
Blood Diseases
Dr. Salma
“ Childhood
Haemolytic Anaemia ”
Total Lec: 39

Childhood
Hemolytic Anemia
Dr. Salma AL-Hadad
Objectives
•
Describe the presentation
& management of G6PD ,AIHA ,Thalassemia major
& Sickle cell
disease.
•
Describe the presentation
& management of Bone marrow failure
Case scenario
•
7 years old boy ,otherwise healthy presented with sudden pallor ,malaise,
fatigue, he mentioned that he passed tea color urine .His mother noticed that
he is jaundiced too.
•
He was pale, jaundiced ,inactive, PR 120 beats/minute, no organomegaly .
Action
•
What is the differential diagnosis?
•
What investigation will you order?
•
What is your action?
G6PD Deficiency
•
Most common RBC enzyme defect ;
•
Sex linked ,affecting males
& carried by females who show half normal RBC
G6PD values .
•
Associated with potentially life-threatening hemolytic disease because of
severe deficiency .
•
Results from oxidative damage to RBCs as a consequence of the loss of the
protective effect of the enzyme G6PD, so the cells can’t convert the oxidized
substrate to a reduced state .
Clinical presentations
I .Neonatal jaundice :Jaundice usually appears by age 1-4 days .
II .Acute hemolytic anemia beyond the neonatal period :
•
Typically; most patients are asymptomatic until exposed to an exciting agent
(such as oxidative drugs or chemicals, infection, or ingestion of fava beans.(
•
The onset of hemolysis usually is within 24 to 48 hours of exposure .
•
Non specific symptoms; acute abdominal pain, vomiting or diarrhea ,
•
Hemoglobinuria (cola-colored urine) ----- jaundice------symptoms of anemia
such as lethargy and irritability----cardiovascular decompensation may occur .
•
Most acute hemolytic episodes are mild
& self-limiting, even if continuing
exposure, because there is an increased level of enzymes in the remaining
younger population of cells ,anemia usually resolves in 3 to 6 weeks .
•
Possible Complications ;renal failure or death following a severe hemolytic
event .
•
Outside of these episodes; no evidence of chronic hemolysis exists .
•
Chronic hemolysis (congenital non-spherocytic hemolytic anemia) is rare
Diagnosis
I. During an attack, the following lab. findings are present :
1. Anemia
2. Peripheral Blood film (smear) shows ;
§
Normochromic normocytic anemia of varying degrees
§
Small cells (poikilocytes), some of which are spherocytic or
fragmented .
§
Characteristic findings include
“ bite” cells ,
3. Reticulocytosis .
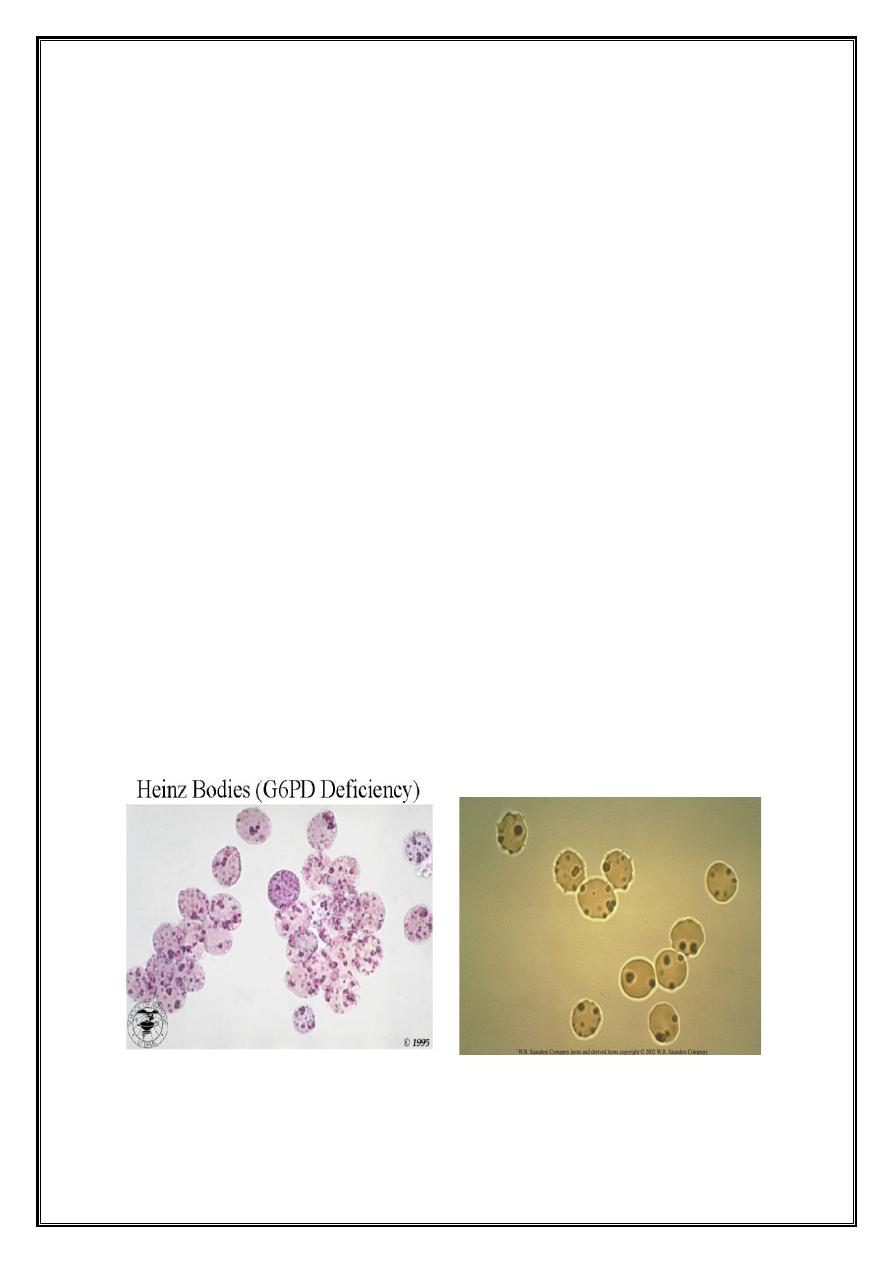
4. Heinz bodies (inclusion bodies) detected by using special
(supravital) stains
5. There is evidence of intravascular hemolysis ;
§
Serum haptoglobin is reduced ,
§
Increased unconjugated hyperbilirubinemia ,
§
In severe cases, hemoglobinemia and hemoglobinuria .
