
Medicine
Dr. Ghyath
Neurology
“
Cranial nerve palsy
”
Dr. Ghyath
LECTURE 18

Cranial nerve palsy Dr. Ghyath
3
Cranial nerve palsy
Oculomotor nerve palsy
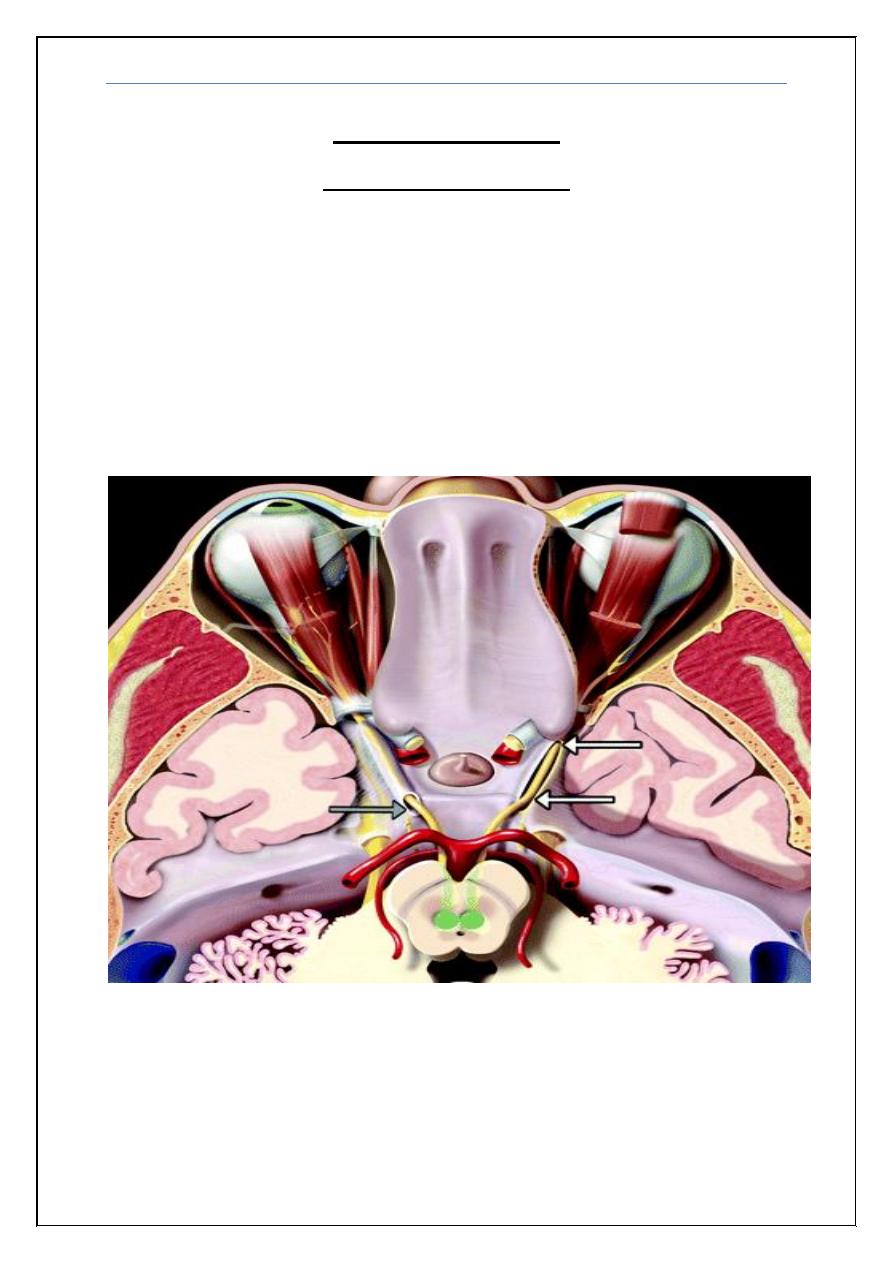
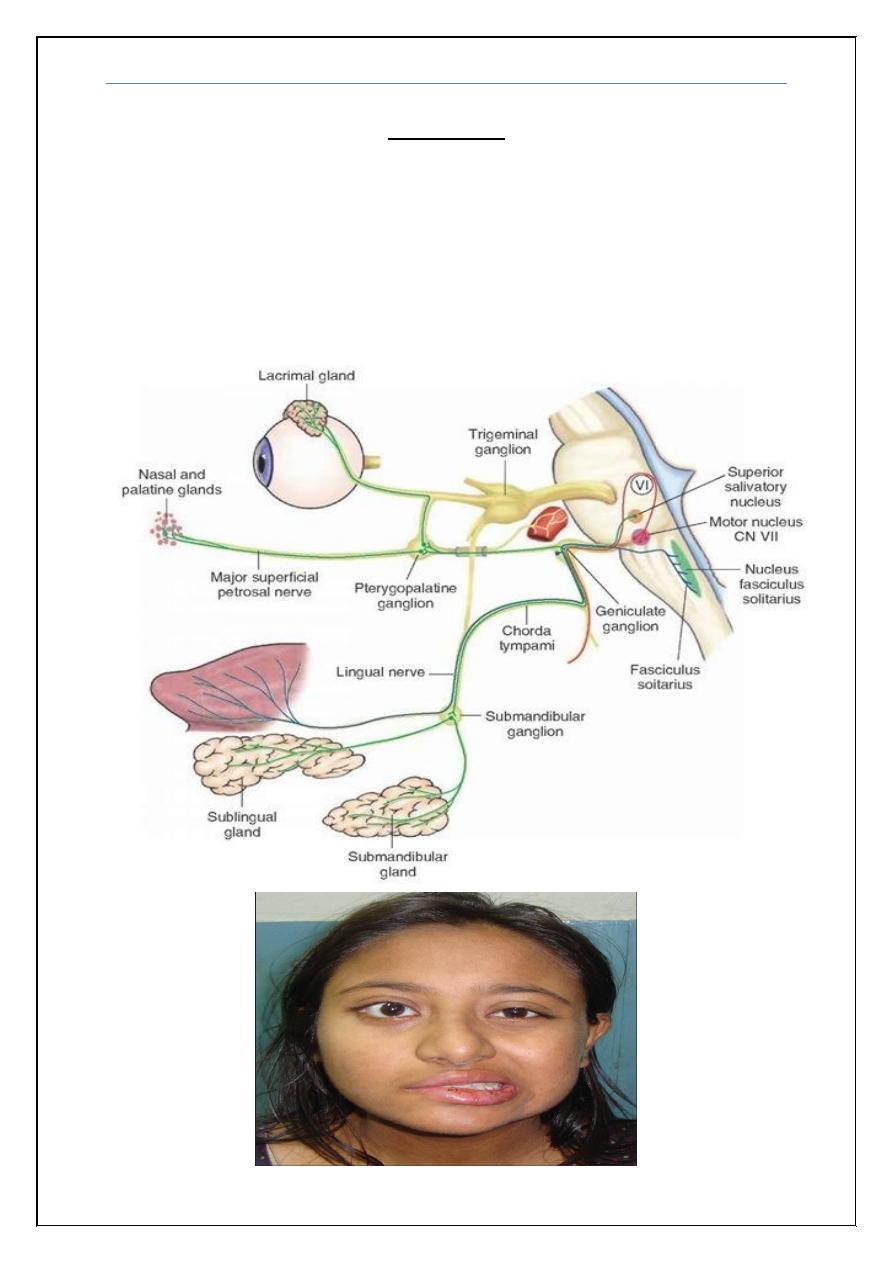
The nuclear complex of the third (IIIrd) nerve lies in midbrain after leaving the
brainstem, the nerve enters subarachnoid space and courses forward and
laterally between posterior cerebral artery and superior cerebellar artery. At this
level the nerve is compressed by Berry Aneurysms then the artery pass through
cavernous sinus, together with trochelear 4th, abducent 6th, first division
(ophthalmic) and second division (maxillary ) of the 5th cranial nerve ,after that
through superior orbital fissure to supply somatic: Superior rectus (SR), inferior
rectus (IR), inferior oblique (IO), medial rectus (MR)
and levator palpebrae
superioris (LPS) as well as autonomic (pupillary sphincter and ciliary) muscles
of the eye .
