatively is reduced renal perfusion resulting from
perioperative hypotension or inadequate fluid replacement