Hienz bodies in G6PD deficiency
II. G-6-PD enzyme deficiency can be detected using several screening tests .
III. The blood count is normal between attacks
Treatment
Ø
During the attack :
1. Remove offending drug
& treat any underlying infection
2. Brisk hydration to ensure adequate urine output that will prevent
clogging of renal tubules .
3. Transfusion may be necessary in severe hemolysis .
Ø
Teaching to avoid oxidant drugs, chemicals & ,fava beans
Auto Immune hemolytic
anemia (AIHA(
•
Production of Antibodies against an individual’s own RBC membrane Antigens,
which leads to hemolysis .
•
Acquired form of hemolysis with a defect arising outside the red cell .
•
Divided into ‘warm ’and ‘cold ’types depending on whether the antibody
reacts better with red cells at 37°c or 4°c .
•
The peak incidence occurs in the preschool age group .
•
The hemolysis is largely extravascular , usually involves IgG ,and occurs
primarily in the liver and spleen .
Clinical features
•
Pallor ,
•
Jaundice ,
•
Non specific: lethargy ,abdominal pain, or low-grade fever .
•
If hemolysis is severe ,the urine may be dark .
•
Hyperdynamic circulation
•
Enlarged spleen and liver .
Laboratory findings
I. Anemia; Hemoglobin level—very low
II. Peripheral blood smear ;prominent spherocytes ,polychromasia, macrocytes ,
autoagglutination (antibodies best detected at 37°C)
III. Reticulocytosis—common
IV. Evidence of hemolysis :
1. Hyperbilirubinemia
2. Haptoglobin level—markedly decreased
3. Hemoglobinuria
4. Increased urinary urobilinogen
Direct coomb’s test—positive
Treatment
Most patients who have AIHA exhibit mild anemia of limited duration and ,
therefore ,do not need therapy .
I. Compensated hemolysis
–
observation and folic acid at an oral dose
1 mg/day
II. Decompensated hemolysis (definitive therapy depends on the cause) :
Ø
Steroid therapy
Ø
Immunoglobulins
Ø
Splenectomy
Ø
Blood transfusion: only in life-threatening situations as a temporary solution
while waiting for other modalities to begin working .The "least incompatible”
blood .
Thalassemia syndromes
•
Inherited disorders of Hb synthesis that result from an alteration in the rate of
globin chain production .
•
Their clinical severity widely varies, ranging from asymptomatic forms to
severe or even fatal entities .
B-Thalassemia
I .Thalassemia minor; Deficiency of one beta genes leads to essentially no significant
hemolysis and no unusual signs or symptoms are encountered .
II .Thalassemia major; Deficiency of both genes leads to significant hemolytic
anemia .
III .Thalassemia intermedia is a condition in which the degree of hemolysis is milder
even though the patient may have a deficiency of both beta genes. It is essentially a
descriptive term that refers to minimal or no need for transfusions .
Case Scenario
•
A 7-month old boy brought by family after they noticed a progressive pallor,
with abdominal distension .
•
Feeding history is normal
•
Family history positive for a sibling with B-Thalassemia major
•
O/E pale ,liver
3 cm BCM, spleen 3cm BCM
ß -thalassaemia major
Clinical features
:
• Anemia first becomes apparent between 3-6 months when production of HbF
declines, the infant clinically normal at birth (as fetal Hb does not contain ß
chains) then during first year of life; Progressive anemia will occur .
• Failure to thrive
• Hepatosplenomegaly
& jaundice .
• The severity of this anemia results from a combination of ineffective
erythropoiesis and shortened survival of the red blood cell in circulation .
