Penis – Bowen disease
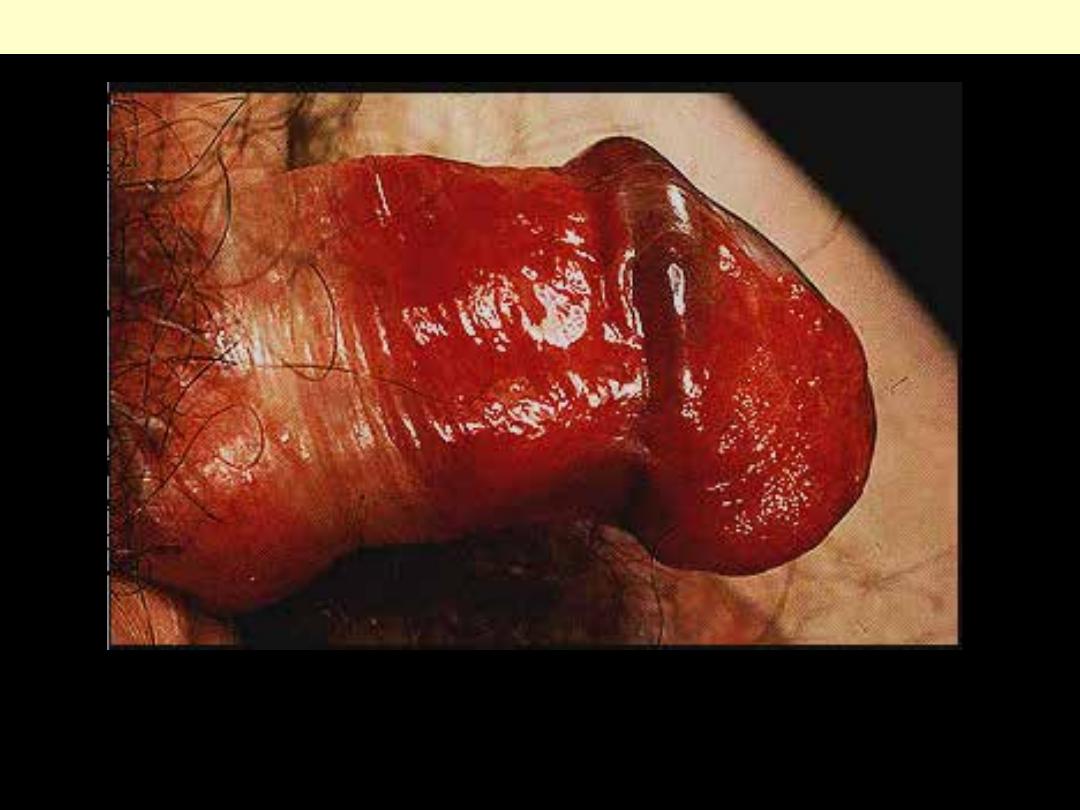
Carcinoma in situ: there is intense erythema of the glans penis and distal shaft. In the older literature,
Bowen’s disease at this site is sometimes referred to as erythroplasia of Queyrat.
Bowen disease of the penis (erythroplasia of Queyrat)
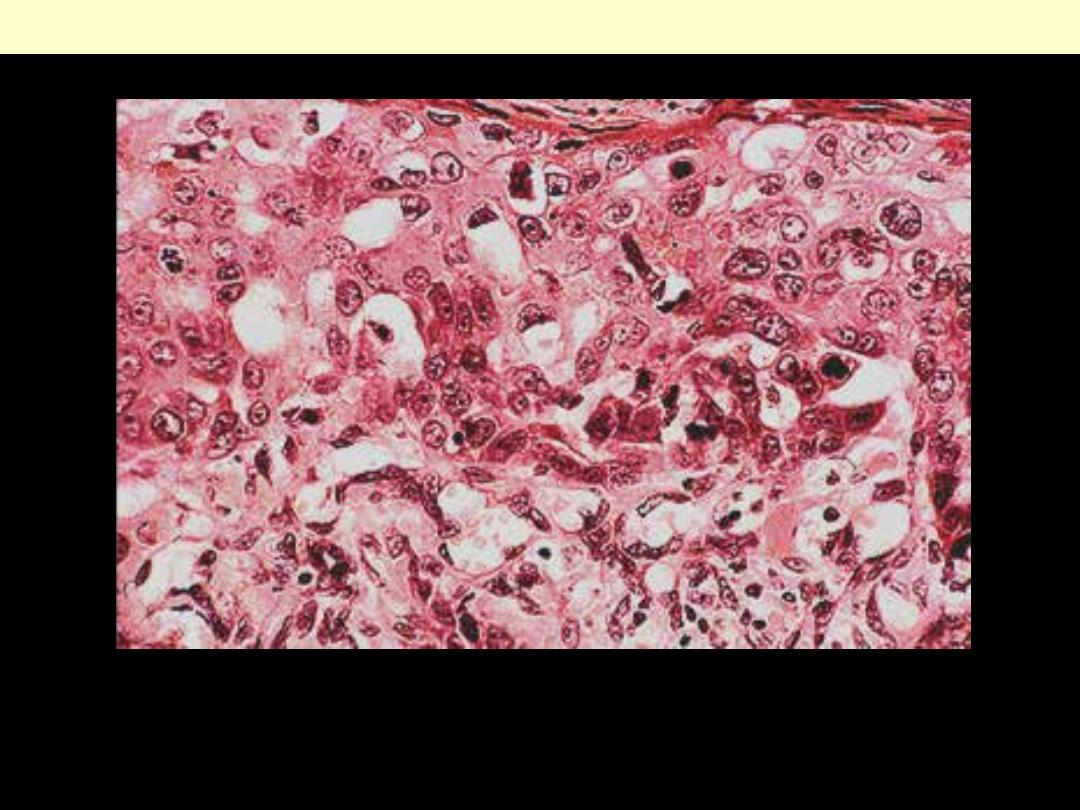
Bowen’s disease (SCC in situ): the epidermis is completely disorganized. Note the nuclear
pleomorphism.
Bowen disease of the penis (erythroplasia of Queyrat)
Penis - Carcinoma
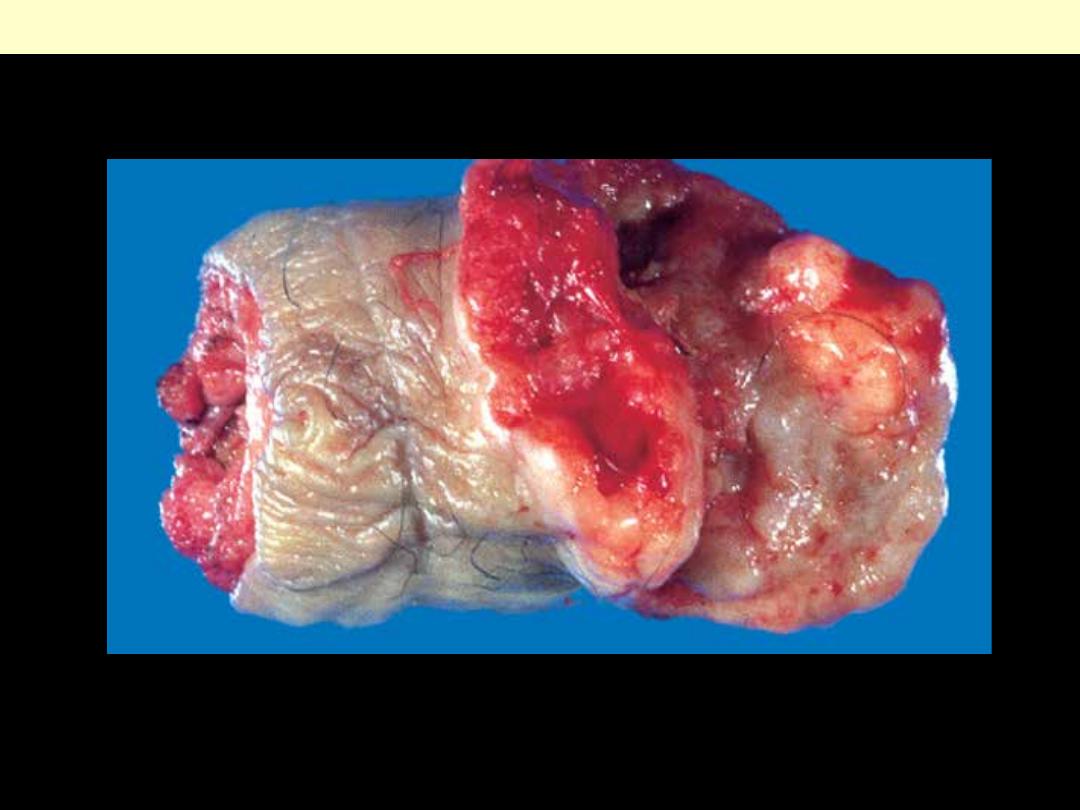
The glans penis is deformed by a firm, ulcerated, infiltrative mass .
Carcinoma of the penis
Prostate - Adenocarcinoma
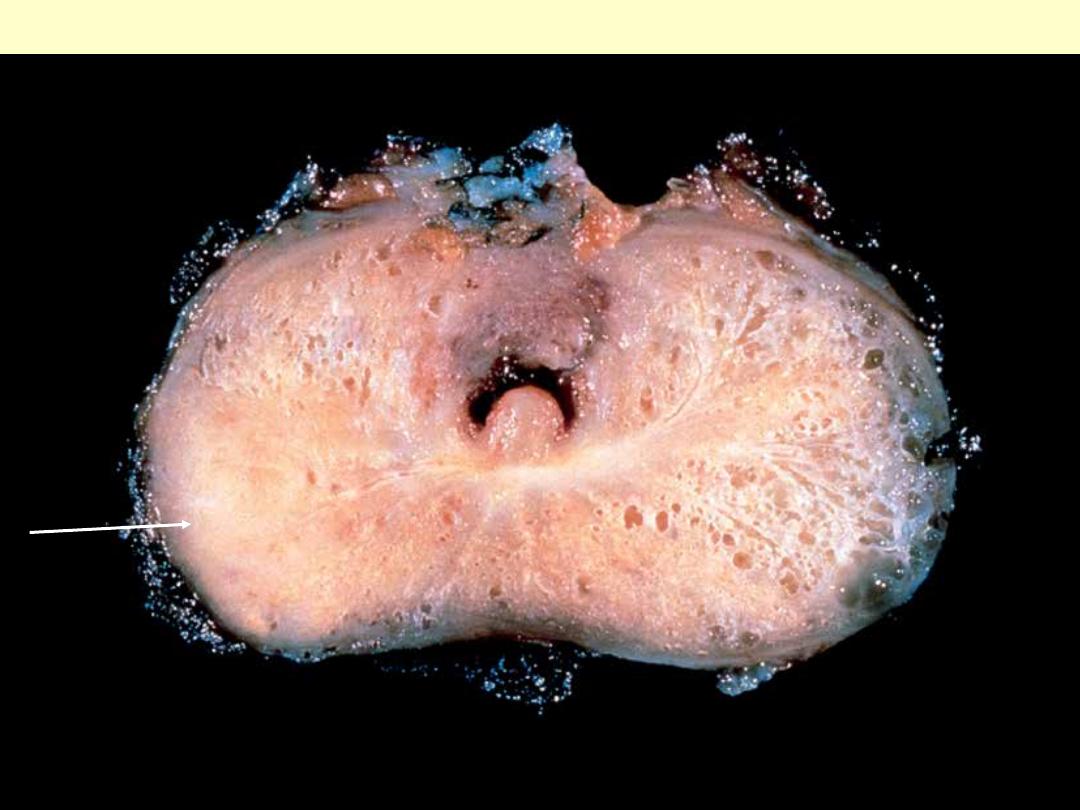
Carcinomatous tissue is seen on the posterior aspect (lower left). Note the solid whiter tissue of cancer
in contrast to the spongy appearance of the benign peripheral zone on the contralateral side.
