Baghdad College of Medicine / 4
th
grade
Student’s Name :
Dr. Saad Dakhil
Lec. 4 & 5
Scrotal Disorders
Mon. 11 / 4 / 2016
Mon. 18 / 4 / 2016
DONE BY : Ali Kareem
مكتب اشور لالستنساخ
2015 – 2016
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
2
©Ali Kareem 2015-2016
SCROTAL DISORDERS
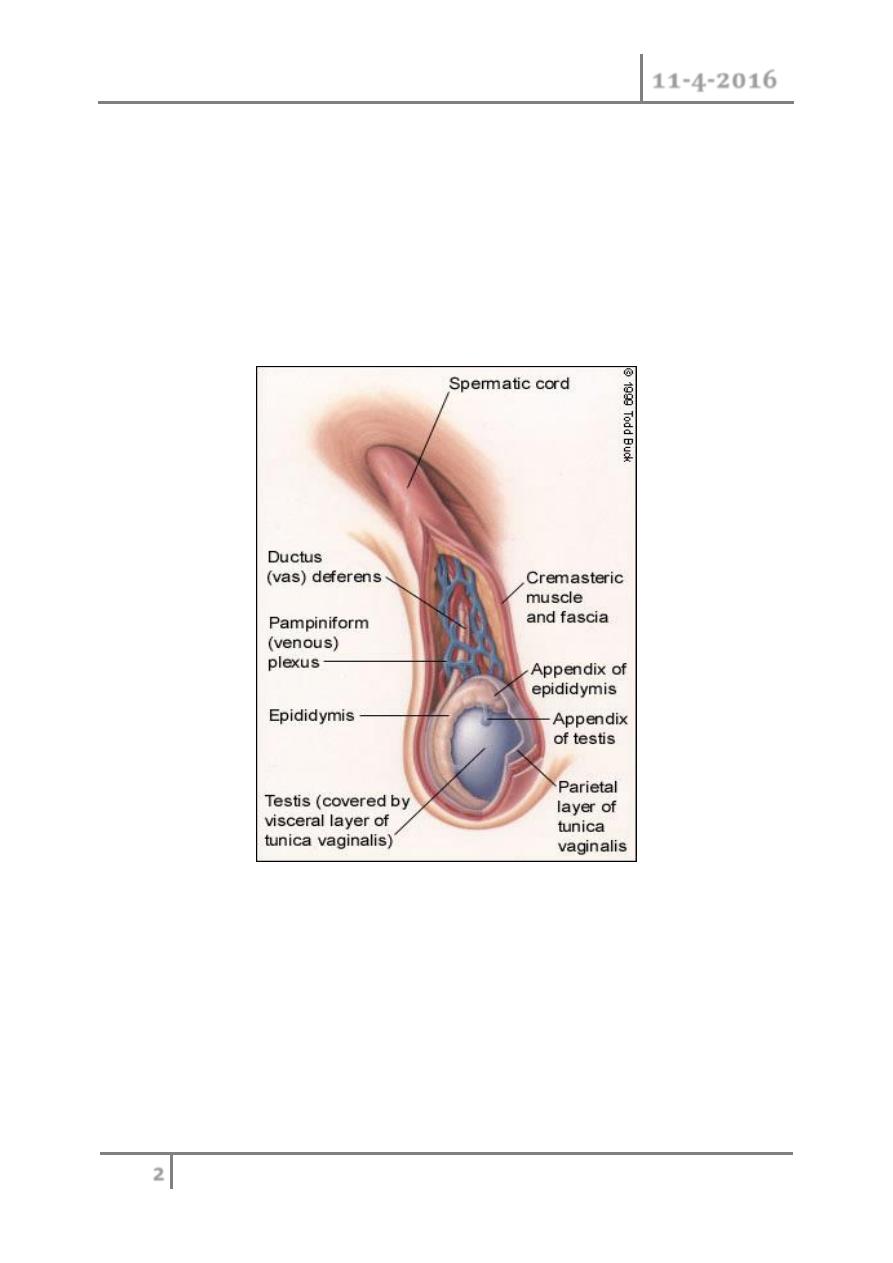
Anatomy
o Scrotum;can be considered as an outpouching of the lower part of the
anterior abdominal wall.it contains the Testis,Epididymides,lower end of
spermatic cord
Spermatic cord
Structure of spermatic cord ;
1-vas deferens
2-testicular artery
3- testicular veins (pampiniform plexus)
4-testicular lymph vessels
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
3
©Ali Kareem 2015-2016
5-autonomic nerves
6-processus vaginalis
7-cremasteric artery
8-artery of the vas deferens
9-genital branch of the genitofemoral nerve
Hydrocele
o Collection of abnormal quantity of serous fluid in the tunica vaginalis.
o If it contains pus or blood it is called pyocele or haematocele
respectively.
o Hydrocele is more common than the two other varieties.
Scrotal
Swellings
Cystic
Solid
Neither
Tumor
(benign/
Malignant)
varicocele
Hernia
Hydrocel
e
Epididymal
cyst/
spermatocele
Hematocele
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
4
©Ali Kareem 2015-2016
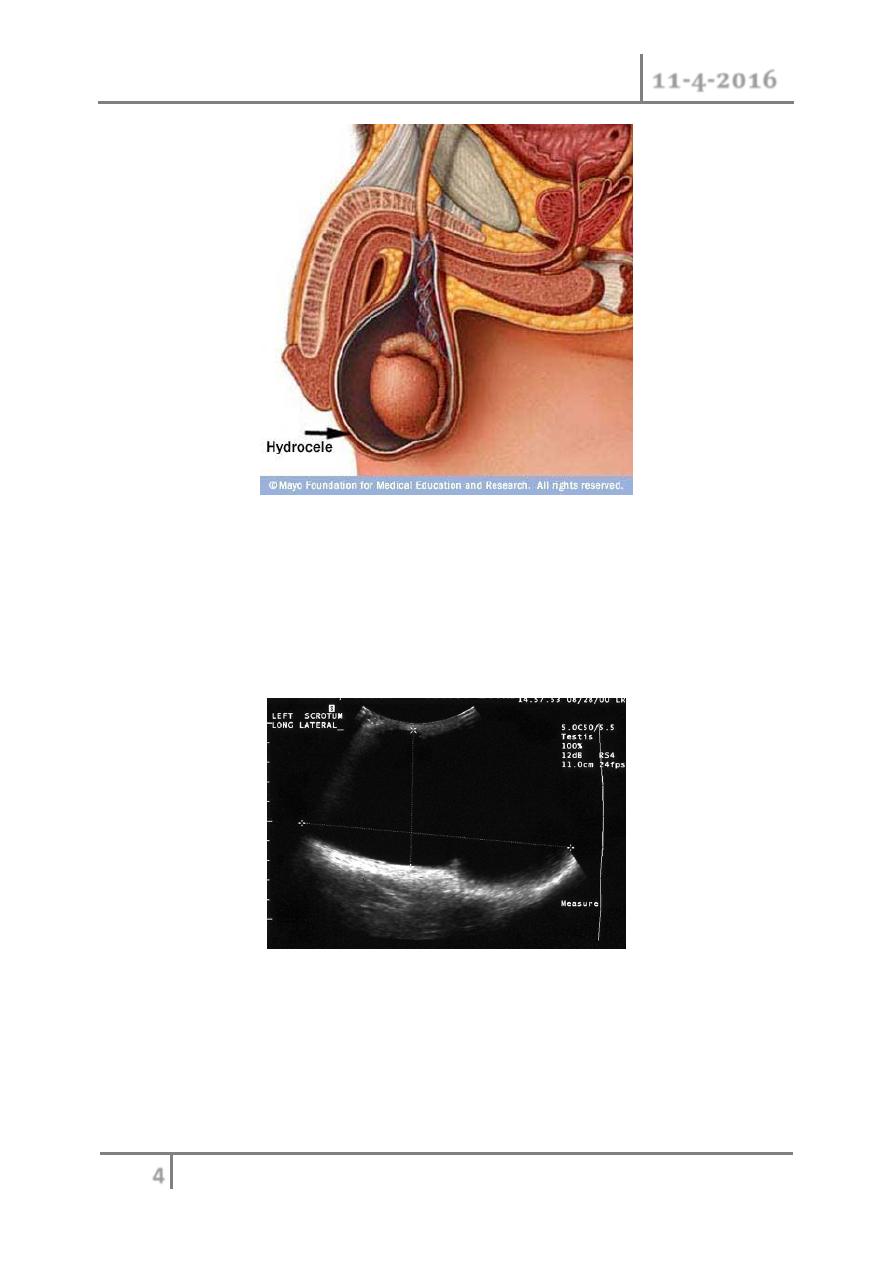
Hernia / Hydrocele
o Hydrocele: incomplete obliteration of the processus vaginalis
o Hernia: large opening of the processus vaginalis which may allow
abdominal contents to enter scrotal sac.