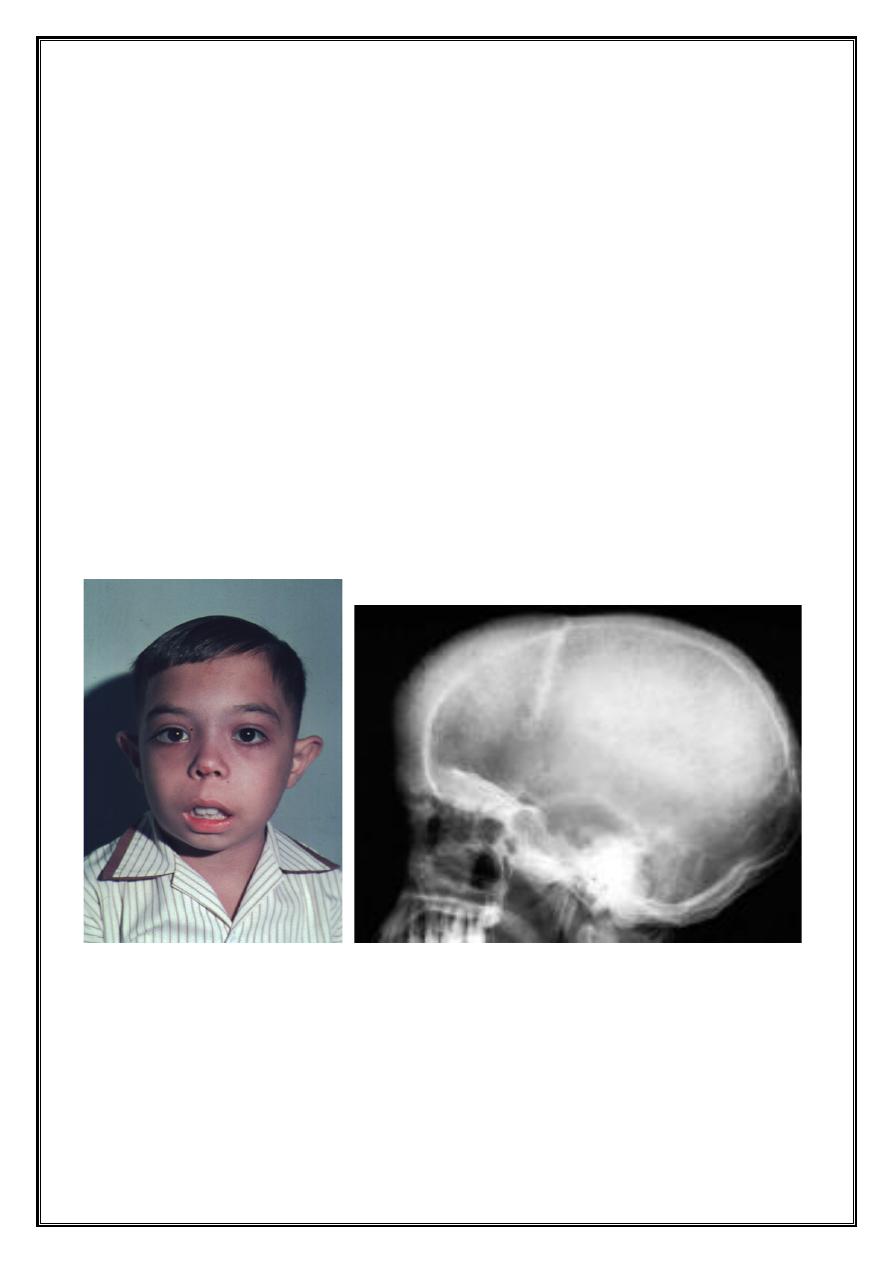
Complications
ü
Hemolysis include expansion of bones leads to thinning of cortex
& tendency
to fractures, bossing of skull
& specific facies with hair-on-end appearance on
x-ray, gallstones
& chronic leg ulcers .
ü
Iron overload caused by repeated transfusion, increased iron absorption due
to ineffective erythropoiesis; The complications of iron overload affect all
organs of the body, including the heart (failure), liver )cirrhosis), thyroid
(hypothyroidism), pancreas (diabetes), and (delayed growth and sexual
maturity) unless chelation therapy is given .
ü
Infections secondary to splenectomy
& blood transfusion transmitted viruses
B-Thalassemia Major
Hair on End Appearance
Laboratory diagnosis
I. Complete blood picture :
1. The Hb level ranges from
2
-
8
g/dL .
