1
4
th
stage
Medicine
Lec-
. د
15/5/2016
MECHANISM OF TOXICITY:
Overdose (adult 7.5 - 10gm and children 150 – 200mg/kg), leads to exhausting glutathione
reserves; a substance that is very important for cellular metabolism especially in liver.
Clinical course
in first few hours after ingestion: Patients may be asymptomatic or report anorexia, nausea
or vomiting, and malaise.
In next 1-3 days(early hepatotoxicity): patients generally develop RUQ abdominal pain with
increasing nausea and vomiting.
In 3-4 days after ingestion (severe hepatic damage: the most dangerous period): Hepatic
necrosis and dysfunction are associated with jaundice, coagulopathy, hypoglycemia, and
hepatic encephalopathy .
Acute renal failure develops in some critically ill patients. Death from multi-organ failure may
occur.
TREATMENT
Approach Considerations
1. Initial appropriate supportive care is essential in acetaminophen (paracetamol) poisoning.
Immediate assessment of the patient's airway, breathing, and fluid status (ie, ABCs) is critical
before treatment for suspected acetaminophen overdose is initiated. In addition, assessing
for other potential life-threatening co-ingestions (eg, salicylate) is very important.
2. Administer activated charcoal (AC) if the patient has a stable mental and clinical status and
presents to the emergency department within 1 hour of ingestion.
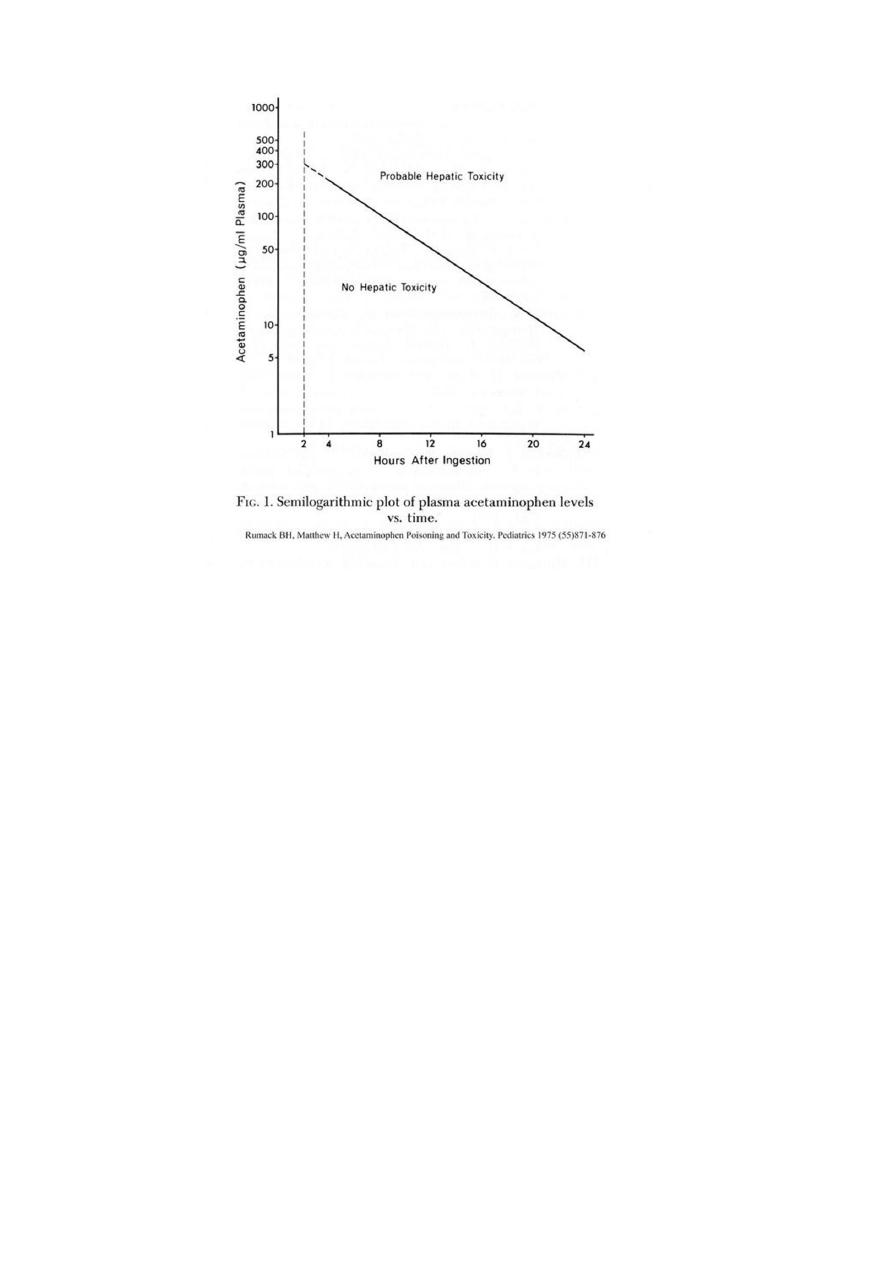
2. Draw a 4-hourly serum acetaminophen concentration to determine the risk for
hepatotoxicity, plot this value using the R-M nomogram. Start 4 hours after ingestion.
