Urinary problems in gynecologyDr. Samar D. Samar
Urogynecological conditions include:urinary incontinence
voiding difficulties
frequency
urgency
UTI
prolapse
fistula
Urinary incontinence
It is involuntary loss of urine and is a social and hygienic problem. It is associated with significant reduction in quality of life.EPIDEMIOLOGY — the prevalence of urinary incontinence in women, using the inclusive definition of any leakage at least once in the past year, ranges from 25 to 45 percent.
the prevalence of urinary incontinence appears to be higher in non-Hispanic white women compared with African American women.
Incontinence increases with age.
RISK FACTORS — Established risk factors for urinary incontinence in women are:
childbearing
obesity
other urinary symptoms
and functional impairment.
The role of caffeine, alcohol and asymptomatic bacteruria has not been proven.
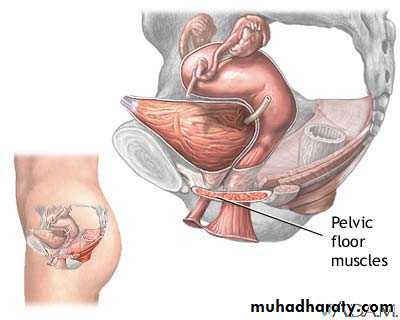
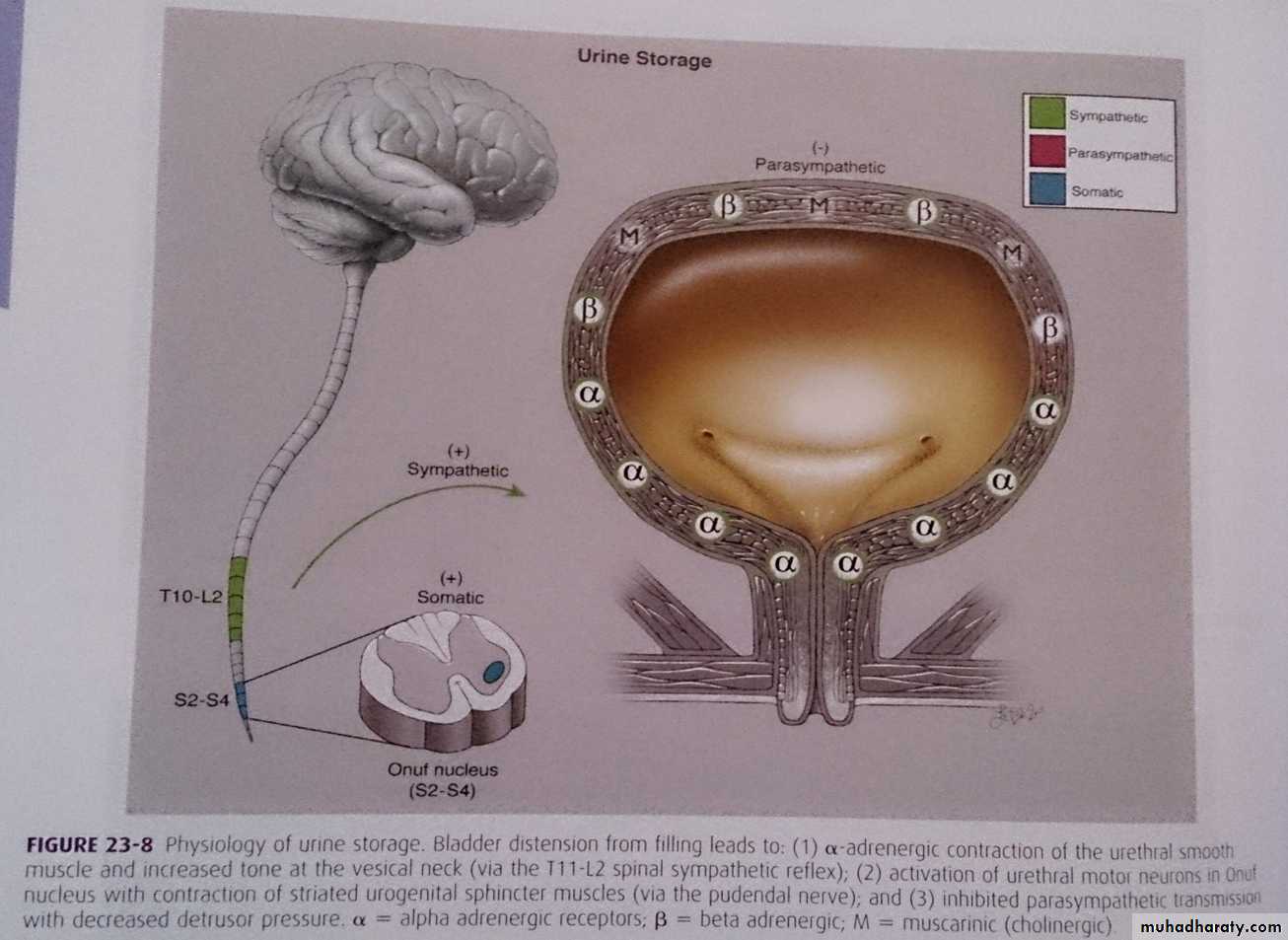
