
DISEASES OF THE
FEMALE GENITAL
TRACT
Part 3
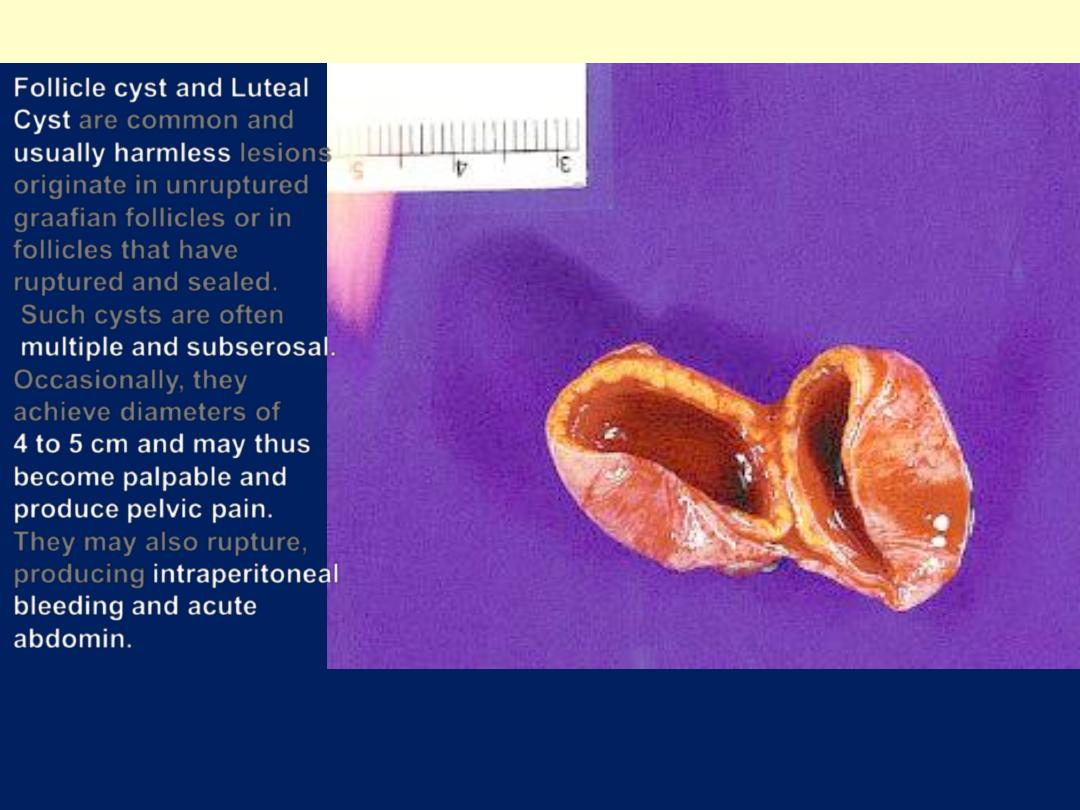
Luteal Ovarian Cyst
The luminal content is typically hemorrhagic. Note the golden
yellow rim
Follicle cyst and Luteal
Cyst
are common and
usually harmless
lesions
originate in unruptured
graafian follicles or in
follicles that have
ruptured and sealed.
Such cysts are often
multiple and subserosal.
Occasionally, they
achieve diameters of
4 to 5 cm and may thus
become
palpable
and
produce
pelvic pain
.
They may also rupture,
producing
intraperitoneal
bleeding
and acute
abdomin.
(Stein-Leventhal syndrome)
Oligomenorrhea
,
hirsutism
,
infertility
, and
sometimes
obesity
may appear in young women
secondary to
excessive production of androgen
(which inhibit FSH and ovulation)
by multiple
cystic follicles in the ovaries
.
Microscopically
,
there is a thickened, fibrotic
tunica with underlying follicular cysts
.
The diagnosis of this syndrome can not be made
on morphological grounds alone; both clinical &
endocrine data are also required.
TUMORS OF THE OVARY
Tumors of the ovary are diverse and this
diversity is attributable to the three cell types
that make up the normal ovary:
1. The surface (coelomic) covering epithelium
2. The germ cells
3. The sex cord/stromal cells.
Each of these cell types gives rise to
a variety of
tumors.
Neoplasms of surface epithelial
constitute the great majority of primary
ovarian tumors (70%), and their
malignant forms account for 90% of
ovarian cancers.
Germ-cell and sex cord/stromal cell
tumors constitute 20% to 30% of
ovarian tumors, but are collectively
responsible for fewer than 10% of
malignant tumors.
Pathogenesis of ovarian cancer
Nulliparity ,unmarried ,low parity and family
history
Up to10% of ovarian cancers are familial
; the
majority of these hereditary cancers seem to be
caused by
mutations in BRCA1 and BRCA2
genes,
these are also associated with hereditary
breast cancer.
Other molecular changes of ovarian neoplasms
include
HER2/NEU & K-RAS proteins
over-expression and p53 mutation.
The latter is
present in about 50% of all ovarian cancers.
Surface Epithelial Tumors
These neoplasms are derived from the surface
coelomic mesothelial covering of the ovary.
repeated ovulation & scarring the surface
epithelium is pulled into the subjacent cortex,
forming small epithelial cysts. These can undergo
metaplasia with subsequent neoplastic
transformation.
The surface epithelial tumors also have an
intermediate, borderline category
referred to as
tumors of low malignant potential
.
These seem
to be
low-grade cancers with limited invasive
potential.
Thus, they have a better prognosis
than the fully malignant ovarian carcinomas.
• Surface epithelial tumors are divided into:
• serous
• mucinous
• endometrioid
• Brenner tumors.
A.Serous Tumors
Are the most frequent of the ovarian
tumors.
Combined, borderline and frankly
malignant serous carcinomas are the
most
common malignant ovarian tumors (60% of
all ovarian cancers).
Benign lesions are usually encountered
around 35 years of age, and malignant
ones around 55.
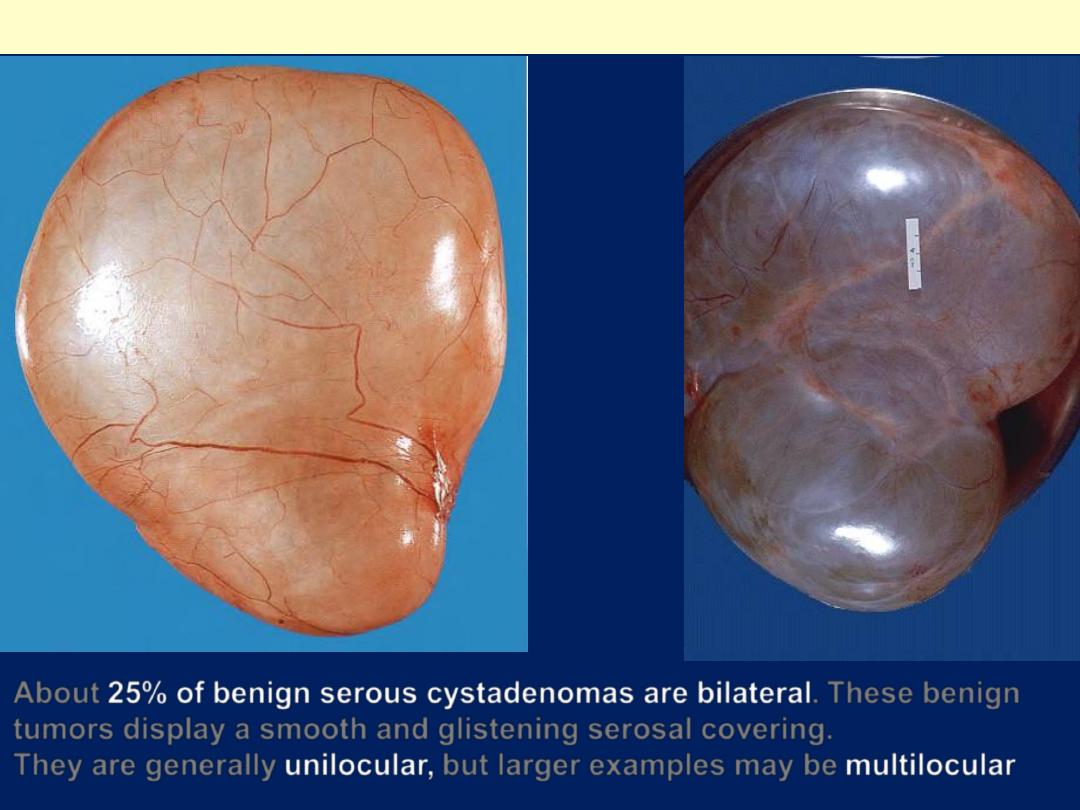
About
25% of benign serous cystadenomas are bilateral
. These benign
tumors display a smooth and glistening serosal covering.
They are generally
unilocular,
but larger examples may be
multilocular
Benign serous cystadenoma
The lining of serous cystadenoma is usually smooth but occasionally show papillary
structures protruding within. The cyst is usually filled by serous fluid.
Benign serous cystadenoma
Note the papillary
projections in the
lumen of the cyst,
and also on its
surface. In a
benign papillary
cystadenoma the
papillae are
present only on the
inner surface of the
cyst.