Scrotal Ultrasound
Large left hydrocele
Causes :
1- Primary;cause unknown associate with patency of proccessus vaginalis.
It classified as follows;
1- Communicating;it connect with the peritoneal cavity.
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
5
©Ali Kareem 2015-2016
2- Noncommunicating;it dose not connect with peritoneal cavity.
2- Secondary; where the fluid accumulate secondary to pathology inside the
testis like epididymo-orchitis,testicular tumor and trauma.
Clinical presentation;
Symptoms;
1- Painless swelling
2- Embarrassment
3- Frequent and painful micturation may occur if hydrocele is secondary to
epididymo-orchitis
o Hydrocele not affect fertility
Examination;
o Position; the swelling usually unilateral but can be bilateral .if
communicating can not feel the cord above the lump.
o Colour and temperature; normal
o Tenderness; primary are not tender but secondary may be tender
o Composition; fluctuant and have fluid thrill if large enough
o Reducibility; can not reduced
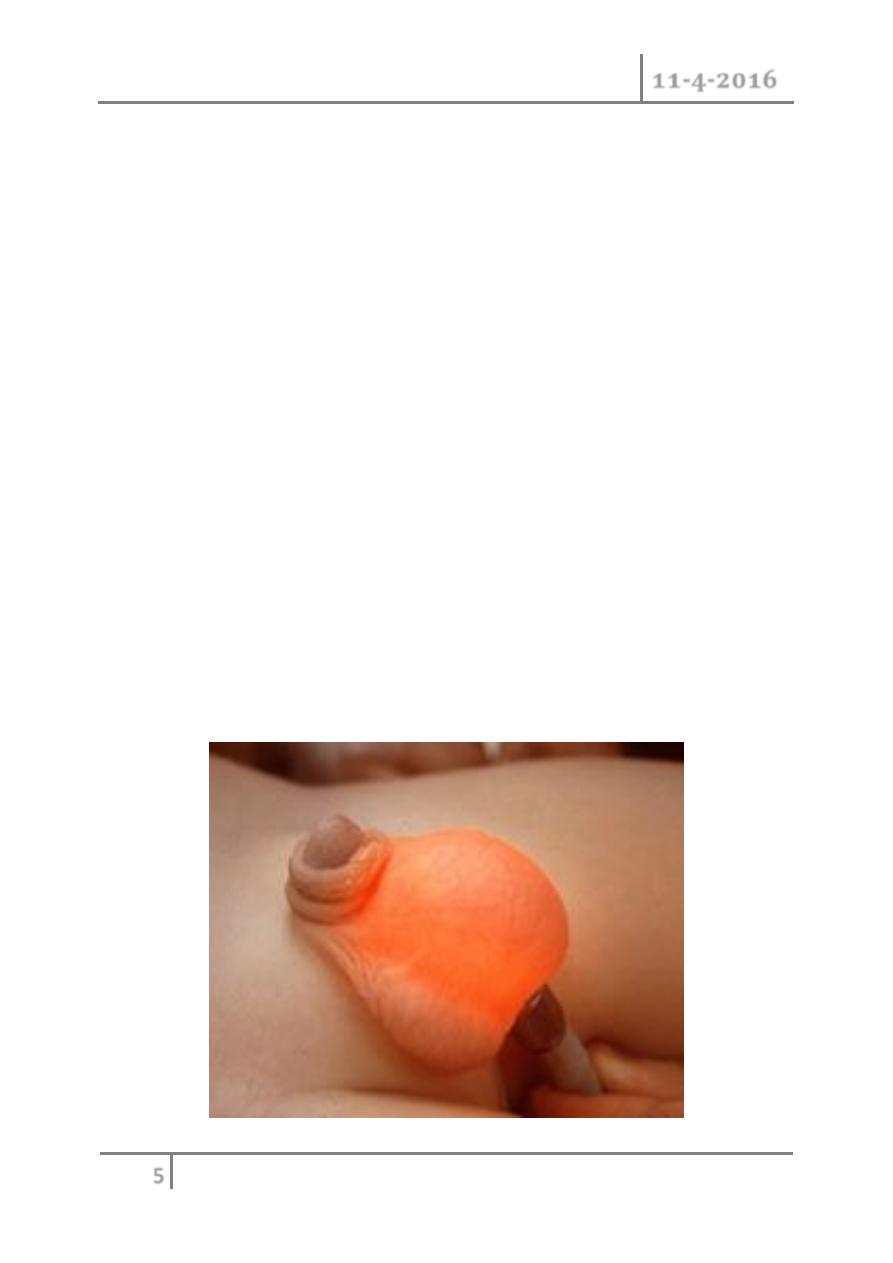
o Testis impalpable and transillumenate
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
6
©Ali Kareem 2015-2016
Mangement;
Primary :
In children:
o Most neonatal hydrocel resolve in first 2 year of life if persists repair as
herniotomy.(communicating).
o The scrotal approach (Lord or Jaboulay technique) is used in the
treatment of a secondary non-communicating hydrocele.
In adult :
o Surgical excision.
Secondary :
Treatment the underlying condition.
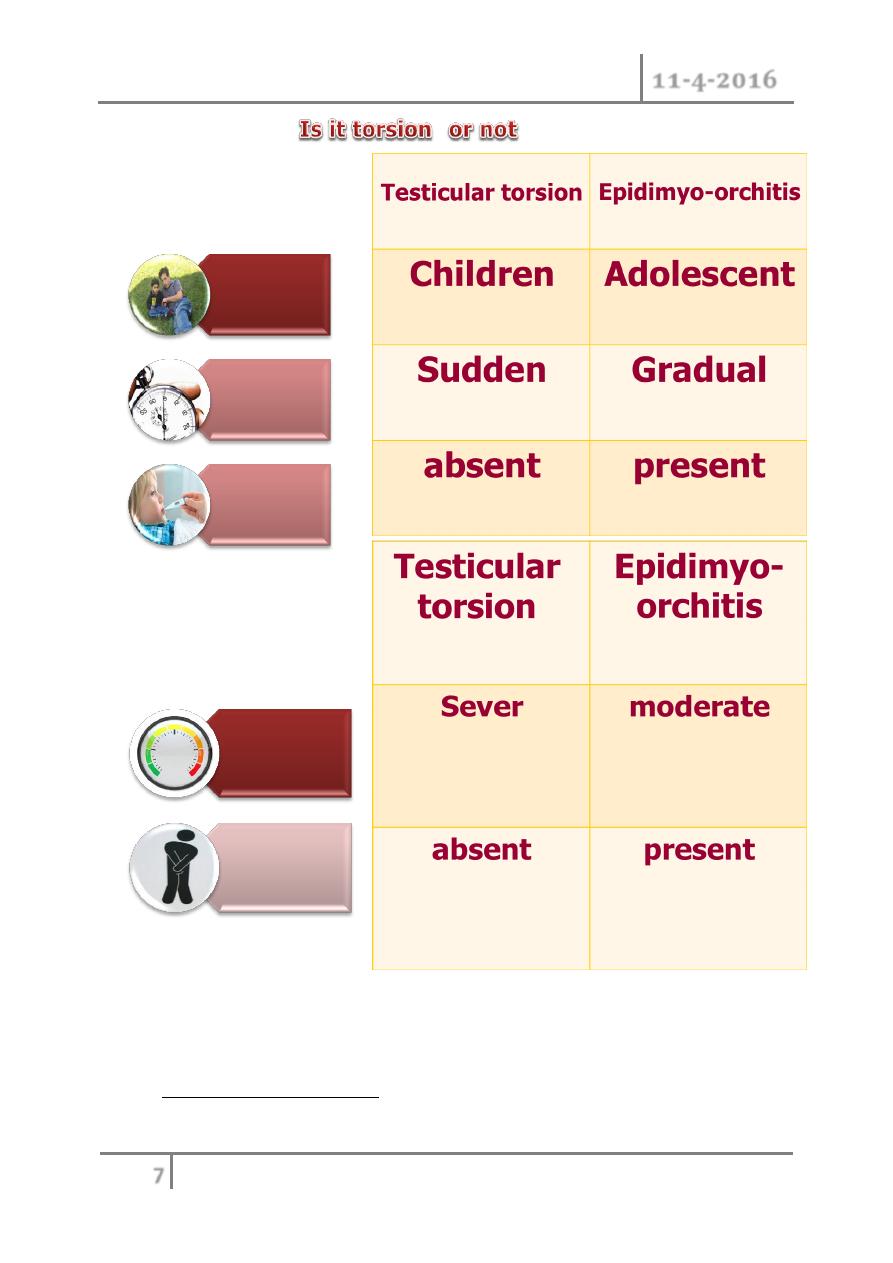
ACUTE SCROTUM IN CHILDREN
o A child or adolescent with acute scrotal pain, tenderness, or swelling
should be looked on as an emergency situation requiring prompt
evaluation, differential diagnosis, and potentially immediate surgical
exploration.