2
3. Patients with acetaminophen levels below the “possible” line for hepatotoxicity on the
Rumack-Matthew nomogram may be discharged home after they are medically cleared. If
the ingestion occurred with intent to do self-harm, a thorough psychosocial, psychological
and/or psychiatric evaluation is indicated before the patient can be discharged safely from
the medical care facility.
4. Admit patients with acetaminophen plasma levels above the possible line on the Rumack-
Matthew nomogram for treatment with antidote: N -acetylcysteine (NAC), most effective in
first 8 hours of ingestion and usually by IV infusion. Rarely may cause allergy.
5. Treat patients with evidence of hepatic failure, metabolic acidosis, coagulopathy, and/or
encephalopathy in an intensive care unit (ICU). Transfer patients with evidence of clinically
significant hepatotoxicity to a medical facility with intensive care support and organ
transplant services.
Criteria for liver transplantation include the following:
•Metabolic acidosis
•Renal failure
•Coagulopathy
•Encephalopathy

3
Organophosphorus insecticides and nerve agents
Organophosphorus (OP) compounds are widely used as pesticides, especially in developing
countries. Nerve agents developed for chemical warfare are derived from OP insecticides but
are much more toxic. The toxicology and management of nerve agent and pesticide poisoning
are similar.
Summary:
inactivating the enzyme acetylcholinesterase by OP compounds leading to the accumulation
of acetylcholine (ACh) in cholinergic synapses and presences of many cholinergic symptoms
like excessive body secretions, abdominal colic, diarrhea, dyspnea (pulmonary oedema like,
etc. Treatment consists of giving anticholinergic drugs like atropine and OXIMES which cause
cholinestrase recovery.
Features of Acute cholinergic syndrome
The acute cholinergic syndrome usually starts within a few minutes of exposure. Nicotinic or
muscarinic features may be present . Vomiting and profuse diarrhoea are typical following
oral ingestion.
Bronchoconstriction, bronchorrhoea and salivation may cause severe respiratory
compromise.
Miosis is characteristic and the presence of muscle fasciculation strongly suggests the
diagnosis, although this feature is often absent, even in serious poisoning. Subsequently, the
patient may develop generalised flaccid paralysis which can affect respiratory and ocular
muscles and result in respiratory failure. Ataxia, coma and convulsions, cardiac arrhythmia,
pancreatitis may develop.
Management
1. Supportive:
The airway should be cleared of excessive secretions, breathing and
circulation assessed, high-flow oxygen administered and intravenous access obtained. In the
event of external contamination, further exposure should be prevented, contaminated
clothing and contact lenses removed, the skin washed with soap and water, and the eyes
irrigated. Gastric lavage or activated charcoal may be considered if the patient presents
within 1 hour of ingestion. Convulsions should be treated.The ECG, oxygen saturation, blood
gases, temperature, urea and electrolytes, amylase andglucose should be monitored closely.
4
2. Specific (atropine):
Early use of sufficient doses of atropine is potentially life-saving in
patients with severe toxicity. Atropine reverses ACh-induced bronchospasm,
bronchorrhoea,bradycardia and hypotension. atropine should be administered in doses of
0.6–2 mg IV, repeated every 10–25 mins until secretions are controlled, the skin is dry
and there is a sinus tachycardia.
Large doses may be needed but excessive doses may cause anticholinergic effects.
3. Specific (Oximes):
In patients requiring atropine, an oxime such as pralidoxime if
available, should also be administered, as this may reverse or prevent muscle weakness,
convulsions or coma, especially if given rapidly after exposure. The pralidoxime dose for an
adult is 2 g IV over 4 mins, repeated 4–6 times daily.
Note: This is less important than atropine and may causes some problems.
4. Rarely Benzodiazepines may be used to reduce agitation and fasciculations, treat
convulsions and sedate patients during mechanical ventilation but should be given with
caution and after the starting of atropine .
Tricyclic antidepressants
Tricyclic antidepressants (TCAs) are used frequently in overdose and carry a high morbidity
and mortality relating to their sodium channel-blocking, anticholinergic and α
adrenoceptor-blocking effects.
Clinical features:
Anticholinergic effects are common. Life-threatening complications are frequent, including
convulsions, coma, arrhythmias (ventricular tachycardia, ventricular fibrillation and, less
commonly, heart block) and hypotension, which results from inappropriate vasodilatation
or impaired myocardial contractility.
Serious complications appear to be more common with
Tricyclic anti-depressant: dosulepin (an old drug) and amitriptyline.

5
Management
1. Activated charcoal should be administered if the patient
presents within 1 hour.
2. All patients with possible TCA overdose should have a 12-lead ECG and ongoing cardiac
monitoring for at least 6 hours. Prolongation of the QRS interval (especially if > 0.16 s)
indicates severe sodium channel blockade and is associated with an increased risk of
arrhythmia. QT interval prolongation may also occur.
3. Arterial blood gases should be measured in suspected severe poisoning.
4. Intravenous sodium bicarbonate (50 mL of 8.4% solution) should be administered and
repeated to correct pH in significant acidosis and cardiac arrhythmia.
5. Hypoxia and electrolyte abnormalities should also be corrected.
6. Anti-arrhythmic drugs should only be given on specialist advice.
7. Prolonged convulsions should be treated with intravenous benzodiazepines.