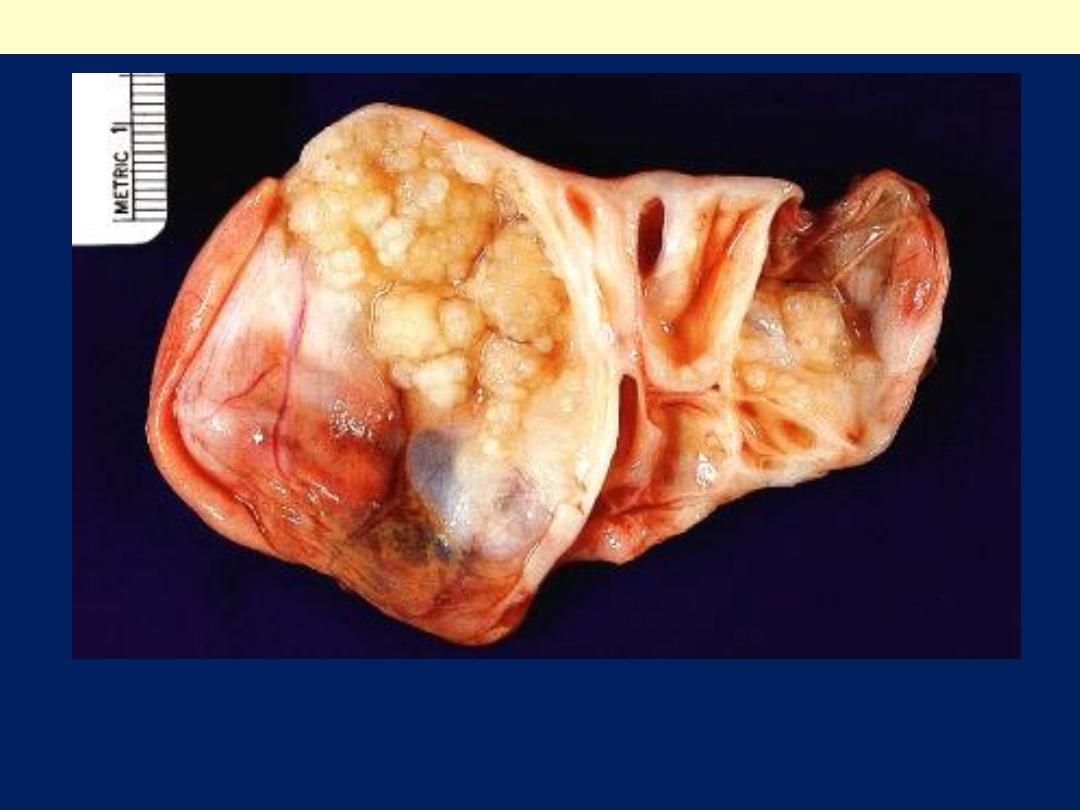
Papillary cystadenocarcinoma of the ovary.
This 17 cm serous
cystadenocarcinoma
was discovered during
exploratory laparotomy
of a woman who
presented with intestinal
obstruction, which was
caused by extrinisic
compression of the
bowel by one of the
many intra-abdominal
metastases of this
tumor. Grossly, the
tumor's cut surface
demonstrates both
cystic and papillary
architectural patterns.
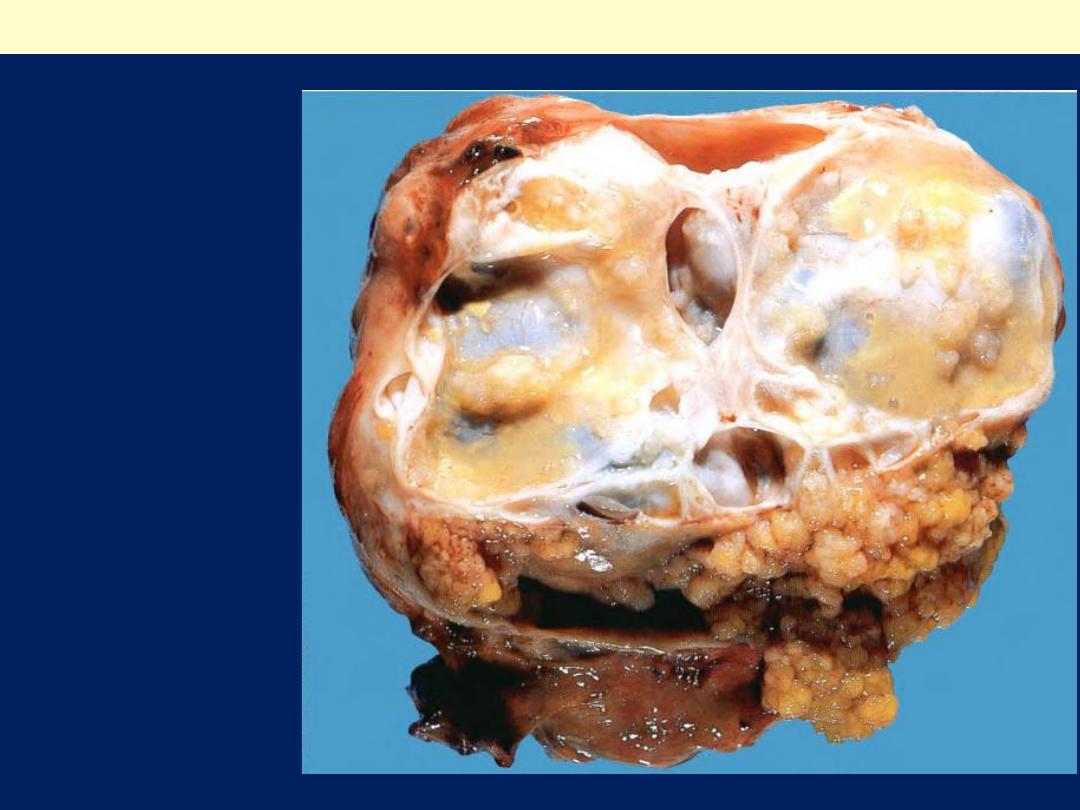
Papillary cystadenocarcinoma of the ovary.
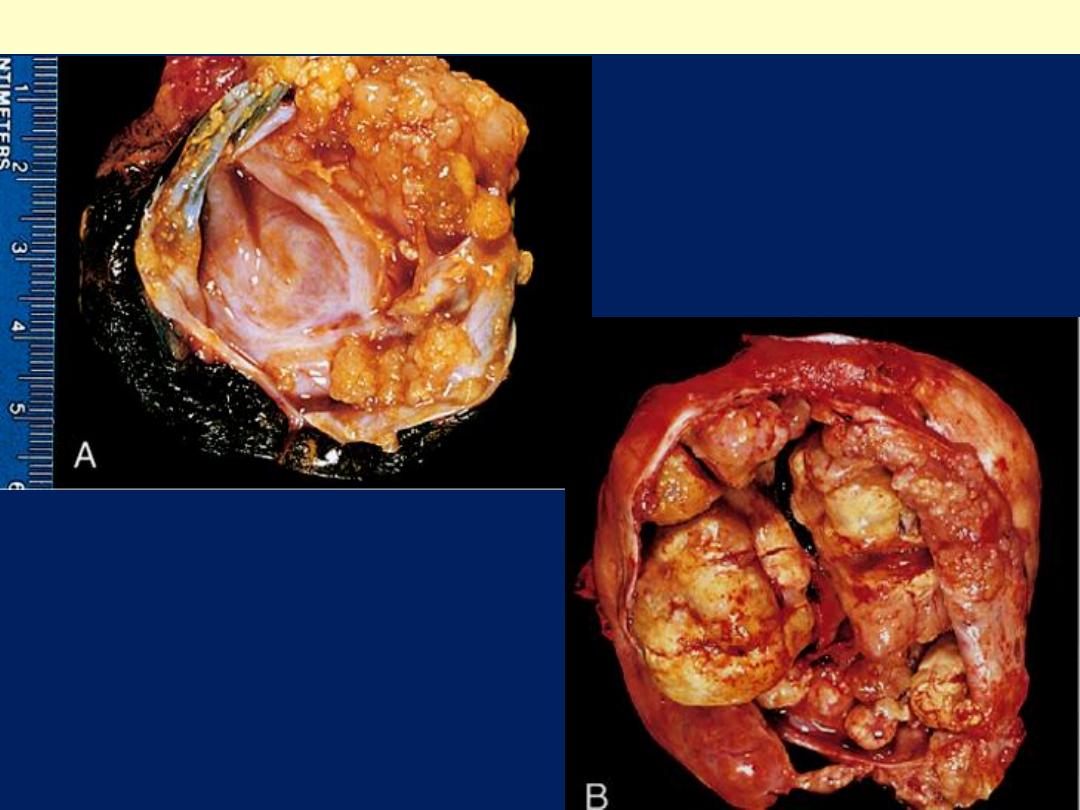
A, Borderline serous
cystadenoma opened to
display a cyst cavity
lined by delicate
papillary tumor growths.
Serous cystic tumors: borderline Vs malignant
B, Cystadenocarcinoma.
The cyst is opened to reveal
a large, bulky tumor mass.
Benign serous cystadenoma
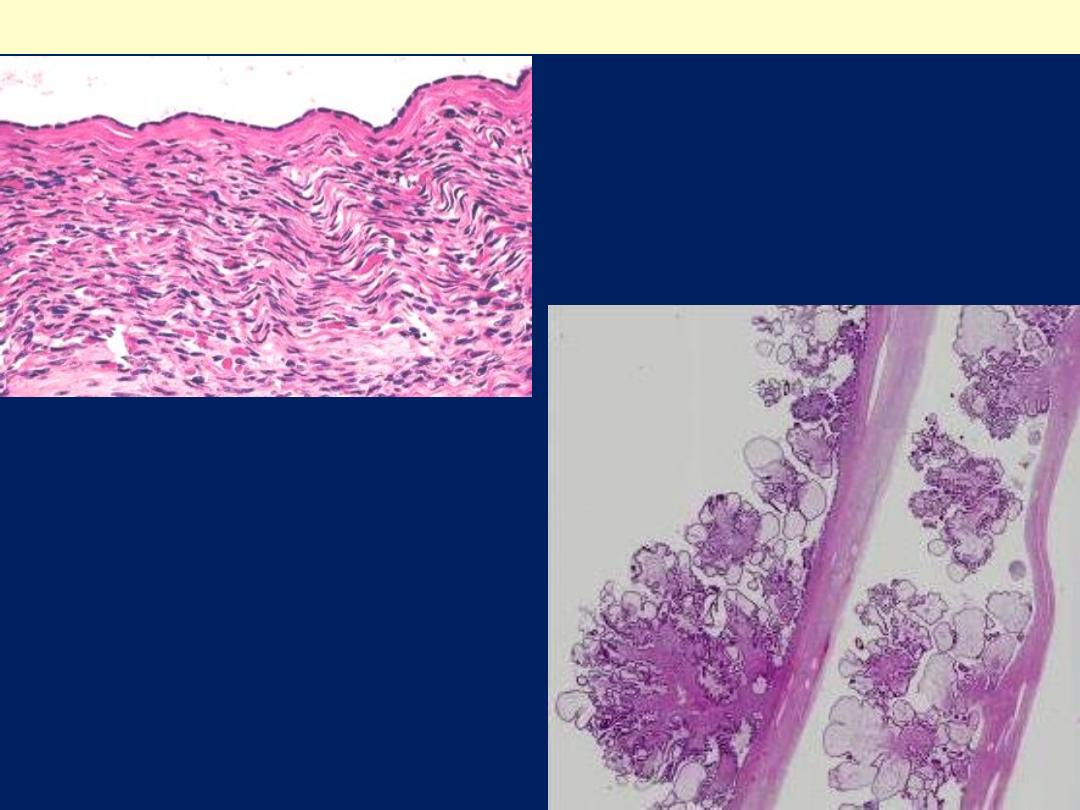
Single layer of bland-looking
epithelial cells lining one of the
cystic structures of a serous
cystadenoma.