Cranial nerve palsy Dr. Ghyath
4
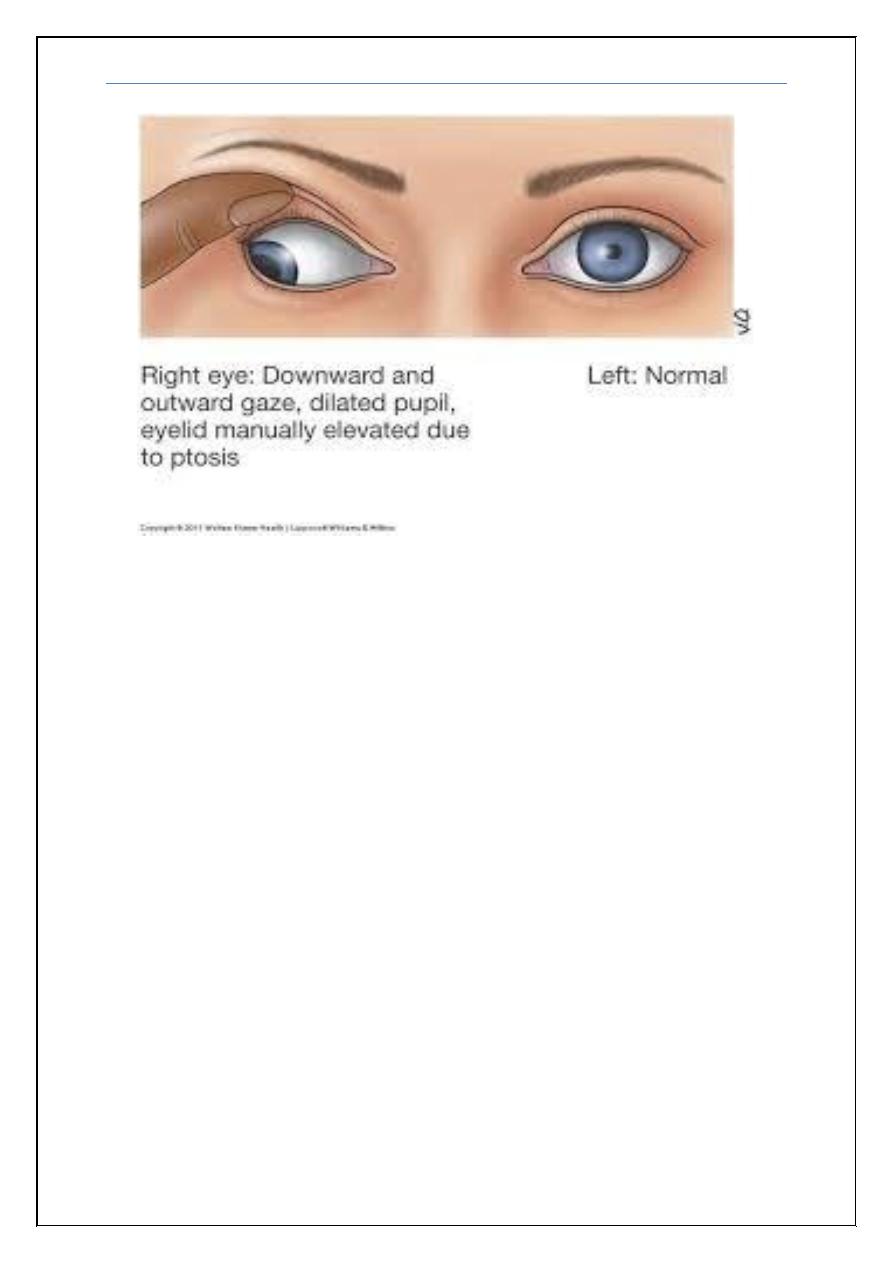
Oculomotor nerve lesions:
1-In nuclear lesions in the midbrain; most common cause is stroke
2-Subarachnoid space is the most likely site of involvement in isolated IIIrd
nerve palsies.the pathology may be compressive or infarction secondary to
microvascular involvement in diabetics and hypertensives. Also compress by
an aneurysm.