PATHOGENESIS — Continence depends upon: both intact micturition physiology
and an intact functional ability to toilet oneself.Normal micturition —
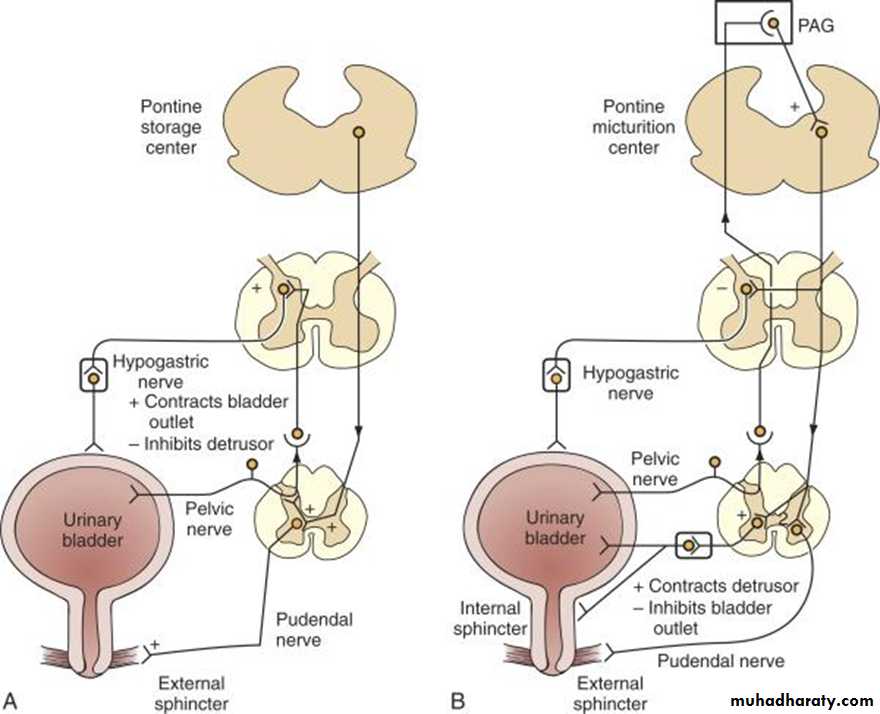
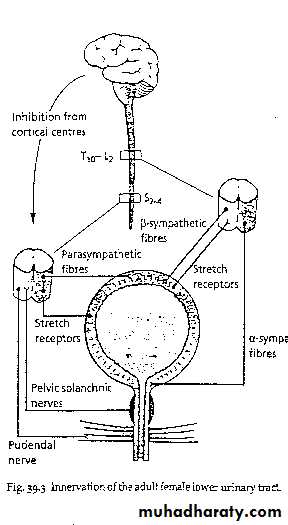
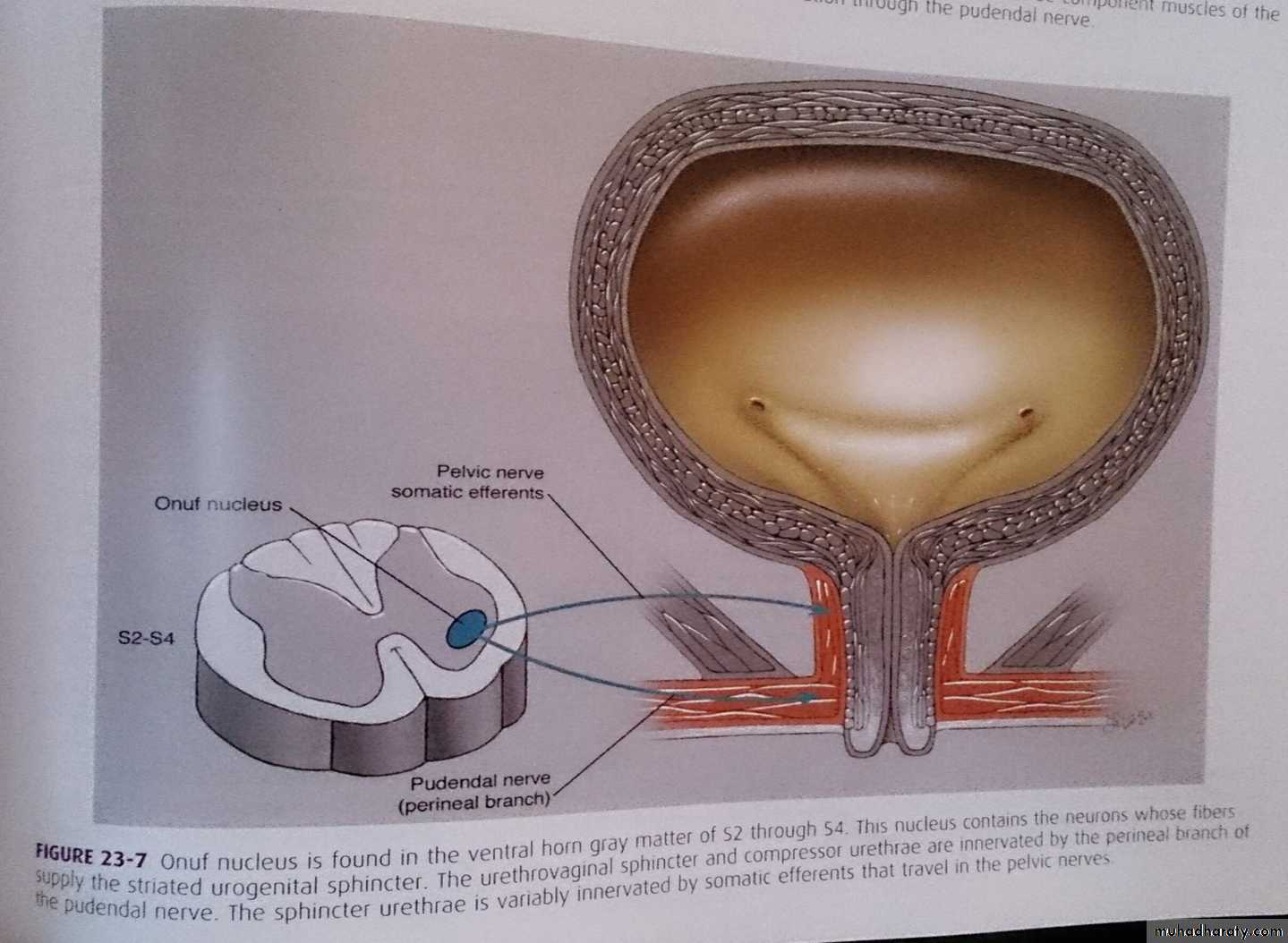
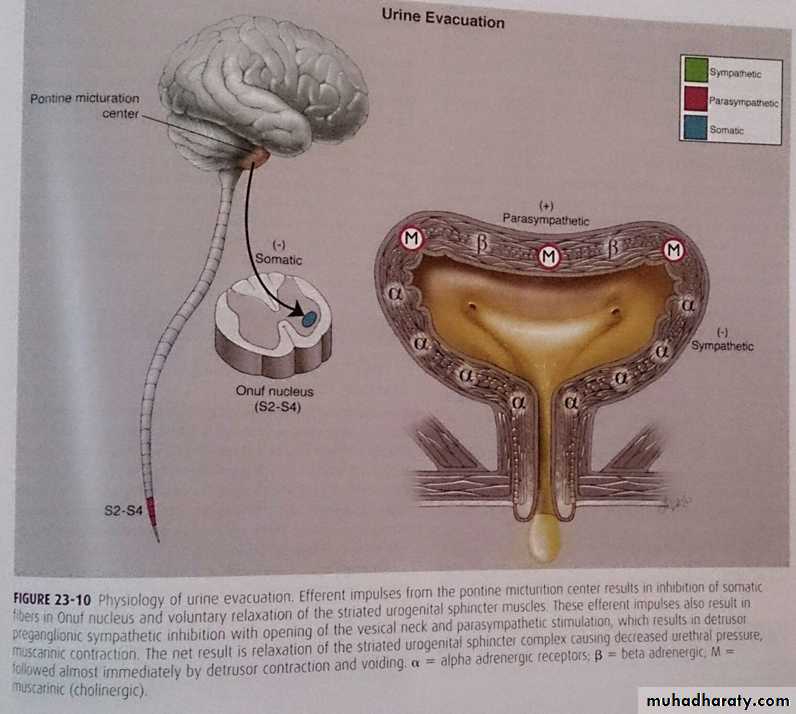
*Central coordination of micturition occurs in the pontine micturition center.*Peripheral coordination occurs in the sacral micturition center at cord levels S2-S4.
Normal micturition
Central nervous control of micturition is complex requires sacral spinal reflex arc controlled by the upper centers it is controlled by excitatory and inhibitory centers.
Somatic innervation for striated muscles
Autonomic innervation for smooth muscles, (sympathetic and parasympathetic).
Continence:
Continence requires the complex coordination of multiple components that include:Muscle contraction and relaxation.
Appropriate Connective tissue support.
Integrated innervation and communication between these structures.