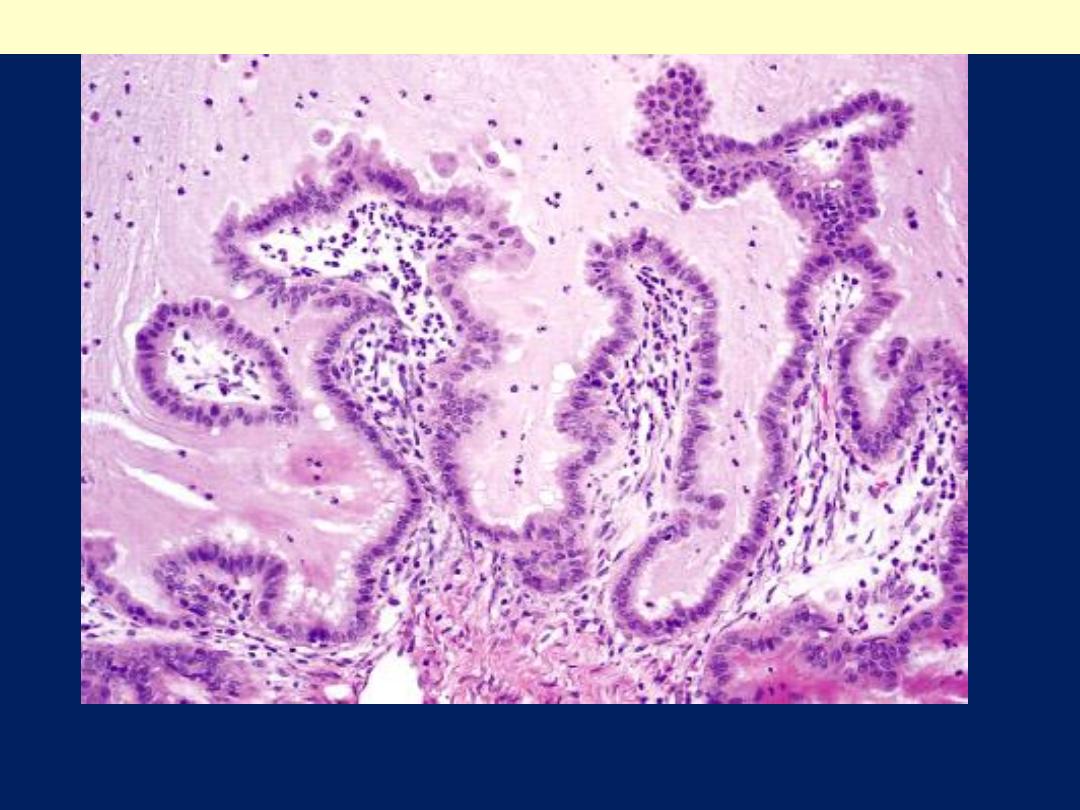
Papillary areas in serous
cystadenoma
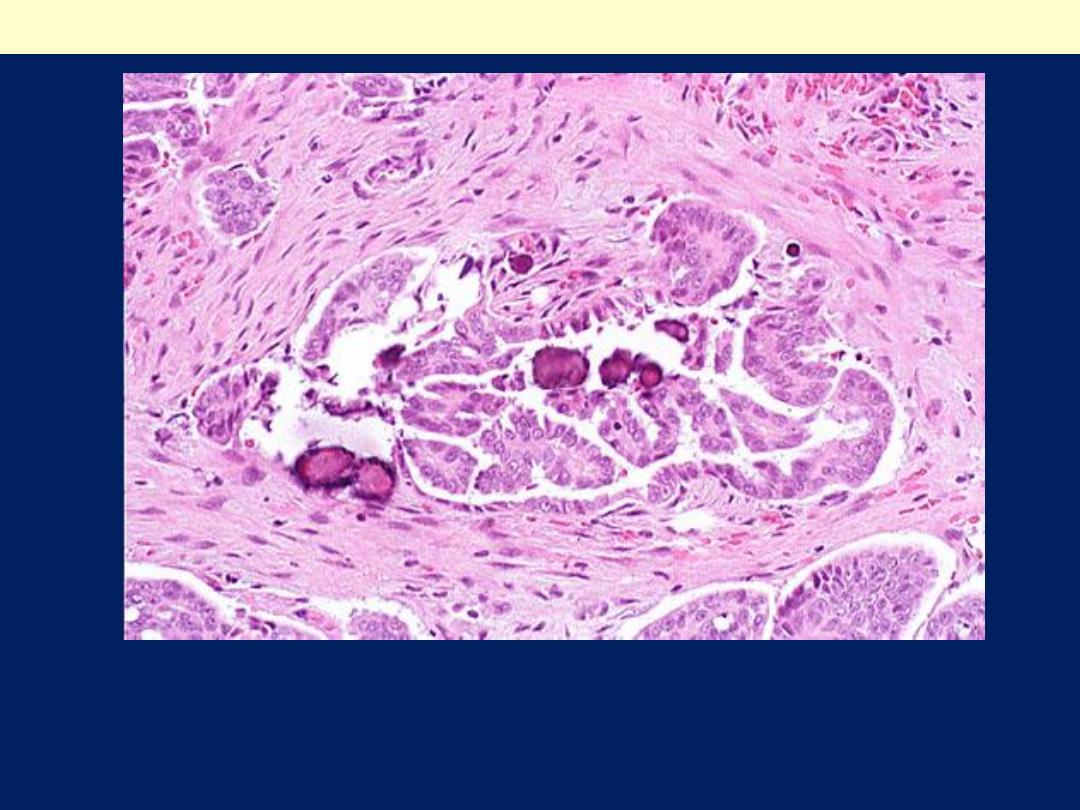
Ovarian papillary serous cystadenocarcinomas may contain small
concretions called psammomma bodies, seen here as purplish rounded
and laminated objects. They are essentially just a form of dystrophic
calcification in neoplasms.
Papillary cystadenocarcinoma of the ovary
Borderline serous tumors display cellular atypia,
but lack stromal invasion
In general,
malignant serous tumors spread to
regional lymph nodes, including para-aortic
lymph nodes, but distant lymphatic and
hematogenous metastases are infrequent.
The prognosis for the clearly invasive serous
cystadenocarcinoma is poor and depends
heavily on the stage of the disease at the time of
diagnosis. But it is much better for the
borderline tumors even with the presence of
peritoneal implants.
B. MucinousTumors
Differ from serous tumors essentially in
the epithelium, which is of
mucin-
secreting cells similar to those of the
endocervical or intestinal mucosa.
only 10% are malignant
(cystadenocarcinomas),
and 10% are of low malignant potential.
Other are benign.
Gross features
The incidence of bilateral ovarian
involvement is much lower than for their
serous counterparts.
Bilateral mucinous carcinomas and
(Krukemberg tumors).
Compared to their serous tumors, they show
mucinous cystic contents and tend to be
larger and multilocular but papillary
formations are less common.
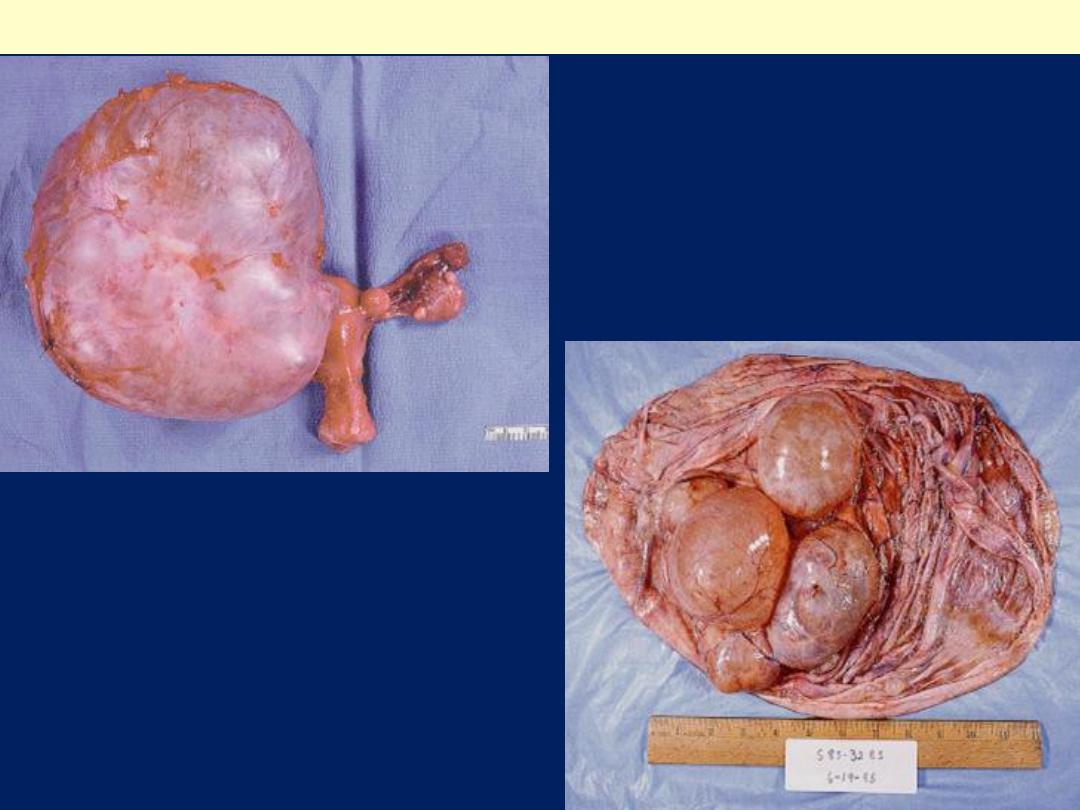
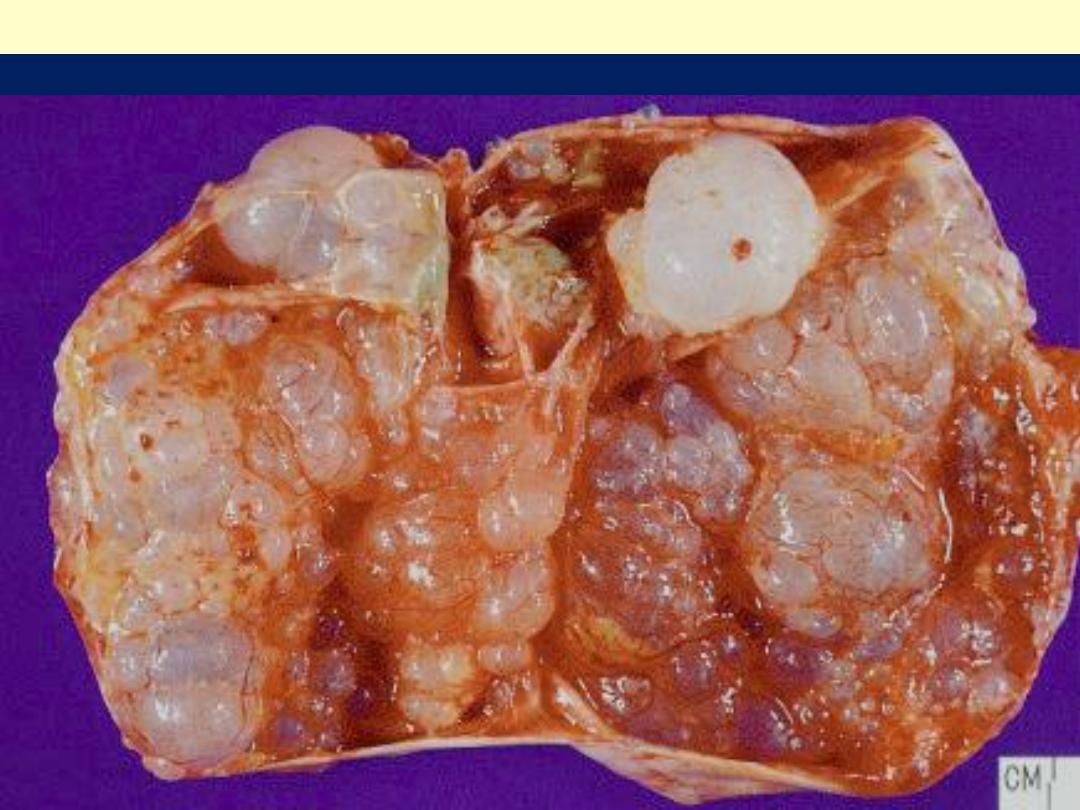
Mucinous cystadenoma
Outer and inner aspect
of mucinous
cystadenoma
.