2. Microcytic hypochromic anemia .
3. Blood film: nucleated RBCs, target cells, polychromasia,
anisopoikilocytosis, basophilic stippling
4. MCV and MCH are significantly low .
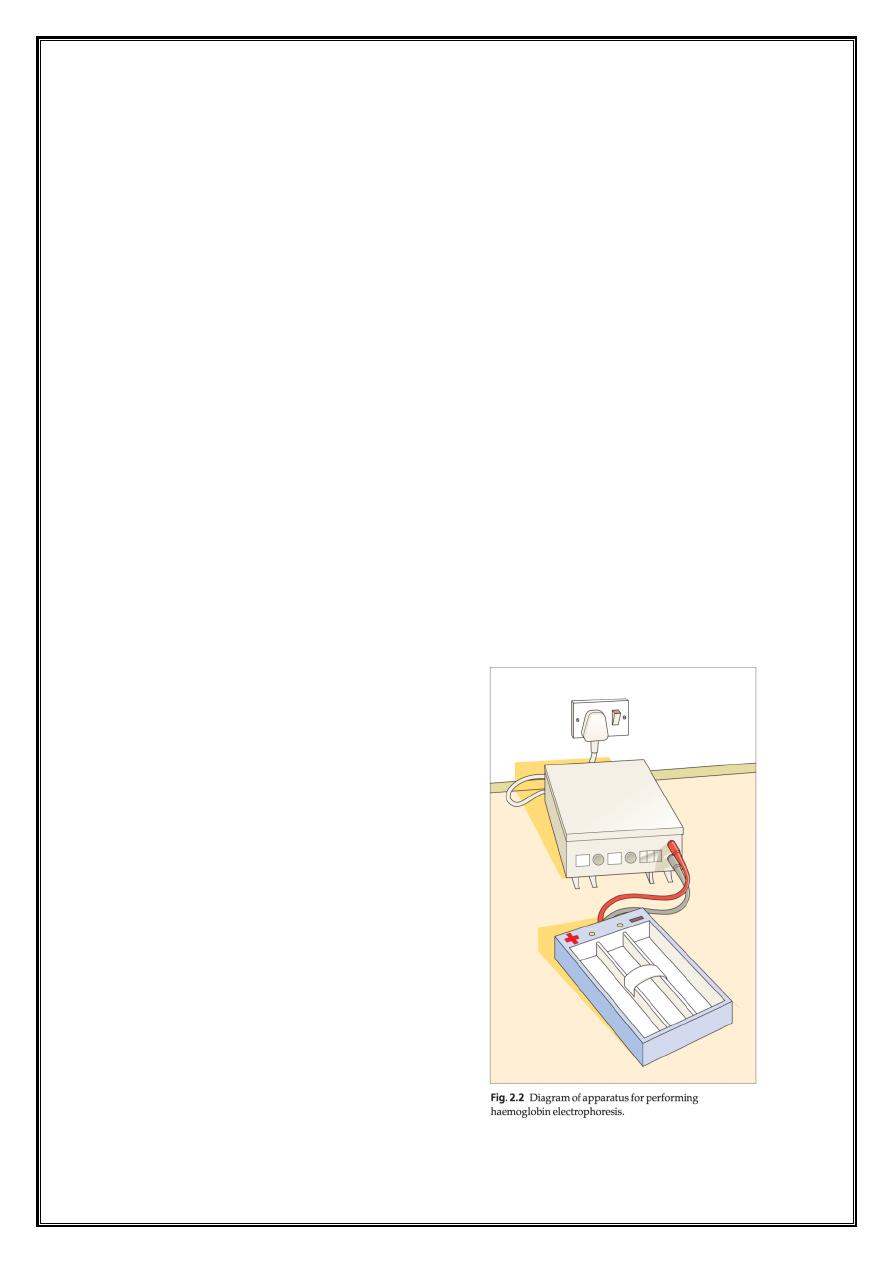
II. Hemoglobin electrophoresis :elevated HbF >50% with variable HbA2 .
III. Evidence of hemolysis: Unconjugated hyperbilirubinaemia .
IV. Iron studies show high serum iron
& ferritin levels
V. DNA analysis. detect deletions
& mutations in the β globin producing genes .
Both parents will have β -thalassemia trait
Diagram of apparatus for performing Hb
electrophoresis
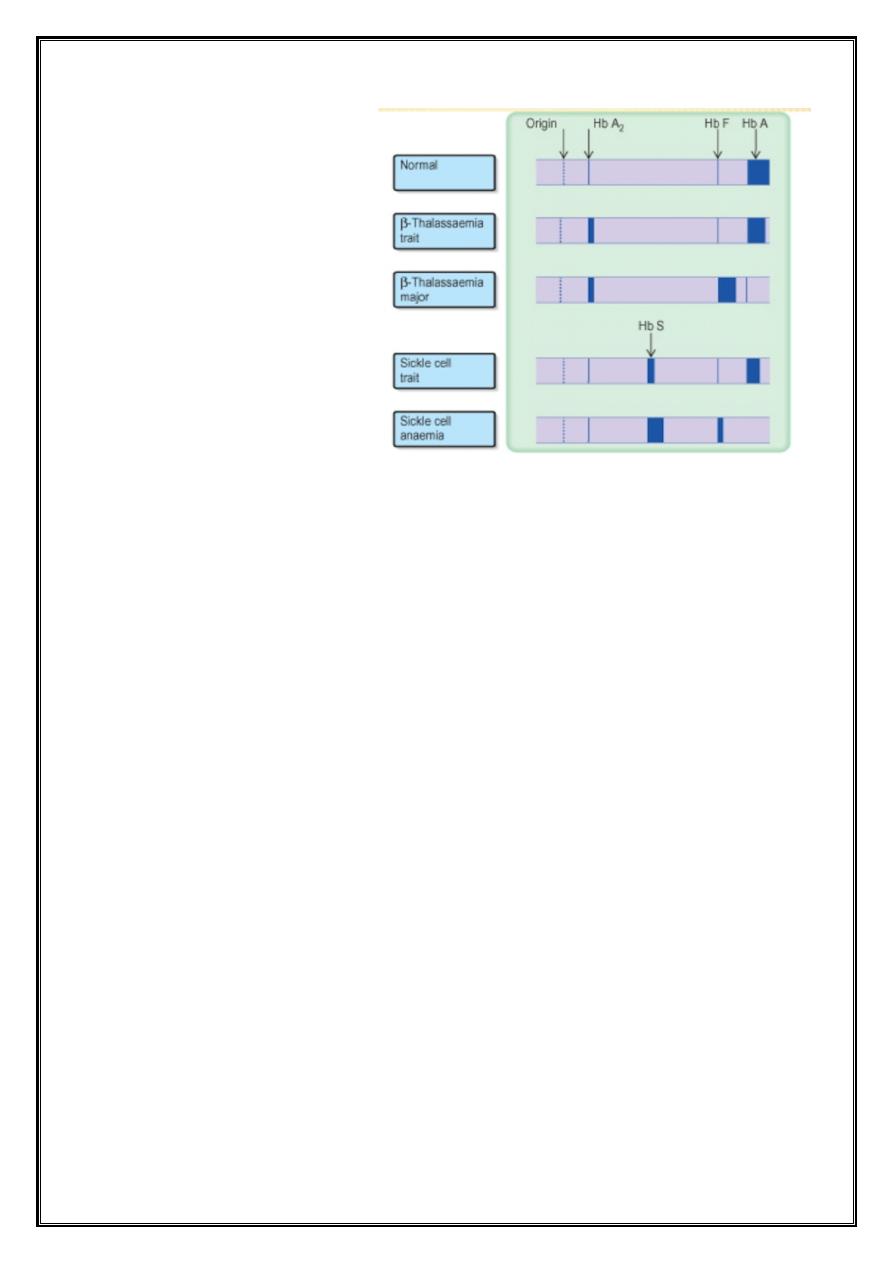
Patterns of Hb electrophoresis
Management
I. Blood transfusion :every 4-6 weeks with fresh, filtered blood to maintain the
Hb
<
10 g /dl
II. Iron chelation :start after 10-15 units of blood ,
1. Desferioxamine by s.c infusion over 8-12 hours, 5-7 days weekly ,
2. Deferasirox (Exjade) a new oral chelator with few side effects
III. Splenectomy ; indicated if the spleen is enlarged substantially or there is
evidence of hypersplenism leading to pancytopenia, it can reduce the
transfusion frequency .
