Woman Imaging
Qais A. Altimimy, DMRD, CABMS-RAD.Lecturer, Radiology
2016
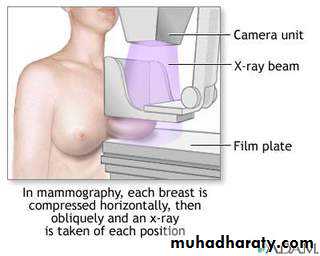
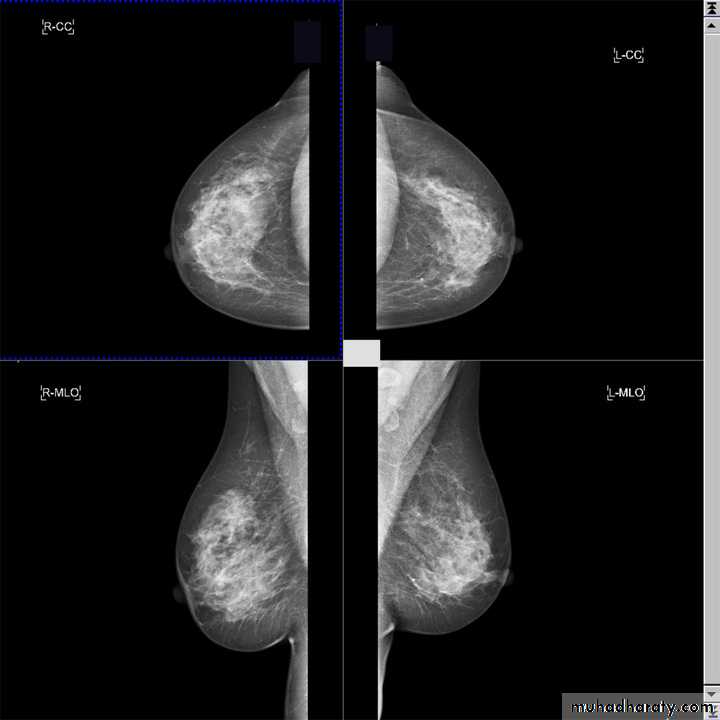
Alkindy college of medicine, university of BaghdadThe two standard views are :.
craniocaudal view (CC view)mediolateral oblique view (MLO view)
Mammography is a dedicated radiographic technique for imaging the breast.
Types of mammographyIn general terms, there are two types of mammography: screening and diagnostic.
Mammography differs significantly in many respects from the rest of diagnostic imaging.
Mammography
:Adequate craniocaudal views
all glandular tissue identifiednipple in profile
nipple in midline of image
images symmetric
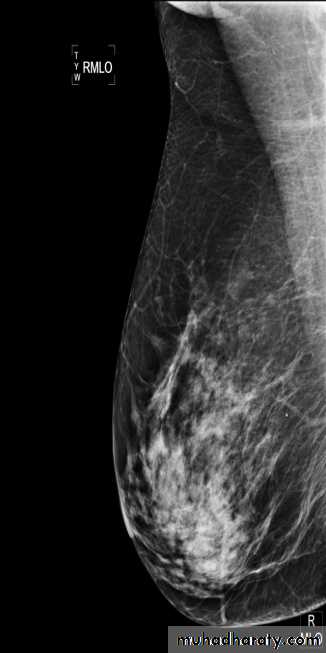
Adequate medio-lateral oblique views
pectoral shadow seen down to level of nipple or lowerinframammary fold well seen
nipple in profile
images symmetric
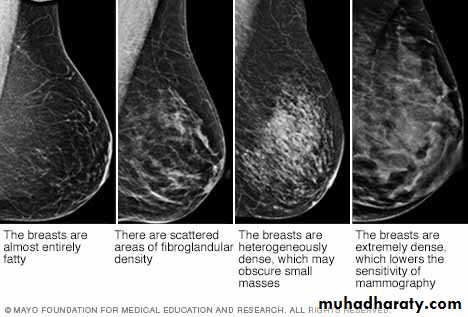
Essentially, breast density is a comparison of the relative amounts of fat versus fibroglandular tissues in the breast.