Causes
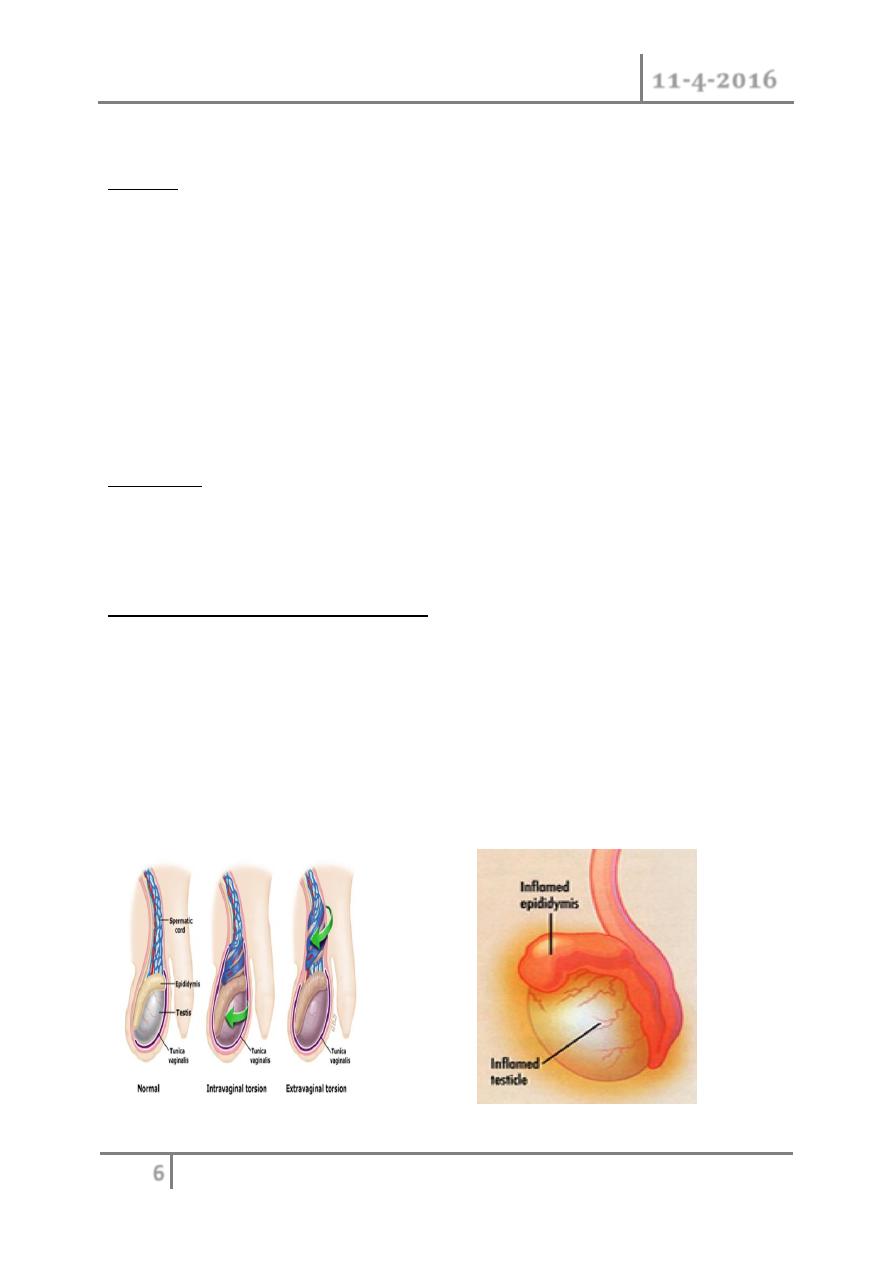
Epididmyo-orchitis
Testicular Torsion
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
7
©Ali Kareem 2015-2016
Testicular Torsion
o The most urgent problem.
o High risk of loss due to infarction (90%)
Age
Onset
Fever
Severity
Irritative
symptoms
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
8
©Ali Kareem 2015-2016
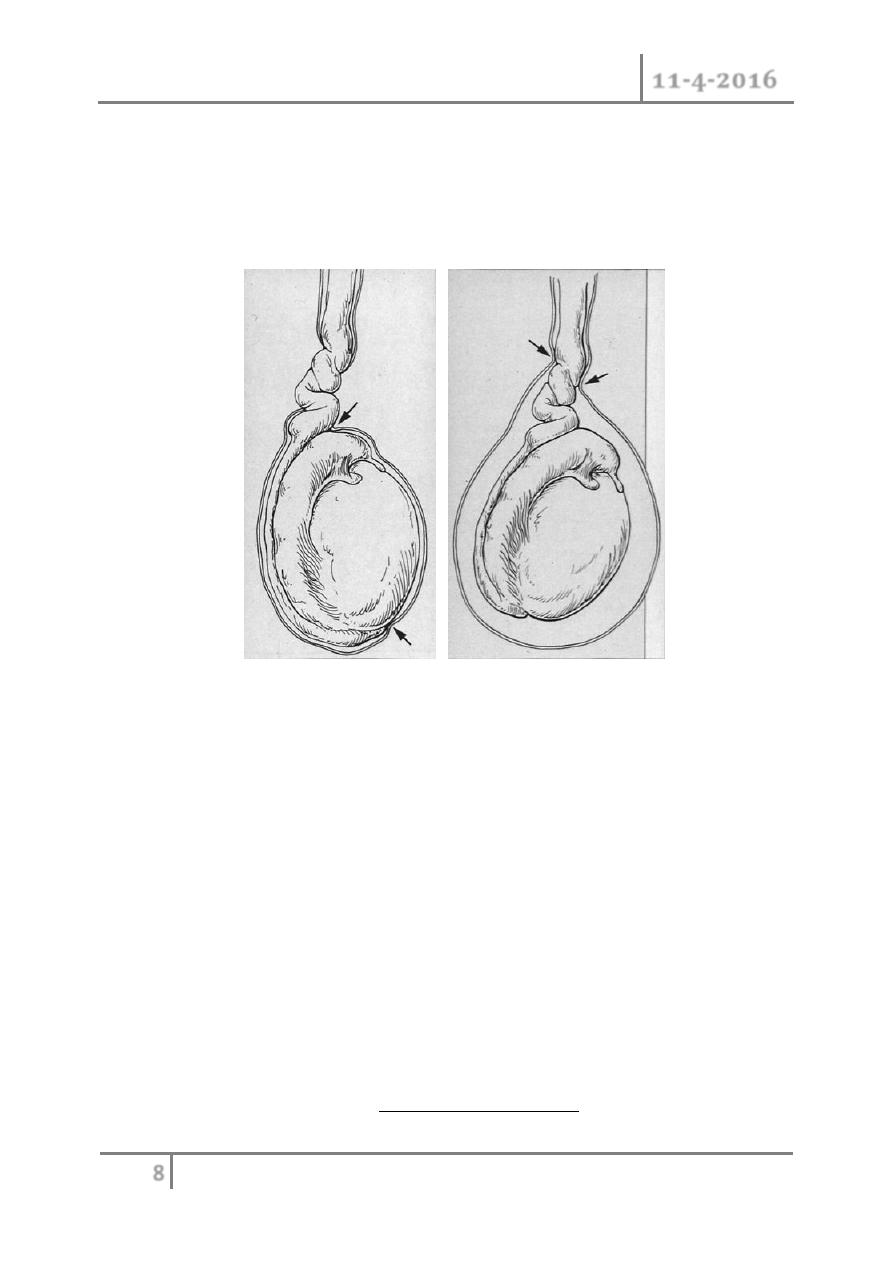
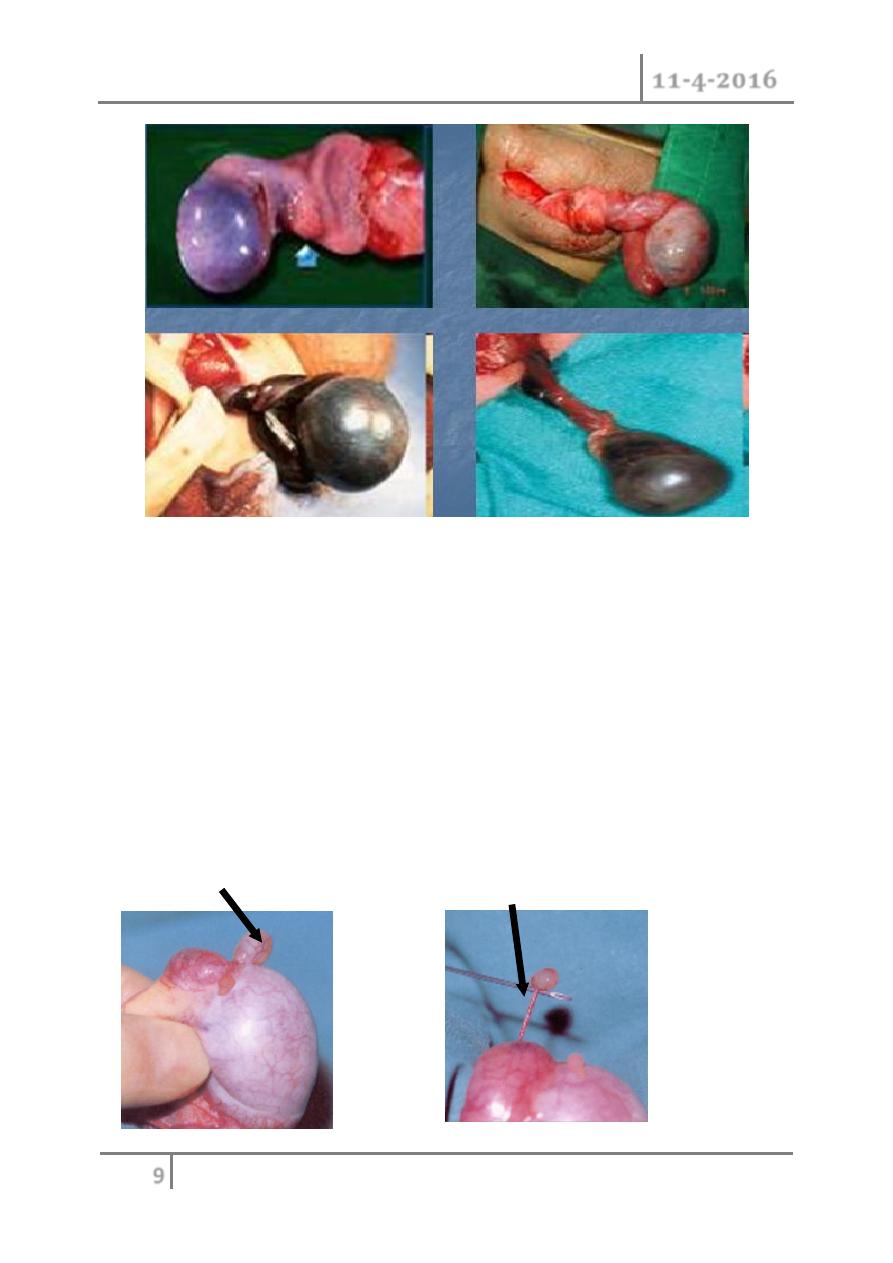
o May have torsion of cord or appendages
o Neonatal and adolescence
o more common in undescended testes due to absence of fixation
o Extravaginal: exclusive to perinatal
o Intravaginal: 90% of adolescent age group
Extravaginal Intravaginal
Torsion Torsion
History
o Sudden onset of pain
o Past history of similar pain in 50%
Physical
o Cremasteric reflex may be absent
o
Prehn’s sign: elevation of testes does not relieve pain
