Protein Synthesis InhibitorsThey work by targeting bacterial ribosomesAminoglycosidesMacrolidesTetracyclinesSpectinomycin
AminoglycosidesGentamicinTobramycinAmikacinStreptomycin
MOA: Inhibit protein synthesis by binding to 30s ribosomal subunitConcentration dependent killers
AMGS
MoACross the outer membrane to periplasmic space through porin proteins
Actively transported across the cell membrane by an oxygen-dependent process
Irreversibly bind to the 30S ribosomal subunit leading to misreading of the genetic code and inhibition of protein synthesis.Pharmacokinetics
Penetrate most body fluids well, except for the CSF.
High concentration of AMG accumulate in the renal cortex and inner ear
Nephrotoxcity: directly related plasma levels and duration of treatment
Ototoxicity: Severe acute tubular necrosis may occur
Aminoglycosides-Pharmacodynamic
SE: Renal Dysfunction: 5-25%
Monitor BUN / S.Cr and adjust doseMonitor TROUGH levels for toxicity
Goal Trough: < 1 mg / dL for once daily dosing
Neuromuscular block: Rare, associated with rapid IV infusion
Extended interval Dosing : less nephrotoxicity
Post antibiotic effect against Gram -
Aminoglycosides
AgentsGentamicin
Tobramycin
Amikacin
Netilmicin
Streptomycin
Primary Coverage:
GRAM - !!!!!!!!
Including Pseudomonas
Very little Gram +
Synergy for endocarditis
Staph, enterococcus
MacrolidesBacteriostatic in generalBacteriocidal against Streptococci-Time Dependent
Erythromycin
Clarithromycin
Azithromycin
Macrolides
AgentsErythromycin
Clarithromycin
Azithromycin
Primary Coverage
Atypicals!!!
Chlamydia
Legionella
Mycoplasma
Moderate Gram +
Moderate Gram -
Macrolides
• MOA: Inhibit bacterial protein synthesis• Bind to 50s ribosomal subunit
• Erythromycin:
• More SE’s ( especially GI )
• More DI’s ( CYP1A2, CYP3A4 inhibitor )
• Azithro / Clarithro better tolerated
• Less SE’s, QD - BID dosing
• Clarithromycin needs renal adjustment at Crcl <30 ml/min
• Azithromycin has very few clinically significant drug interactions
• Indication: Skin and soft tissue infections
Macrolide Side Effects
• Side Effect
• Erythro
• Clarithro/Azithro
• GI upset
• 25-30%
• 5-10%
• Rash
• 5%
• Rare
• LFTs
• 2-5%
• Rare
• Transient hearing loss
• Rare
• Rare
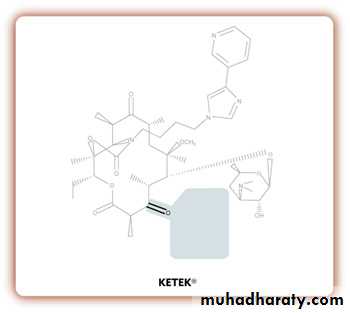
Ketolides:Telithromycin (Ketek)
• Structurally related to macrolides• MOA: same as macrolides, but has activity against resistant strains
• Conc dependent, bactericidal
• PO formulation
• FDA indication:
• Community-acquired pneumonia
Lacks portion of macrolide structure = less resistance
Telithromycin (Ketek)
Adverse effectsVision problems: 3%
Blurred vision
Accomodation issues
Diarrhea: 11%
Nausea: 8%
Headache: 6%
Dizziness: 4%
Pregnancy category C
ActivityStreptococcus spp.
Staphylococcus aureus
not MRSA
H. influenzae
Moraxella
Chlamydia
Mycoplasma
Legionella
Requires renal and hepatic dosing adjustment!
TetracyclinesDoxycycline, Tetracycline, Minocycline
TetracyclinesDoxycycline, Tetracycline, Minocycline
MOA: bind to 30s ribosomal subunit to inhibit bacterial protein synthesisNot used as much anymore: other options available
Coverage:
Gram +: Staph (not MRSA), Strep
Gram -: moraxella, H. flu, E. coli
Anaerobes: B. frag, C. difficile
Atypicals: chlamydia, legionella, mycoplasma
Doxycycline used for outpatient tx. of CAP
All can be used to treat acne
Trimethoprim-Sulfamethoxazole (Bactrim, Cotrim, Septra)
Trimethoprim-Sulfamethoxazole (Bactrim, Cotrim, Septra)MOA: Each inhibits a step in bacterial folic acid synthesis
No folic acid bacterial cell death (bactericidal)
High urinary concentrations
Primary use currently:
UTI
HIV prophylaxis of opportunistic infections
Primary Coverage:
Strep pneumo Proteus
H. Flu Enterobacter
E. coli
Community acquired MRSA (methicillin resistant staphylococcus aureus)
Trimethoprim-Sulfamethoxazole
Side Effects
N/V ( >10%)
Diarrhea (>10%)
Rash (>10%)
Fever (>10%)
Leukopenia/Thrombocytopenia
Stevens-Johnson syndrome (1-10% )
Drug Interactions
Bactrim may displace other highly protein bound drugs
Warfarin
Phenytoin
Methotrexate
Contraindications:
Pregnancy (3rd trimester only)
Severe liver disease
Clindamycin & Metronidazole
ClindamycinMOA: inhibits bact. protein synthesis
Side Effects:
GI!!!!! 25-30%
#1 ABX causing C.Diff colitis/ # treated
LFTs: rare
Rash: 2-5%
DIs
May enhance neuromuscular blockade of such agents
Also active against:
Strep, MSSA
Metronidazole
MOA: damage bacterial DNA bacteriocidal
Side Effects:
GI: 5-10%
Seizures 2-5%
Pancreatitis: rare
Dark urine: high incidence
DIs
ETOH: disulfiram-like reaction
Inhibits Warfarin metabolism
INR
Only requires renal dosing if Clcr <10 ml/min
Grouped together because they are potent at treating ANAEROBES