3- In cavernous sinus, one must note the associated signs and symptoms. It
may be associated with the dysfunction of IVth and VIth nerves, first or
second division of trigeminal nerve most common cause is thrombosis and
infection especially in diabetic
4-in the superior orbital fissure together with cranial nerves 4th, 6th and first
division of trigeminal nerves associated with proptosis.
Cranial nerve palsy Dr. Ghyath
5
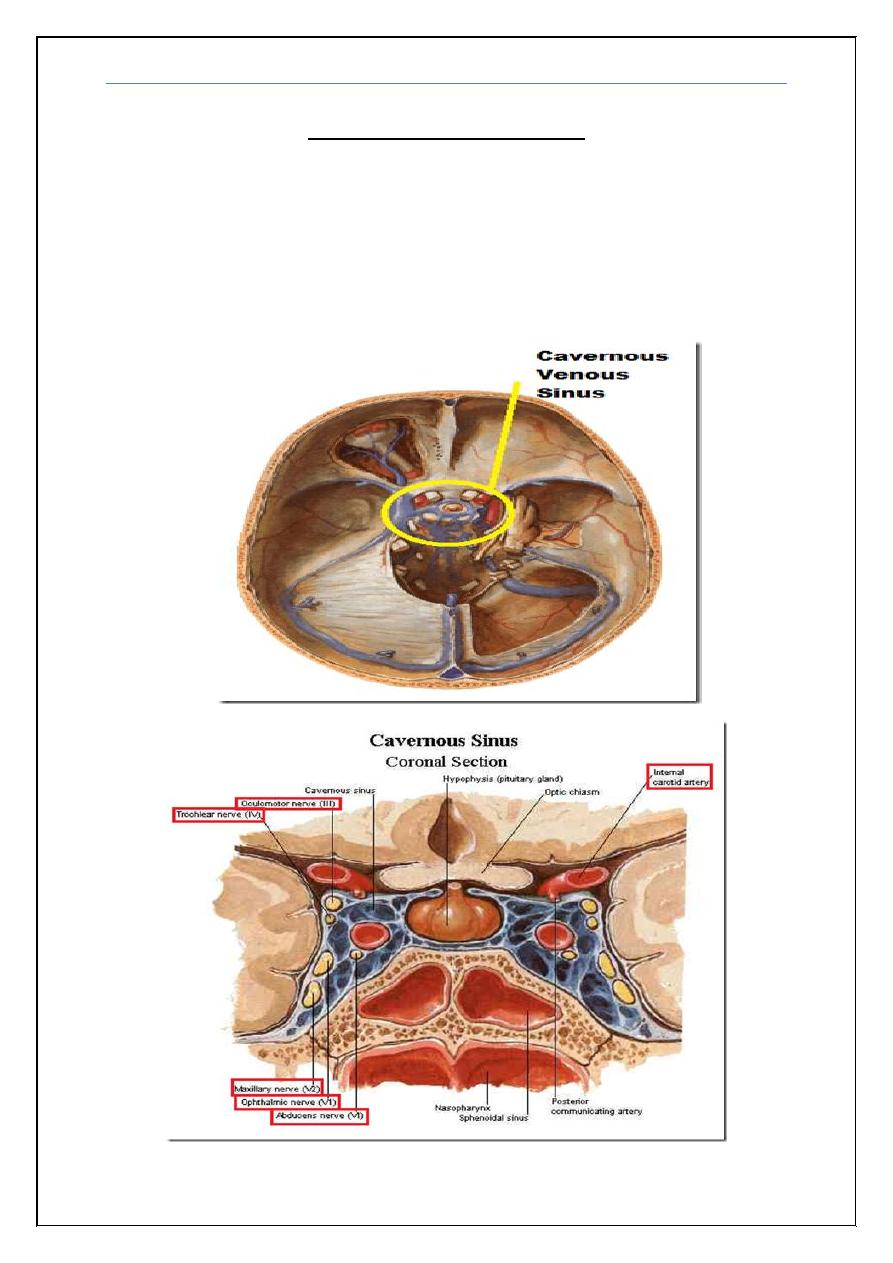
Cavernous sinus syndrome
The cavernous sinuses are paired, venous structures located on either side of the
sella turcica, they receive venous tributaries from the superior and inferior
orbital veins, the cavernous sinus contains the carotid artery, its sympathetic
plexus, and the oculomovement nerves (third, fourth, and sixth cranial nerves).