A, displaying multicystic
appearance and delicate
septa. Note the presence of
glistening mucin within the
cysts.
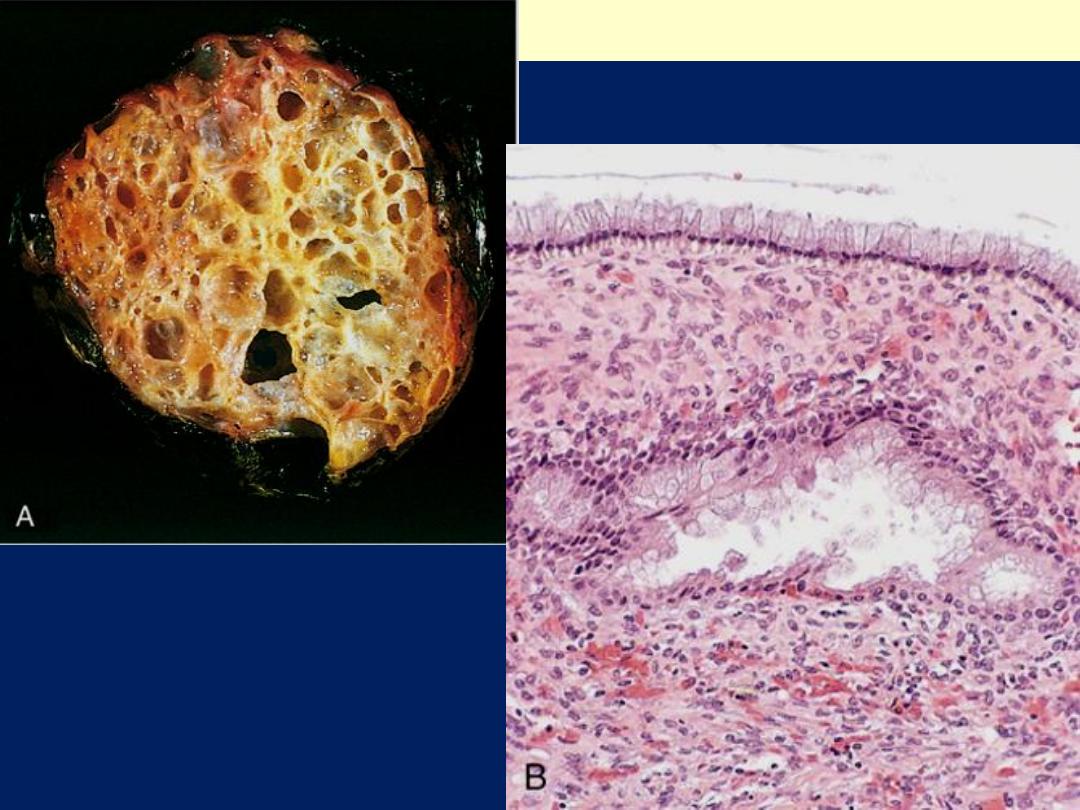
Mucinous cystadenoma
B, Columnar cell lining.
.
Mucinous ovarian tumor- borderline
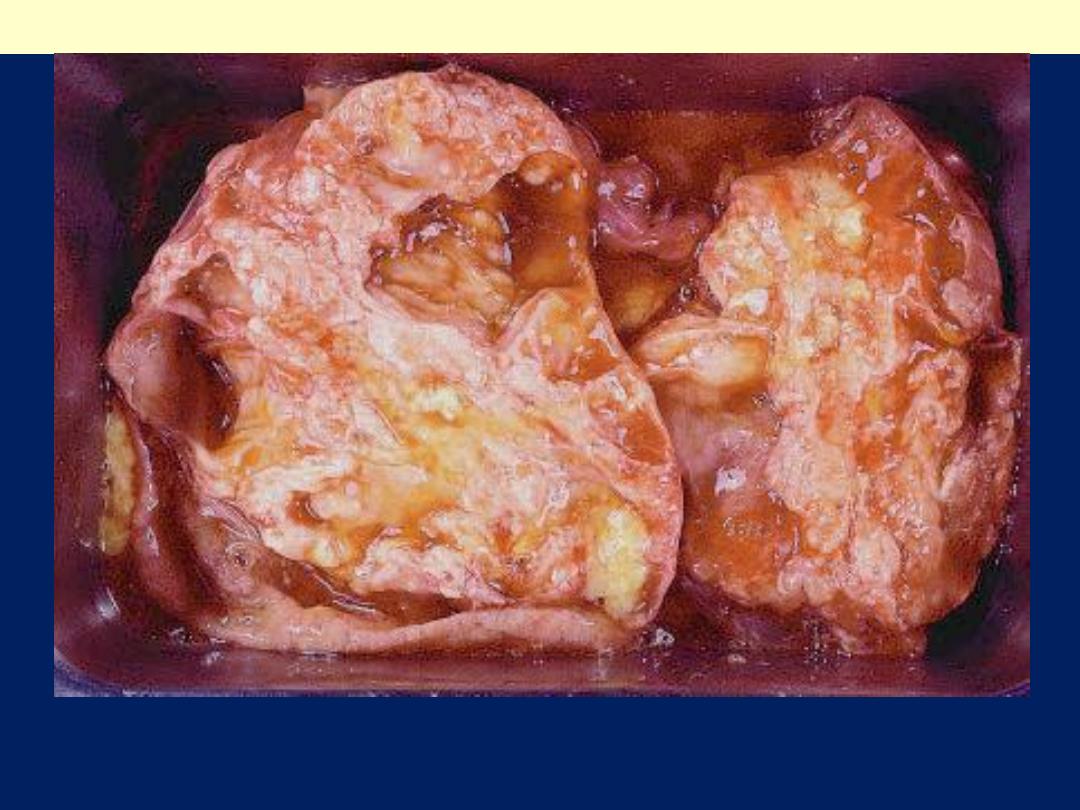
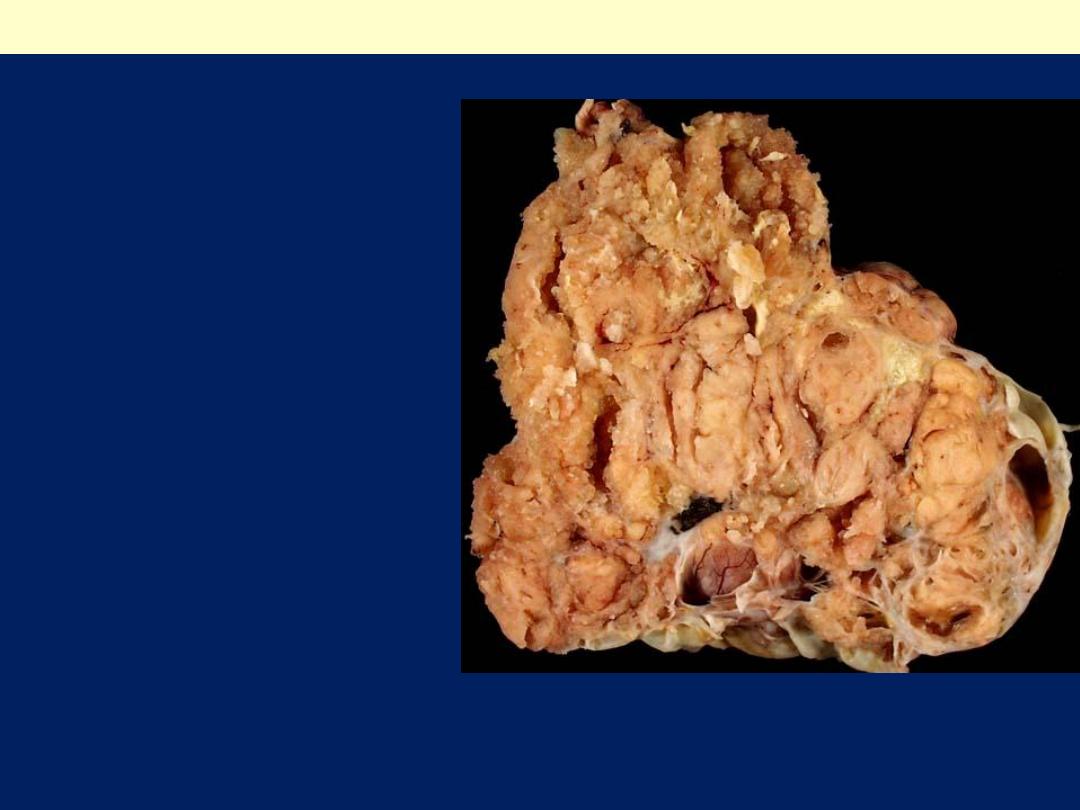
Mucinous cystadenocarcinoma
The neoplasm is predominantly solid, but some mucin-
containing cystic spaces can still be appreciated.