o lateral testicular lie.
Diagnosis
o if certain : emergent surgery
o if uncertain:
Nuclear scan: not done often depending on facility
Ultrasonography: documents blood flow
PROVIDES ANATOMY
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
9
©Ali Kareem 2015-2016
Refer Emergently!
o < 6 hours, 90% salvage
o > 24 hours, 100% loss and atrophy
Attempt manual detorsion- outward
o
“ open the book “
Some may be twisted 360, 720 degrees
Testicular Appendages
Appendix testis Appendix epididymis
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
10
©Ali Kareem 2015-2016
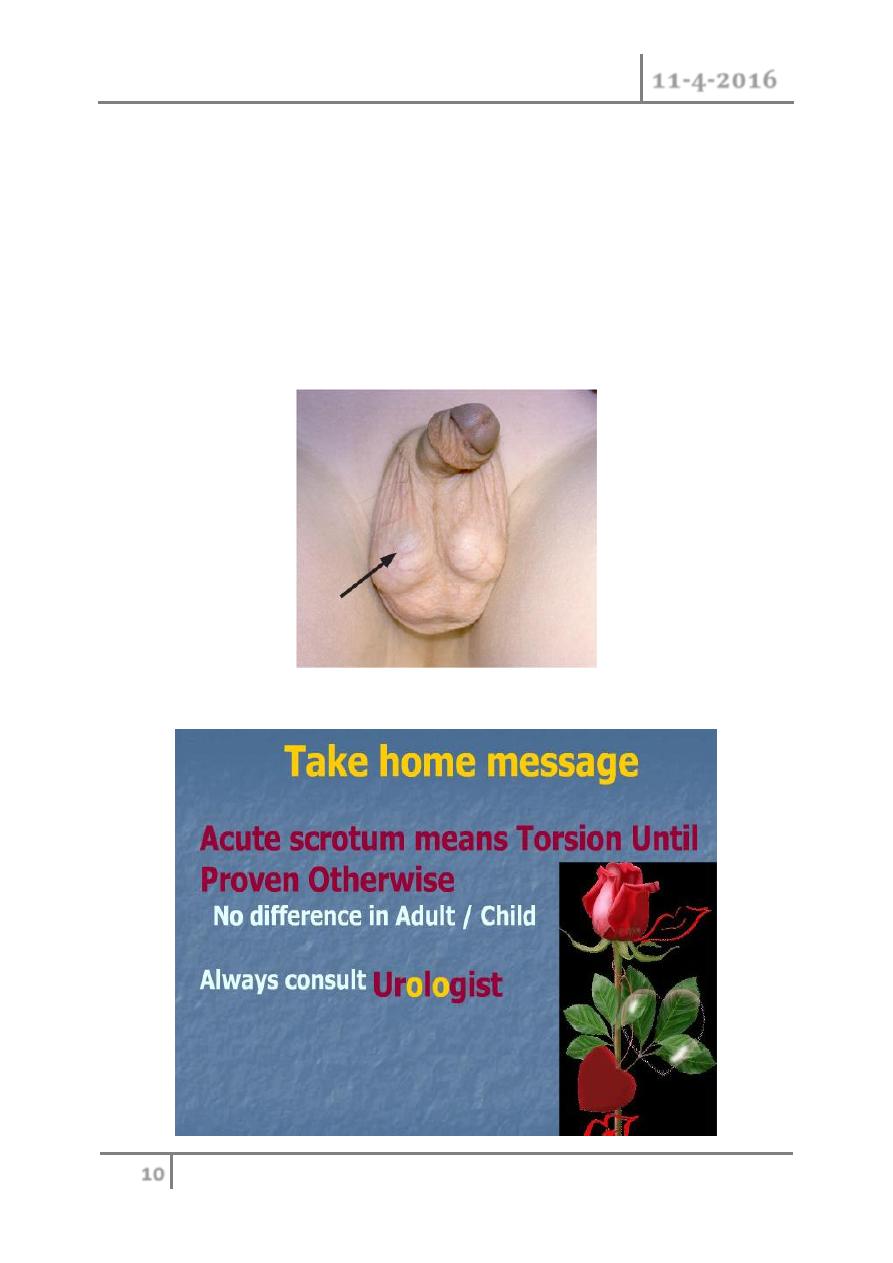
o Torsion of appendages rarely seen after puberty
o Presents with pain
o Physical
may develop scrotal swelling & erythema
“ blue dot sign” seen early
Ultrasound required to rule out testis torsion
o Treat symptomatically
Be sure of early exam before swelling makes any further exam
suspect!