IV. Stem cell transplantation (SCT ,(the probability of survival exceeds 90% .
V. Gene therapy :Stimulation of fetal hemoglobin production and somatic gene
therapy
Sickle Cell Disease
Pathogenesis
:
• In HbS, glutamic acid has been replaced by Valine at the 6
th
amino acid of the
B globin chain
• In the deoxygenated state the red cell loses its normal deformability and
becomes characteristically sickle shaped .
• Hemolysis - because sickle RBCs are too fragile to withstand the mechanical
trauma of circulation
• Occlusion in microvascular circulation caused by distorted, inflexible RBCs
adhering to vascular endothelium
Clinical features
• Most patients have asymptomatic periods alternates with recurrent
symptomatic episodes.
• Vaso-occlusive episodes ;The most common complaint is of pain
& recurrent
episodes may cause irreversible organ damage .
• It can affect nearly all organs .
• It may occur early in the first year of life as
“ dactylitis ”that involves the small
bones of the hands and feet (hand-foot syndrome), but more commonly it
occurs later .
• Most common sites are bones, lungs, spleen, liver, penis, and brain .
• Precipitating events; infection, stress, dehydration, or changes in temperature .
• Transient red blood cell aplastic episode ;Acute infection with Parvovirus B19
is usually associated with red cell aplasia ,fever, and pain .