Adenocarcinoma of the prostate
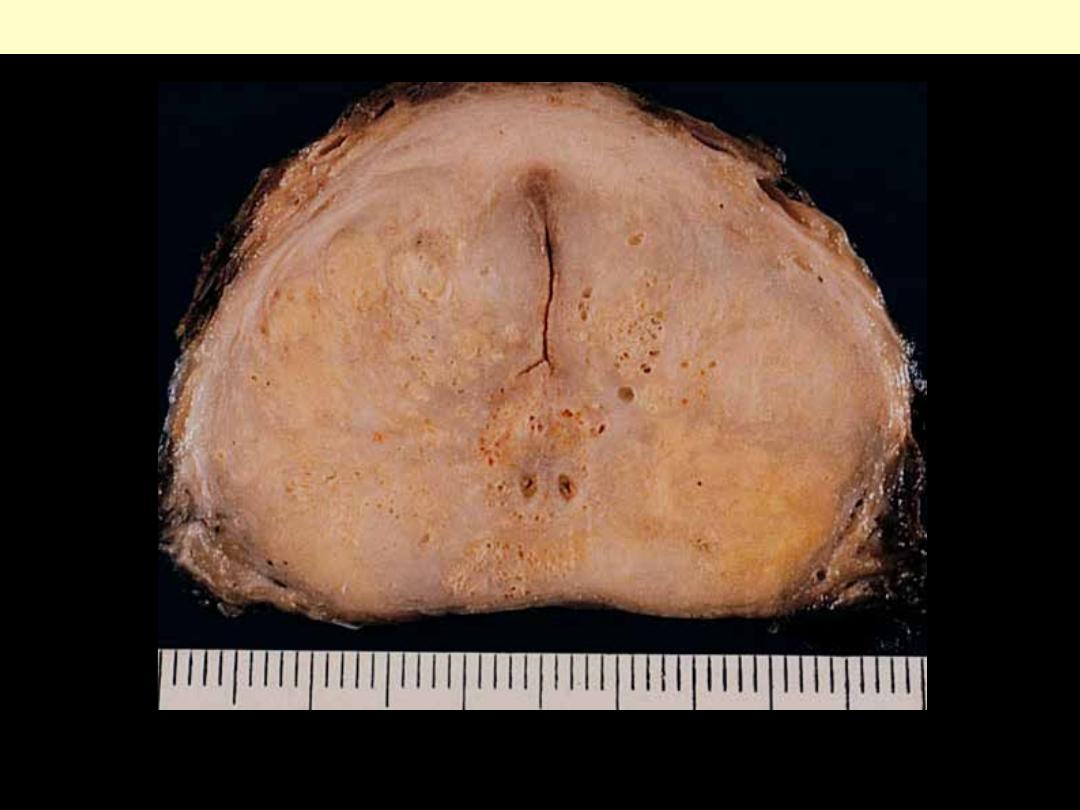
Extensive tumor appearing as an irregularly shaped, yellowish mass in a gland that is also involved by
nodular hyperplasia.
Adenocarcinoma of the prostate
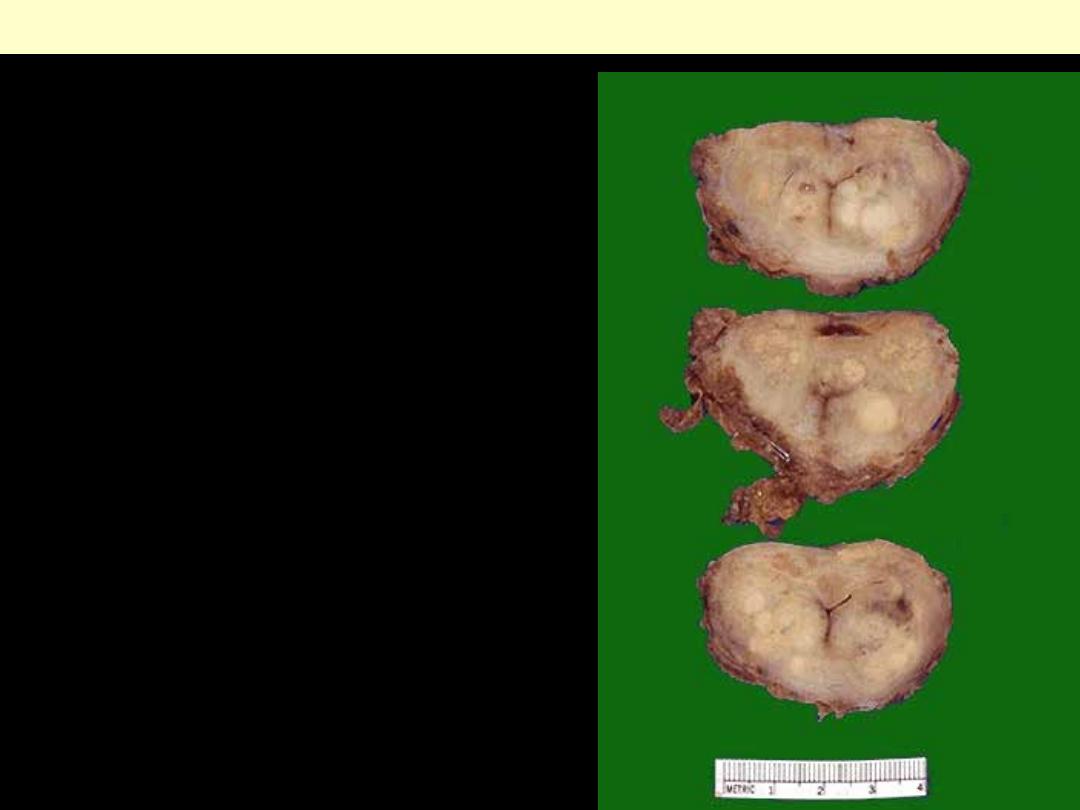
Prostatic adenocarcinoma
These sections through a prostate removed via radical
prostatectomy reveal irregular yellowish nodules,
mostly in the posterior portion. This proved to be
prostatic adenocarcinoma. Prostate glands containing
adenocarcinoma are not necessarily enlarged.
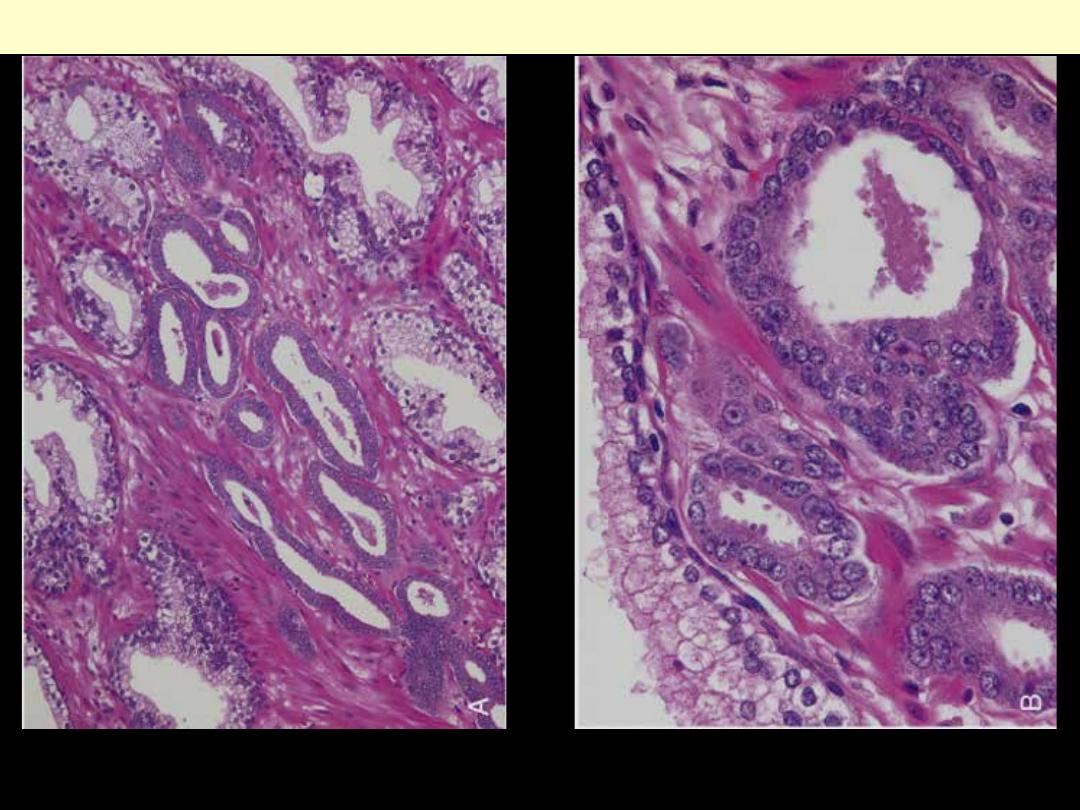
A, Photomicrograph of a small focus of adenocarcinoma of the prostate demonstrating small glands
crowded in between larger benign glands. B, Higher magnification shows several small malignant
glands with enlarged nuclei, prominent nucleoli, and dark cytoplasm.
Prostatic adenocarcinoma
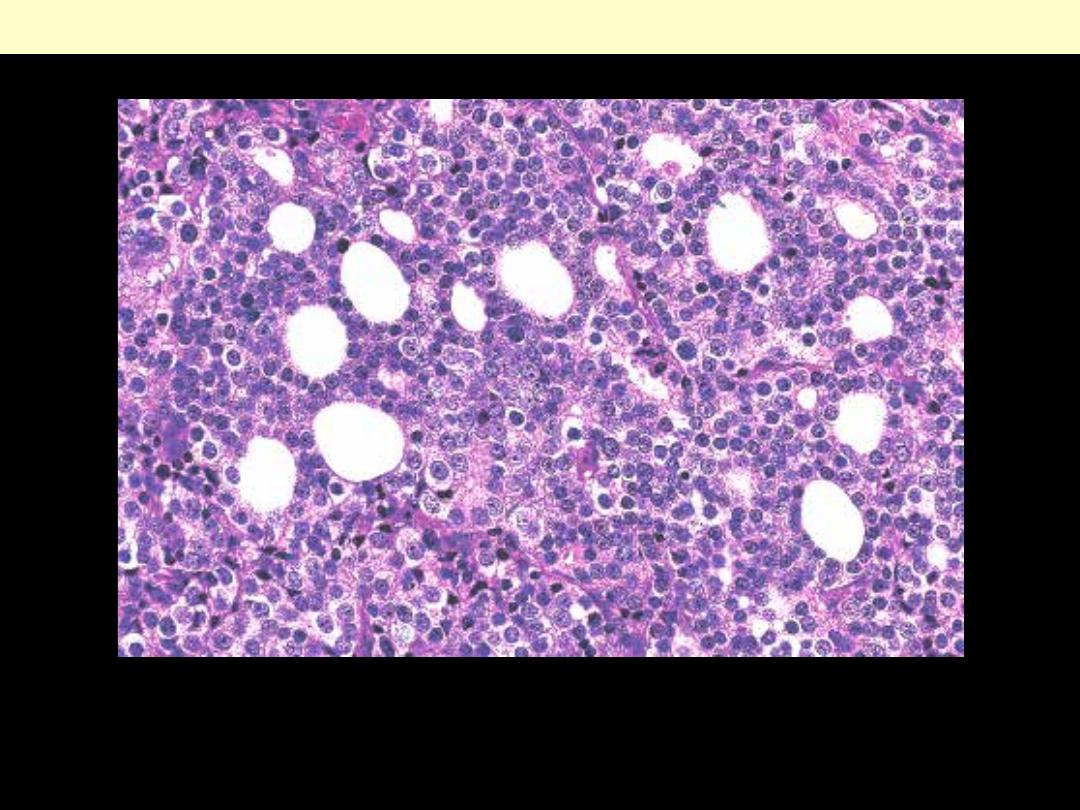
Prostatic adenocarcinoma initially presenting as left supraclavicular lymphadenopathy.