In addition, the ophthalmic branch and the maxillary branch of the fifth nerve
traverse the cavernous sinus.
Cranial nerve palsy Dr. Ghyath
6
Clinical manifestation
Ophthalmoplegia, chemosis, sometimes proptosis, trigeminal sensory loss in
opthalmic and maxillary branches.
Casuses
1- Cavernous sinus thrombosis is a serious condition that can follow infection of
the face, paranasal sinuses (particularly the sphenoid sinus) or teeth most
commonly in diabetic
2- Metastases and nasopharyngeal carcinoma
3- Aneurysms of the intracavernous portion of the carotid artery
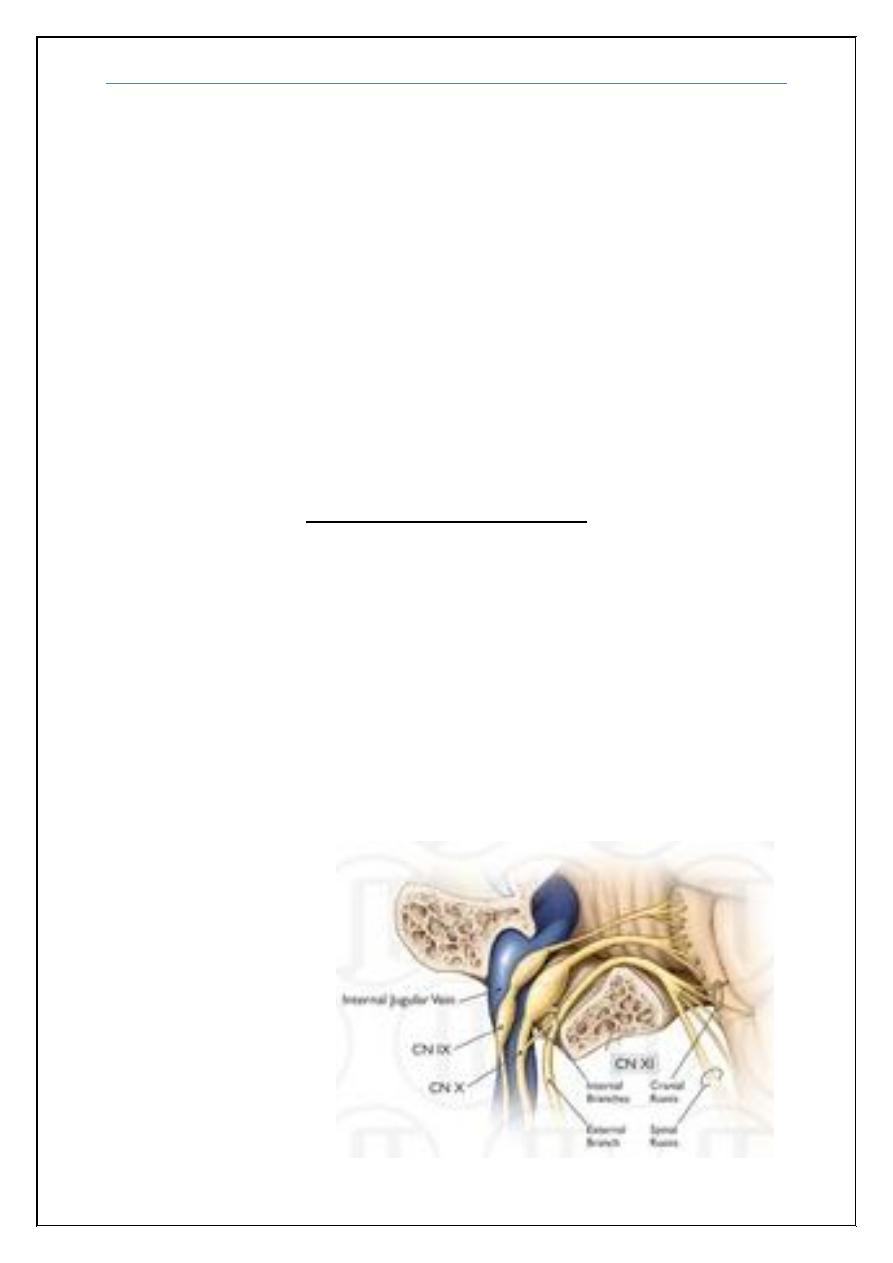
Jugular foramen syndrome
The jugular foramen is a large aperture in the base of the skull, Cranial nerves
IX, X, and XI and the internal jugular vein pass through the jugular foramen.