Pathophysiology of urinary incontinence
Normally: urine leave the bladder via urethra only when the intravesical pressure exceeds the maximum urethral pressure.In urinary incontinence:
bladder pressure exceeds the urethral pressure if:
Urethral sphincter mechanism is weak
Detrusor pressure excessively high (over active)
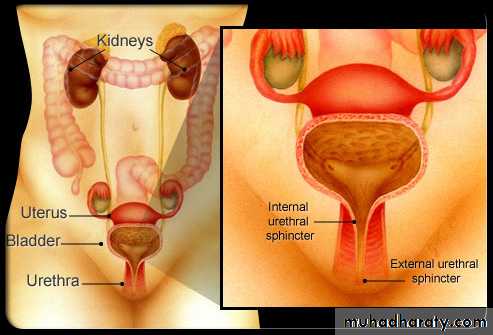
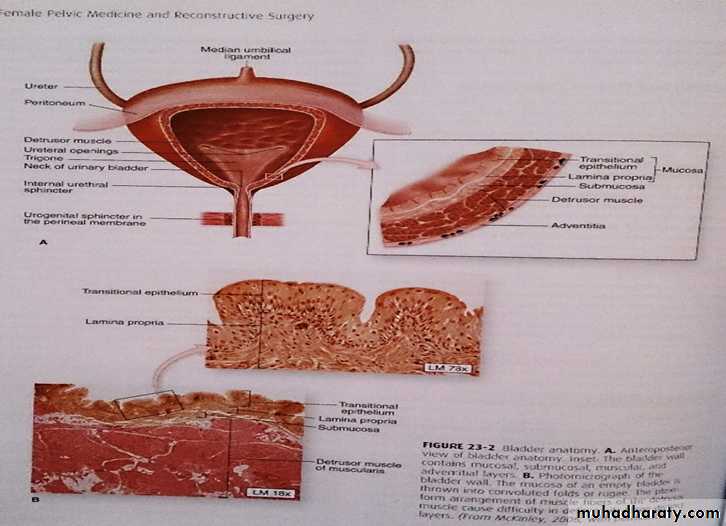
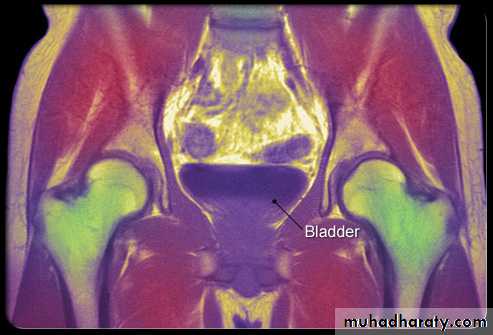
Bladder:
Is situated behind the symphysis pubis and is covered superiorly and anteriorly by peritoneum.
Transitional epithelium (uroepithelium) covered with glycosaminoglycan (GAG) this prohibit bacterial adherence.
Then detrusor muscles in three layers arranged in plexiform fashion this arrangement is responsible for bladder expansion during filling.
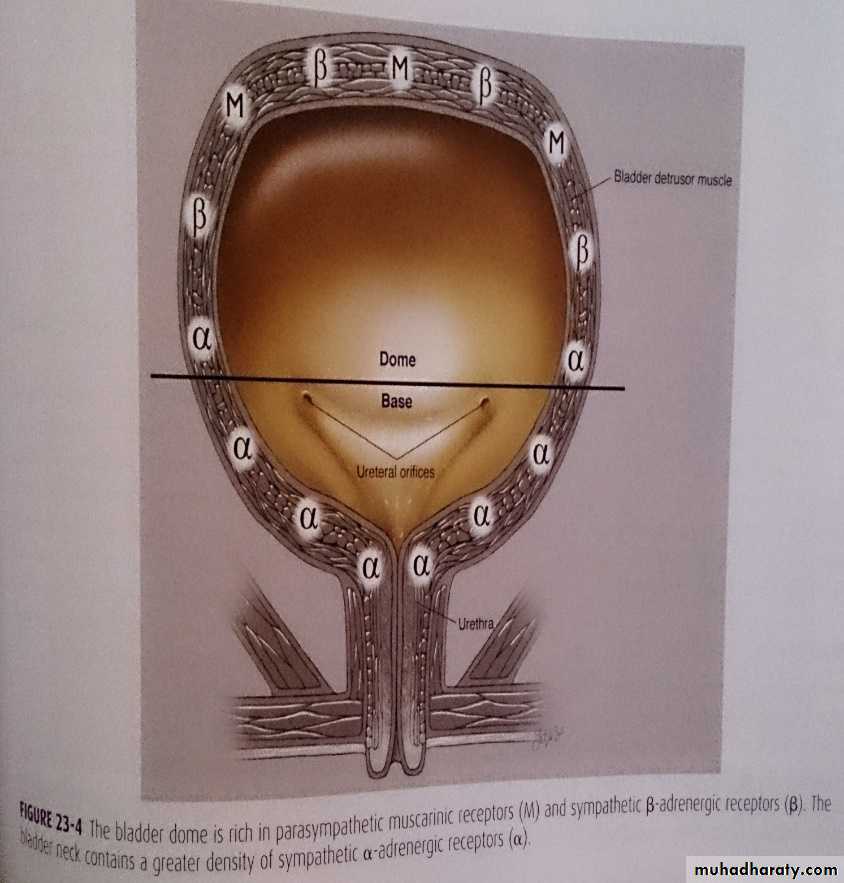
Innervation:
Detrusor muscles is rich in parasympathetic muscarinic receptors.Dom of bladder and bladder neck has B adrenergic receptors
Bladder neck and urethra has alpha adrenergic receptors
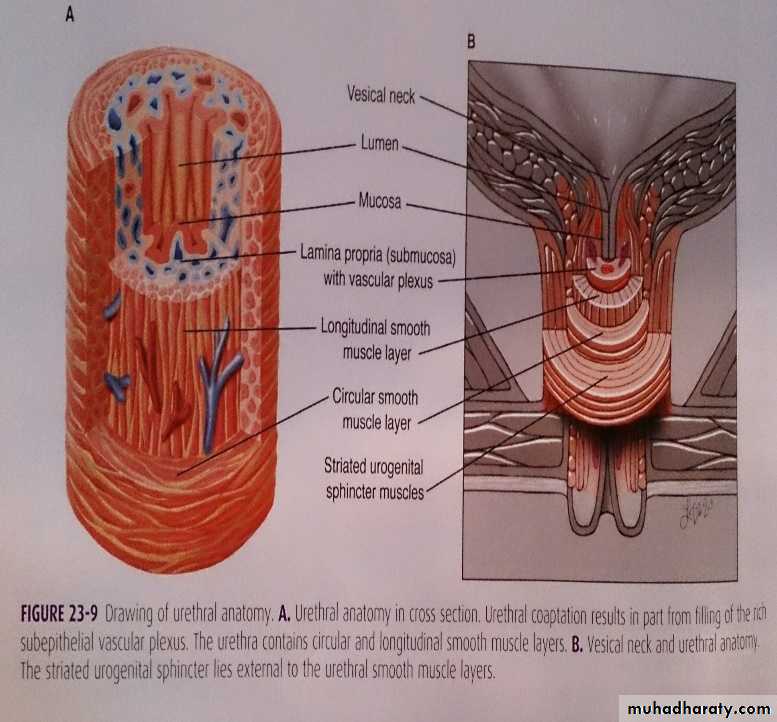
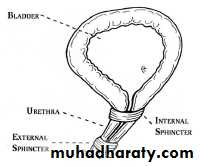
Urethra
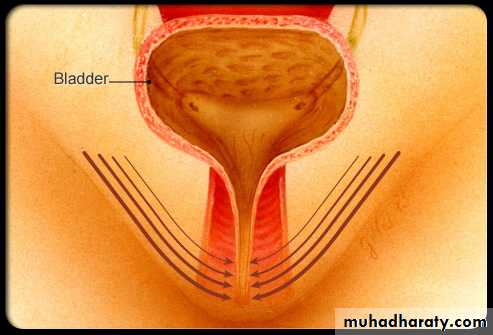
Urethral length is from 3-5 cm in female.One key in adequate continence is: urethral mucosal coaptation
The urethra consists largely of a rich vascular "sponge", lined by a moist mucosal layer and surrounded by a coat of smooth muscle, fibro-elastic tissue and striated muscle.