Prostatic adenocarcinoma lymph node metastasis
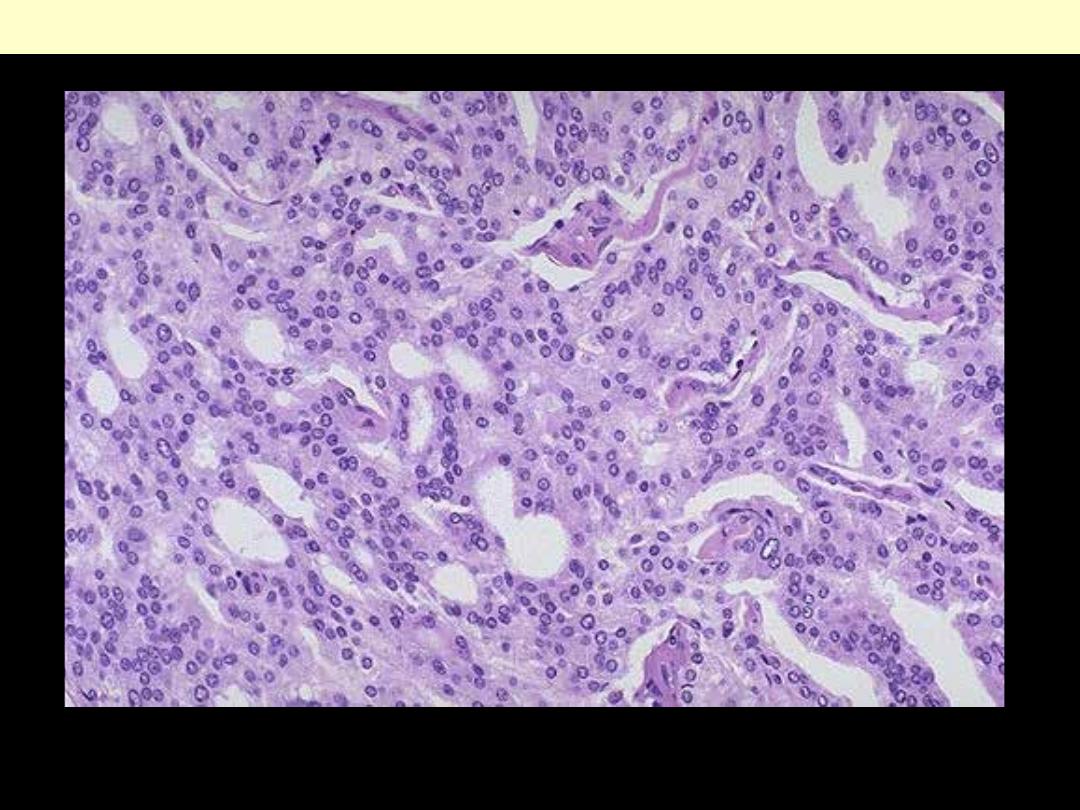
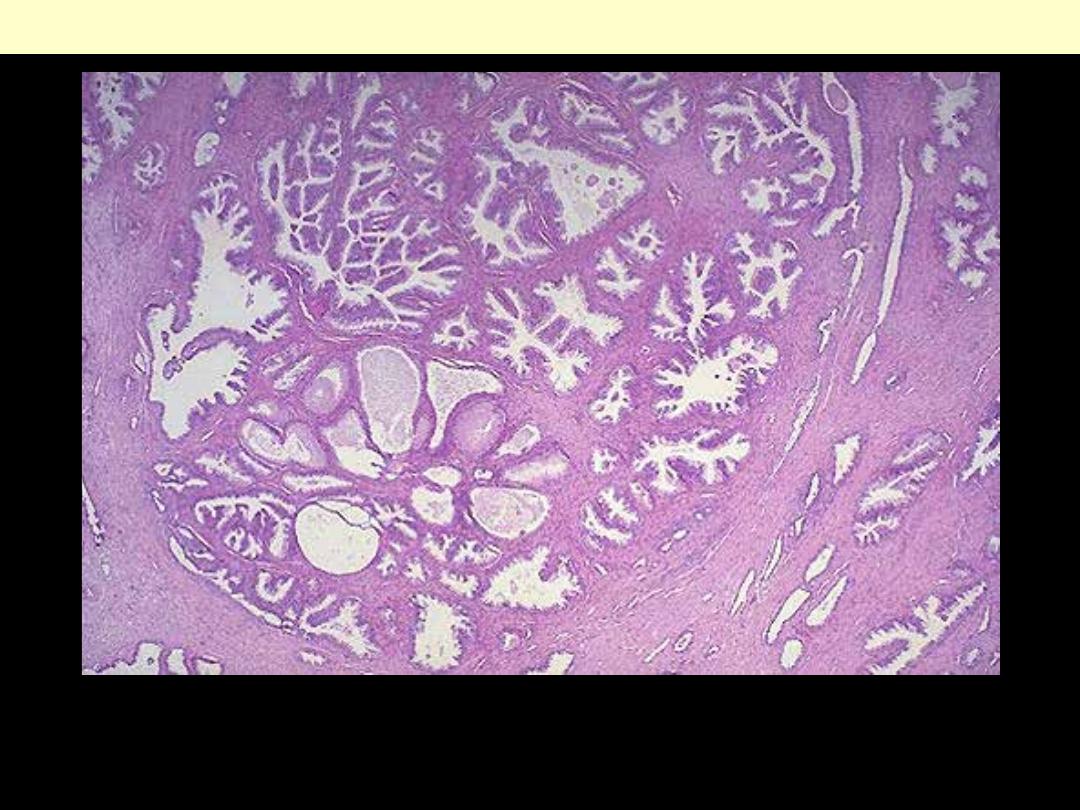
Prostatic adenocarcinoma back to back glands
At high magnification, the neoplastic glands of prostatic adenocarcinoma are still recognizable as
glands, but there is no intervening stroma and the nuclei are hyperchromatic.
Prominent cytoplasmic vacuolation in
prostatic carcinoma as a result of hormonal
treatment. The vacuolization is also present in
the area of perineurial invasion.
Prostatic adenocarcinoma perineurial invasion & effects of hormonal treatment
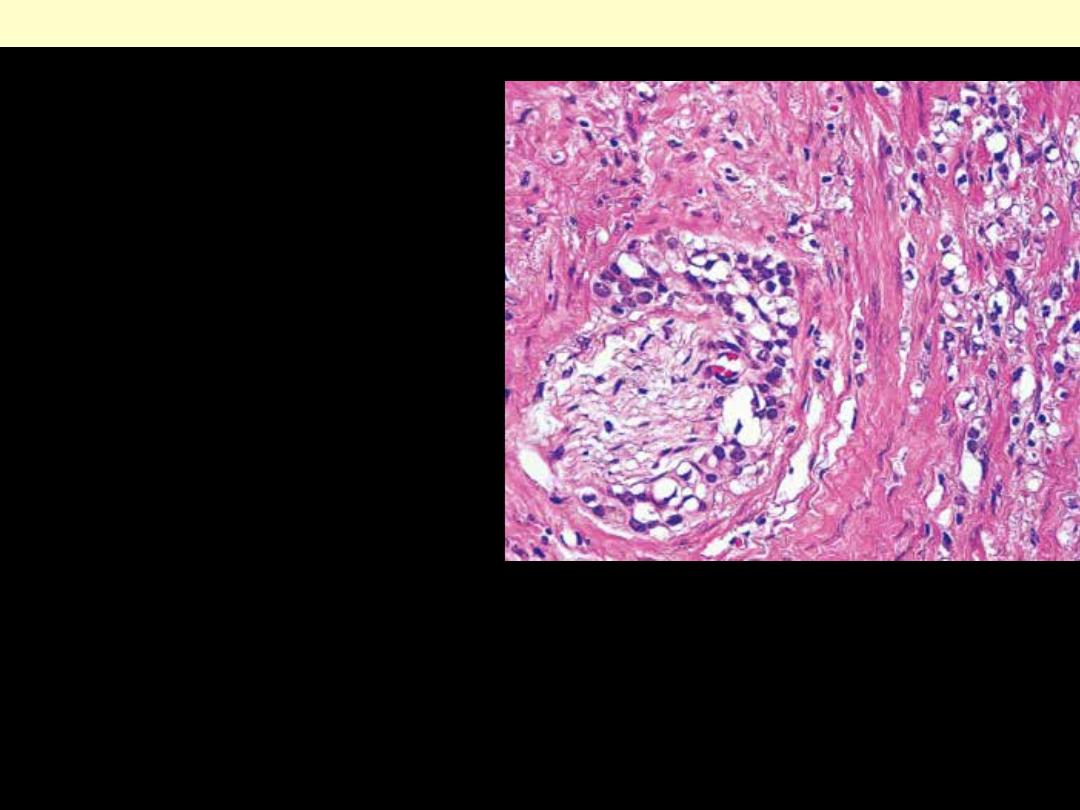
The pr esence of pr ostatic glands within per ineur al spaces is common in these tumor s. This
finding is a str ong indicator of malignancy but is not pathognomonic. It does not r epr esent
per meation of per ineur ial lymphatic vessels, as for mer ly believed, but r ather spr ead
of glandular tissue along planes of lesser r esistance. Its pr esence in a needle biopsy specimen is
a good pr edictor of capsular invasion by the tumor.
Prostate - Diagram
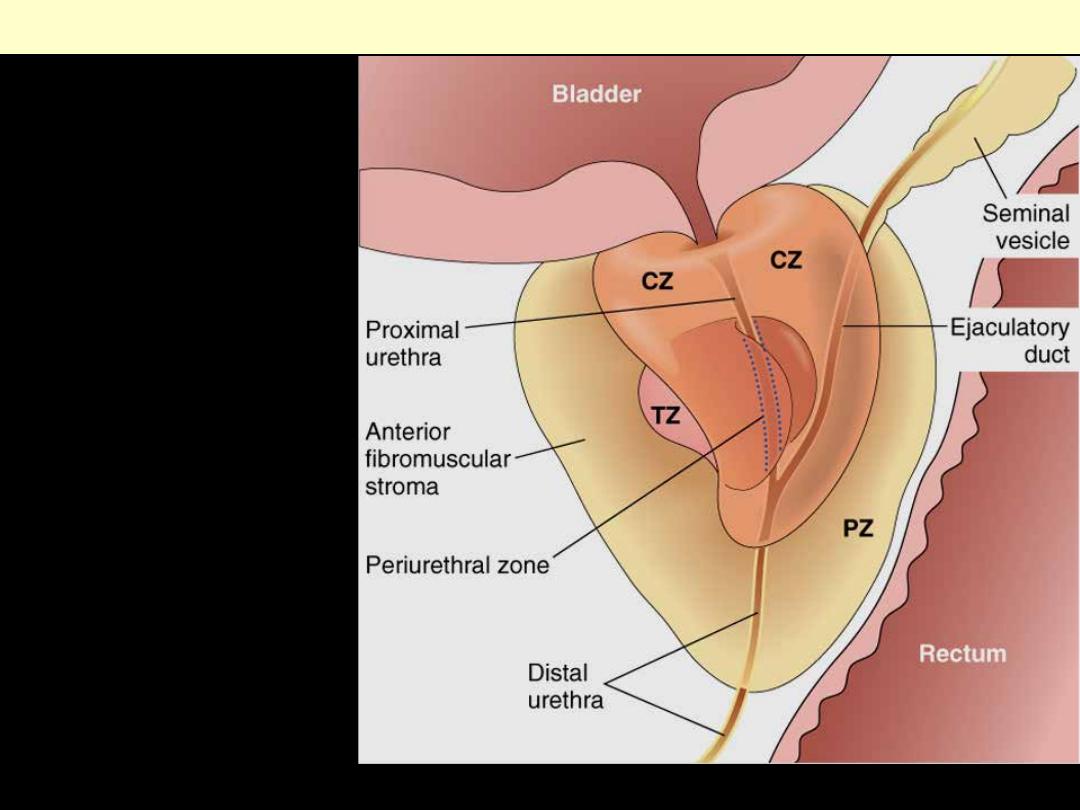
The normal prostate contains
several distinct regions,
including a central zone (CZ), a
peripheral zone (PZ), a
transitional zone (TZ), and a
periurethral zone. Most
carcinomas arise from the
peripheral glands of the organ
and are often palpable during
digital examination of the
rectum. Nodular hyperplasia, in
contrast, arises from more
centrally situated glands and is
more likely to produce urinary
obstruction early in its course
than is carcinoma.
Adult prostate
Prostate - Infarction
Infarction prostate
Gross appearance of infarct of
prostate. The lesion has a bright
red color (due to associated
hemorrhage, otherwise it is
yellow) and bulges on the cut
surface. Nodular hyperplasia is
also present.
Prominent metaplastic changes at the edge of a prostatic infarct. These are sometimes overdiagnosed as
carcinoma. The infarct is of ischemic type (coagulative).