Clinical significance:
Is characterized by the paresis of (9
th
, 10
th
& 11
th
) cranial nerves together so
patient may complain from
1- Dysphagia, dysphonia/hoarseness,
2- Deviation of the uvula towards the normal side
3- Sternocleidomastoid and trapezius muscles paresis
Common Causes
A- Metastatic tumors
B- Infections
Cranial nerve palsy Dr. Ghyath
7
Bell’s palsy
Bell’s palsy is an acute peripheral facial palsy, Bell’s palsy may occur in
childhood; incidence increases steadily with age. There is no change in
incidence with season, latitude or geography and no evidence for familial
clustering. Weak associations may exist with diabetes and hypertension. A viral
aetiology has been postulated on the basis that detection of herpes simplex virus
type 1 (HSV-1) DNA in endoneurial fluid in most patients. Both primary HSV-
1 infection and reactivation of latent infection have been implicated
Cranial nerve palsy Dr. Ghyath
8
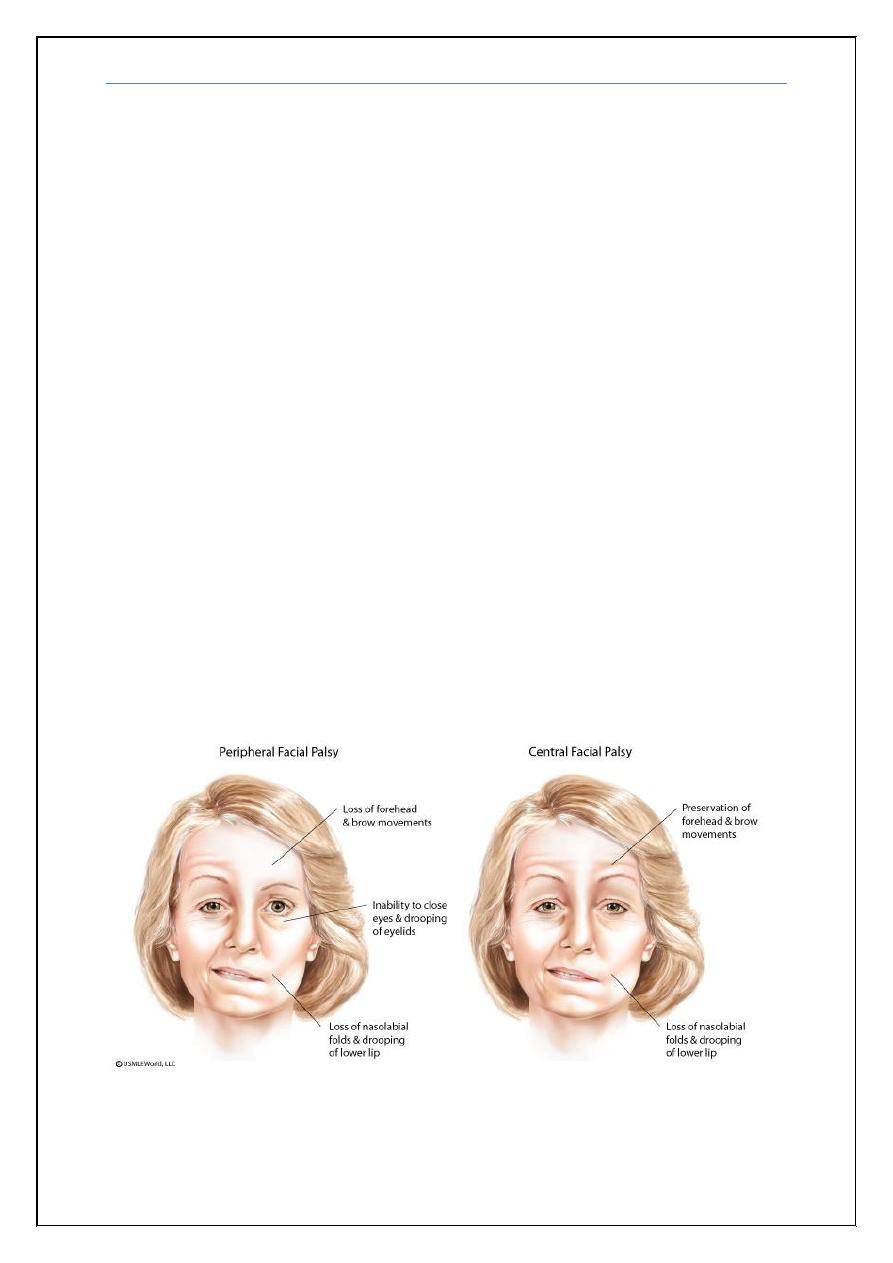
Clinical features
Rapid onset of facial weakness progressing over 48 hours (and occasionally up
to 5 days) is preceded or accompanied by diffuse retro-auricular pain in the
region of the mastoid, Facial weakness and asymmetry with drooling of liquids
from the corner of the mouth on the affected side often lead the patient to
suspect a stroke; most patients present promptly to primary care physicians. Not
infrequently, patients mistakenly report that the contralateral unaffected side is
the weak side. All facial muscles are usually equally affected, eye closure and
blinking is reduced or absent (with a visible Bell’s phenomenon attempted eye
closure).
Ectropion formation may lead to overflow of tears on to the cheek. The
angle of the mouth droops with reduction of the nasolabial fold, smoothing of
skin wrinkles; the platysma muscle is also involved. The extent of maximal