Blue dot of gangrenous appendix testis
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
11
©Ali Kareem 2015-2016
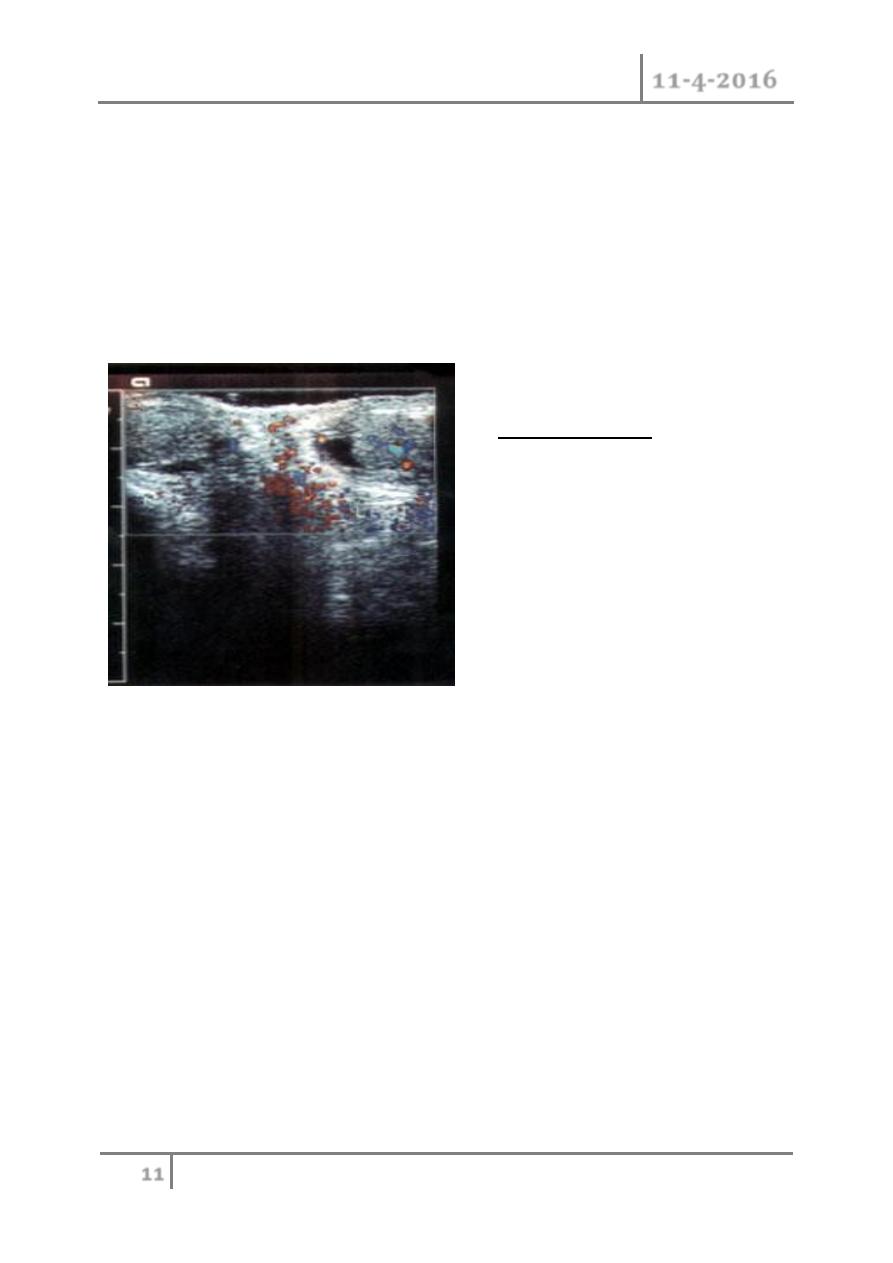
Epididymitis
o Most common acute scrotum post-pubertal
o Gradual onset of pain
o Fever in 40% of patients
o Dysuria in 50% of patients
o Urinalysis may show pyuria in 50%
Doppler Epididymitis
o Confirm that torsion of testis does not exist
Treatment
o scrotal elevation
o Antibiotics considered: keflex, septra
Refer for persistence of pain/swelling.
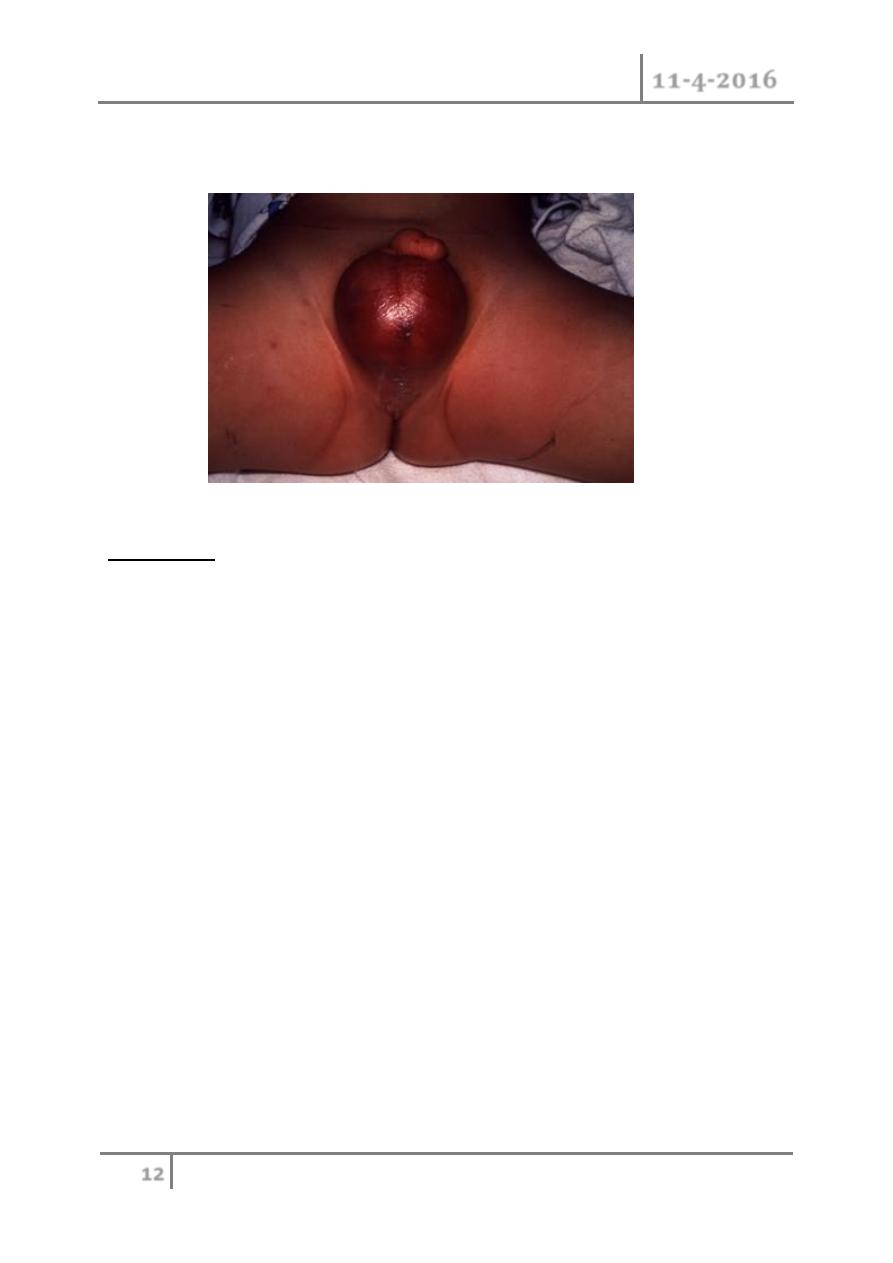
Fournier’s Gangrene
o Necrotizing fasciitis of the perineum
o May ascend of fascial planes
Colles > Dartos > Scarpas
o 20% to 50% Mortality Rate
o Polymicrobial infection
Treat with Gent, Pen G and Flagyl
Left Epididymitis
Increased blood flow
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
12
©Ali Kareem 2015-2016
Debridement surgically
o 20% to 30% related to GU source
CRYPTORCHIDISM
Background
o Almost 1% of all full-term male infants are affected at the age of one
year.
o Categorisation into palpable and non-palpable testis seems to be most the
appropriate method.
o Iliac fossa 3
rd
-5
th
month
o Deep inguinal ring 7
th
month
o Superficial ring 8
th
month
o Scrotum 9
th
month
Complications (THIN)
Higher incidence of:
o Cancer. 25-30 times increased risk.
o Not affected by orchiopexy.
o Infertility.
50% abnormal semen in unilat. UDT
70% in bilateral.
o Testicular torsion.
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
13
©Ali Kareem 2015-2016
o Trauma.
o Hernia
Assessment
o A physical examination is the only method of differentiating between
palpable or non-palpable testes.
o Radiological imaging: 44%
o There is no reliable examination to confirm or rule out an intra-
abdominal, inguinal and absent/vanishing testis (nonpalpable testis),
except for diagnostic laparoscopy.
o In cases of bilateral non-palpable testes and any suggestion of sexual
differentiation problems, urgent endocrinological and genetic evaluation
is mandatory.
Treatment
o To prevent histological deterioration, treatment should be undertaken
and completed before the age of 12-18 months.
