Preoperative Assessment, Preparation and Premedication
Dr.Ali Hadihttp://telemed.shams.edu.eg/moodle6
What is Anesthesia ?
Reversible controlled loss of consciousnessAnalgesia
AreflexiaMuscle relaxation
Preoperative Evaluation
Anesthetic drugs and techniques have profound effects on human physiology. Hence, a focused review of all major organ systems should be completed prior to surgery.Goals of the preoperative evaluation is to ensure that the patient is in the best (or optimal) condition.
Patients with unstable symptoms should be postponed for optimization prior to elective surgery.
Problem Identification
Risk AssessmentPreoperative Preparation
Plan of Anesthetic TechniqueSteps of the preoperative visit :
• I. Problem Identification
Cardiovascular : hypertension ; ischemic , valvular or congenital heart disease; CHF or cardiomyopathy, , arrhythmiasRespiratory : smoking; COPD; restrictive lung disease; altered control of breathing (obstructive sleep apnea, CNS disorders, etc.)
Neuromuscular : raised ICP ; TIA's or CVA's; seizures; spinal cord Injury; disorders of NM junction e.g myasthenia gravis, muscular dystrophies ,MH
Endocrlne : DM; thyroid disease; pheochromocytoma; steroid therapy
GI - Hepatic : hepatic disease; gastresophageal reflux
Renal : renal failureHematologic : anemias; coagulopathies
Elderly , Children, PregnancyMedications and Allergies
Prior AnestheticsRelated to Surgery : significant blood loss; respiratory compromise; positioning
I. Problem Identificationthrough :
History (including a review of the patient's chart)Physical examination
laboratory investigation
Physical Examination:General & Local examination
Should focus on evaluation of :
• Upper airway• Respiratory system
• Cardiovascular system
• other systems’ problems identified from the history
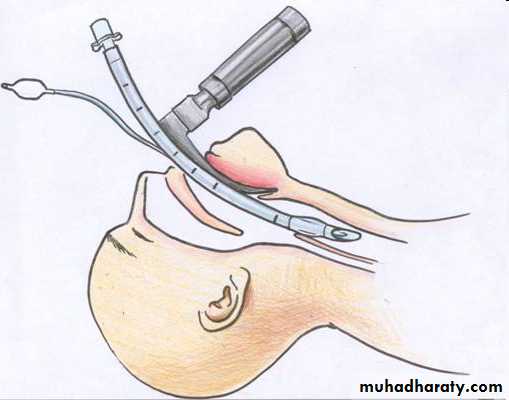
Predictors of difficult intubation ( 4 M )
MallampatiMeasurements 3-3-2-1 or 1-2-3-3 Patient ‘s fingers
Movement of the Neck
Malformations of the Skull
Teeth
Obstruction
Pathology
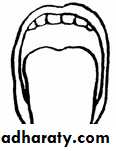
Class I = visualize the soft palate, fauces, uvula, anterior and posterior pillars.
Class II = visualize the soft palate, fauces and uvula.
Class III = visualize the soft palate and the baseof the uvula.
Class IV = soft palate is not visible at all.
MallampatiMeasurements 3-3-2-1
3 Fingers Mouth Opening3 Fingers Hypomental Distance. (3 Fingers between the tip
of the jaw and the beginning of the neck (under the chin)
2 Fingers between the thyroid notch and the floor of the mandible (top of the neck)
1 Finger Lower Jaw Anterior sublaxation
Movement of the Neck
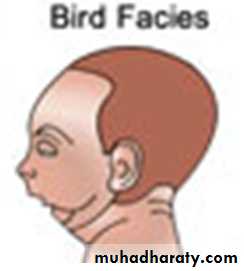
Skull (Hydro and Microcephalus)
Teeth (Buck, protruded, & loose teeth. Macro and Micro mandibles)Obstruction (obesity, short Bull Neck & swellings around the head and neck)
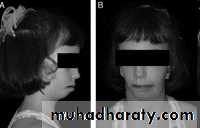
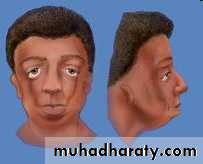
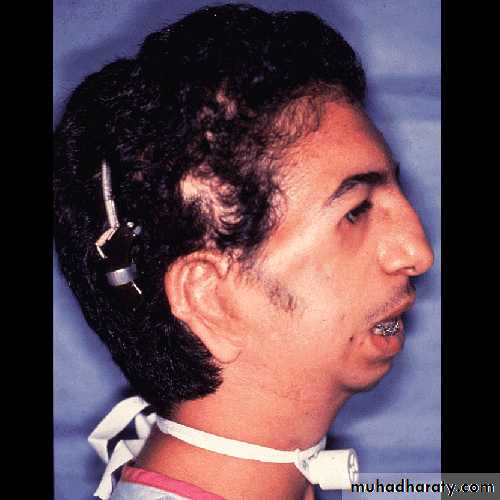
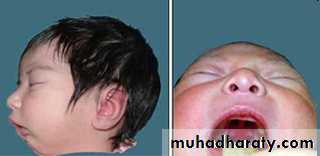
Pathology (Craniofacial abnormalities & Syndromes e.g. Treacher Collins, Goldenhar's, Pierre Robin syndromes)
“Patients with an abnormal airway (including Class III or IV airway) should be considered at higher risk “.