• Acute sequestration episode ;This is an acute trapping of blood in the spleen
and less frequently in the liver caused by impaired egress of blood out of these
organs due to clogging by sickled cells .
• Infection ;due to functional asplenia which can appear as early as 6 months of
age up to 5 yr of age in most children .
• The risk of infection is highest with encapsulated organisms such as
pneumococci ,Haemophilus influenzae ,meningococci
& Salmonella sp .
• Others; Gall stones ,chronic osteomyelitis, chronic leg ulcers, Lung disease
(acute chest syndrome ,(Renal disease, Recurrent priapism, etc ..
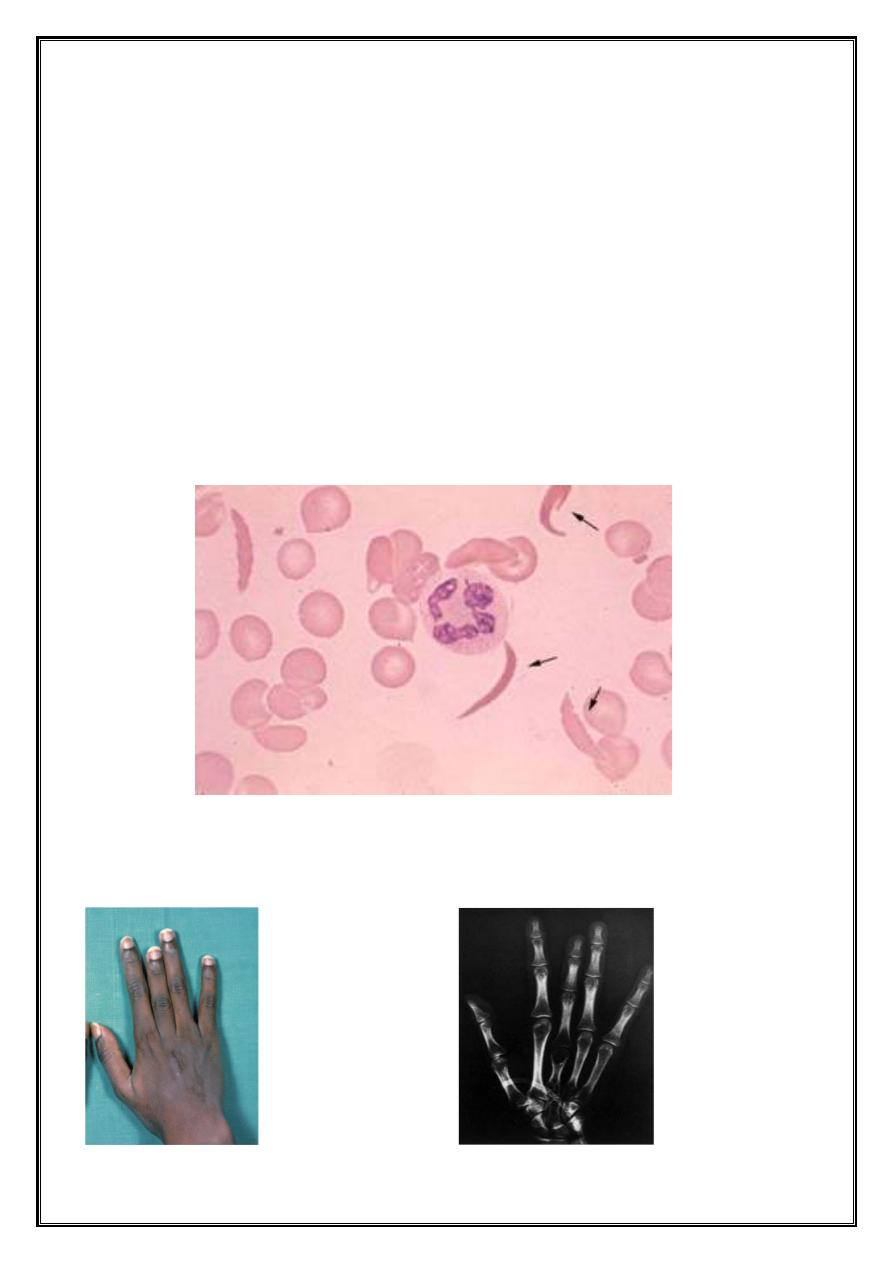
Diagnosis of SCA
•
Blood film :sickled cells, marked poikilocytosis, target cells .
•
Screening tests for sickling: the blood sample is deoxygenated to induce
sickling
•
Hemoglobin electrophoresis :in sickle cell anemia (HbSS)
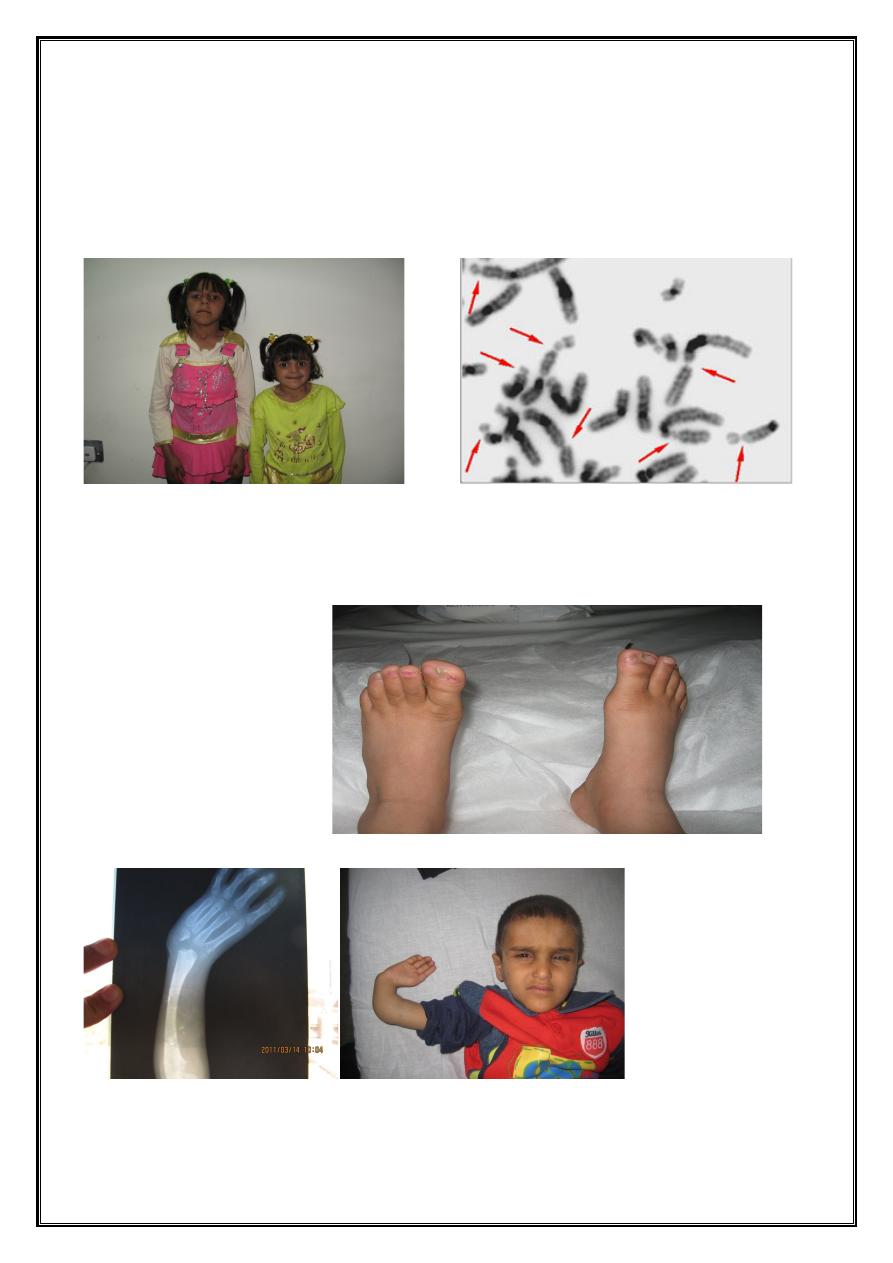
Long term result of dactylitis in sickle cell anemia
Hand of 18-year old boy X-ray of his hand
Treatment
I. Treatment of vaso-occlusive crisis include :
ü
Hydration
ü
Pain control
ü
Empirical antibiotics
ü
Blood transfusion (simple or exchange transfusion (
II. Chronic transfusion therapy .
III. Prophylactic oral penicillin at least until 5 years of age
IV. Routine childhood immunizations
& annual administration of influenza vaccine
are highly recommended .