The surrounding smooth muscle tone is mediated by alpha-adreno receptors in the sympathetic nervous system. All three layers are under estrogen control.
urethral muscles
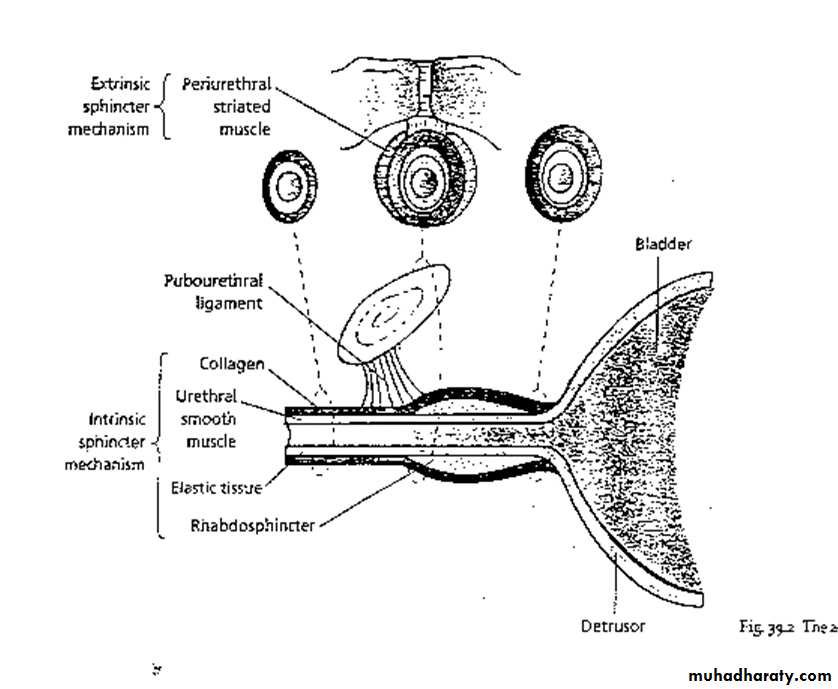
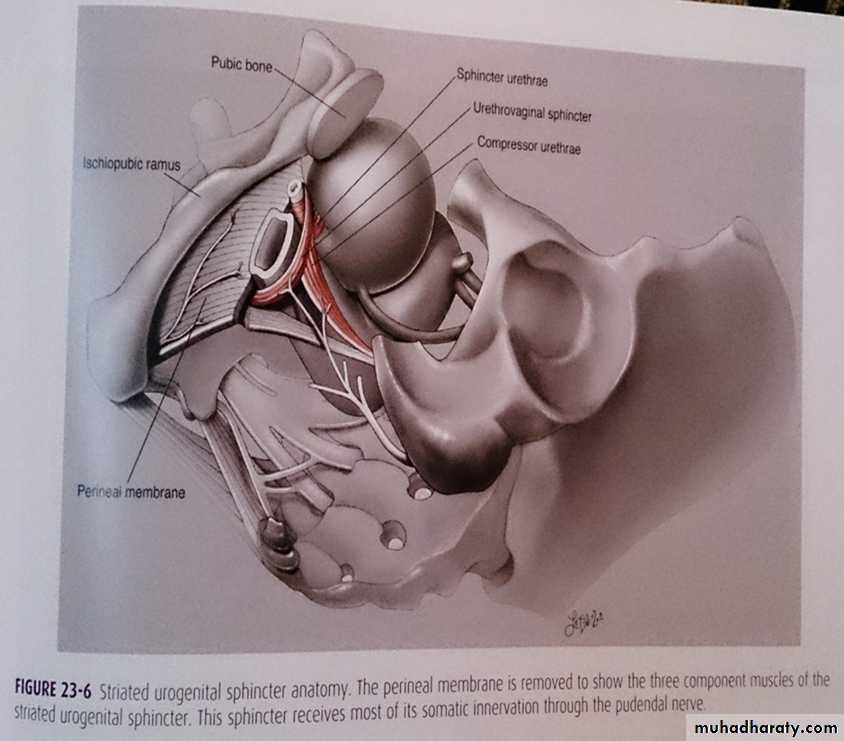
longitudinal oriented smooth muscles is continuous morphologically with detrusor muscles ( when contract lead to shortening and opening urethra)main bulk of striated muscles located in the middle third of urethra circularly arranges called rhabdosphincter urethrae this is the intrinsic sphincter mechanism (responsible for urethral closure at rest)
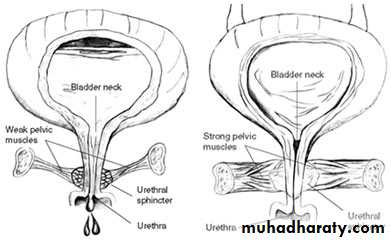
Weakness of the urethral muscles result in funneling of the proximal urethra and shortening of the functional urethral length
Extrinsic sphincter mechanism: consist of striated periurethral muscle (levator ani) is situated at the junction of the middle and lower urethra this contributes to additional closure force at time of physical effort.
Pubourethral ligament support the proximal urethra, it attach the urethra to pubic bone
So intrinsic and extrinsic sphincter mechanism are responsible for greater pressure within the urethra than in the bladder called positive closure pressure partly responsible for the maintenance of continence.
Innervation
Urethral smooth muscles with sympathetic fibers.Somatic part originate spinal levels S2-S4 innervate striated muscles of the sphincter.
- nerves involved here are branches of pudendal (innervate levator ani)
- and pelvic nerves (innervate rhabdosphincter urethrae).
Innervation at storage:
Urogenital sphincter :pudendal nerve and pelvic nerve for somatic muscle
sympathetic ( B adrenergic receptors) stimulation of the bladder dome and bladder neck result in smooth muscle relaxation.
alpha adrenergic receptors in bladder neck, base and urethra leads to urethral contraction and urine storage.