facial weakness is variable, but is severe in the majority, although occasionally
patients present with very mild facial weakness.
Loss of taste, often described as a muddy or metallic taste, and
hyperacusis (because of paralysis of stapedius) indicate involvement of the
chorda tympani and the branch to stapedius, respectively.
Note: The picture above were added by the students and it shows the differences
between central and peripheral facial palsy
Cranial nerve palsy Dr. Ghyath
9
Management and outcome
Complete or almost complete recovery, without recurrence, over 3–8 weeks is
the norm in at least 85% of cases, even without any treatment. Reassurance
about the good prognosis is important. Inability to blink in severe facial
weakness may lead to exposure keratitis and early evaluation should include
assessment of the eye.
Lubricating eye drops are often required and patients should be shown
how to tape the eye closed at night. Severe facial weakness with complete
inability to close the eye requires urgent ophthalmological assessment; lateral
tarsorrhaphy and/or temporary insertion of a gold weight into the upper lid
may be necessary. Early treatment with oral steroids (prednisolon) and
antiviral agents (oral acylovire) is worthy.
END
Cranial nerve palsy Dr. Ghyath
10
Note
: there is missing slide on lecture 9 (peripheral neuropathy) page 7
(Chronic Inflammatory Demyelinating Polyneuropathy).
You should add it before (Thoracoabdominal radiculopathy (Chest,
abdomen))
Treatment
Glucocorticoids (prednisolon) may be with immunosupression drugs like
azathioprine,IVIg, PE(plasma exchange)and are all effective.
Diabetes Mellitus
Neuropathies associated with diabetes
Polyneuropathy
Mixed sensory,motor, and autonomic (Symmetric, distal, lower > upper limbs)
But most likely is primarily sensory
Mononeuritis multiplex
Polyradiculopathy/plexopathy (Diabetic amyotrophy) Asymmetric,
proximal (pelvic girdle and thighs)