V. Medical intervention ;Stimulation of increased hemoglobin F production
(hydroxyurea)
VI. Cellular and genetic levels include
1. Stem cell transplant
2. Gene therapy
Bone Marrow Failure
Acquired Bone Marrow
Failure
•
The majority of cases in childhood are
“ idiopathic ”in that no causative agent is
identified
•
Drugs, chemicals, toxins, infectious agents ,radiation, and immune disorders
can result in pancytopenia .
Pathology
& Pathogenesis
•
The hallmark of Aplastic anemia is peripheral pancytopenia ,coupled with
hypoplastic or Aplastic bone marrow
•
Acquired pancytopenia is typically characterized by anemia, leukopenia, and
thrombocytopenia .
Laboratory findings
Bone marrow examination should include both aspiration and a biopsy ,and the
marrow should be carefully evaluated for morphologic features, cellularity, and
cytogenetic findings
Complications
The major complications
of severe pancytopenia are related to the risk of life-
threatening
bleeding from prolonged thrombocytopenia or to infection secondary to
protracted neutropenia
.
Treatment
•
Supportive care coupled with an attempt to treat the underlying marrow
failure
•
For patients with HLA–identical sibling marrow donor ,allogeneic bone
marrow transplantation offers a 90% chance of long-term survival
•