Microscopic features
Mucinous tumors are classified according to the
type of the mucin-producing epithelial cells into
endocervical, intestinal and müllerian-types.
The intestinal type is almost always present in
borderline mucinous tumors and mucinous
carcinomas.
Unlike in their serous counterparts,
psammoma
bodies are not found.
Serosal penetration and solid areas point to
malignancy.
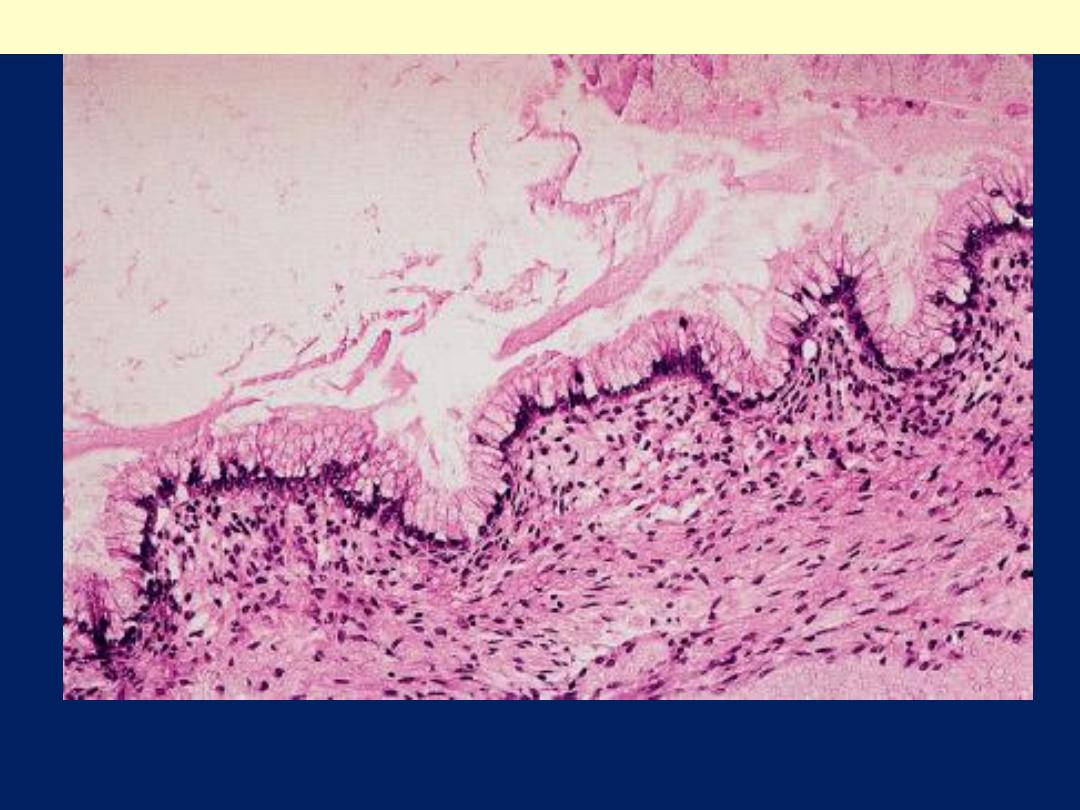
Lining of mucinous cystadenoma, intestinal subtype. Goblet
cells are evident. This subtype, is the most common
Mucinous cystadenoma
The lining of mucinous cystadenoma here resembles
endocervical epithelium.
Mucinous cystadenoma
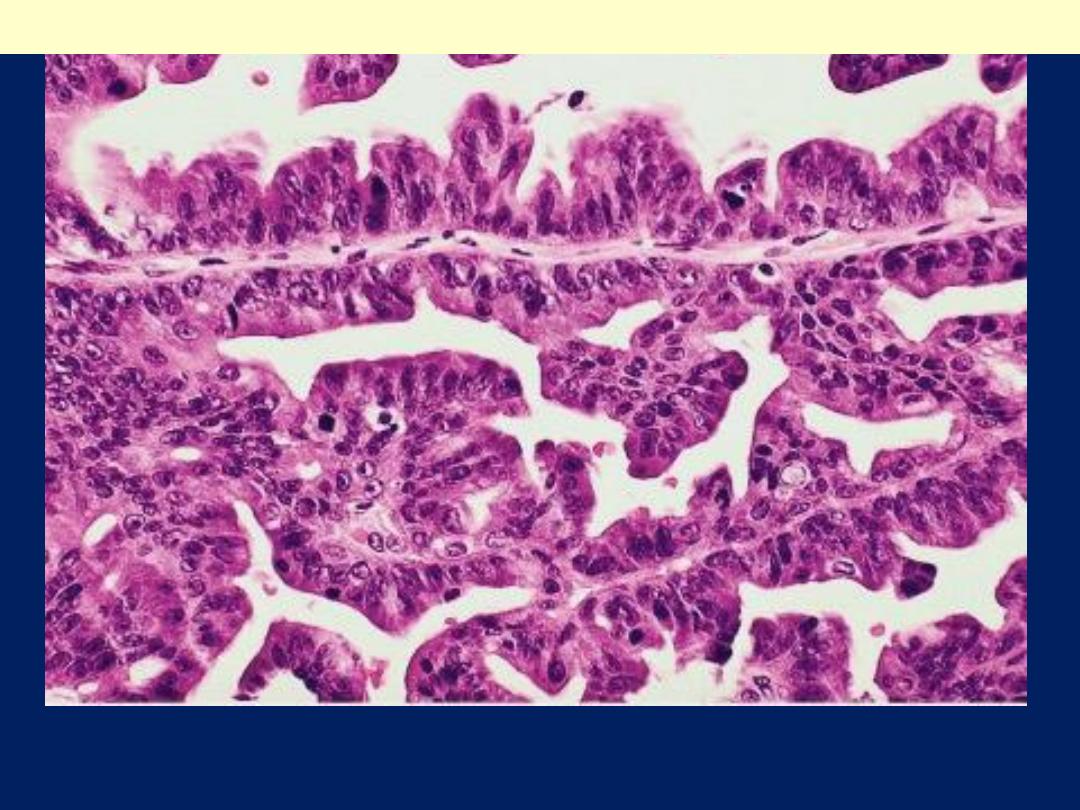
Complex architecture and obvious nuclear atypia in
mucinous cystadenocarcinoma
.
Mucinous cystadenocarcinoma
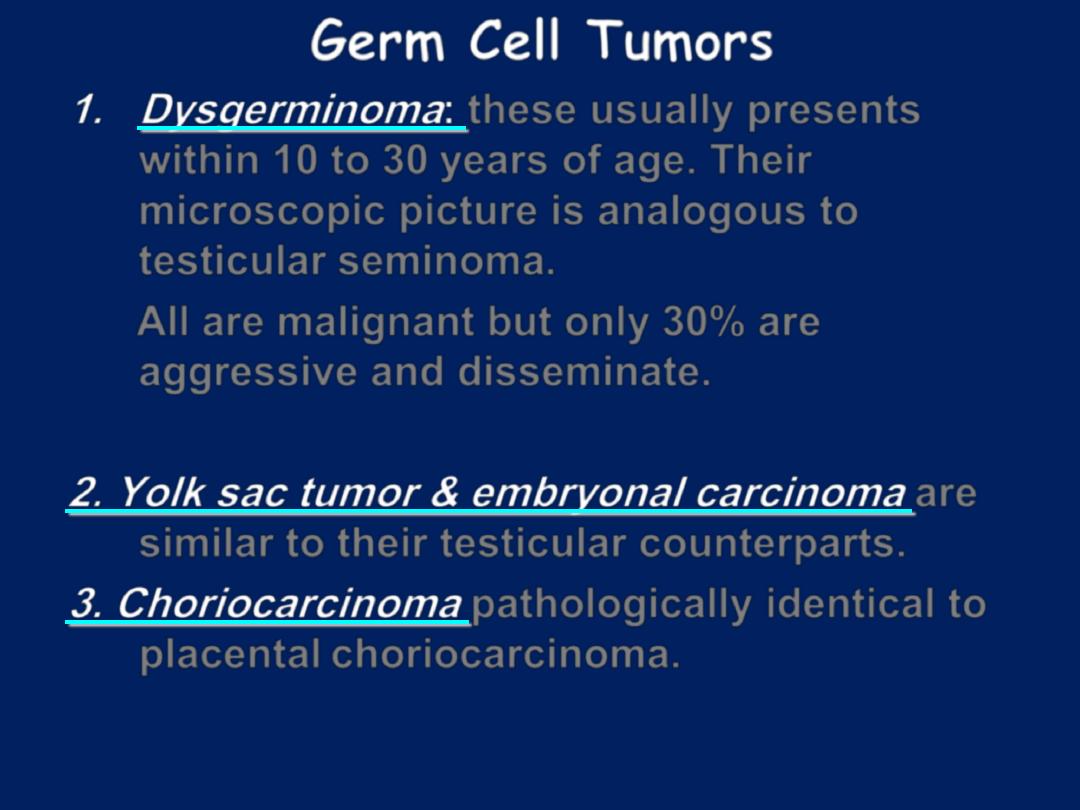
Germ Cell Tumors
1. Dysgerminoma
:
these usually presents
within 10 to 30 years of age. Their
microscopic picture is analogous to
testicular seminoma.
All are malignant but only 30% are
aggressive and disseminate.
2. Yolk sac tumor & embryonal carcinoma
are
similar to their testicular counterparts.
3. Choriocarcinoma
pathologically identical to
placental choriocarcinoma.