.
Malformation of the skull
Treacher Collins (mandibulofacial dysostosis)
Pierre Robin
( hypertelorism; and external and middle ear deformities)Goldenhar's
(oculoauriculovertebral dysplasia)Preoperative Laboratory Testing:
only if indicated from the preoperative history and physical examination."Routine or standing" pre operative tests should be discouraged
-CBC anticipated significant blood loss, suspected hematological disorder (eg.anemia, thalassemia, SCD), or recent chemotherapy.
-Electrolytes diuretics, chemotherapy, renal or adrenal disorders
-ECG age >50 yrs ,history of cardiac disease, hypertension, peripheral vascular disease, DM, renal, thyroid or metabolic disease.-Chest X-rays prior cardiothoracic procedures ,COPD, asthma, a change in respiratory symptoms in the past six months.
-Urine analysis DM, renal disease or recent UTI.
-tests for different systems according to history and examination
II. Risk Assessment
Components for evaluating perioperative risk:patient's medical condition preoperatively
extent of the surgical procedure
risk from the anesthetic
“Most of the work, however, addresses the operative risk
according to the patient's preoperative medical status”medical status
mortalityASA I
normal healthy patient without organic, biochemical, or psychiatric disease
0.06-0.08%
ASA II
mild systemic disease with no significant impact on daily activity e.g. mild diabetes, controlled hypertension, obesity .
Unlikely to have an impact
• 0.27-0.4%
ASA III
severe systemic disease that limits activity e.g. angina, COPD, prior myocardial infarction
Probable impact
1.8-4.3%
ASA IV
an incapacitating disease that is a constant threat to life e.g. CHF, unstable angina, renal failure ,acute MI, respiratory failure requiring mechanical ventilation
Major impact
7.8-23%
ASA V
moribund patient not expected to survive 24 hours e.g. ruptured aneurysm
9.4-51%
ASA VI
brain-dead patient whose organs are being harvested
ASA Physical Status Classification System
For emergent operations, you have to add the letter ‘E’ after the classification.
III. Preoperative Preparation
• Anesthetic indications:• -Anxiolysis, sedation and amnesia. e.g. benzodiazepine(diazepam ,lorazepam)
• -Analgesia e.g narcotics
• -Drying of airway secretions e.g atropine,glycopyrrolate,scopolamine
-Reduction of anesthetic requirements ,Facilitation of smooth induction
• -Patients at risk for GE reflux :ranitidine ,metoclopramide , sodium citrate
• Surgical indications:
• -Antibiotic prophylaxis for infective endocarditis.
• -Prophylaxis against DVT for high risk patients : low-dose heparin or aspirin
• intermittent calf compression, or warfarin.
• Co-existing Disease indications:
Some medications should be continued on the day of surgery e,g B blockers, thyroxine. Others are stopped e.g oral hypoglycemics and antidepressants .
• Steroids within the last six months may require supplemental steroids
• MEDICATION
• ADMINISTRATION ROUTE• DOSE (mg)
• Lorazepam
• Oral, IV
• 0.5–4
• Midazolam
• IV
• Titration of 1.0–2.5-mg doses
• Fentanyl
• IV
• Titration of 25–100–µg doses
• Morphine
• IV
• Titration of 1.0–2.5-mg doses
• Meperidine
• IV
• Titration of 10–25-mg doses
• Cimetidine
• Oral, IV
• 150–300
• Ranitidine
• Oral
• 50–200
• Metoclopramide
• IV
• 5–10
• Atropine
• IV
• 0.3–0.4
• Glycopyrrolate
• IV
• 0.1–0.2
• Scopolamine
• IV
• 0.1–0.4
Common Preoperative Medications, Doses, and Administration Routes (adult)
• INGESTED MATERIAL
• MINIMUM FASTING PERIOD, APPLIED TO ALL AGES (hr)• Clear liquids
• 2
• Breast milk
• 4
• Infant formula
• 6
• Nonhuman milk
• 6
• Light meal (toast and clear liquids)
• 6
Fasting Recommendations
IV. Plan of Anesthetic Technique
• Is the patient's condition optimal?• Are there any problems which require consultation or special tests? “Please assess and advise “
• 3. Is there an alternative procedure which may be more appropriate?
4. What are the plans for postoperative management of the patient?