Infarction prostate
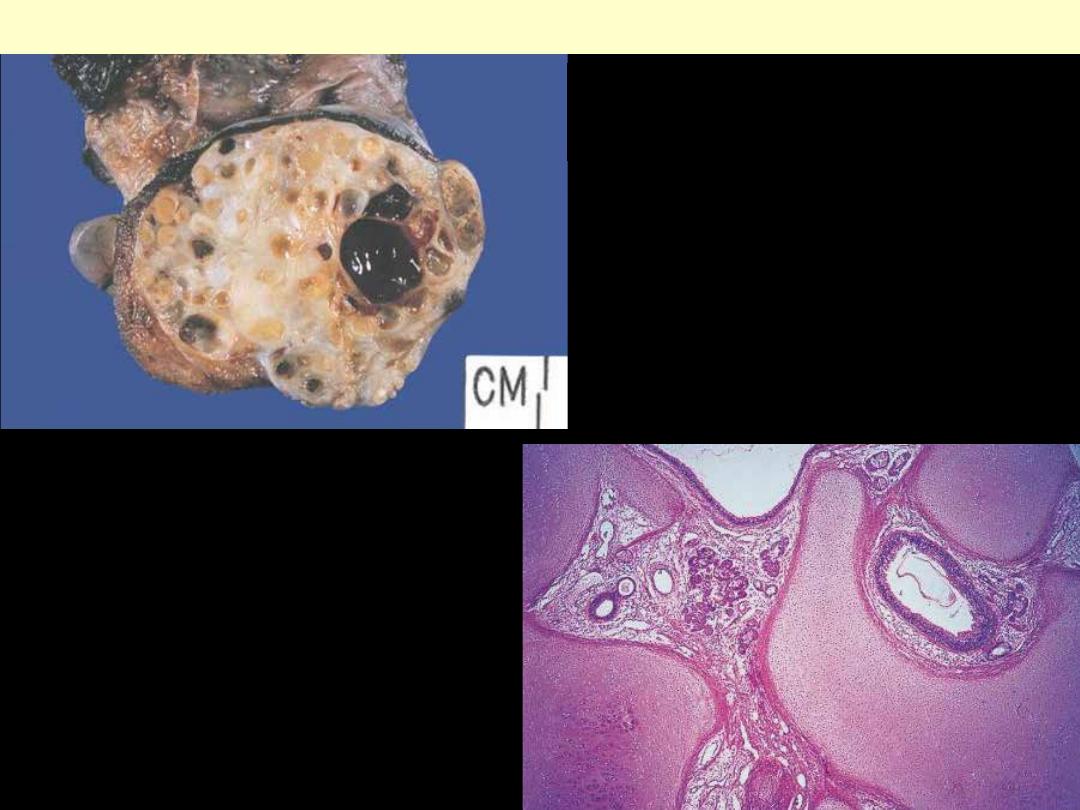
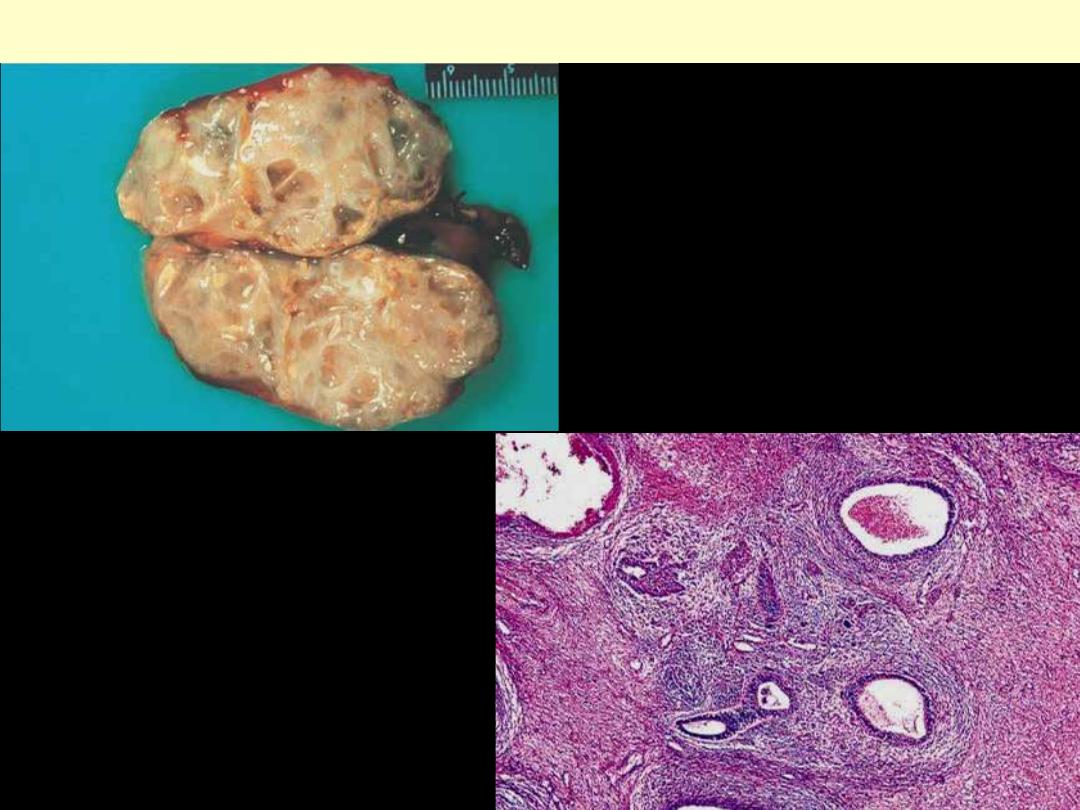
Prostatic hyperplasia - Benign
The nodules occur mainly in the lateral lobes. Such an enlarged
prostate can obstruct urinary outflow from the bladder and lead to an obstructive uropathy.
Benign prostatic hyperplasia (BPH)
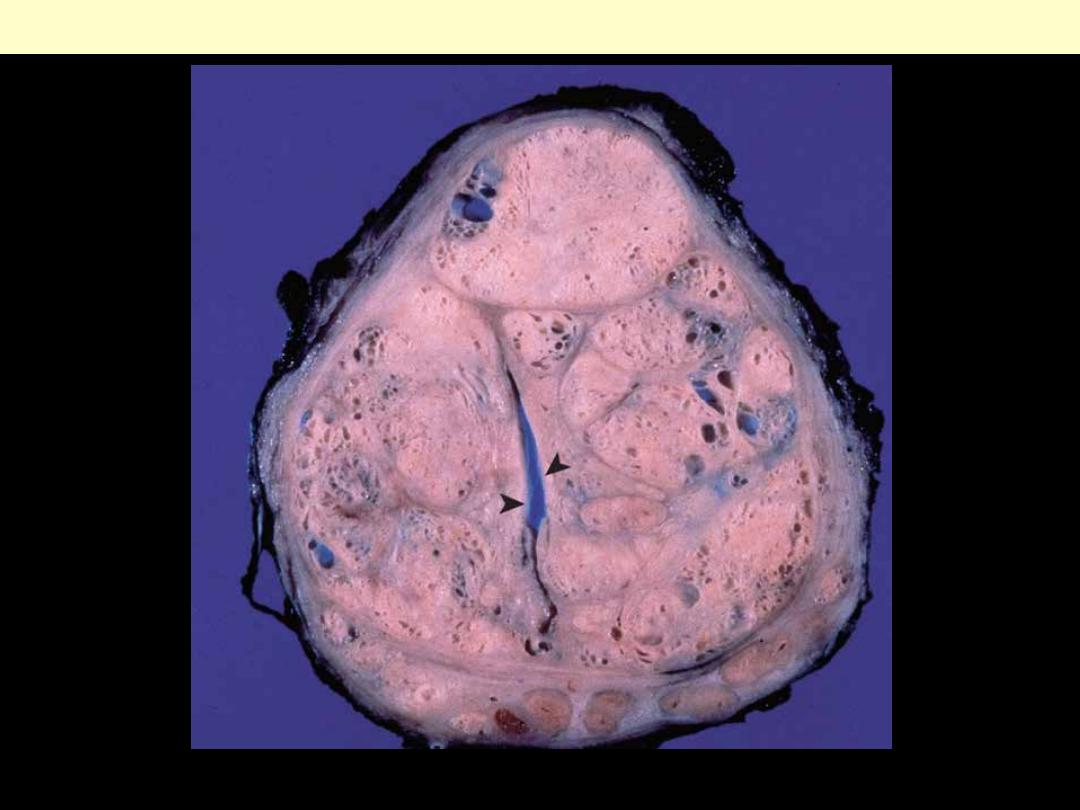
There are well-defined nodules that compress the urethra (arrowheads) into a slitlike lumen.
Nodular prostatic hyperplasia
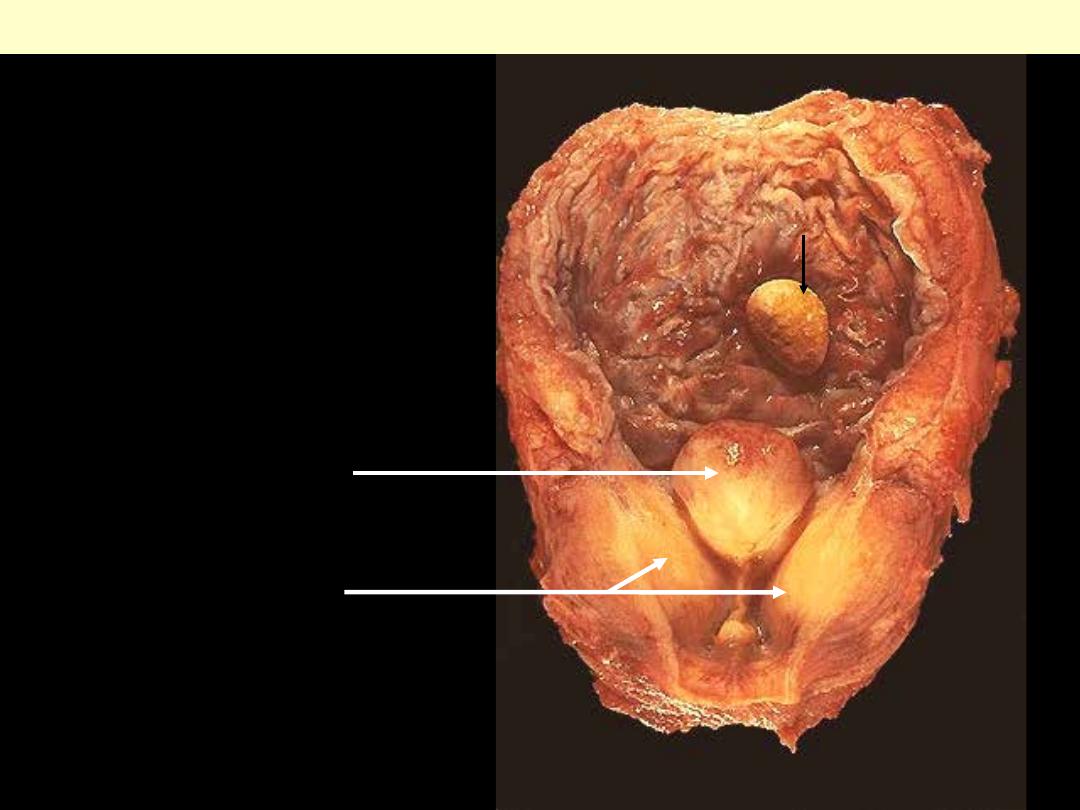
Enlarged lateral lobes and median lobe that
obstructs the prostatic urethra. This led to
obstruction with bladder hypertrophy, as
evidenced by the prominent trabeculation of
the mucosal surface. Obstruction with stasis
also led to the formation of the yellow-brown
stone (arrow).