Medical therapy
o Medical therapy using human chorionic gonadotrophin (hCG) or
gonadotrophin-releasing hormone (GnRH) is based on the hormonal
dependence of testicular descent, with success rates of a maximum of
20%.
o Palpable testis:
Surgery for the palpable testis includes orchidofuniculolysis and
orchidopexy, with success rates of up to 92%.
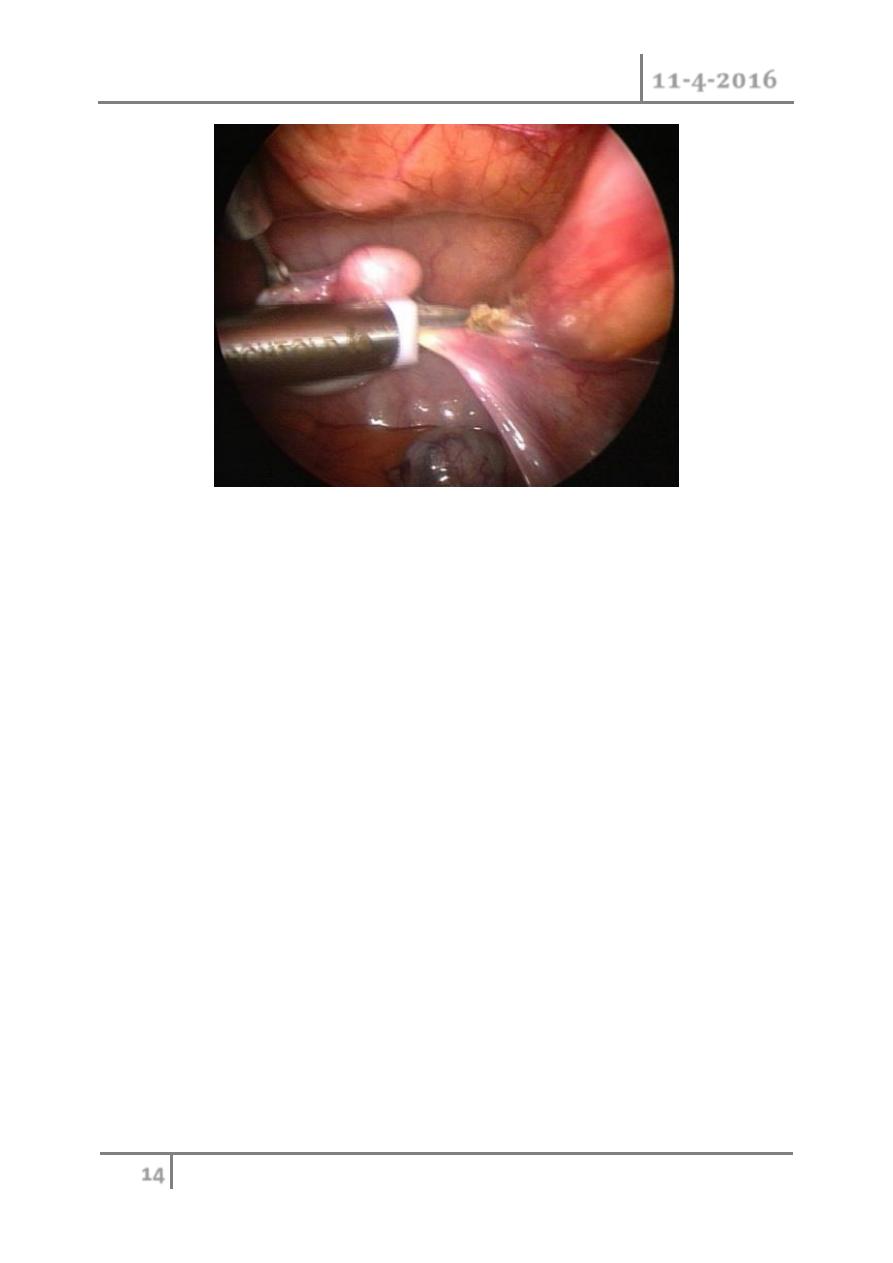
o Non-palpable testis:
Inguinal surgical exploration with the possibility of performing
laparoscopy should be attempted. Laparoscopy is the most
appropriate way of examining the abdomen for a testis.
o Microvascular autotransplantation is also an option.
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
14
©Ali Kareem 2015-2016
Ectopic Testes
o perineal
o prepenile.
o femoral.
o inguinal pouch.
Retractile Testes
o functions normally.
o normal size & consistency
o scrotum well developed.
o ? Hyperactive cremasteric reflex.
o most are normal by 12 yrs.
Atrophied Testes ?
o Trauma.
o Torsion.
o Infection.
o Previous inguinal surgery.
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
15
©Ali Kareem 2015-2016
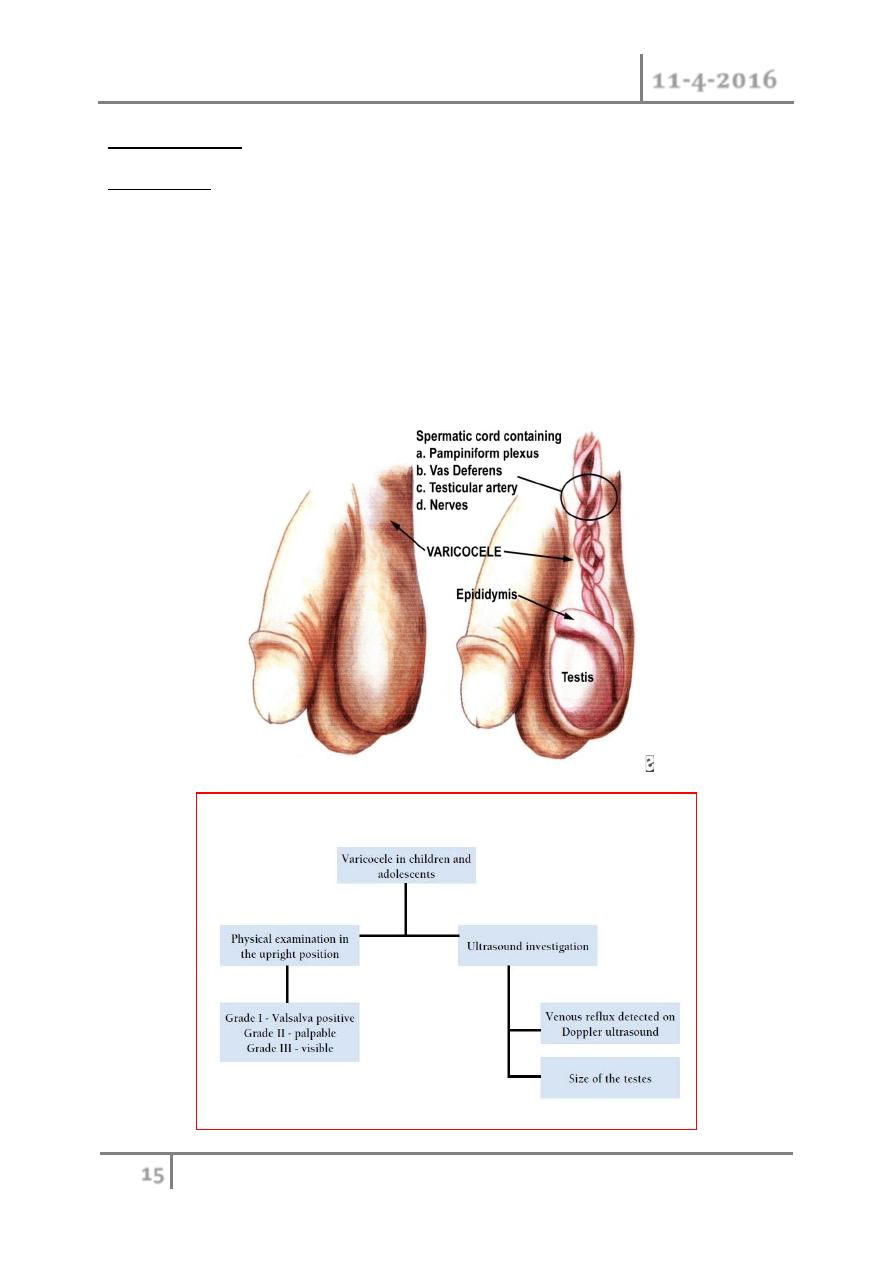
VARICOCELE
Background
o Ectatic and tortuous veins of the pampiniform plexus of the spermatic
cord are found in approximately 15% of male adolescents, with a marked
left-sided predominance .
o This is unusual in boys under 10 years of age, but becomes more frequent
at the beginning of puberty.
o Fertility problems will arise in about 20% of adolescents with varicocele.
o The adverse influence of varicocele increases with time.