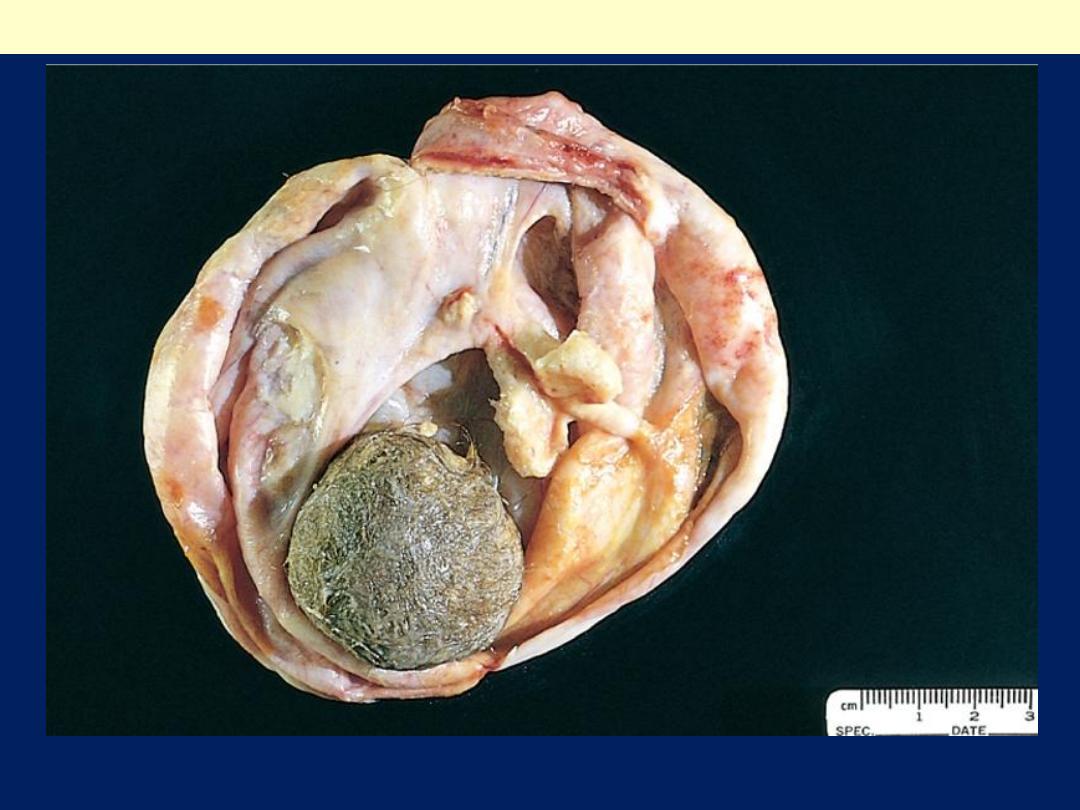
On opening a ball of hair (bottom) and a mixture of tissues are evident
Mature cystic teratoma (dermoid cyst) of the ovary
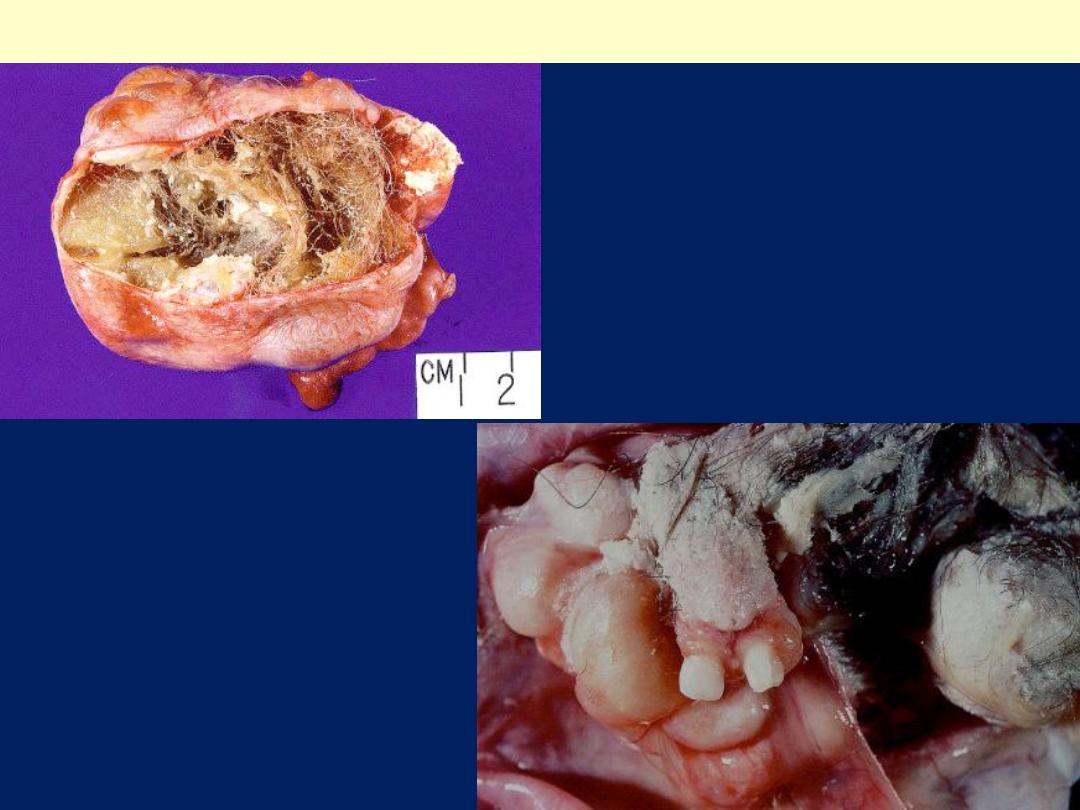
Mature cystic teratoma
Well-developed teeth in ovarian
mature cystic teratoma.
Tuft of hair admixed with sebum
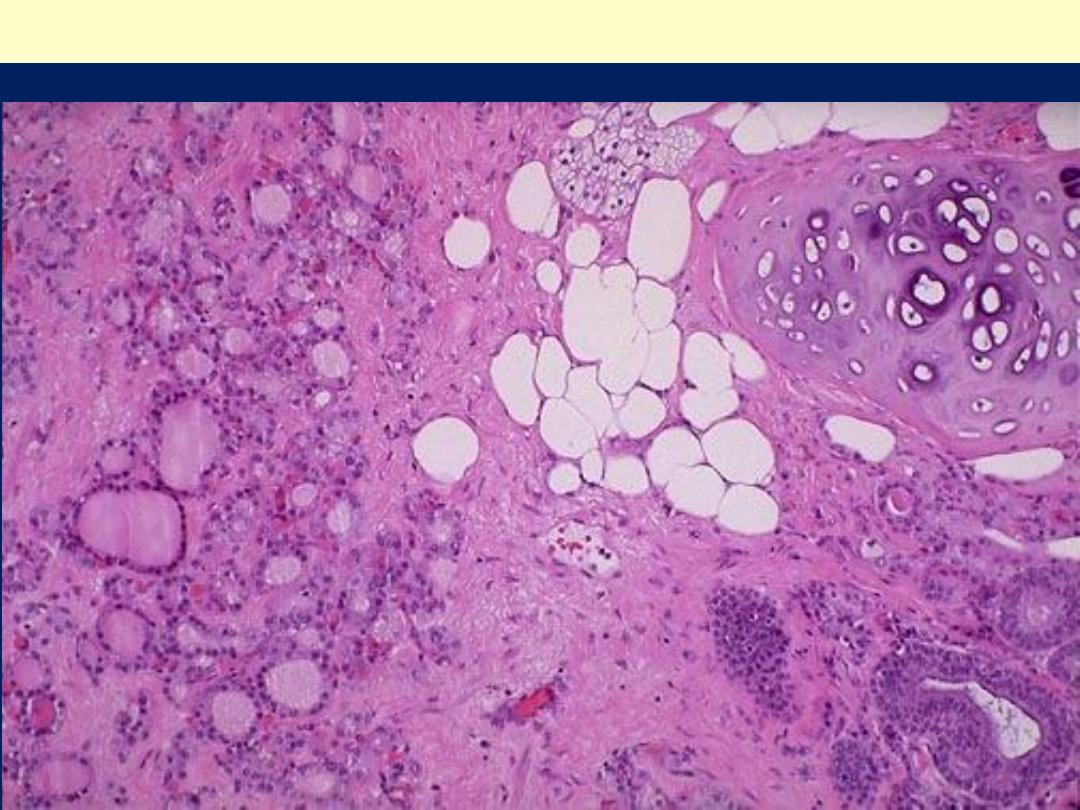
Mature cystic teratoma: A mixture of thyroid follicles, fat, cartilage and
glandular formations
Various tissues in mature
cystic teratoma: skin adnexa,
glial tissue (pale areas), and
choroid plexus.
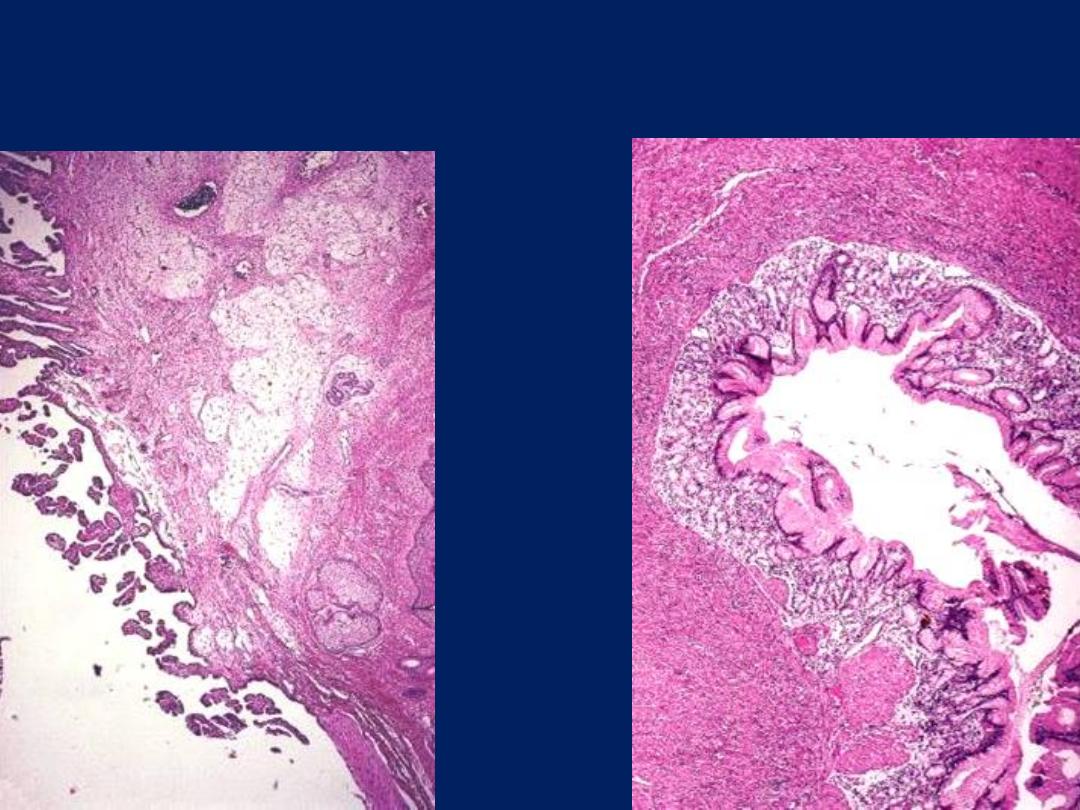
Various tissues in mature cystic
teratoma of ovary: gastric
mucosa of pyloric type.