Innervation related to voiding:
Parasympathetic stimulation (muscarinic and nicotinic receptors) acetylcholine act on muscarinic receptors of bladder and urethra leads to detrusor muscle contraction and urethral relaxationStriated muscles relax.
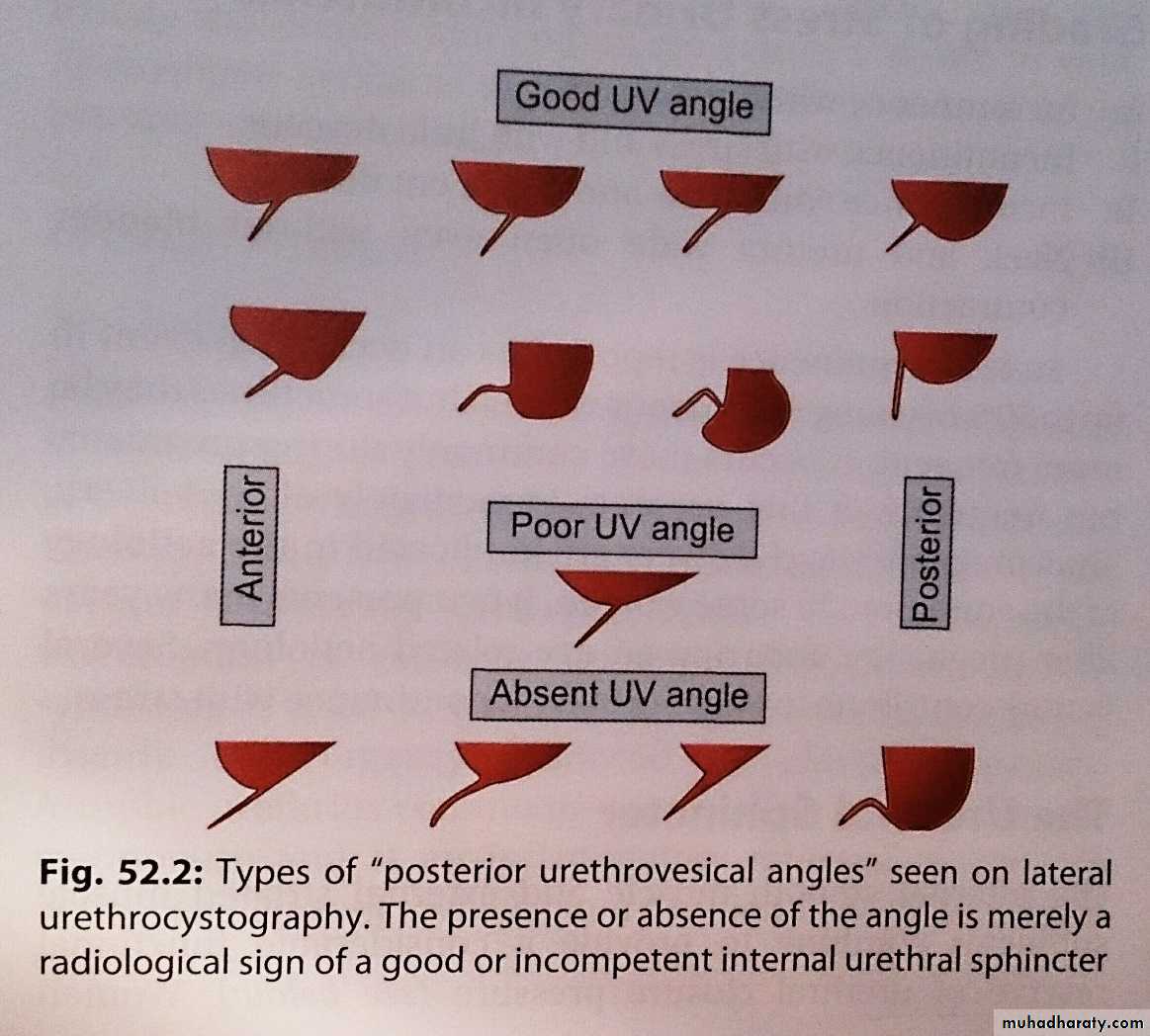
These are different types of posterior urethra vesical angles
Striated urogenital sphincter: (Sphincter complex includes)
1-The sphincter urethra: wraps circumpherentially around the urethra
2-Urethrovaginal sphincter3-Compressor urethra: act ventrally over the urethra and insert into the fibromuscular tissue of the anterior vaginal wall.
Symptoms associated with incontinence:
Urgency is the complaint of a sudden and compelling desire to pass urine that is difficult to defer.Urge incontinence is the complaint of involuntary leakage accompanied by urgency.
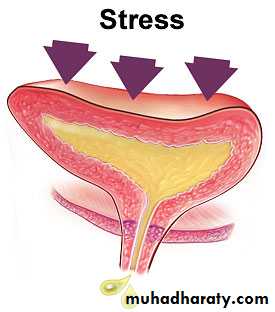
Stress incontinence is the complaint of involuntary leakage with effort, exertion, sneezing, or coughing.
Immediate leakage suggests failure of sphincter mechanisms, while delayed leakage suggests maneuver-induced uninhibited detrusor contraction.
Frequency is passing urine seven or more times a day or being awoken from sleep more than once a night to void.
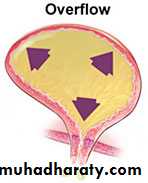
Overflow incontinence occurs without any detrusor activity when the bladder is over distended.
Classification of incontinence:
Urethral causes-Urethral sphincter incompetence (genuine stress incontinence).
-Detrusor instability-this is neuropathic or non-neuropathic.
-Retention overflow
-Congenital
-miscellaneous
Extra urethral causes
-Congenital
-Fistula
Incontinence related to reversible conditions.
Continence depends not only on the integrity of the lower urinary tract and its neurological control, but also on cognition, mobility, environmental factors, and the absence of medical factors that can affect these components and/or urine output
Urethral causes
Geniune Stress incontinence —Stress leakage occurs when increases in intra abdominal pressure overcome sphincter closure mechanisms in the absence of a bladder contraction.
Pathophysiology and causes of genuine stress incontinence:
*abnormal descent of the bladder neck and proximal urethra leading to negative urethral closure pressure.
*Impaired urethral support
*complete failure of urethral closure, called intrinsic sphincter deficiency (ISD). This usually results from operative trauma and scarring, but it can also occur with severe mucosal atrophy in postmenopausal women. Unlike the episodic, stress-maneuver-related leakage of genuine stress urinary incontinence, ISD leakage typically is continual and can occur while sitting or standing quietly.
Etiology:
*Damage to the nerve supply of the pelvic floor and urethral sphincter caused by child birth and trauma to the pelvic floor muscles and endo-pelvic fascia and ligaments.*Menopause and tissue atrophy
*congenital causes due to altered connective tissue and collagen.
*chronic causes as obesity, constipation and lung diseases.
Symptoms:
Stress incontinence
Frequency
Urge incontinence and prolapse may be present
Examination
It is demonstrated when the patient coughs.
Cystourethrocele or prolapse seen
Urodynamic studies will define the cause.