Nodular prostatic hyperplasia
Median lobe
Lateral lobes
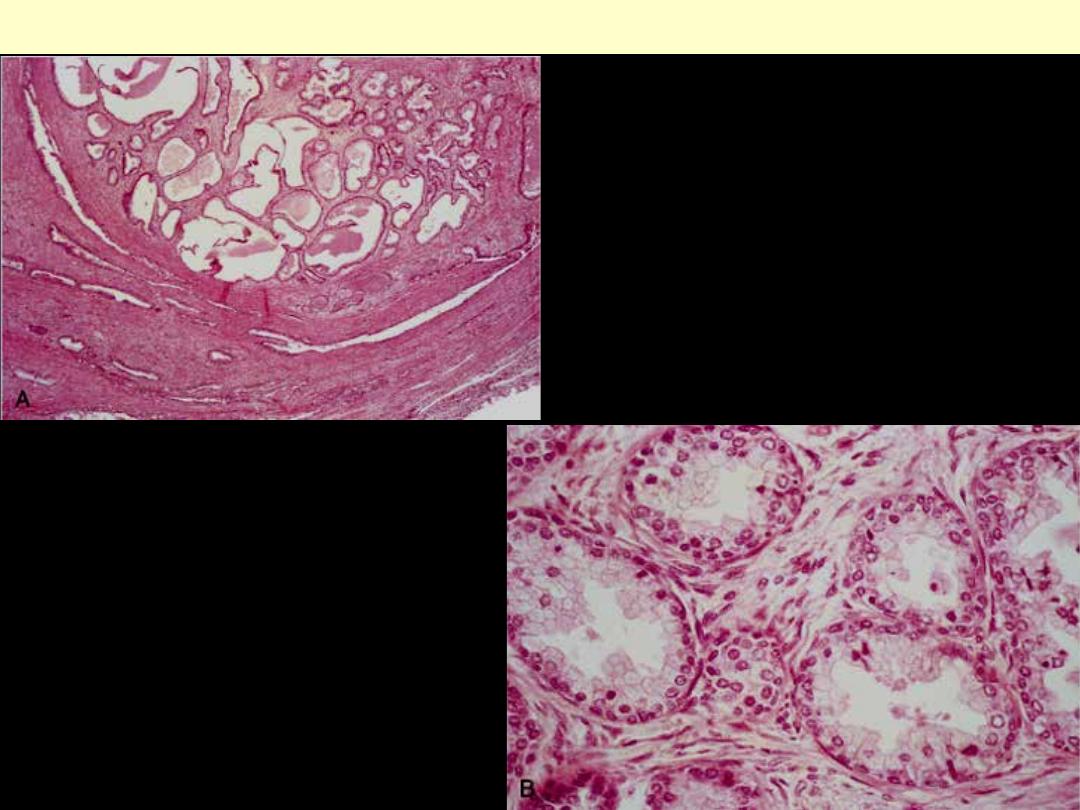
A, Low-power photomicrograph demonstrates a
well-demarcated nodule at the top of the field,
populated by hyperplastic glands. In other cases of
nodular hyperplasia, the nodularity is caused
predominantly by stromal, rather than glandular,
proliferation.
Prostatic nodular hyperplasia
B, Higher power photomicrograph
demonstrates the morphology of the
hyperplastic glands, with the characteristic
dual cell population: the inner columnar
secretory cells, and the outer flattened basal
cell layer.
The hyperplasia can involve both glands and stroma, though the
former is usually more prominent. Here, a large hyperplastic nodule of glands is seen.
Benign prostatic hyperplasia (BPH)
Scrotum – Bowenoid papulosis
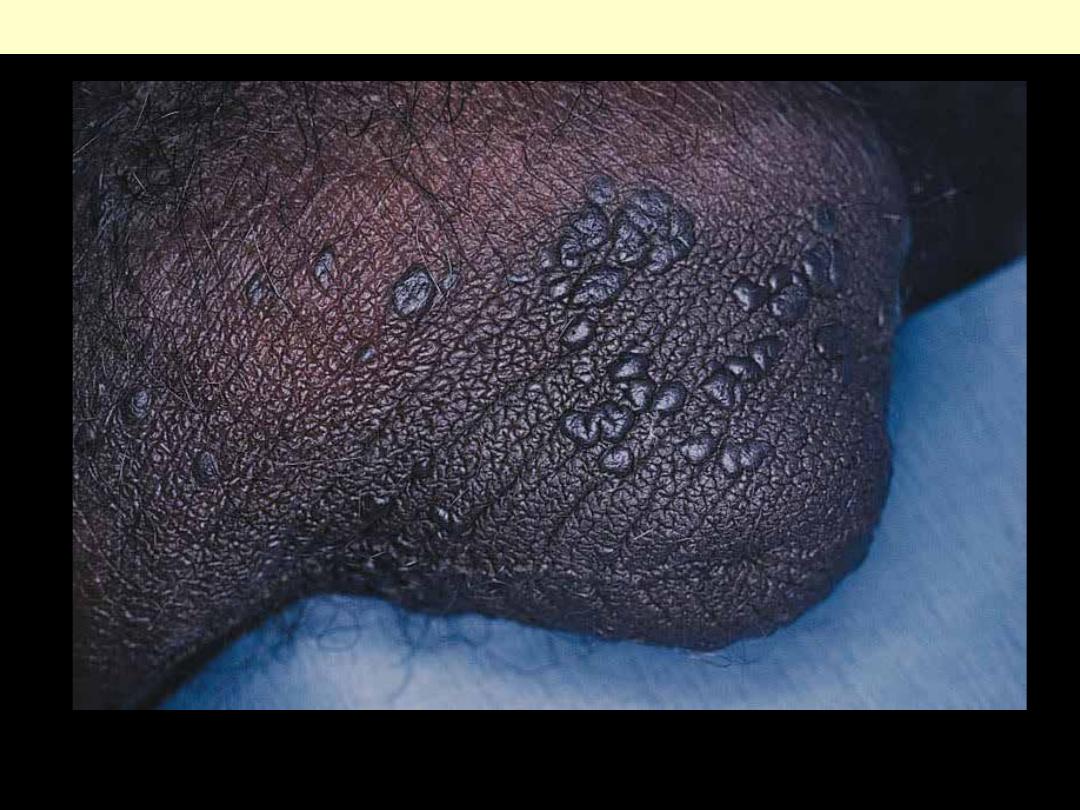
Clinical appearance of bowenoid papulosis in the skin of the scrotum. The lesions are small, multiple,
and hyperpigmented.
Bowenoid papulosis of the scrotum
Testis - Atrophy
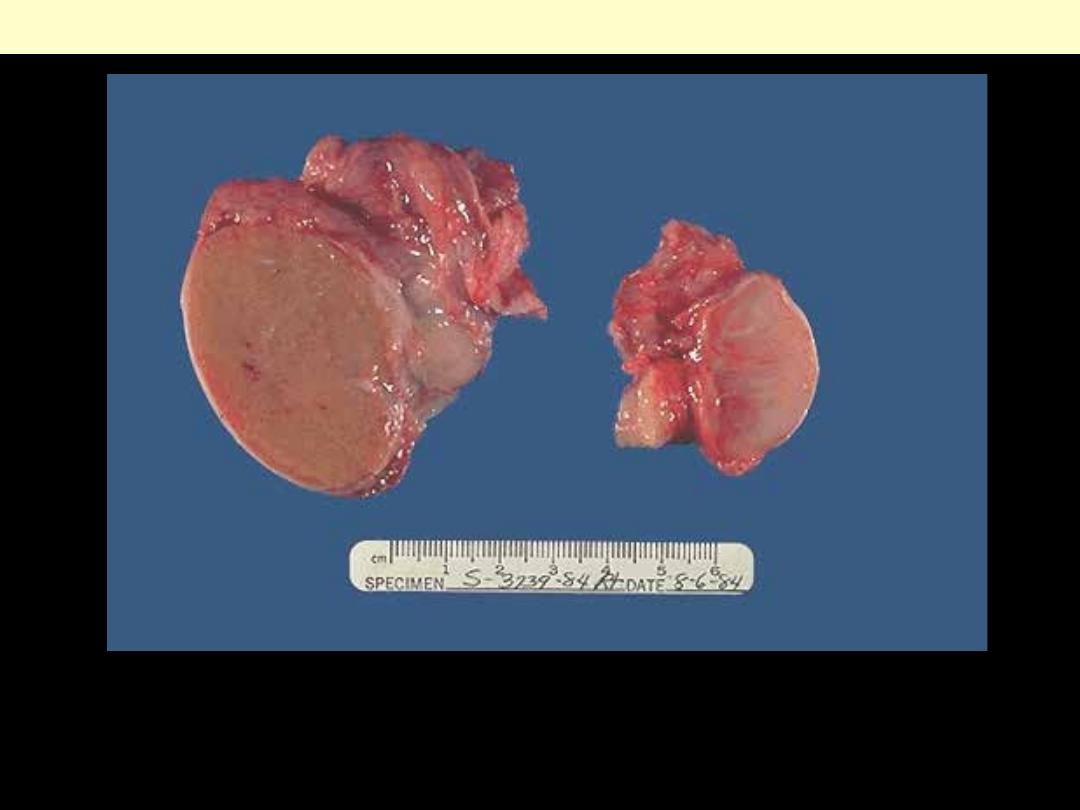
On the left is a normal testis. On the right is a testis that has undergone atrophy. Bilateral atrophy may
occur with a variety of conditions including chronic alcoholism, hypopituitarism, atherosclerosis,
chemotherapy or radiation, and severe prolonged illness. A cryptorchid testis will also be atrophic.
Inflammation may lead to atrophy including mumps.
Normal Vs testicular atrophy
Testis - Tumors
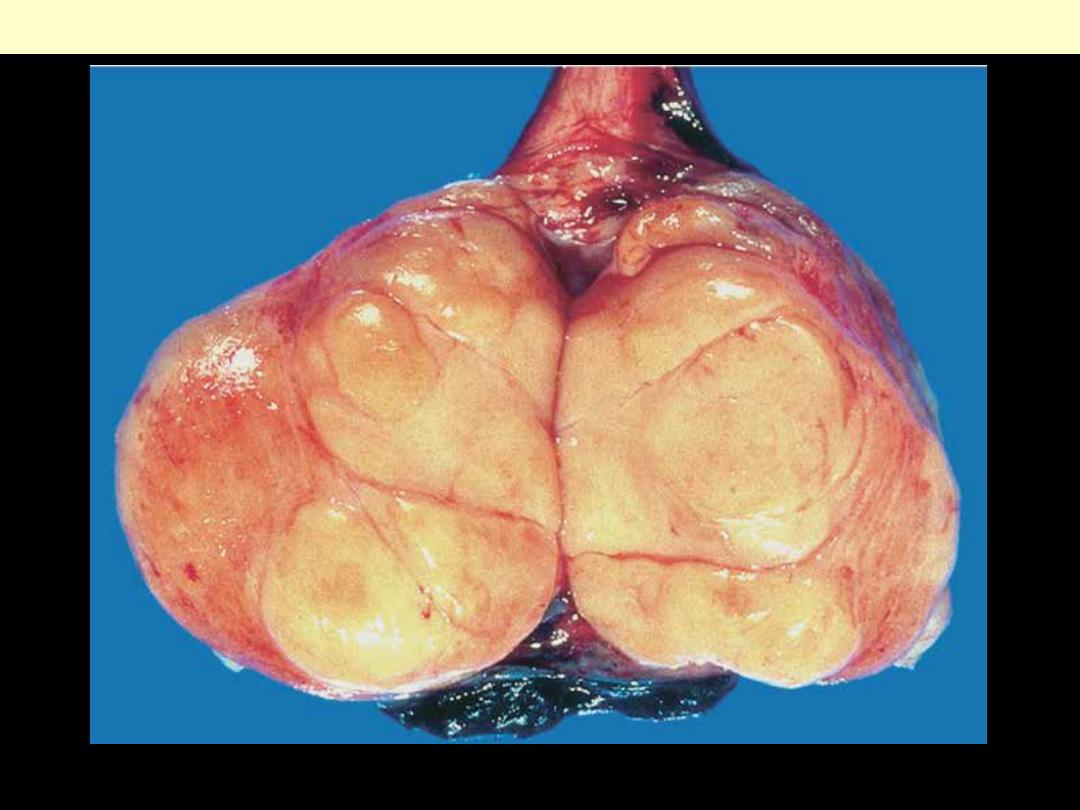
The tumor appears as a fairly well circumscribed, pale, fleshy, homogeneous mass
Seminoma of the testis
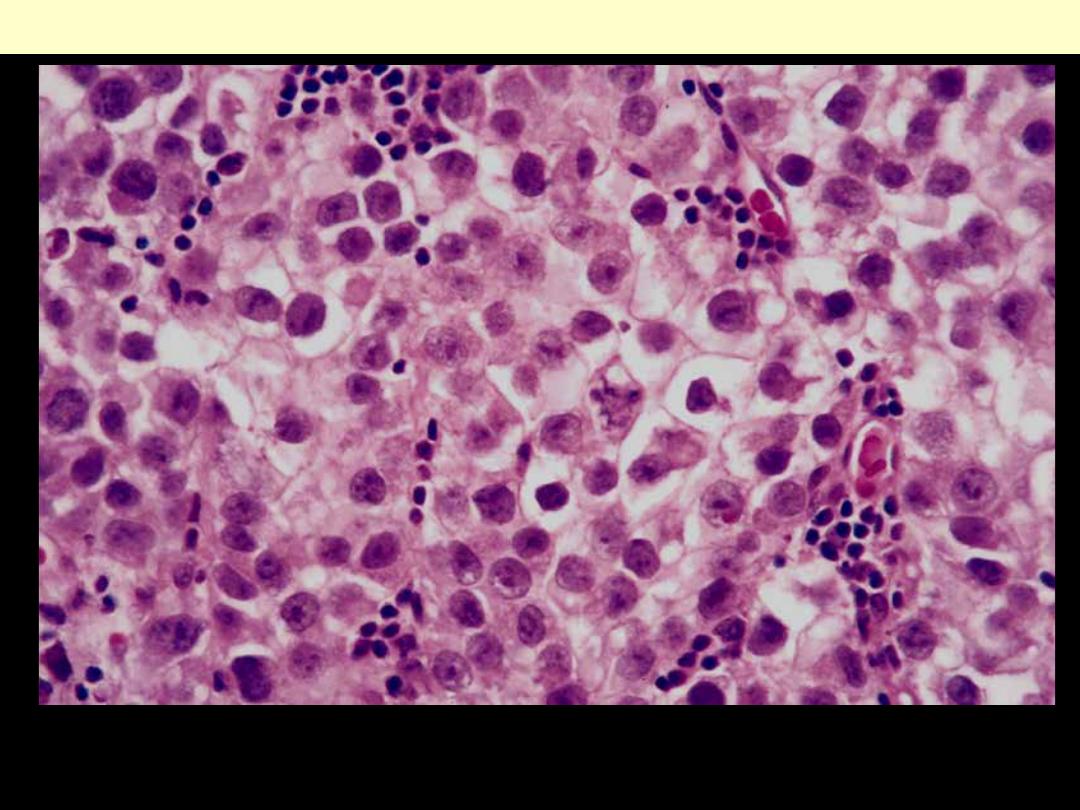
Large cells with distinct cell borders, clear cytoplasm, rounded nuclei, prominent nucleoli, and a sparse
lymphocytic infiltrate.