Glial tissues
Choroid plexus
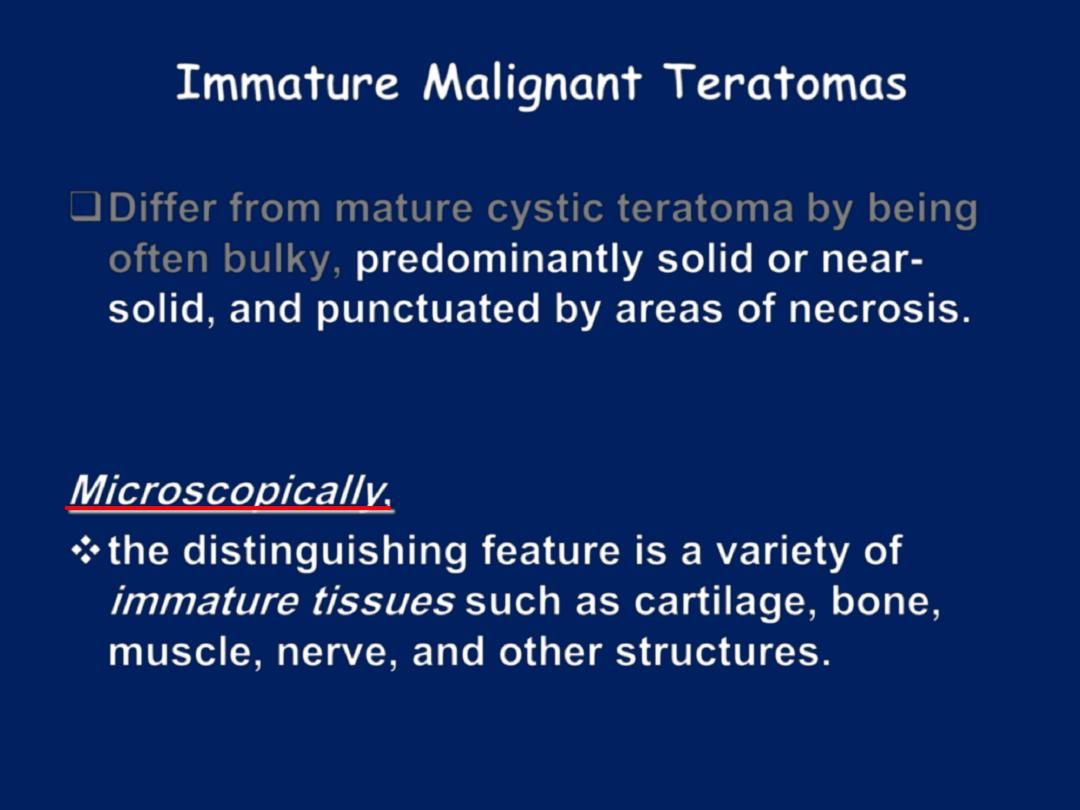
Immature Malignant Teratomas
Differ from mature cystic teratoma by being
often bulky,
predominantly solid or near-
solid, and punctuated by areas of necrosis.
Microscopically
,
the distinguishing feature is a variety of
immature tissues
such as cartilage, bone,
muscle, nerve, and other structures.
Immature (malignant) teratoma ovary
Immature teratoma may be solid throughout, solid with multiple minute cysts, or
predominantly cystic. It is a tumor of children and adolescents.

Ovarian immature teratoma with predominance of primitive
neuroepithelial elements
(
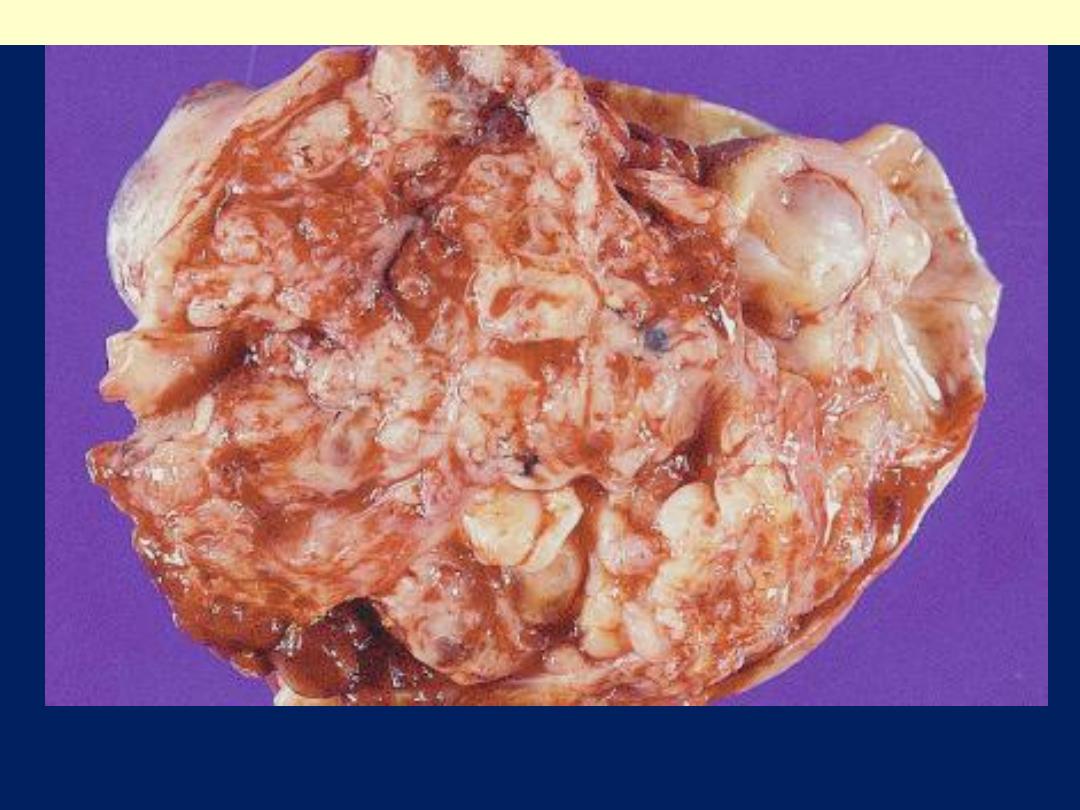
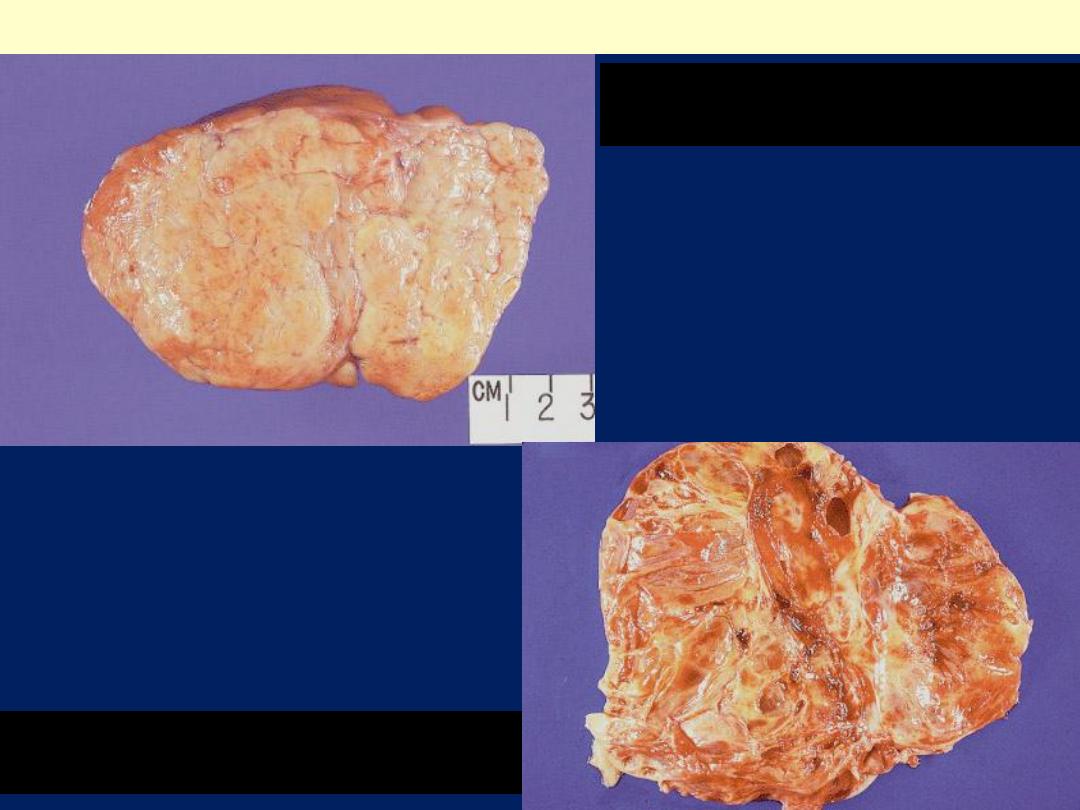
Granulosa cell tumor ovary (sex cord tumors
GCT with solid & lobulated,
yellow-gray cut surface.
GCT showing admixture of solid
and cystic areas.