There are four levels of breast density in keeping with relative increases in the amount of levels of fibro-glandular tissue. These are:
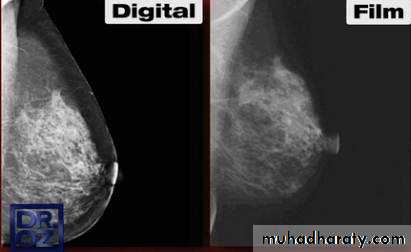
A digital mammography system tends to require a lower radiation dose than film screen mammography for the same image quality. Digital detector converts the X-ray photons to an electronic signal, which is further processed and displayed as a gray scale image. This image can either be electronically sent to a viewing station and displayed on a high-resolution monitor or printed and read on luminant-view boxes similar to how the film screen mammograms are read.
The digital system provides greater contrast resolution and thus better visualization of skin, peripheral breast tissue, and dense breasts. Besides this, it allows for changes in zoom, contrast, and brightness, which increase the ability to detect subtle abnormalities.
A film screen system does not offer such facilities and also tends to suffer from artifacts during processing and storage. These deficiencies are, however, partly compensated for by the advantage of a higher spatial resolution in film screens as compared to digital systems. However, despite of all these technological differences, studies have shown that the overall diagnostic accuracy was similar with these 2 modalities except for premenopausal and perimenopausal women in whom digital mammography was found to be more accurate. This is at least partly because digital mammography is relatively more sensitive than film mammography in detecting cancer in dense breasts.
Breast ultrasound is an important modality in breast imaging. It is the usual initial breast imaging modality in those under 30 years of age in many countries.
Indications for breast US:
1. to evaluate a young (usually under 30 years of age) or pregnant patient who is symptomatic
2. to evaluate a palpable lump with negative or equivocal mammographic findings
3. can help to distinguish between benign vs malignant characters
4. for guiding biopsy
5. for evaluation of breast implants for rupture
US characters of malignant breast mass
• 1.spiculation: alternate hypo-hyperechoic lines radiating perpendicularly from surface of nodules
• 2.deeper (taller) than wide
• 3.microlobulations: small lobulations 1-2 mm on the surface; risk of malignancy
• rises with increasing numbers
4.angular margins: part of the lesion have sharpe corner
5.thick hyperechoic halo
6.markedly hypoechoic nodule
7.sonographic posterior acoustic shadowing
8.punctate calcifications: which usually do not shadow
9.heterogeneous echotexture
10.not compressible
11.increased vascularity ( by Doppler )
12.associated axially LNP
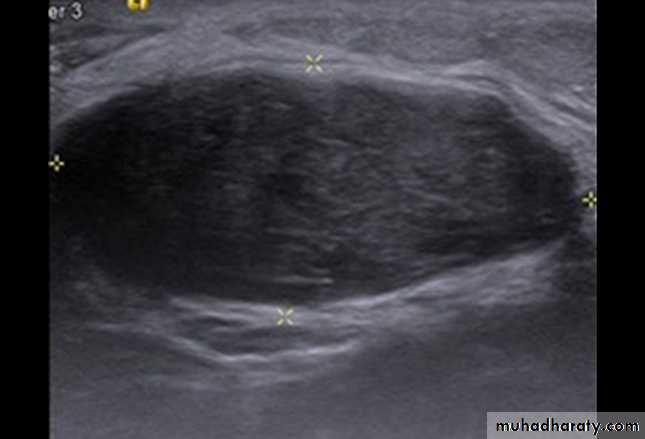
US characteristics of benign breast mass
1.well circumscribed, hyperechoic tissue2.wider than deep
3.gently curving smooth lobulations (<3 in no.)
4.thin echogenic pseudocapsule
5.sonographic posterior acoustic enhancement
6.homogeneous echotexture
7.compressible
8.normal/poor vascularity ( by Doppler )
9. no associated axially LNP
What is a BI-RADS score?
Doctors use a standard system to describe mammogram findings and results. This system (called the Breast Imaging Reporting And Data System or BI-RADS) sorts the results into categories numbered 0 through 6.By sorting the results into these categories, doctors all over the country can describe what they find on a mammogram using the same words and terms. This makes accurately communicating about these test results and following up after the tests much easier.
Category
DefinitionWhat it means
0
Additional imaging evaluation and/or comparison to prior mammograms is needed.