Detrusor instability
The etiology of urge urinary incontinence and the overactive bladder syndrome is presumed to be uninhibited bladder contractions (called detrusor over activity). However, detrusor over activity may be found in healthy, continent elderly individuals, suggesting that the over activity alone is not sufficient to cause incontinence.
Urge leakage symptoms may be due to factors outside of the lower urinary tract
Causes of detrusor over activity:
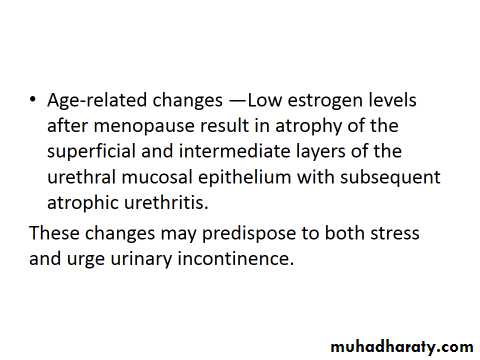
Age-related changes Interruption of central nervous system (CNS) inhibitory pathways (e.g., by stroke, cervical stenosis)
Bladder irritation caused by infection, bladder stones, inflammation, or neoplasms
Detrusor over activity in many cases may be idiopathic.
Pathophysiology:
It is poorly understood, poor toilet habit training and psychological factors have been implicated. Neuropathy is an important factor. Incontinence surgery, outflow obstruction and smoking are also associated with detrusor over activity.Symptoms:
Urgency
Urge incontinence
Frequency
Nocturia
Stress incontinence
Enuresis
Voiding difficulties
Examination
Any mass or prolapse
Mixed incontinence —
Mixed incontinence is the most common type of urinary incontinence in women. Although generally thought to represent the overlap of two mechanisms, detrusor over activity and impaired urethral sphincter function, the actual pathophysiology of mixed urinary incontinence is still under investigation.Retention with Overflow —
The term "overflow incontinence" has been used to describe the dribbling and/or continuous leakage associated with incomplete bladder emptying due to:impaired detrusor contractility
and/or bladder outlet obstruction.
Leakage typically is small volume, although its continual nature can lead to significant wetting. The post void residual is elevated, and there may be a weak urinary stream, dribbling, intermittency, hesitancy, frequency, and nocturia. Stress-related leakage may be apparent, reflecting an otherwise intact sphincter mechanism overwhelmed by the large bladder volume.
Causes:
Upper or lower motor neuron lesion
Urethral obstruction
Pharmacological.
Symptoms
Poor stream, incomplete bladder emptying, over flow incontinence and recurrent UTI.Cystometry, U/S, IVU are usually needed.
Congenital: Epispadias, due to faulty midline fusion of mesoderm result in a widened bladder neck and short urethra.
Miscellaneous
UTI
Urethral diverticulum
Extra urethral incontinence
*Congenital:Bladder extrophy absence of anterior abdominal wall and anterior bladder wall, surgery is necessary in neonatal period.
Ectopic ureter: cure is by excision of the ectopic ureter and the kidney that it drains.
*Fistula:
Is abnormal opening between the urinary tract and the outside.
* Incontinence related to reversible conditions —.
Frequency and urgency: it occurs in 15-20% of women.Voiding difficulties: 10-15% may have voiding difficulties.
Urinary tract infection:Investigations:
*Accurate and detailed history and examination*Mid stream urine specimen
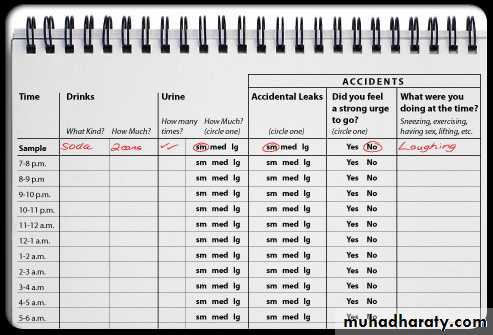
*Urinary diary — a diary of continent and incontinent voids is a reproducible and reliable method to establish the baseline urinary incontinence severity that can be followed with treatment. It also provides useful diagnostic and therapeutic clues, such as the usual timing and circumstances of urinary incontinence, modal voided volume (amount of urine per void, a proxy for functional bladder volume), voiding and urinary incontinence frequency, and the total daytime and nocturnal urine output
Patients (or caretakers) should be instructed to record the time and volume of every continent and incontinent void over at least 48 to 72 hours.
*Pad test – used to verify and quantify urine loss, it takes one hour the patient wears a pre weighed sanitary towel, drinks 500 cc of water the pad is reweighed, urine loss of more than 1 gm is considered significant. Methylene blue can be used to differentiate between urine and other loss.
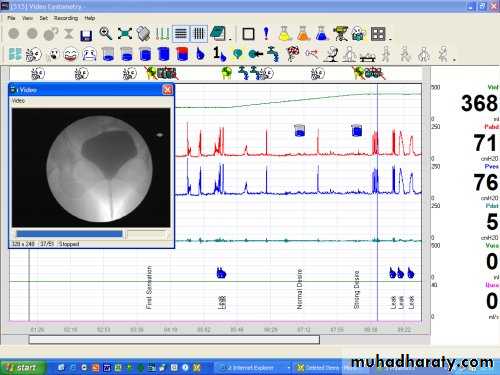
Urodynamic testing — routine urodynamic testing in the evaluation of urinary incontinence is not recommended.
Urodynamics are the diagnostic "gold standard," but are invasive, expensive, require special equipment and training, are not usually necessary to make the diagnosis, and have not been found to affect outcome.
Uroflowmetry: measurement of urine flow rate, non invasive.
Cystometry: measurement of pressure – volume relation ship of the bladder.
Videocystourethrography: is radio opaque filling medium used during cystometry and visualized by x-ray screening.
IVU
U/S
MRI
Cystourethroscopy
Urethral pressure profilometry-
Ambulatory monitoring – fine transducers are inserted in the bladder and urethra the device is carried by the patient the pressure is recorded.
Treatment:
Simple measures, exclude UTI, restrict fluid intake, modify medication, and treat chronic cough and constipation.
Genuine stress incontinence:
Prevention:Shortening second stage and reduce traumatic delivery.
Hormone replacement and pelvic floor exercise may be of help.
Conservative management:
Physiotherapy is the mainstay of the conservative treatment of stress incontinence it is more effective in pre menopausal than postmenopausal women.
Using weighed cones or electrical stimulation may give some benefit.
Surgery:
Aim of surgery
1-Restore proximal urethra and bladder neck
2-increase urethral resistance
3-a combination of both
Choice of operation depends on clinical and urodynamic features and route of approach.
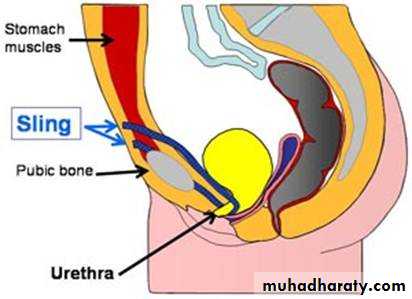
Surgical cure of stress incontinence necessitate elevation of the proximal urethra to an intra abdominal position to improve pressure transmission and posterior urethra vesical angle.