Scrotal Disorders Dr. Saad Dakhil
11-4-2016
16
©Ali Kareem 2015-2016
Treatment
o Surgery
Surgical intervention is based on ligation or occlusion of the
internal spermatic veins. Microsurgical lymphatic-sparing repair
(microscopic or laparoscopic) are associated with the lowest
recurrence and complication rate.
o Follow-up
During adolescence, testicular size should be checked annually.
After adolescence, repeated sperm analysis is to be recommended.
The potential complications of varicocelectomy
o Hydrocele formation, varicocele recurrence and testicular infarction
(atrophy).
o Hydrocele formation is related to failure to preserve the lymphatic
vessels associated with the spermatic cord.
Testicular tumors
o Commonest malignancy in men < 35 years.
o Rare in african men and before puberty.
o Peaks in the early twenties.
o One in 10 testicular tumors occurs in association with maldescent of the
testis.
o Prognosis is good particularly if there was no lymph node involvement.
Classification
According to the cells of origin, they’re classified into:
1- Primary cell tumors (90-95%), which include:
o Germ cell tumors: Seminoma, teratoma,Embryonal CA, Yolk Sac
Tumor.
o Non-germ cells tumors: like sertoli cells tumors, Lyedig cell tumor.
2- Secondary tumors: lymphoma, leukemic infiltration of the testes.

Scrotal Disorders Dr. Saad Dakhil
11-4-2016
17
©Ali Kareem 2015-2016
Germ cell tumors
1. Seminomas - 40%
(a) Classic Typical Seminoma
(b) Anaplastic Seminoma
(c) Spermatocytic Seminoma
2. Embryonal Carcinoma - 20 - 25%
3. Teratoma - 25 - 35%
(a) Mature
(b) Immature
4. Choriocarcinoma - 1%
5. Yolk Sac Tumour
Clinical features
o Painless Swelling of One testis
o Dull Ache or Heaviness in Lower Abdomen
o 10% - Acute Scrotal Pain
o 10% - Present with Metatstasis
o
- Neck Mass / Cough / Anorexia / Vomiting / Back Ache/ Lower
limb swelling
o 5% - Gynecomastia
o Rarely - Infertility
Physical Examination
o Examine contralateral normal testis.
o Firm to hard fixed area within tunica albugenia is suspicious.
o Seminoma expand within the testis as a painless, rubbery enlargement.
o Embryonal carcinoma or teratocarcinoma may produce an irregular,
rather than discrete mass.

Scrotal Disorders Dr. Saad Dakhil
11-4-2016
18
©Ali Kareem 2015-2016
Differential Diagnosis
o Testicular torsion
o Epididymitis, or epididymo-orchitis
o Hydrocele,
o Hernia,
o Hematoma,
o Spermatocele,
o Syphilitic gumma .
DICTUM FOR ANY SOLID SCROTAL SWELLINGS
o All patients with a solid, Firm Intratesticular Mass that cannot be
Transilluminated should be regarded as Malignant unless otherwise
proved.
Tumor markers
TWO MAIN CLASSES
o Onco-fetal Substances : AFP & HCG
o Cellular Enzymes : LDH & PLAP
AFP - Trophoblastic Cells
HCG - Syncytiotrophoblastic Cells
( PLAP- placental alkaline phosphatase, & LDH lactic acid dehydrogenase)
ROLE OF TUMOUR MARKERS
o Degree of Marker Elevation Appears to be Directly Proportional to
Tumor Burden
o Markers indicate Histology of Tumor:
If AFP elevated in Seminoma - Means Tumor has Non-Seminomatous
elements
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
19
©Ali Kareem 2015-2016
o Negative Tumor Markers becoming positive on follow up usually
indicates - Recurrence of Tumor
o Markers become Positive earlier than X-Ray studies
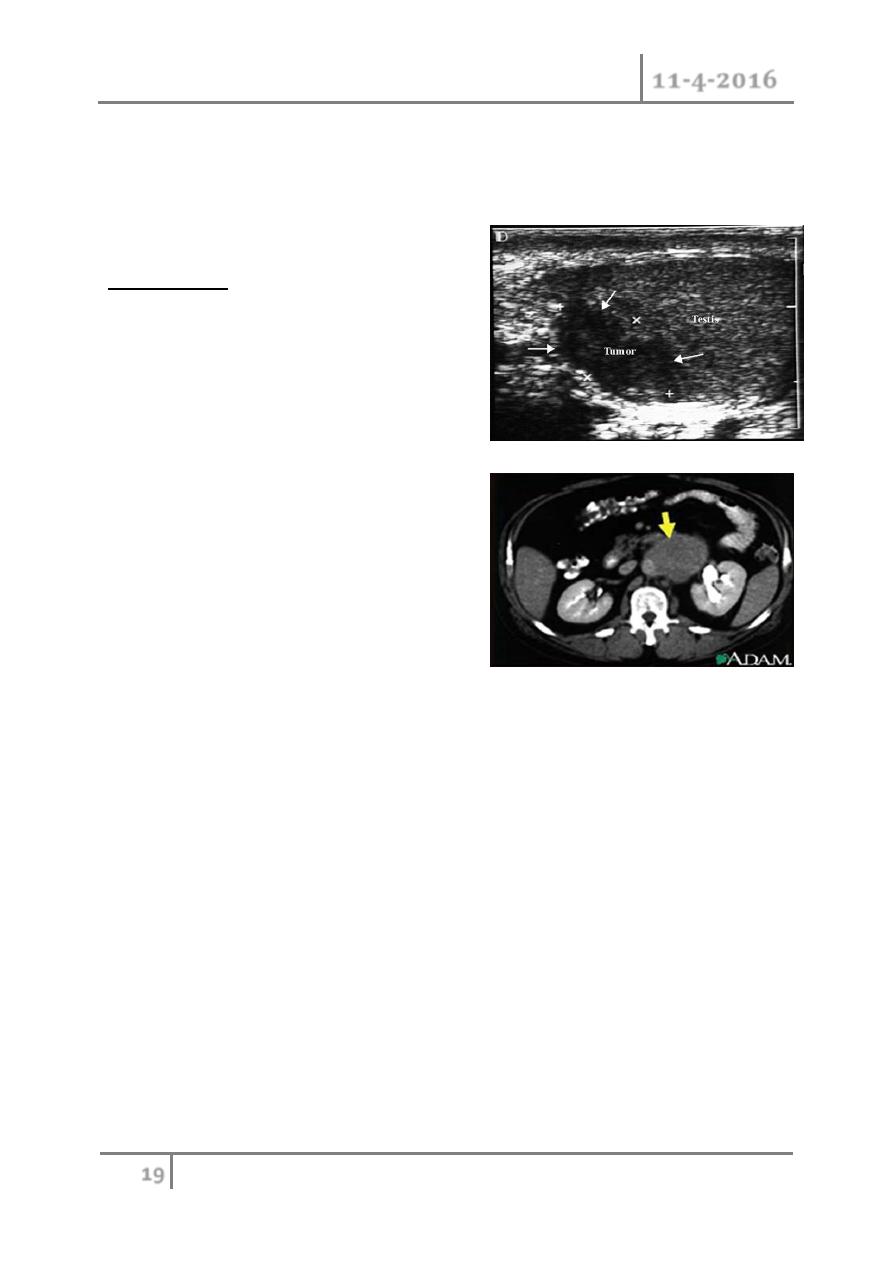
Investigation:
o US testis
o CXR
metastasis
o CT scan
abdomen and
chest to identify lymph
nodes and pulmonary mets
o Tumor markers :AFP (yolk-sac cell),
βHCG (trophoblastic cells).
Tumor staging
o Primary Tumor (T)pTX - Primary tumor cannot be assessed .
o pT0 - No evidence of primary tumor.
o pTis - Intratubular germ cell neoplasia.
o pT1 - Tumor limited to the testis and epididymis.
o pT2 - Tumor limited to the testis and epididymis with vascular/lymphatic
invasion or tumor extending through the tunica albuginea with
involvement of tunica vaginalis
o pT3 - Tumor invades the spermatic
o pT4 - Tumor invades the scrotum
Regional Lymph Nodes
o Clinical NX - Regional lymph nodes cannot be assessed
o N0 - No regional lymph node metastasis
o N1 - Lymph node mass 2 cm or less in greatest dimension.