Seminoma of the testis
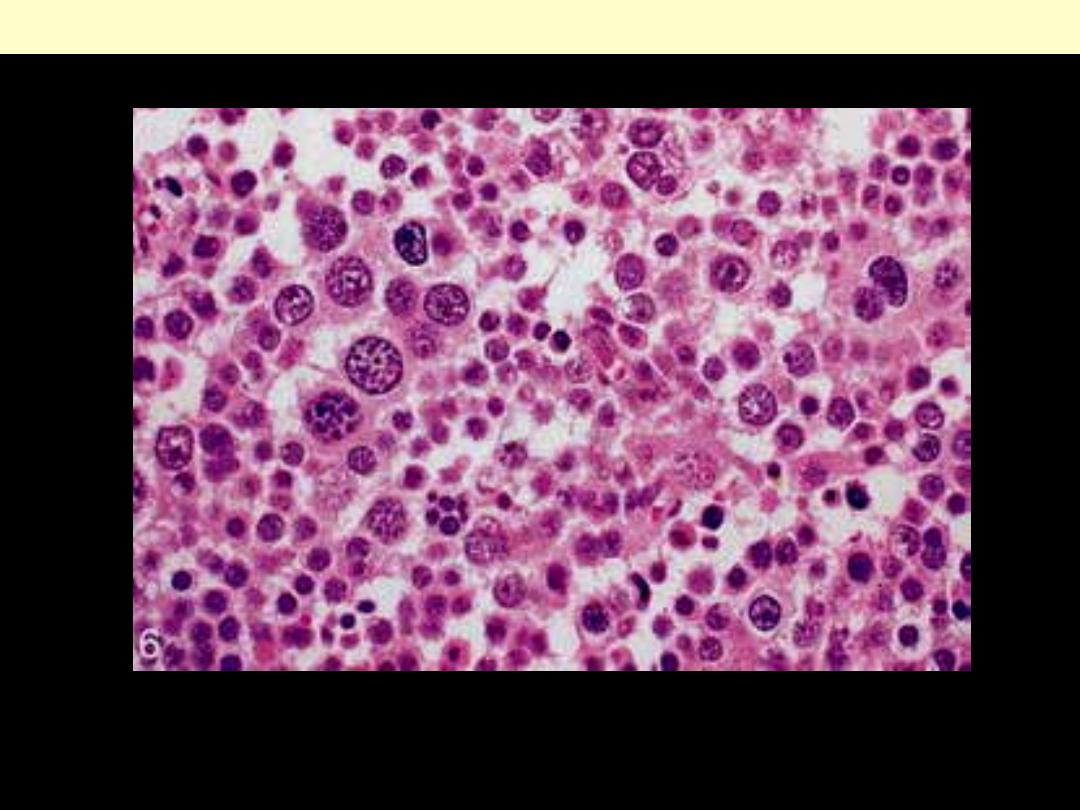
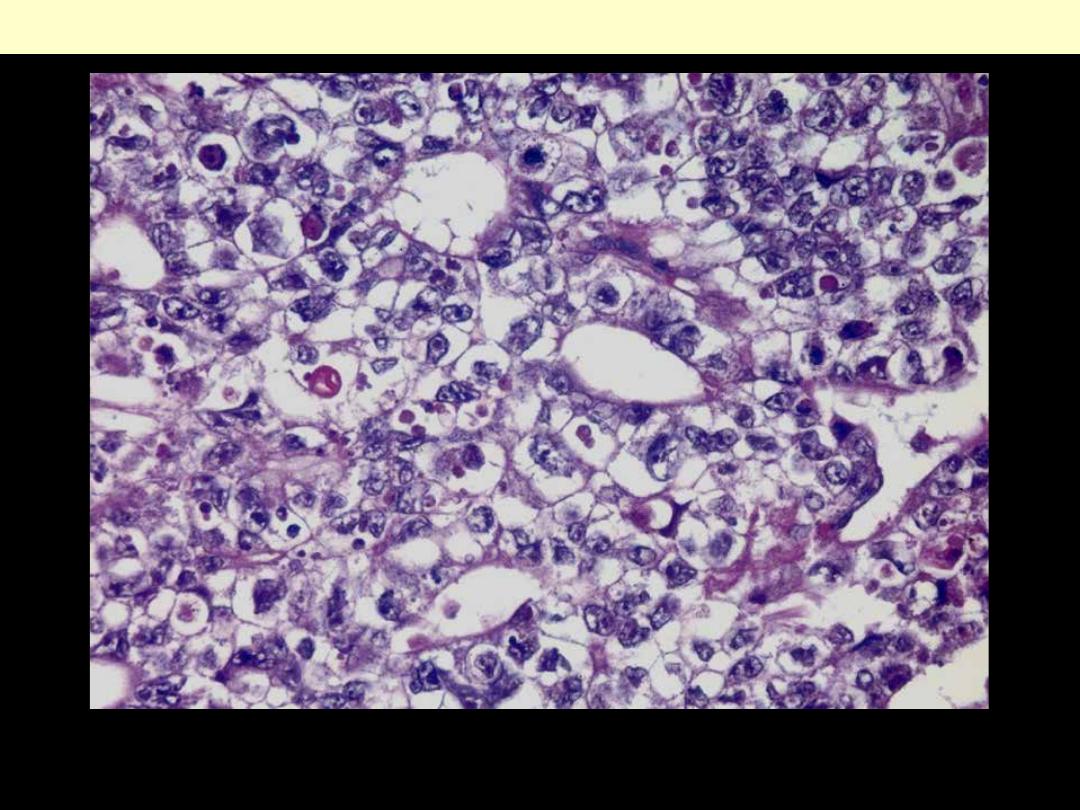
There is diffuse proliferation of tumor cells with characteristic spireme-type chromatin pattern
Spermatocytic seminoma
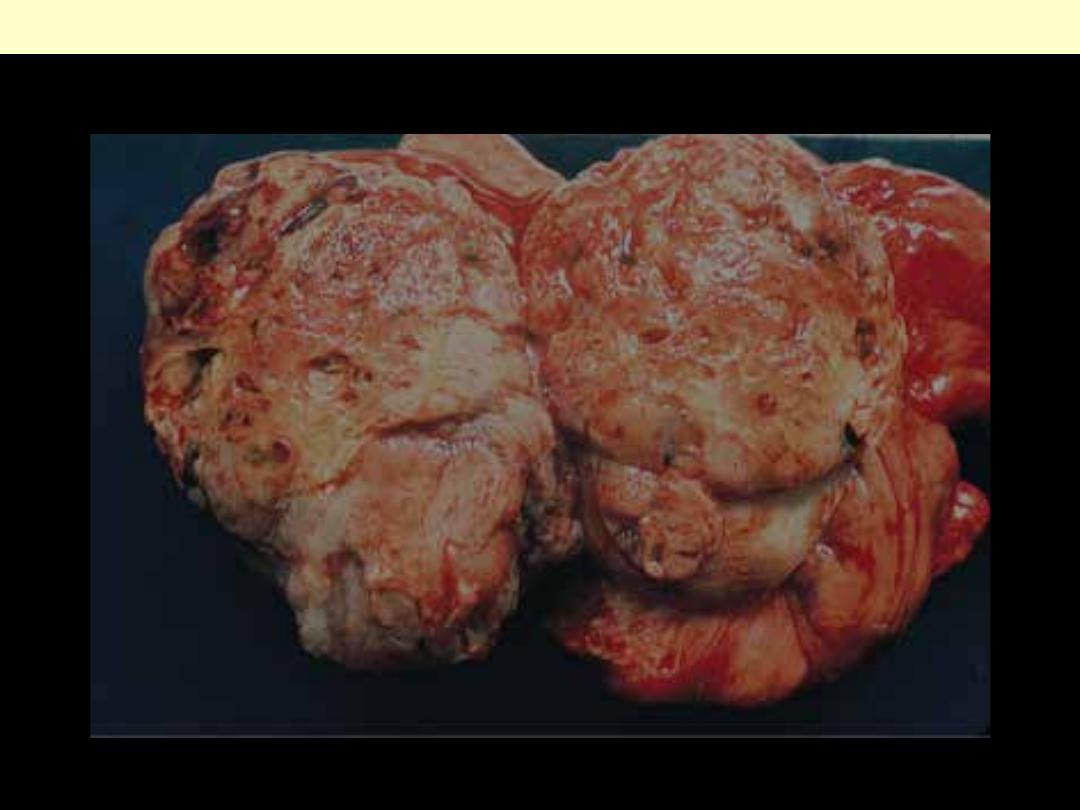
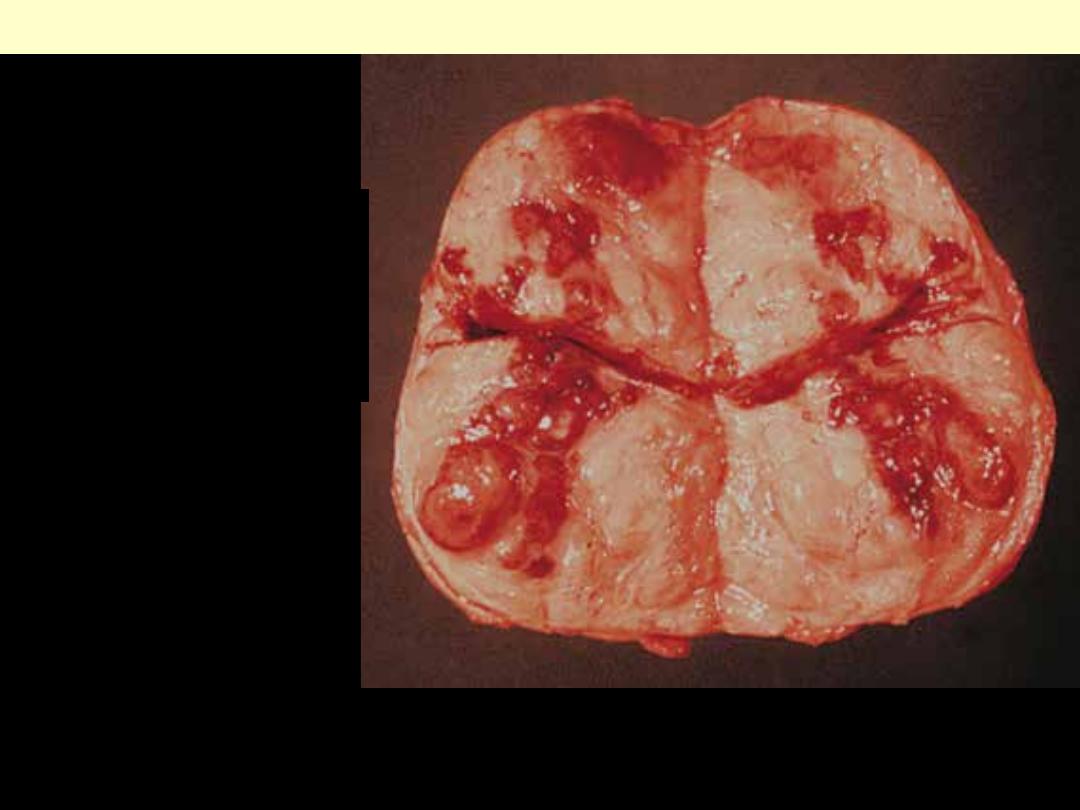
Embryonal ca testis
This shows solid nodular invasive (ill-defined) cut surface with numerous areas of necrosis and hemorrhage.