For patients without a sibling donor, the major form of therapy is
immunosuppression , with a response rate of 60–80%
Fanconi’s Anemia
Clinical presentation
:
•
Hyperpigmentation of the trunk, neck, as well as café-au-lait spots and vitiligo.
•
Short stature
& growth failure may be associated with abnormal growth
hormone secretion, or with hypothyroidism .
•
Absent radii and hypoplastic, bifid, or absent thumbs are common.
•
Many patients have a Fanconi “facies ”,including microcephaly, small eyes,
epicanthic folds .
Approximately 10% of patients are mentally retarded.
•
Ectopic ,pelvic, or horseshoe kidneys are detected by imaging
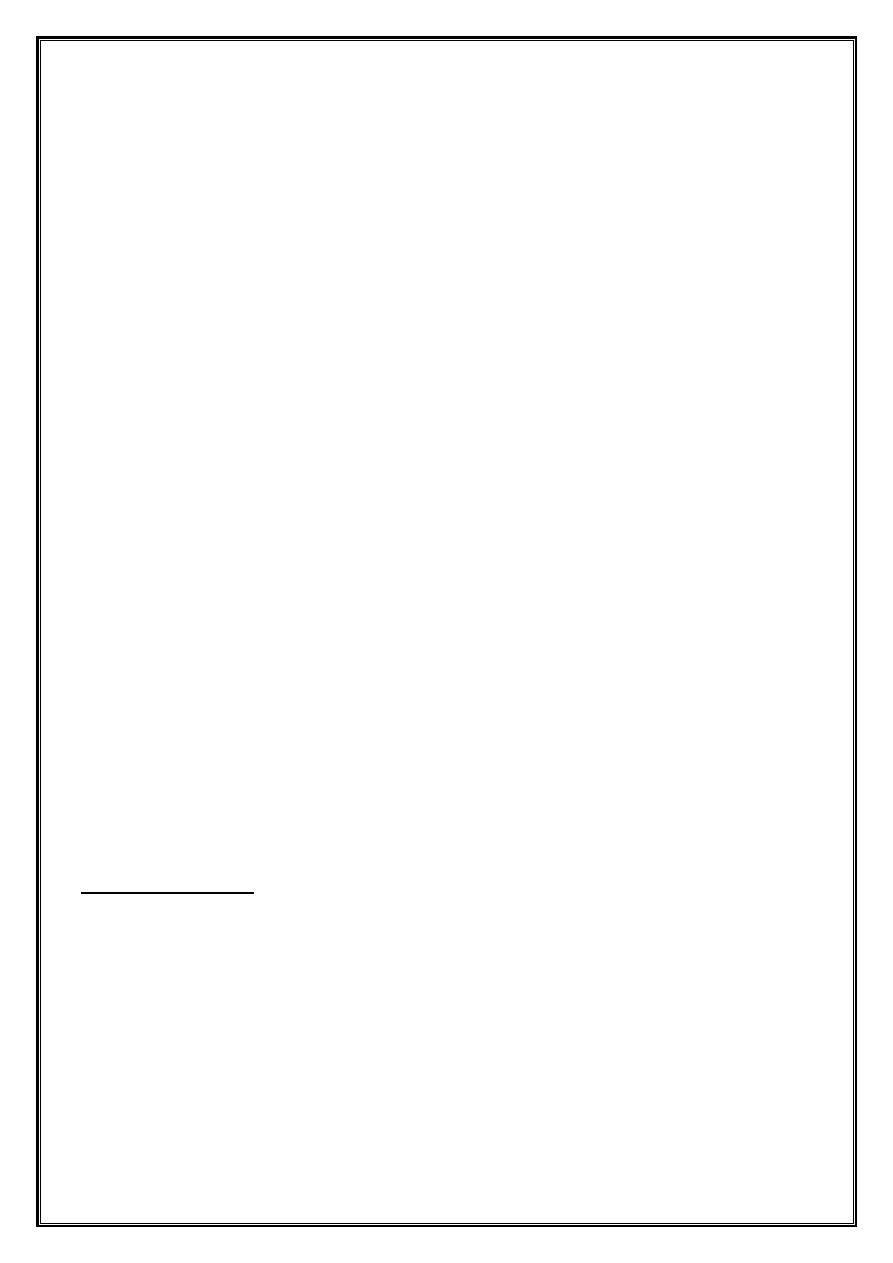
Fanconi anemia Fanconi anemia Chromosomal breakage
Fanconi anemia-
Syndactyly
Fanconi anemia- Absent radius
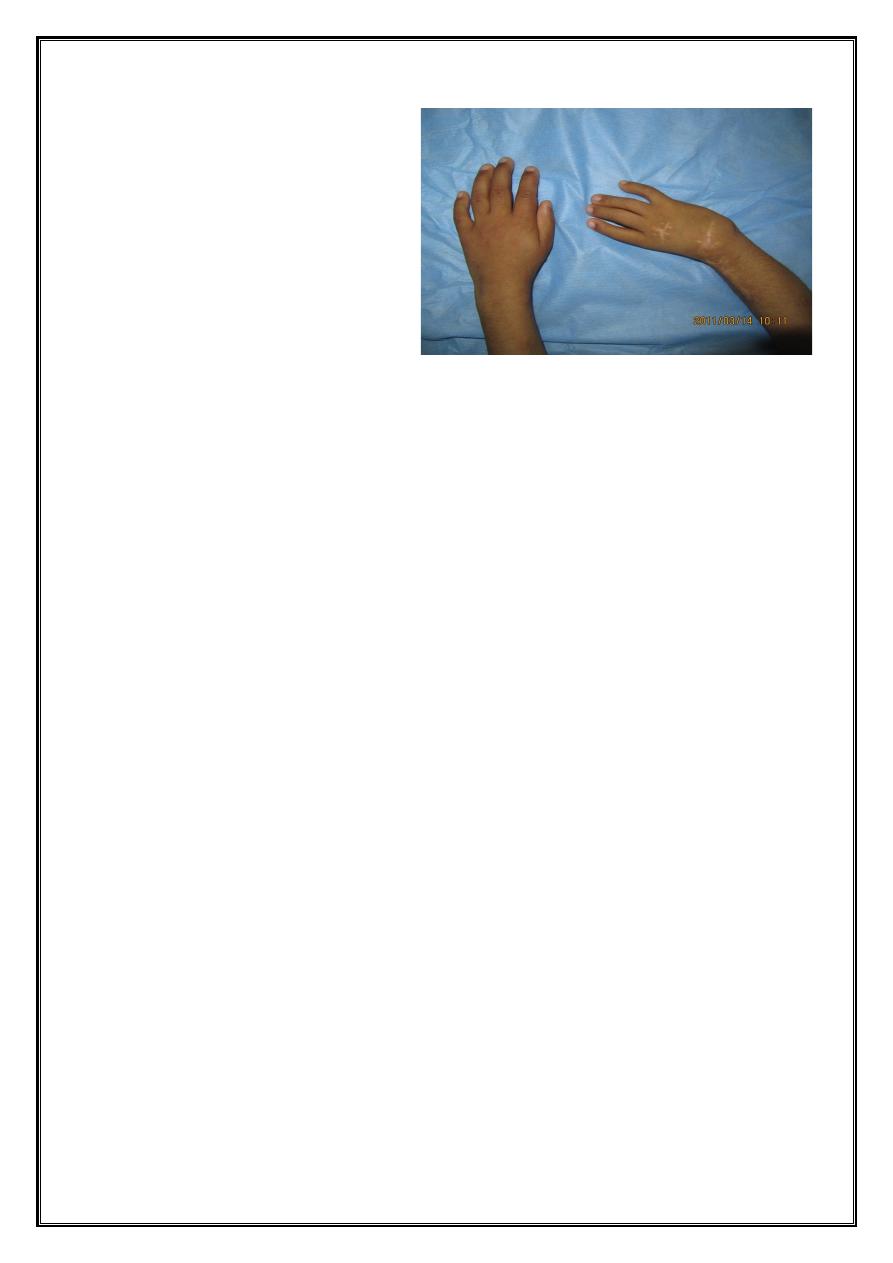
Fanconi anemia-absent thumb
Laboratory Findings
•
Marrow failure usually ensues in the 1st decade of life
•
The marrow becomes progressively hypocellular and fatty, similar to severe
acquired aplastic anemia .
•
Chromosome fragility is due to spontaneously occurring chromatid breaks
Treatment
•
If the hematologic findings are stable and there are no transfusion
requirements ,observation is indicated
•
Hematopoietic stem cell transplantation is the only curative therapy for the
hematologic abnormalities
.
THANKS

