
Neuro
Dr. Nibal
“ Seizures and epilepsy ”
Total Lec: 46

Seizures and epilepsies in children
Dr. Nebal Waill
Terminology & Definition
•
Seizure : a sudden alteration in behavior , awareness, motor movement , body
posture, autonomic function and/or sensory or psychic perception from both
physiological (epileptic ,chemical, anoxic , etc) and nonphysiological
(psychological ) causes, which may be paroxysmal and stereotyped.
•
Epilepsy :the tendency to have recurrent, unprovoked seizures caused by
physiologically abnormal brain electrical activity produced by idiopathic or
diverse brain pathologies.
•
Convulsion: a sudden rhythmical motor behavior , body posture, or alteration
in body tone from diverse physiological (epileptic, hypnic, chemical, anoxic ,
etc) and nonphysiological (psychological) causes, which may be paroxysmal
and stereotyped.
• tonic : characterized by increased tone or rigidity.
• Atonic seizure : are characterized by flaccidity or lack of movement during a
convulsion
• Clonic seizure : consist of rhythmic muscle contraction and relaxation
• Myoclonic seizure : shock like contraction of a muscle.
•
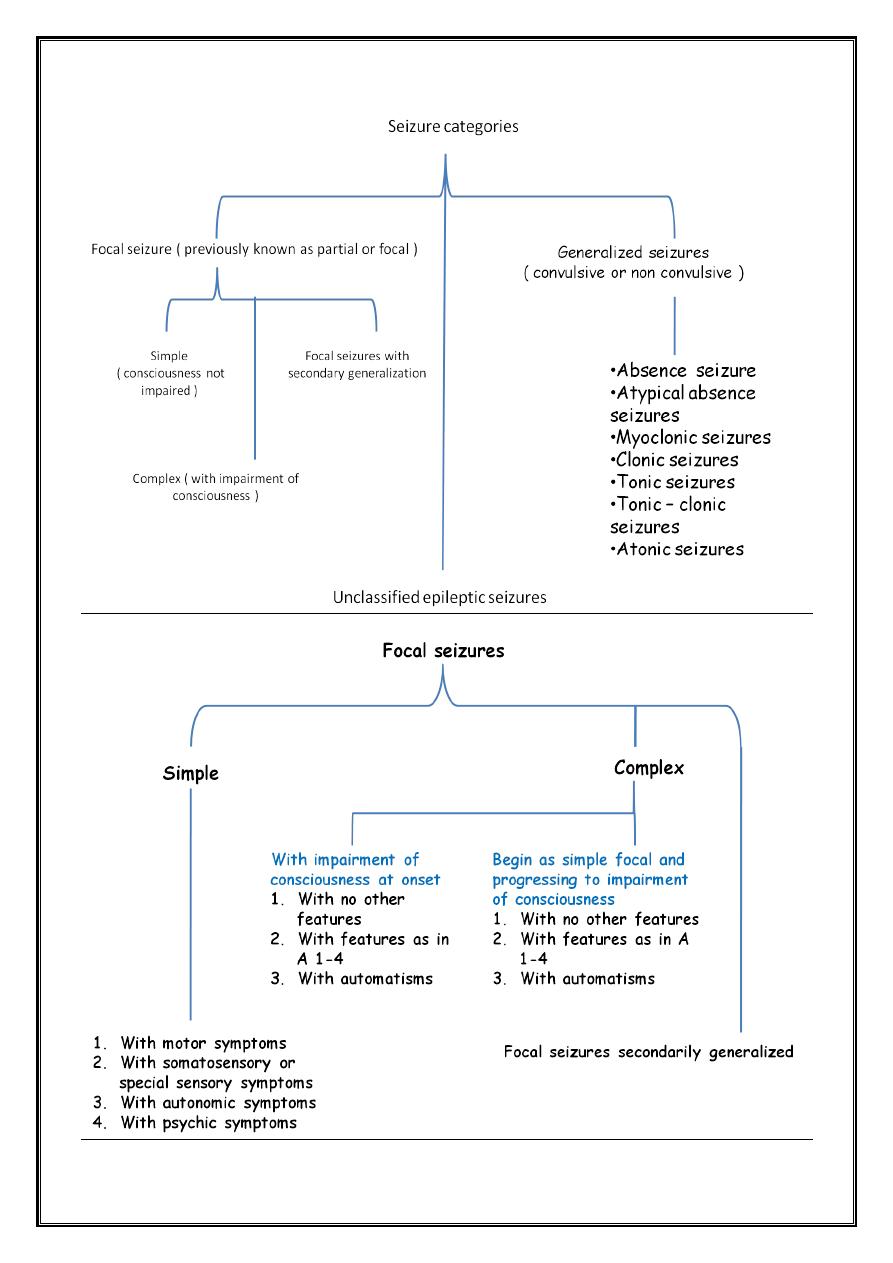
Focal arise in specific loci in the cortex which carry with them identifiable
signatures either subjective or observational
•
Generalized seizure involves large volumes of brain from the outset and are
usually bilateral in their initial manifestations and associated with early
impairment of consciousness
•
Accordingly many different seizures in the immature would be left unclassified
Evaluation of seizure
1. Determine whether it has a focal onset or is generalized
2. Describe the motor type
3. Document the duration of the seizure and state of consciousness ( retained or
impaired )
4. Determine whether an aura proceeded the convulsion & the most common
aura experienced in children consists of epigastric discomfort or pain and a
feeling of fear
5. Posture of patients
6. Presence and distribution of cyanosis
7. Vocalization
8. Loss of sphincter control ( particularly the urinary bladder )
9. Post-ictal state ( sleep, headache, hemiparesis ) should be noted
Febrile convulsion
•
FC : seizure in association with a febrile illness in the absence of a CNS
infection or acute electrolyte imbalance in children older than 1 month of age