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
20
©Ali Kareem 2015-2016
o N2 - Lymph node mass, more than 2 cm but not more than 5 cm in
greatest dimension.
o N3 - Lymph node mass more than 5 cm in greatest dimension
Distant metastasis
o M0 - No evidence of distant metastases
o M1 - Nonregional nodal or pulmonary metastases
o M2 - Nonpulmonary visceral masses
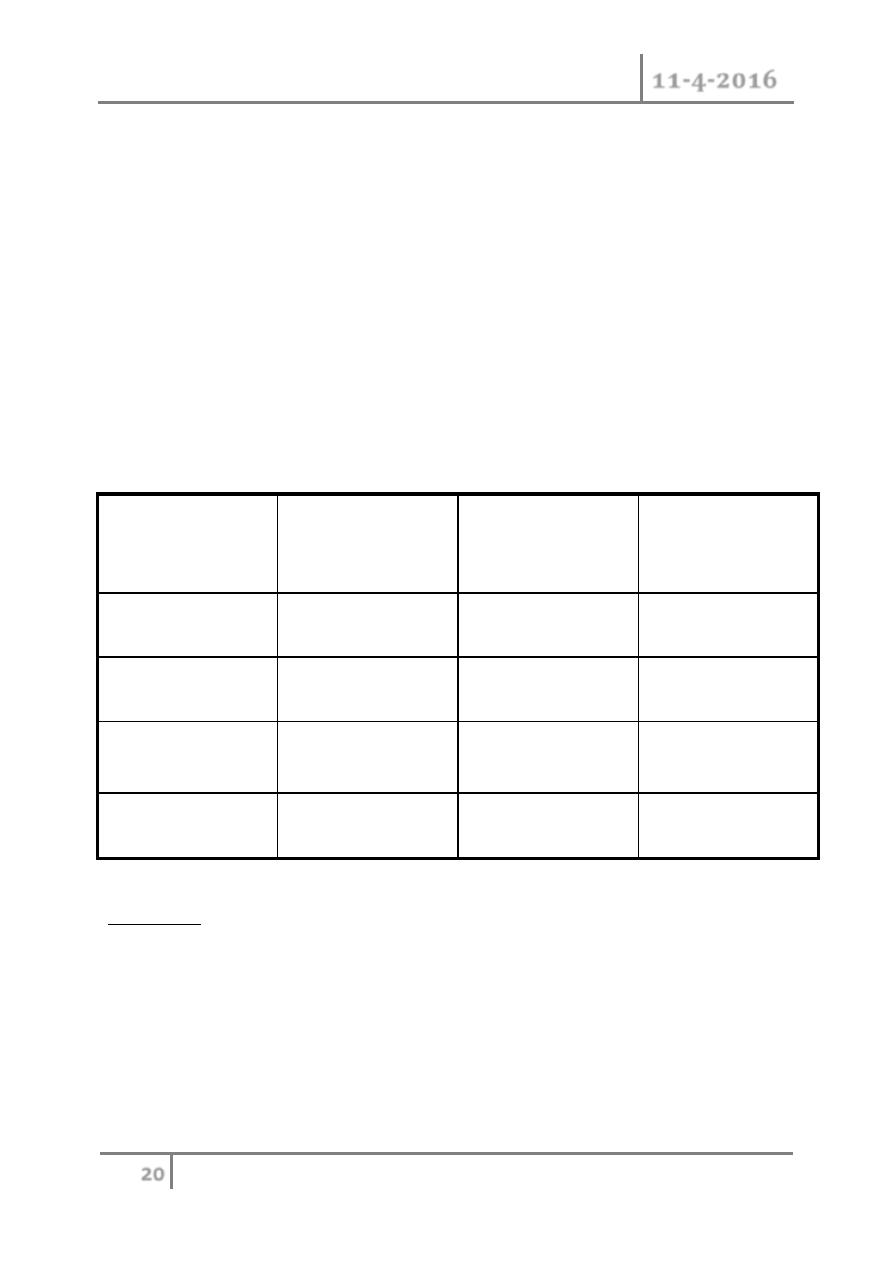
Serum tumor markers
LDH
HCG
Miu/ml
AFP
Ng/ml
S0
_< N
<N
<N
S1
<1.5 x N
< 5000
< 1000
S2
1.5-10x N
5000 to 50000
1000 to 10000
S3
>10x N
> 50000
>10000
Treatment:
o Explore testis through an inguinal incision.
o Radical Orchidectomy.
o Further treatments depends on the type and stage ( see Table) .
o Chemotherapy regimen : BEP :Bleomycine , Etopside ,Cisplatine
o DXT=deep x-ray therapy, RPLND=retroperitoneal lymph node
dissection
Scrotal Disorders Dr. Saad Dakhil
11-4-2016
21
©Ali Kareem 2015-2016
END OF THIS LECTURE …
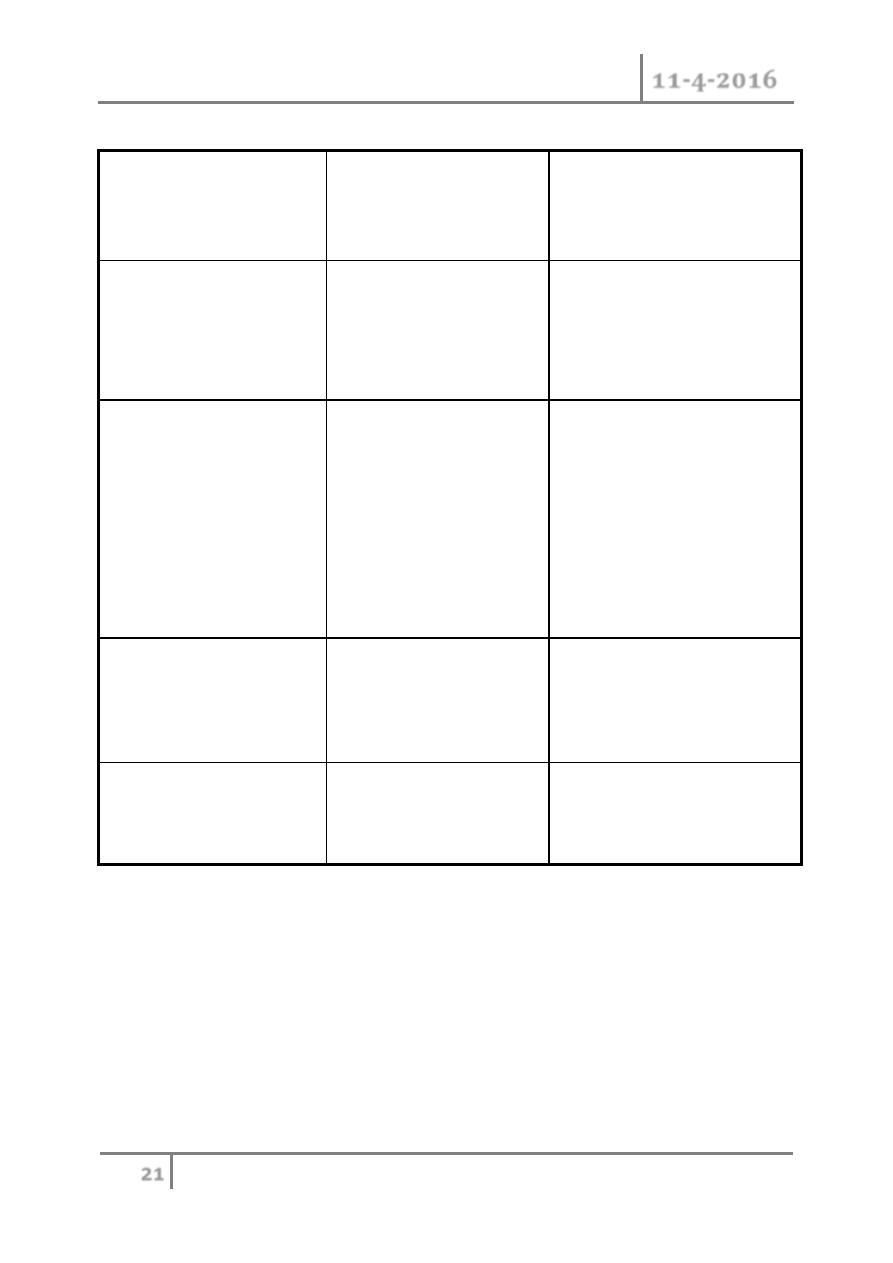
Staging
Treatment of seminoma
Treatment of non-
seminomatous germ cell
tumor
Stage I
confined to the testis
DXT to the abdominal
nodes or single agent
carboplatine chemo
therapy
Observation or
RPLND
Or primary chemotherapy
Stage II
Retroperitolneal LN
involvement
II a : nodes <2cm
II b : nodes 2-5cm
II c : nodes >5cm
DXT to abdominal
nodes.
or
Chemotherapy
Chemo & RPLND of
residual tumor
Stage III
nodal dx above the
diaphragm
DXT to abdominal wall
& thoracic nodes or
chemo therapy
Chemotherapy
Stage IV
visceral metastasis
Chemotherapy
Chemotherapy