Note the variegated cut surface
Granulosa cell tumor ovary
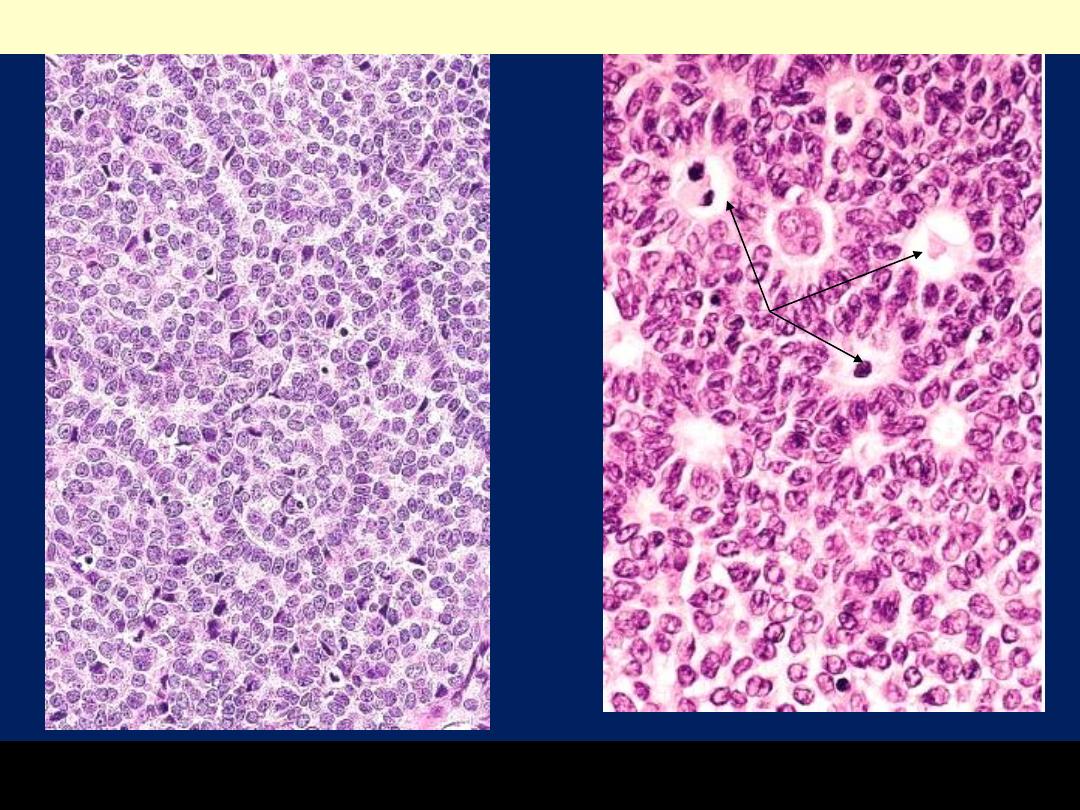
The cells are disposed in cords, trabeculae & microfllicles. Call-Exner bodies are seen on
the Rt (arrow). Note the coffee-bean nuclei
Granulosa cell tumor of the ovary
Hyperestrinism
occurs in 75% of cases; the
effects depend on age: in children there is
isosexual precocity; in adults & elderly there
is abnormal uterine bleeding due to
estrogen-induced endometrial hyperplasia.
However,
the tumor may be hormonally
inactive or paradoxically androgenic
The large amounts of estrogen (from thecal
elements) may encourage the development
of endometrial or breast carcinoma.
Granulosa cell element may be malignant.
2-Thecoma-fibroma group of tumors
occur at any age.
Ovarian fibroma is solid gray and consists of
spindle fibroblastic cells.
Ovarian thecoma is yellow in color because they
are composed of lipid-laden, plump thecal cells.
Few tumors in this group elaborate estrogens.
3.
Sertoli-Leydig cell tumors
• occur at any age.
• They are usually small and recapitulate the
development of testis with tubules, or cords
(Sertoli cells) and plump pink Leydig cells.
• Many of these tumors are functional
(masculinizing or defeminizing).
• They are rarely malignant.

Krukenberg tumor- ovary
Typical gross appearance of Krukenberg tumors of ovary. The
involvement is bilateral and the tumors are characterized by a
multinodular outer appearance.
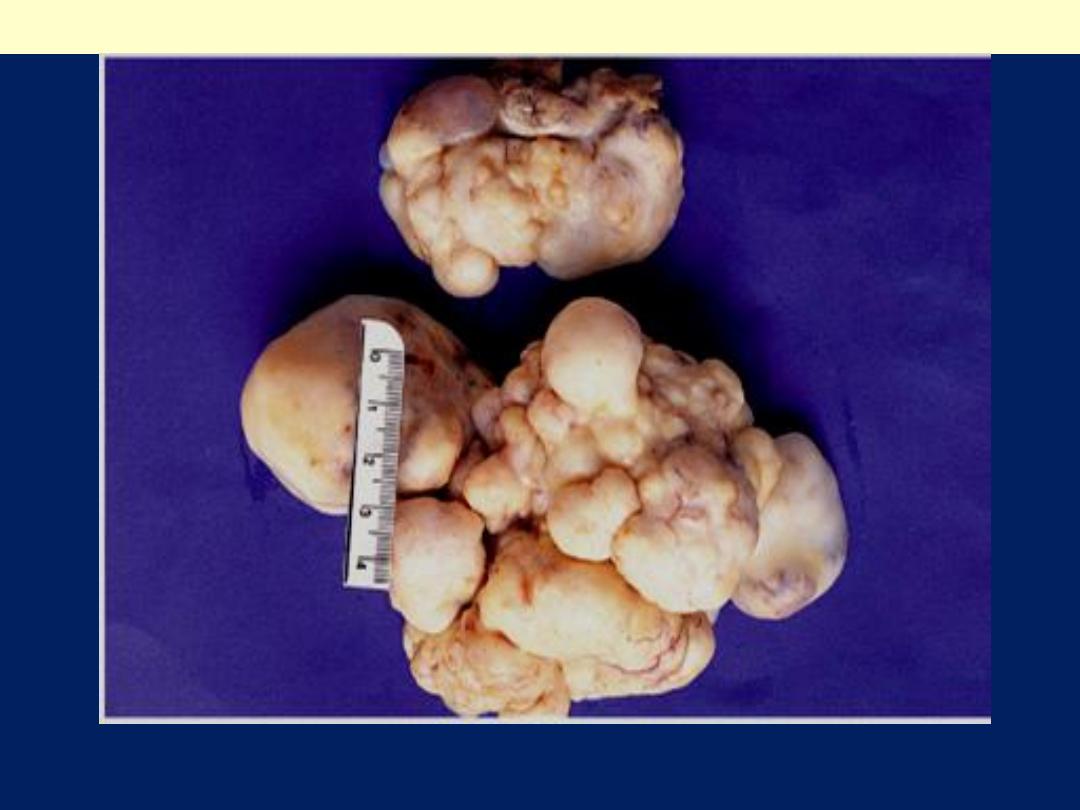
Krukenberg tumors ovary
The multinodular quality of the ovarian metastasis is typical of Krukenberg
tumor. A case of metastatic lobular ca breast
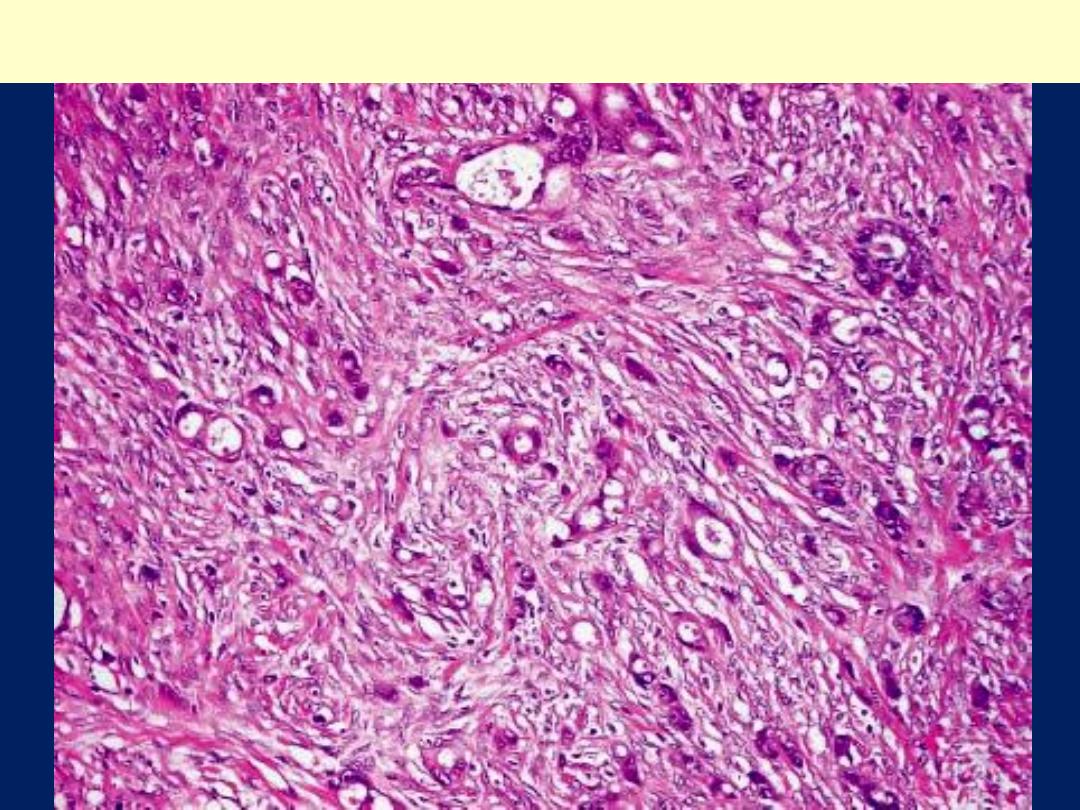
Krukenberg tumor of ovary: Numerous signet ring cells are present in a
highly fibrous stroma, either individually or in small nests
Clinical Correlations of ovarian cancers:
1-All ovarian neoplasms produce no symptoms or
signs until they are well advanced.
2-The clinical presentation of all ovarian tumors is
remarkably similar, except for the functioning
neoplasms that have hormonal effects , large size.
3-twisted on their pedicles (torsion
), producing severe
abdominal pain mimicking an
"acute abdomen.“
4-Fibromas and malignant serous tumors often
cause ascites,
5-Elevations of the
protein CA-125
have been
reported in
75% to 90% of women with epithelial
ovarian cancer.
Serum measurements of this
tumor marker are of greatest value in
monitoring
response to therapy in these patients.