without prior afebrile seizures
•
Conditions :
1. Temperature : the key factor is the actual peak temperature , must be > 38.4 C˚
2. Age : it’s age dependent , most common 6mo – 5 yr.
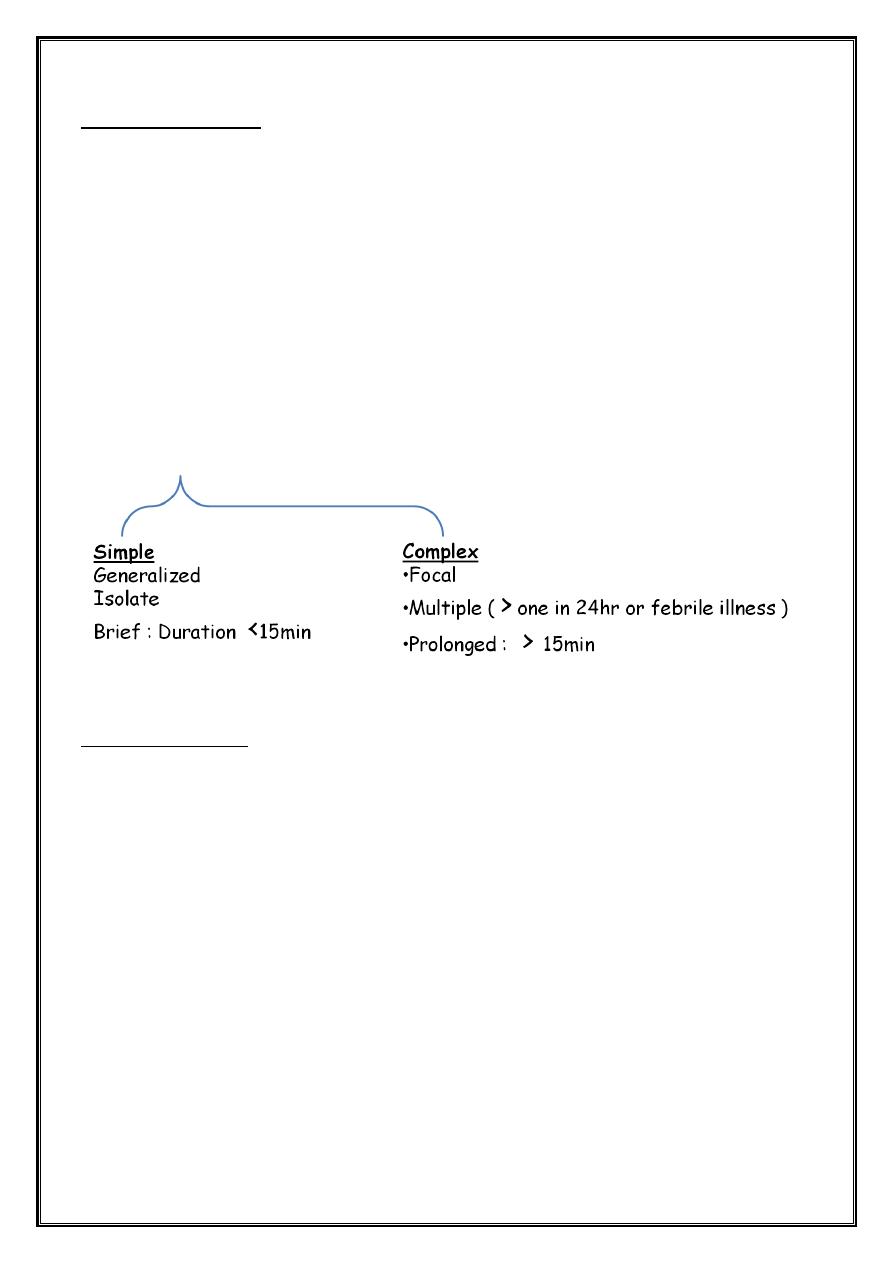
3. Classification
Initial evaluation
1. LP:
•
strongly considered <12 mo
•
12-18mo = need careful assessment
•
> 18 mo = not necessary in absence of suspicious findings on Hx & PE
2. Skull X-ray of no value
3. CT of limited benefit unless suspect trauma or ICP
4. MRI not indicated
5. EEG of limited value
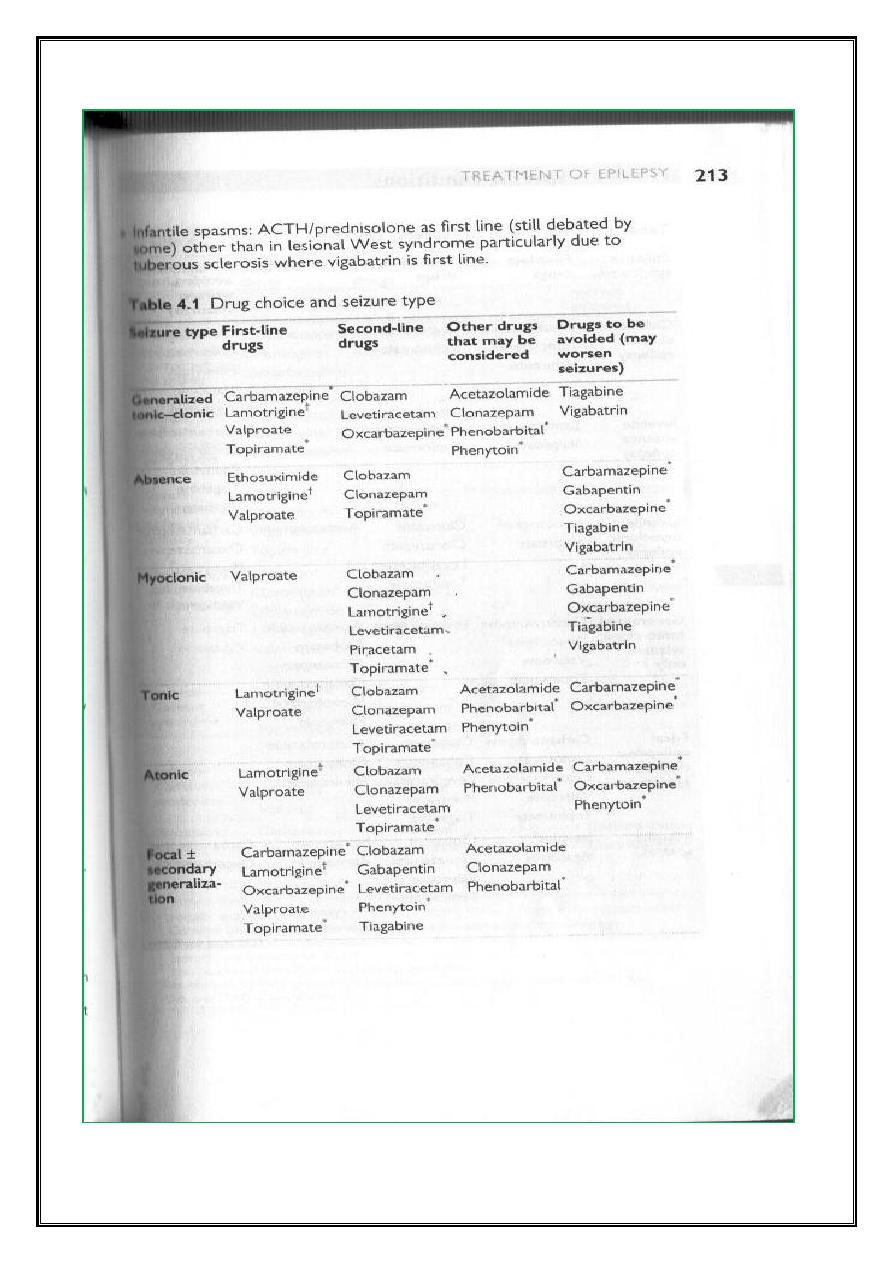
Very general rule of thumb to treat epilepsy
1. Generalized epilepsies and syndromes : Na Valproate
2. Focal seizures +/- generalization :
carbamazepine
lamotrigine
Status epilepticus
Functionally a seizure lasting more than 30 (5, 10) minutes or recurrent seizures
lasting more than 30 (5,10) minutes from which the patient does not regain
consciousness
Precipitating Events
• fever
• Infections (CNS, Systemic )
• Emotional stress
• Toxins, Alcohol, Drugs, Poisons, Convulsive agents
• Cardiac arrhythmia
• Electrolytes imbalance