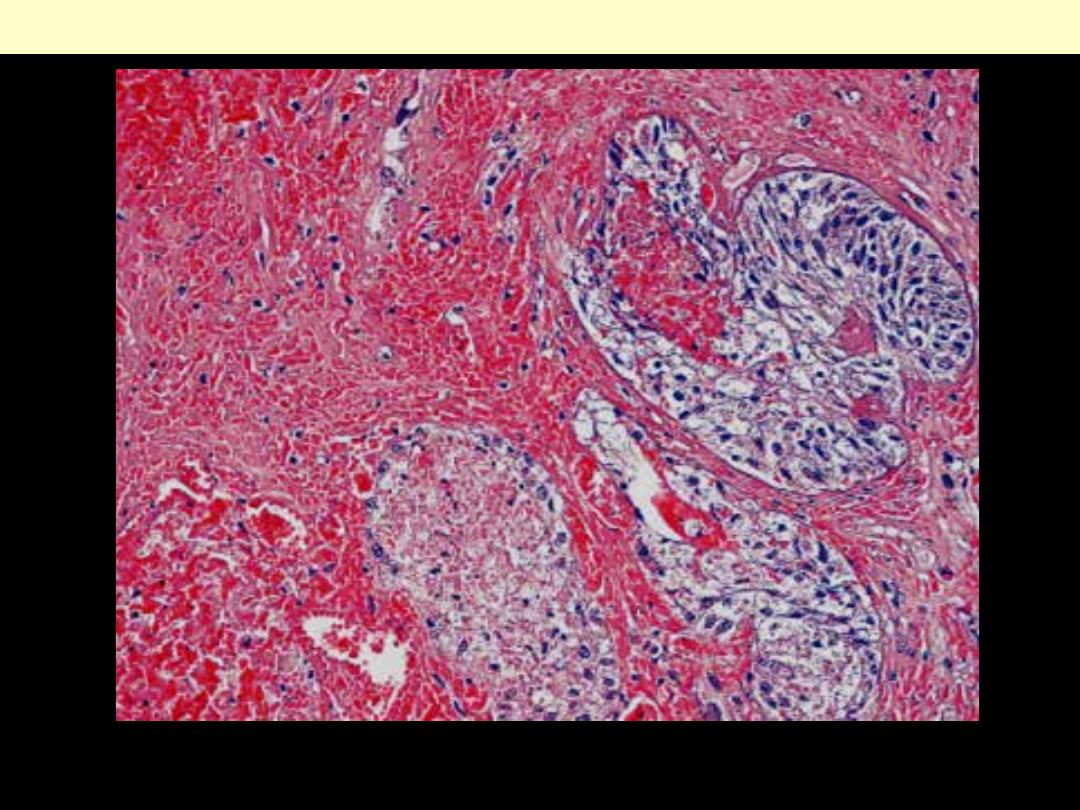
Sheets of undifferentiated cells as well as primitive glandular differentiation. The nuclei are large and
hyperchromatic with prominent nuclei
Embryonal carcinoma
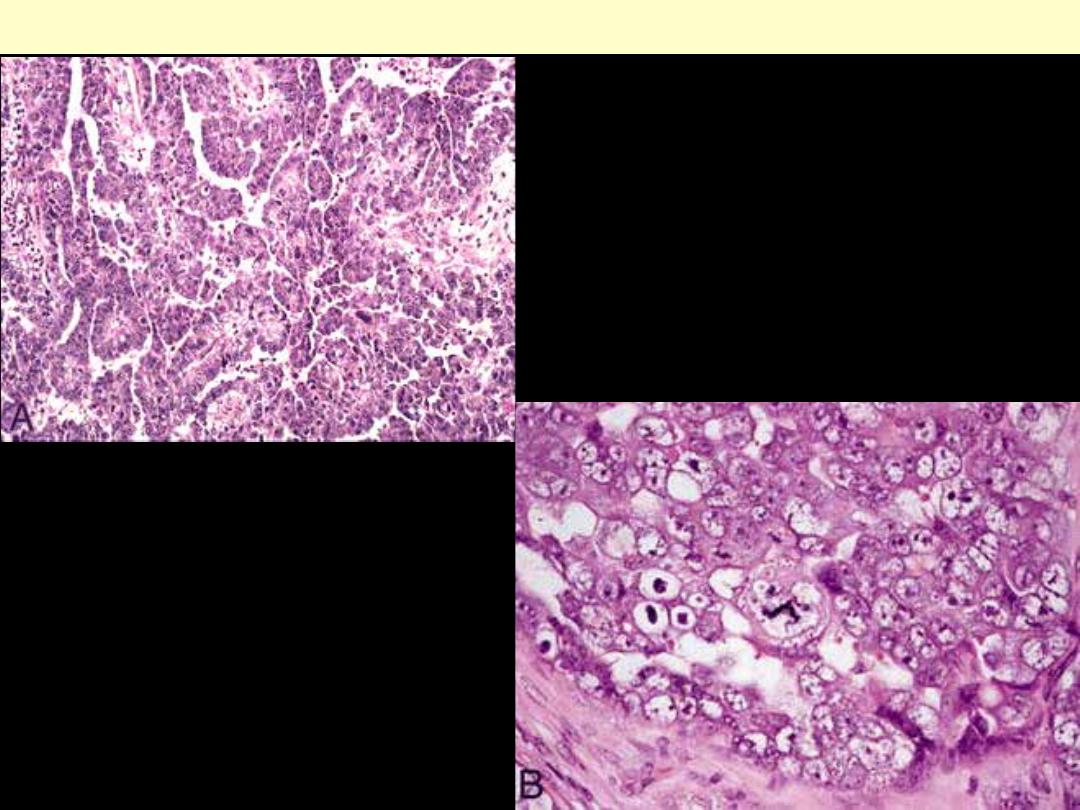
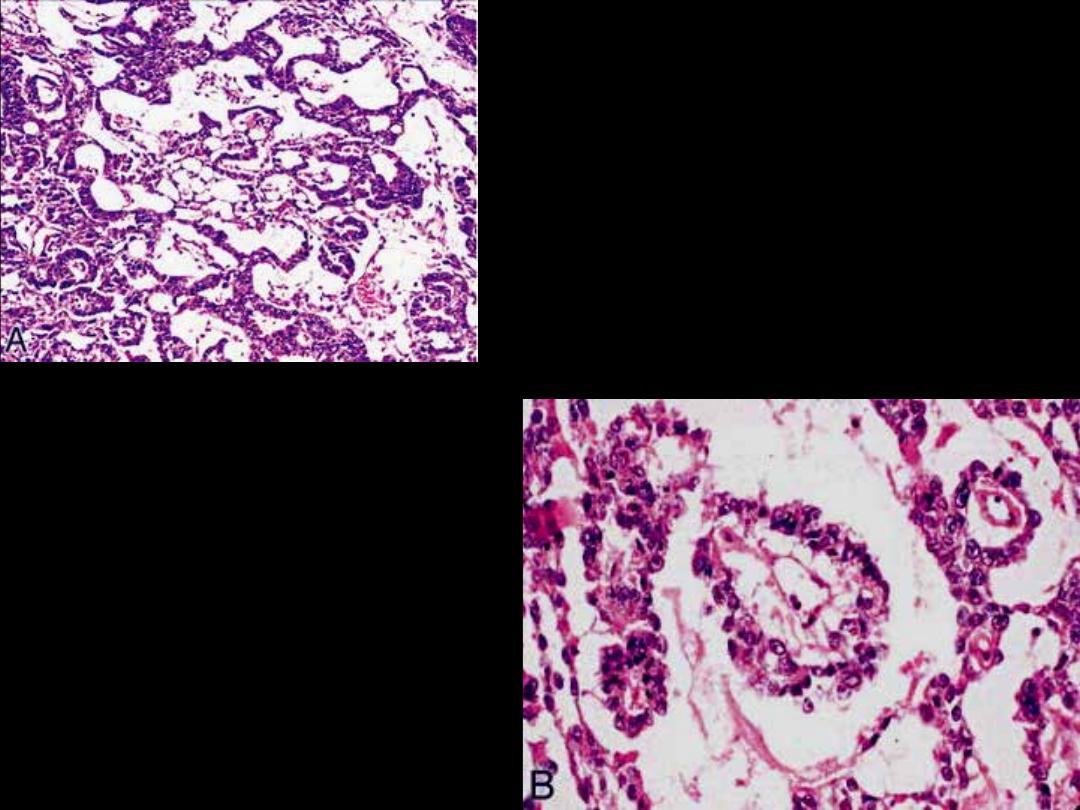
A, Embryonal carcinoma displaying a papillary
pattern of growth (hematoxylin-eosin,
original magnification ×100). B, Embryonal
carcinoma cells characterized by marked
anaplasia and abnormal mitotic figures
(hematoxylin-eosin, original magnification
×400)
Embryonal carcinoma
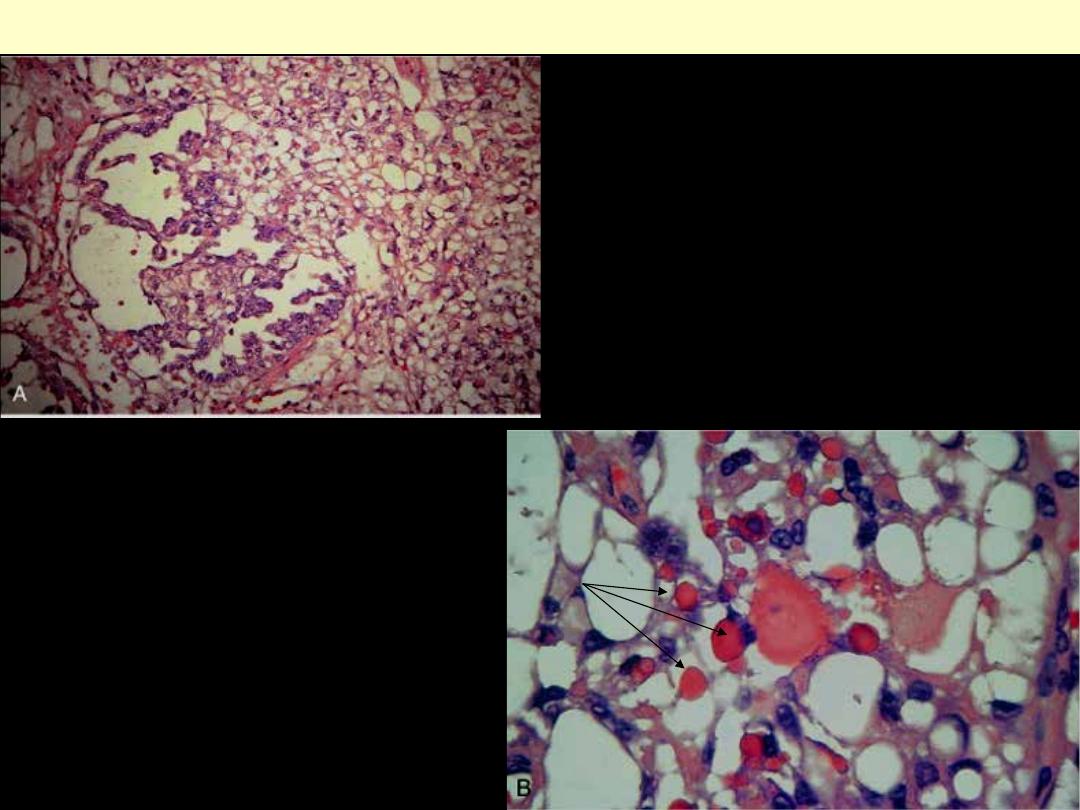
A, Low-power photomicrograph demonstrating
areas of loosely textured, microcystic tissue and
a papillary structure.
B, Higher power photomicrograph
demonstrating characteristic hyaline droplets
within the microcystic areas of the tumor.