This means the radiologist may have seen a possible abnormality, but it was not clear and you will need more tests, such as the use of spot compression, magnified views, special mammogram views, or ultrasound. Or compare your new mammogram with older ones to see if there have been changes in the area over time.
1
Negative
There’s no significant abnormality to report.
2
Benign (non-cancerous) finding
to describe a finding known to be benign, such as benign calcifications, lymph nodes in the breast, or calcified fibroadenomas.
3
Probably benign finding – Follow-up in a short time frame is suggested
The findings in this category have a very high chance (greater than 98%) of being benign (not cancer). The findings are not expected to change over time. you will likely need follow-up with repeat imaging in 6 months and regularly after that until the finding is known to be stable (usually at least 2 years). .
4
Suspicious abnormality – Biopsy should be considered
The findings in this category can have a wide range of suspicion levels (3-95%). The biopsy is recommended. We can divide this category further:
4A: Finding with a low suspicion of being cancer
4B: Finding with an intermediate suspicion of being cancer
4C: Finding of moderate concern of being cancer, but not as high as Category 5
5
Highly suggestive of malignancy – Appropriate action should be taken
The findings look like cancer and have a high chance (at least 95%) of being cancer. Biopsy is very strongly recommended.
6
Known biopsy-proven malignancy – Appropriate action should be taken
This category is only used for findings on a mammogram that have already been shown to be cancer by a previous biopsy. Mammograms may be used in this way to see how well the cancer is responding to treatment.
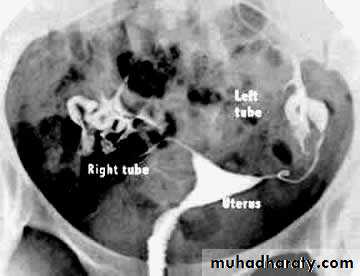
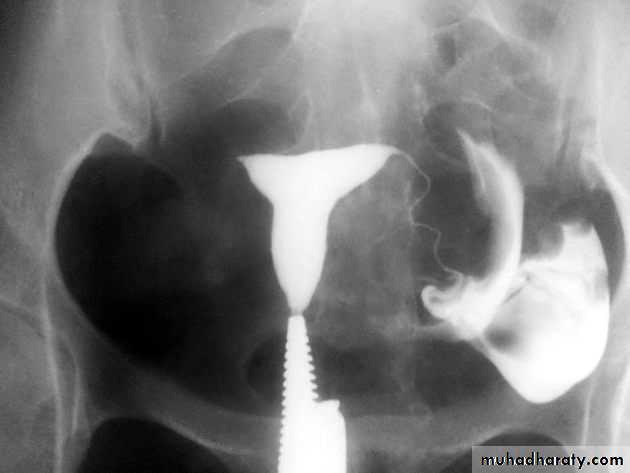
Hysterosalpingogram
Hysterosalpingogram (HSG) is a fluoroscopic examination of the uterus and theFallopian tubes, most commonly used in the investigation of infertility or recurrent spontaneous abortions.
Indications
Infertility to assess uterine morphology and tubal patency.Contraindications
pregnancyactive pelvic infection
recent uterine or tubal surgery
Complications
Common but self limiting: abdominal cramping, PV spotting & venous extravasations
Rare but serious: pelvic infection, contrast reaction
Detectable pathology
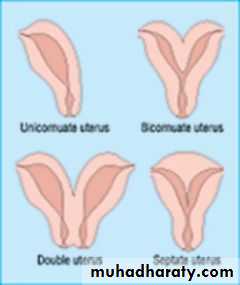
Conditions which may be detected with HSG include:Uterine
uterine congenital anomaliessubmucosal uterine fibroids
uterine malignancy
adenomyosis
intrauterine adhesions
uterine (endometrial) polyps
Tubal
obliteration of fallopian tubes : usually secondary to previous pelvic inflammation. It must be differentiated from incomplete tubal opacification due to tubal spasm, or underfilling of the uterus with contrast
tubal polyps
tubal malignancy
hydrosalpinx
salpingitis isthmica nodosa (SIN)
tubal spasm : can be physiological
HSG : RT corner is blocked
HSG showing a normal uterus and blocked tubes No "spill" of dye is seen at the ends of the tubes Both tubes are slightly dilated and fluid filled - hydrosalpinxHSG : fibroid is pushing in to the uterus cavity
HSG : bicornuate uterus