• Primary apnea
• Sleep deprivation
• Diagnostic procedures and medications
• Progressive-degenerative disease
• Hormonal change
• Structural (Trauma , Ischemic stroke , Hemorrhagic stroke ,Acute
hydrocephalus)
• AED alteration : noncompliance , Withdrawal Interaction , toxicity
Medical complications of SE
• Tachycardia
• Bradycardia
• Cardiac arrhythmia
• Cardiac arrest
• Conduction distrubance
• Congsetive heart failure
• Hypertension
• Hypotension
• Altered respiratory pattern
• Pulmonary edema
• Pneumonia
• Oliguria
• Uremia
• RTA
• Lower nephron nephrosis
• Rhabdomyolysis
• Myoglobinuria
• Apnea
• Anoxia
• Hypoxia
• CO2 narcosis
• Intravascular coagulation
• Metabolic and respiratory acidosis
• Cerebral edema
• Excessive perspiration
• Dehydration
• Endocrine failure
• Altered pituitary function
• Elevated prolactin
• Elevated vasopressin
• Hyeperglycemia
• Hypoglycemia
• Increased plasma cortisol
• Autonomic dysfunction
• Fever
Treatment of status epilepticus
1. Transferred to ICU
2. ABC
3. Remove by gentle suction excessive oral secretion
4. Properly fiting face mask attached to O2
5. Ambubag
6. N/G
7. i.v catherter