Yolk sac (endodermal sinus) tumor
A, Yolk sac tumor with a reticular, microcystic pattern
characterized by thin anastomosing cords and loose
spaces (hematoxylin-eosin, original magnification
×100). B, Yolk sac tumor showing classic Schiller-
Duval bodies with a central fibrovascular core
surrounded by malignant cuboidal to columnar
cells (hematoxylin-eosin, original magnification
×400)
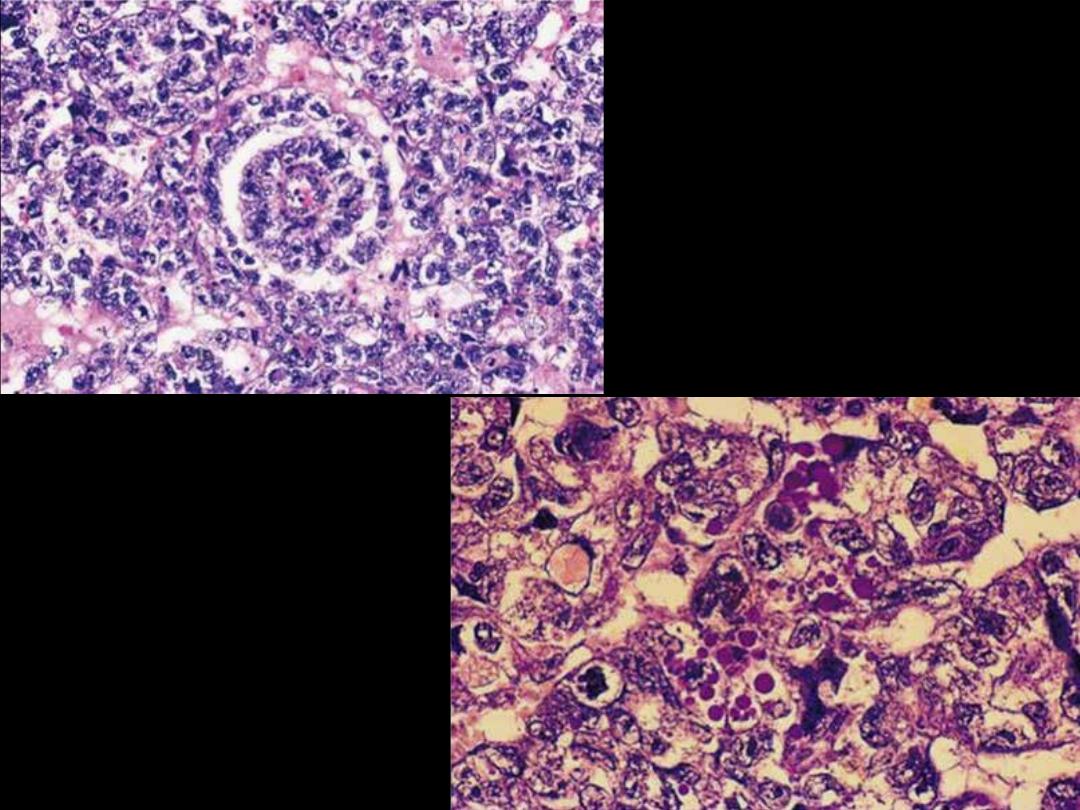
Pleomorphism and hyaline globules in
yolk sac tumor of testis.
Schiller-Duval body in yolk sac tumor of
testis.
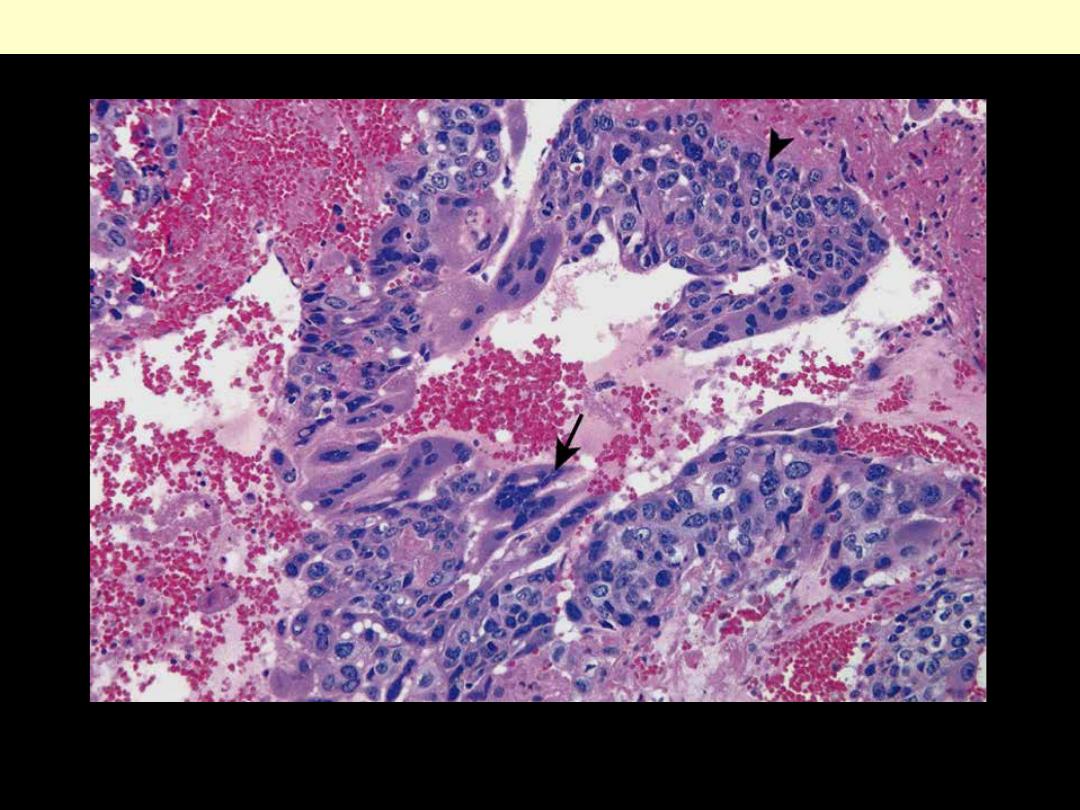
The tumour shows cytotrophoblastic cells with central nuclei (arrowhead, upper right) and
syncytiotrophoblastic cells with multiple dark nuclei embedded in eosinophilic cytoplasm (arrow,
middle). Hemorrhage and necrosis are prominent.
Choriocarcinoma
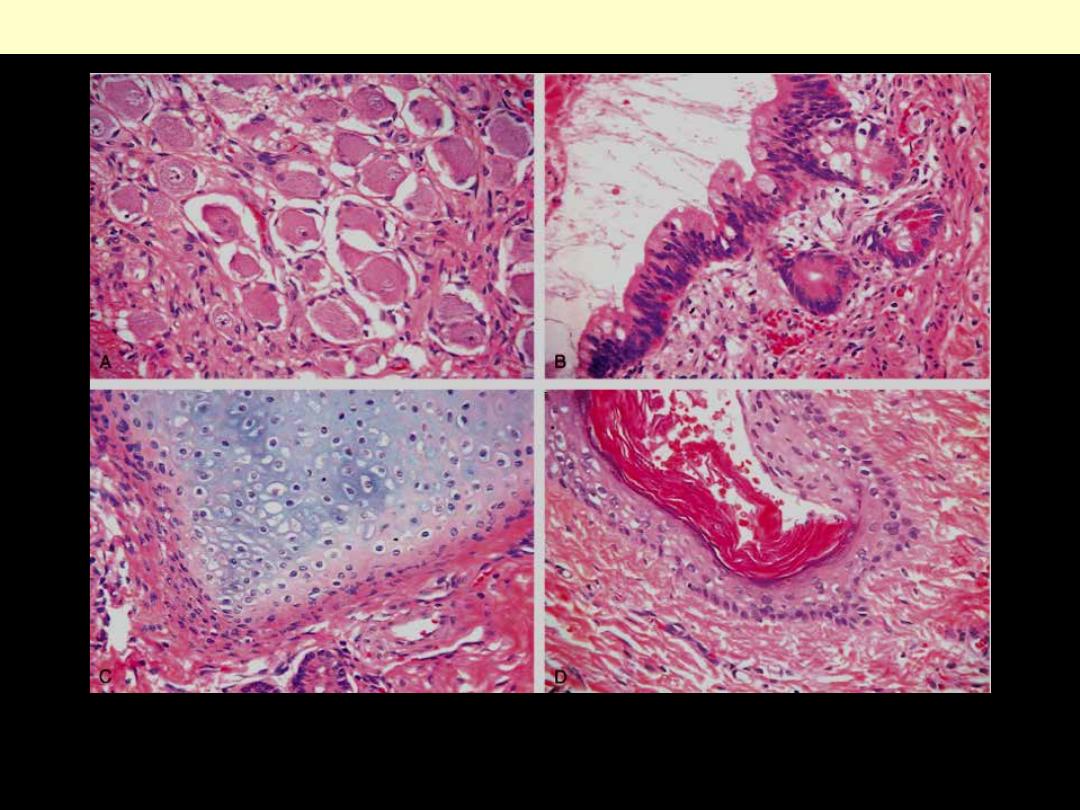
These tumors contain mature cells from endodermal, mesodermal, and ectodermal lines. Pictured here
are four different fields from the same tumor containing (A) neural (ectodermal), (B) glandular
(endodermal), (C) cartilaginous (mesodermal), and (D) squamous epithelial elements.
Testicular teratomas
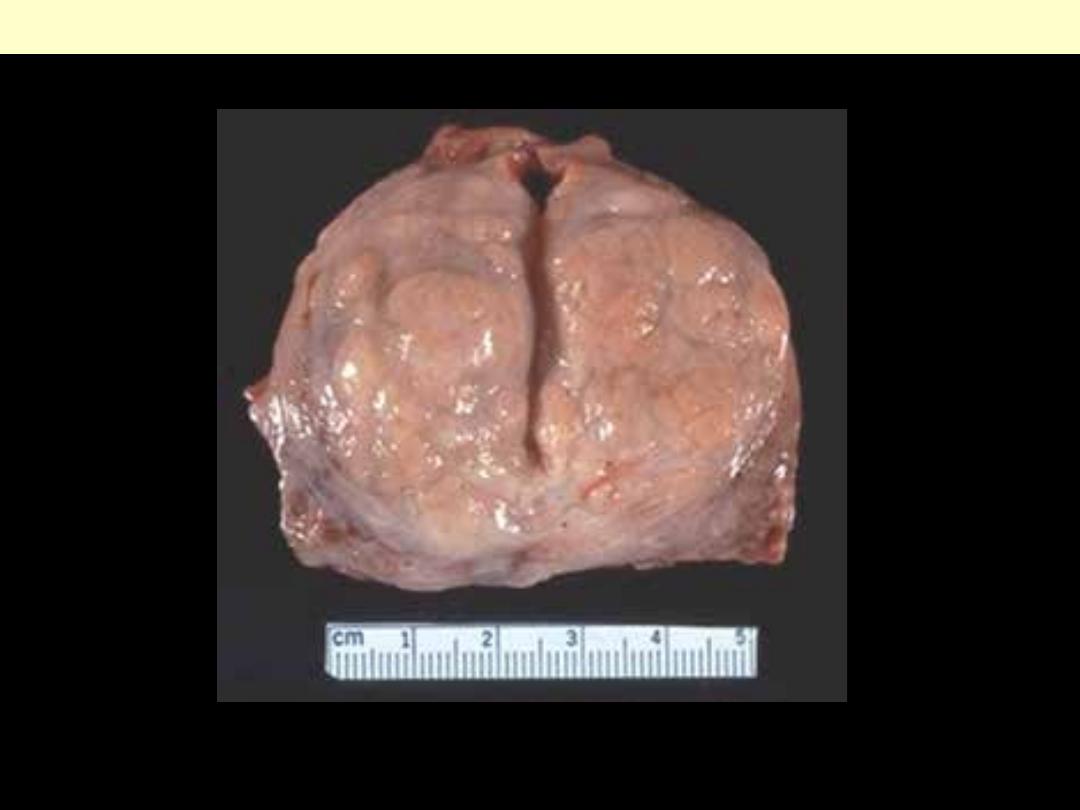
Mature teratoma testis gross
There are multiple cystic areas, lobules of
mature adipose tissue, and shiny solid nodules
corresponding to well-differentiated cartilage.
Large islands of cartilage are seen surrounding
well-differentiated glandular structures.
Immature teratoma testis
Microscopic appearance. Hypercellular
stroma is seen growing in a concentric fashion
around glandular formations.