Recent researches suggest pelvic floor and urethral sphincter muscles denervation.
TYPES OF SURGICAL PROCEDURES
*Kelly-Kennedy plication —The Kelly-Kennedy plication is usually added to the anterior colporrhaphy for the purpose of treating SUI. It involves placement of two sutures underneath the bladder neck, plicating the endopelvic fascia and providing support to the area. The Kelly plication is used in older women with mild stress incontinence undergoing a colpocleisis. Success rates as high as 75 percent have been reported. Long-term data; however, indicate that the success rate declines significantly with time.
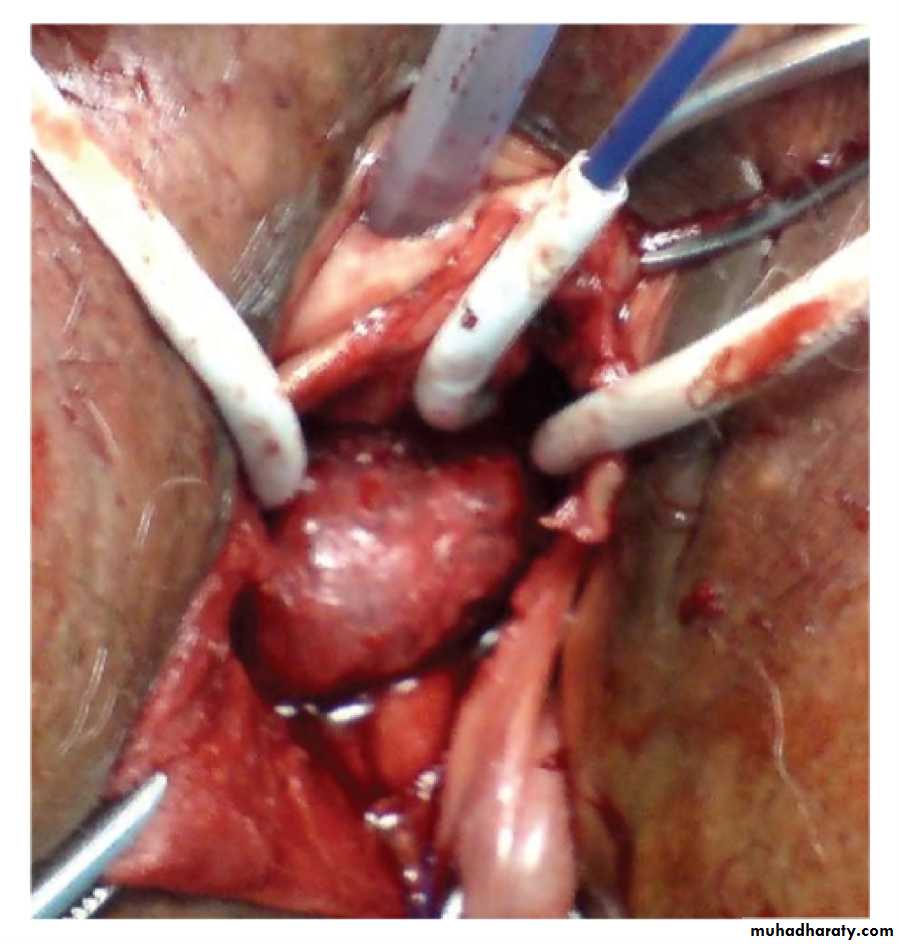
Colposuspension operation is associated with highest success rate95% at one year.
It is effective operation for stress incontinence.Retropubic procedures — The Burch colposuspension and the Marshall-Marchetti-Krantz (MMK) procedure are the two most common retropubic operations for SUI. In the Burch procedure, the endopelvic fascia adjacent to the mid and proximal urethra at the bladder neck is attached to the pectineal (Cooper's) ligaments on the posterior surface of the superior pubic ramus. The MMK procedure attaches the endopelvic fascia next to the bladder neck to the periosteum of the posterior pubic symphysis.
The Burch procedure can be performed by laparotomy or laparoscopically.
Complications of the Burch procedure include:
Urinary retention Detrusor over activity Injury to the bladder or ureter Infection Hemorrhage, Enterocele.Laparoscopic Colposuspension of the bladder neck is gaining popularity. Pereyra or stamey.
*artificial sphincter –increase out flow resistance.
*periurethral injections - increase out flow resistance. collagen is injected I the periurethral tissues at the level of the bladder neck.Early success of 80-90%, but there is time dependent decline.
Complications: UTI and retention of urine.
*Sub urethral slings — first described in 1907, a sub urethral sling is a hammock that supports the bladder neck and urethra, thus preventing rotational descent during increases in abdominal pressure and providing a stable platform for urethral compression. The choice of SUI surgery has been usually based upon the severity of incontinence.
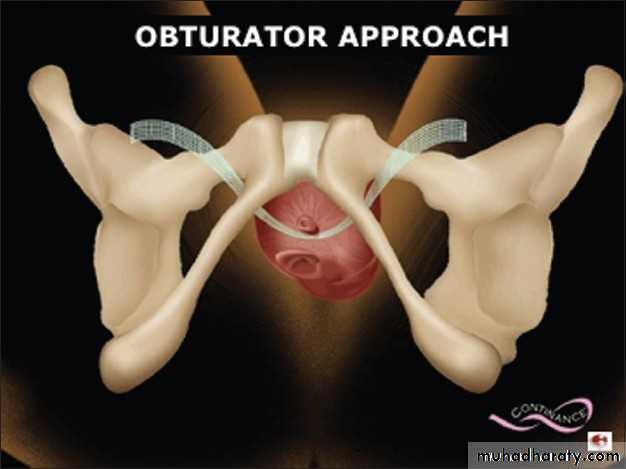
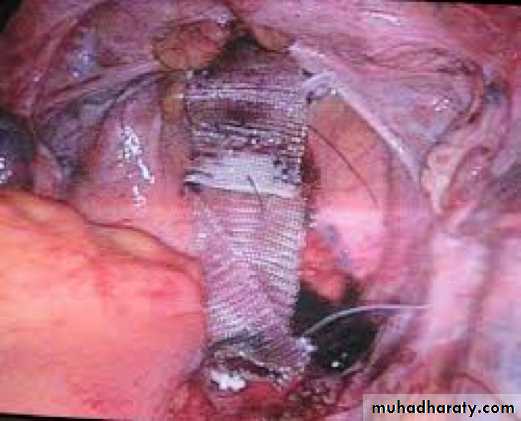
Trans vaginal mesh
The tension free vaginal tape (TVT) procedure is a type of synthetic sub urethral sling, and has become the procedure of choice for treatment of SUI in many institutions. We use prolene tape which is self retaining.
The trans-obturator (TOT) route of sling placement is also gaining in popularity due to decreased rates of postoperative urinary retention and possible avoidance of key structures found in the retropubic space.
Complications — Complications of the sub urethral sling can be divided into intra operative and postoperative complications.
Operative complications include: bladder laceration, urethral transection, vascular damage, gastrointestinal damage and nerve damage.
Postoperatively, the most troublesome complication is urinary retention due to sling obstruction.