8. Rx hypoglycemia
9. Blood sample
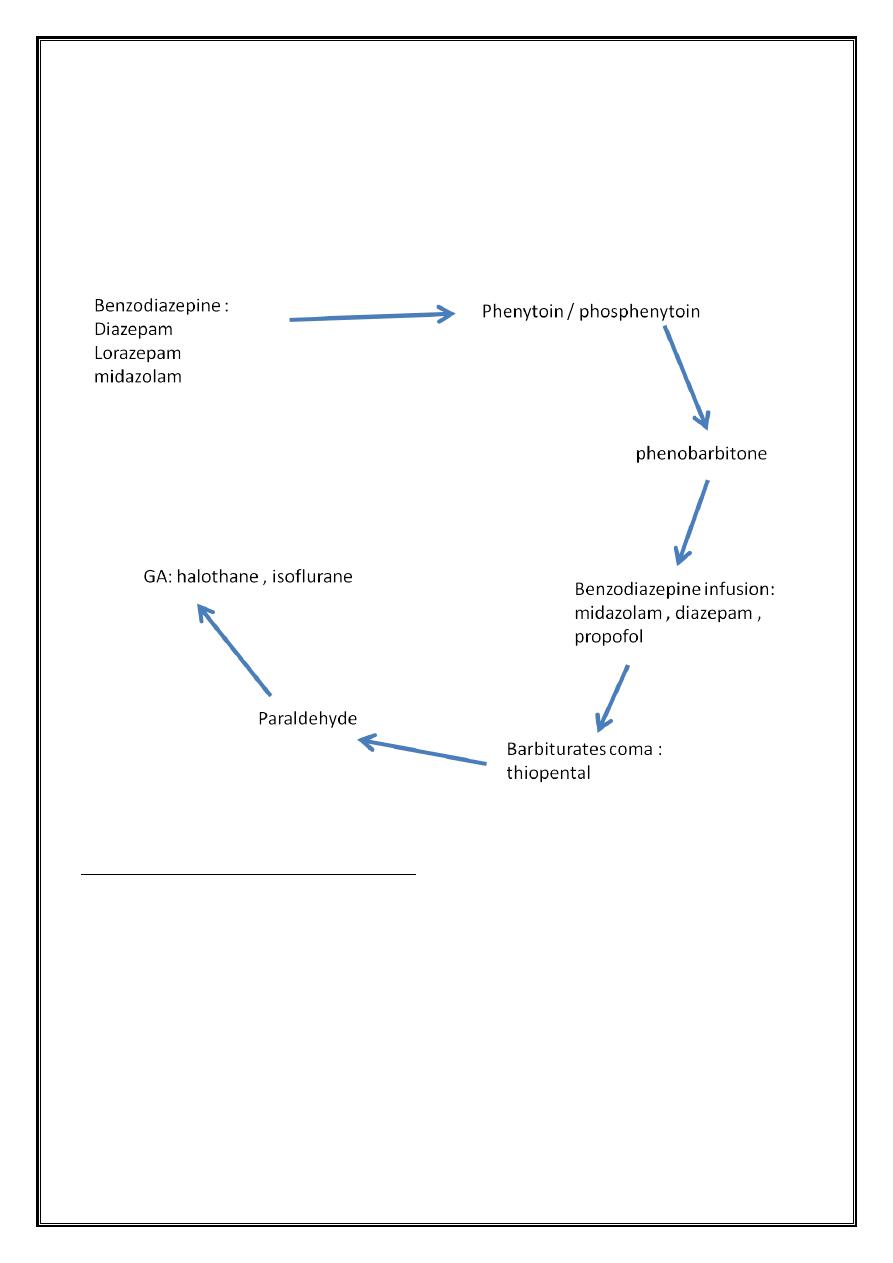
10. ± CSF
11. Neuroimaging
12. Concurrently perform physical and neurological examination
Physical and neurological examination
1. Papilledema
2. Ant. Fontanel
3. Retinal hemorrhage
4. Kussmaul breathing + dehydration
5. Peculiar body odor
6. Abnormal hair pigmentation
7. Pupillary dilatation or constriction
8. After control seizure take detailed history
Doses of drug used in SE
•
Diazepam 0.1-0.3mg/kg at rate not more than 2mg/min
•
Diazepam repeated for max. of 3 doses.
Phenytoin
•
If the convulsive activity cease after diazepam or lorazepam therapy or if
seizures persist
•
Phenytoin : 15-30mg/kg i.v infusion
•
rate 1mg/kg/min
•
If seizure don’t recur maintenance [3-9mg/kg/day ÷ 2 began 12-24hr
Phenobarbital
•
Followed by or in some center initiated with
•
Loading : 15-20mg over 10-30min.
•
With control of seizure, maintenance 3-5mg/kg/day ÷ 2
•
Mortality rate of status epilepticus = 5%
•
Greatest number of death occur in symptomatic type
•
Long-term complications :
1. Hemiplagia
2. Extrapyramidal syndrome
3. Mental retardation
4. Epilepsy