Detrusor instability and voiding difficulty:
Treatment by bladder training, hypnosis, anticholinergics as oxybutynin or tolterodine.Imipramine for enuresis.
Desmopressin for Nocturia.
Self catheterization.
FISTULA IN GYNECOLOGY
TYPES OF FISTULA:Vesico-vaginal fistula.
Recto- vaginal fistula.
Colo-vaginal fistula.
Uretero-vaginal fistula.
Vesico-vaginal fistula:
It is the most distressing type because urine constantly escape from vagina, making the underclothes wet and leaving a persistent smell of urine.
Causes:
Direct trauma:
- Unrecognized penetrating injuries of anterior vaginal wall may involve the bladder leading to fistula.
Unrecognized Bladder injury during obstetric and gynecological operations (cesarean section, abdominal and vaginal hysterectomy).
Obstetric injury:
In cases of cephalo-pelvic disproportion prolonged labor may cause compression of bladder base between fetal head and pubic bone leading to avascular necrosis of the bladder. After some days bladder base sloughs and fistula develops.
Neoplastic fistula:
Carcinoma of cervix may invade the bladder causing fistula.
Bladder cancer rarely.
Radiation:
Vaginal radioactive elements application (cesium).
Diagnosis:
History of constant leak of urine from the vagina.Examination of anterior vaginal wall by Sim’s speculum.
• Small fistulae hardly admit a probe, whereas large ones admit one or two fingers.
Cystoscopy may be used to detect small fistulae.
Treatment:
Prevention is easier than cure:Better obstetric care, hospital deliveries, early recognition of cases of obstructed labor and emergency cesarean section all can prevent fistula formation.
During pelvic operations the bladder must be treated with care to avoid operative injury and if bladder damage is suspected then every effort should be made to repair it at this stage which would be more successful and spare the time for the patient before a secondary repair can be attempted.
If fistula is found within seven days of injury, it can be treated by primary closure, otherwise two or three months should elapse between the development of fistula and its repair which allow local tissue damage and infection to settle down and any urinary infection to be eradicated.
The principle of the operation is to isolate and remove the fistulous track, separate the bladder mucosa from the vaginal skin and then to close the mucosa of the bladder carefully without tension and close vaginal skin. Most of these fistulae can be closed by operations via vaginal route.
Post-operative care is very important and great care should be taken to secure constant drainage of the bladder by catheter for about three weeks to enable the repair to heal (an indwelling suprapubic catheter is ideal).
Fistulae due to radiation damage may be difficult to close because the tissues are so avascular. For patients with short expectation of survival, implantation of the ureters into an isolated loop of ileum with colpocleisis (closing the vagina below the fistula to stop the leak), may be performed.
Sometimes several operations are needed to close the fistula.
Expert obstetric supervision is most important for future labor, many of which will be treated by cesarean section.
Recto-vaginal fistula:
Causes:- Most of recto-vaginal fistulae are the result of unrepaired third degree laceration of the perineum and posterior vaginal wall or repairs that have broken down, so that an opening is left from the rectum into the vagina.
- Advanced carcinoma of the rectum or vagina.
- Burns caused by radiotherapy usually result in a stricture rather than fistula.
Treatment:
If the fistula is very small only mucous will leak from the rectum, but with most fistulae flatus and even feces when loose stool will leak.The fistula is repaired after a course of antibiotics to decrease bowel infection. Its edges are excised and it is repaired in two layers.
When the fistula is near the sphincter, it is advisable to divide the perineum up to the fistula, whenever the sphincter is concerned in the damage; its torn ends must be exposed and sutured together to restore continence.
Rarely a temporary colostomy is needed.
Colo-vaginal fistula:
It is rare. It may result from rupture of pericolic abscess (secondary to diverticulitis) into the posterior vaginal fornix. The fistula is usually small but there is intermittent feculent discharge.
The diagnosis is by barium enema.
Its closure involves laparotomy and resection of the affected part of the colon.
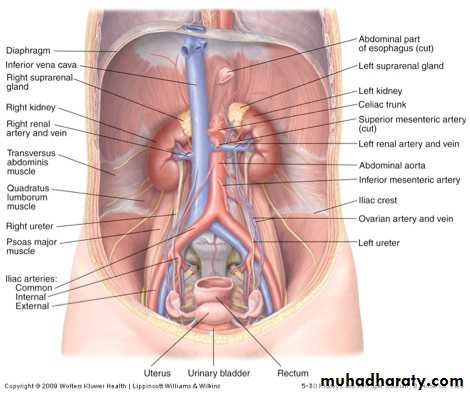
Uretero-vaginal fistula:
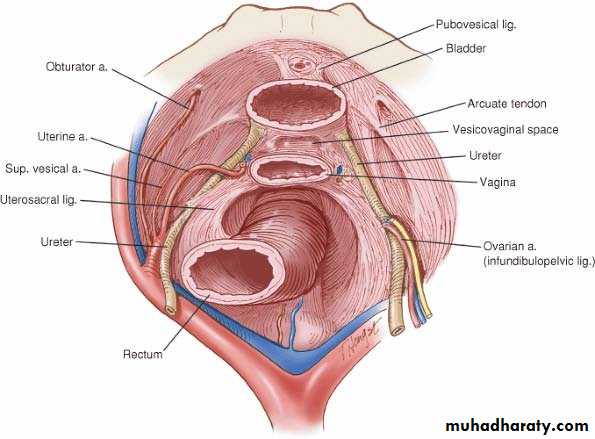
The ureter may be damaged at the pelvic brim when the infundibulopelvic ligament is being cut and tied during oopphorectomy.More commonly it is damaged lower down in its course during abdominal or vaginal hysterectomy when the uterine artery and transverse cervical ligament are clamped or divided.
Fibromyoma which extends into the base of the broad ligament may displace the ureter from its place making it vulnerable to injury.
Also in conditions where there is interference with ureter blood supply when it is dissected out during Wertheim’s hysterectomy especially when the patient has received previous chemotherapy, fistula may occur.
Early diagnosis is essential when in the postoperative period the patient after hysterectomy will complain from pyrexia and renal pain (when the ureter has been tied, acute pain and tenderness of the kidney is immediately obvious).
When the ureter has been cut, the escape of urine into the extra peritoneal tissues of the pelvis may cause high temperature and looks obviously ill. Sometimes large cystic swelling develops without much systemic reaction.
Once the diagnosis is suspected, an intravenous pyelogram will demonstrate the involved ureter (the ureter on the affected site is usually dilated to the site of injury or failure of excretion on that site).
Sometimes the fistula is discovered when the patient passes about half of her urine output from her bladder while leaking urine constantly from the vagina.
If the dignosis is made within 72hours of the operation, an immediate laparotomy is performed otherwise the operation is done electively later.
If ureteric damage is close to the bladder, the cut or tied end is freshened and then re implanted to the bladder. Damage at pelvic brim may call for the use of bladder flap to bridge the distance between the cut end of the ureter and the bladder.
When implantation of the cut end of the ureter is not possible, ureteric anastomosis may be attempted, the two ends being sewn together over a ureteric catheter threaded up towards the kidney and down into the bladder. The ureter will usually heal but there is risk of future stricture at the site of anastomosis.