Baghdad College of Medicine / 4
th
grade
Student’s Name :
Dr. Muayed Abbas
Lec. 6
ADRENAL GLANDS
Thurs. 10 / 3 / 2016
DONE BY : Ali Kareem
مكتب اشور لالستنساخ
2015 – 2016
Adrenal Glands Dr. Muayad Abbas
10-3-2016
2
©Ali Kareem 2015-2016
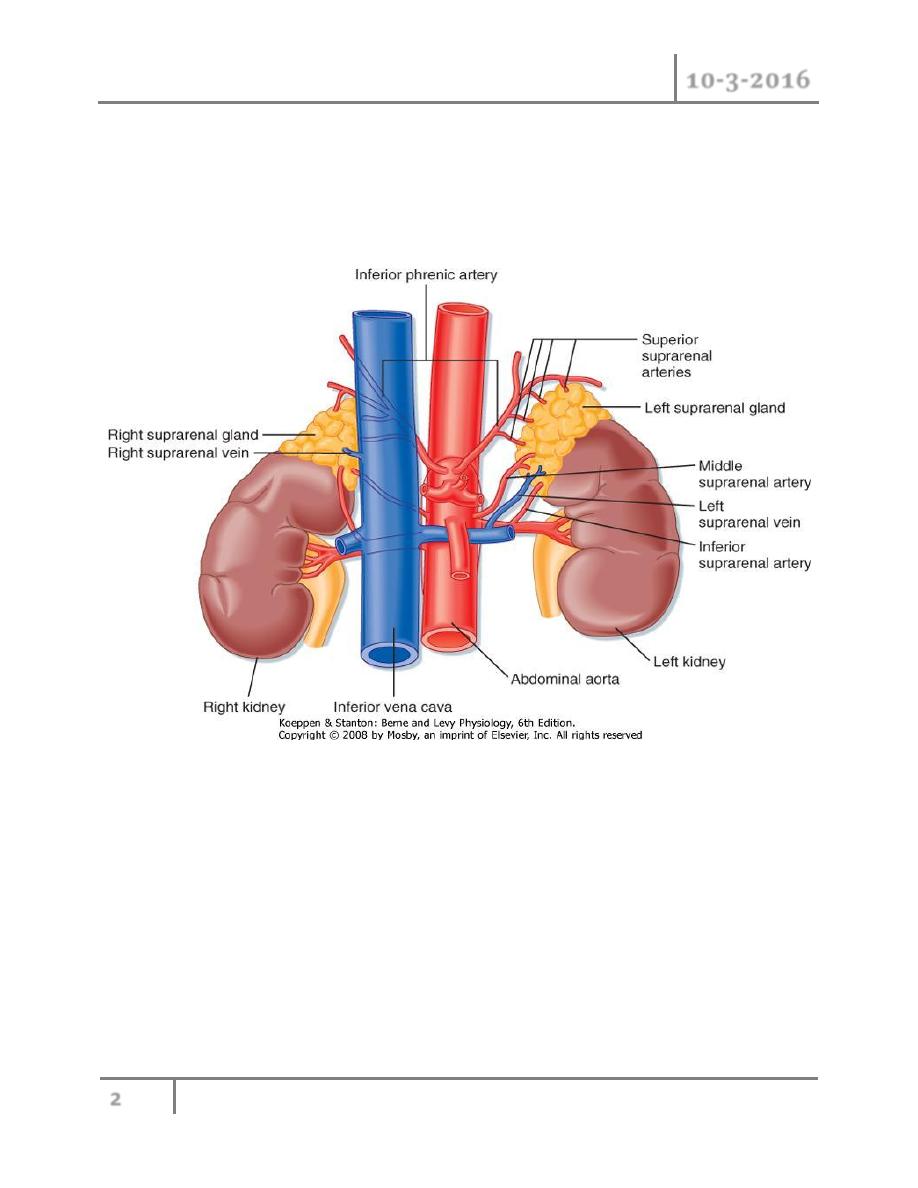
Adrenal Glands
ANATOMY
o Weight
-----
4 g.
o Inner adrenal medulla and the outer adrenal cortex .
o Situated near the upper poles of the kidneys, in the retroperitoneum, within
Gerota’s capsule.
Function of the adrenal glands
o Response to stress
o Catechol amines are secreted by the adrenal medulla

Adrenal Glands Dr. Muayad Abbas
10-3-2016
3
©Ali Kareem 2015-2016
o Corticosteroids, aldosterone and cortisol are synthesised in the adrenal
cortex
o
Catechol amines act on α and β receptors on target organs:
o Increase in blood pressure and heart rate;
o Vasoconstriction of vessels in the splanchnic system and vasodilatation of
vessels in the muscles;
o Bronchodilatation; and increased glycogenolysis in liver and muscles:
o all necessary for the flight/fight
o Zona glomerulosa produce aldosterone, which regulates sodium– potassium
homeostasis.
o The target organs of aldosterone are the kidneys ,sweat and salivary glands
and the intestinal mucosa
o Sodium retention and potassium excretion
o Regulatd by renin–angiotensin system and the serum potassium
concentration.
o Zona fasciculata and zona reticularis synthesise cortisol and the adrenal
androgens dehydroepiandrosterone (DHEA) and its sulphate
(dehydroepiandrosterone sulphate (DHEAS)).
o Precursors of androgens and are converted in peripheral tissues such as fat
Cortisol secretion is regulated by adrenocorticotrophic hormone (ACTH),
which is produced by the anterior pituitary gland.
The hypothalamus controls ACTH secretion by secreting corticotropin-
releasing hormone (CRH).
The serum cortisol level inhibits the release of CRH and ACTH via a closed-
loop system (negative feedback loop).
Cortisol has numerous metabolic and immunological effects
Increases gluconeogenesis and lipolysis,
Decreases peripheral glucose utilisation,
Immunological response and muscular mass.
It affects fat distribution,

Adrenal Glands Dr. Muayad Abbas
10-3-2016
4
©Ali Kareem 2015-2016
Wound healing and bone mineralisa- tion; and alters mood (euphoria or,
rarely, depression) and cortical alertness.
Incidentaloma
Definition
o Incidentaloma is an adrenal mass, detected incidentally by imag- ing studies
conducted for other reasons, not known previously to have been present or
causing symptoms.
Incidence
o
Autopsy….. 1.4 to 8.7 per cent
o Imaging studies in 1 per cent
o 75 per cent are non-functioning adenomas but Cushing’s adenomas,
phaeochromocytomas, metastases, adrenocortical carcinomas and Conn’s
tumours can all be found
Diagnosis
o Complete history and clinical examination
o Exclude a functioning or malignant adrenal tumour.
o Morning and midnight plasma cortisol measurements;
o 1-mg overnight dexamethasone suppression test;
o 24-hour urinary cortisol excretion;
o 12 or 24-hour urinary excretion of metanephrines or plasma- free
metanephrines;
o Serum potassium, plasma aldosterone and plasma renin activity;
o SerumDHEAS,testosteroneor17-hydroxyestradiol(virilising or feminising
tumour).
o Computed tomography (CT) or magnetic resonance imaging (MRI) should
be performed in all patients with adrenal masses.
o Adrenocortical car- cinoma increases with the size of the mass (25 per cent
>4 cm).

Adrenal Glands Dr. Muayad Abbas
10-3-2016
5
©Ali Kareem 2015-2016
o Adrenal metastases are likely in patients with a history of cancer elsewhere
and the sole indications for biopsy of an adrenal mass is to confirm a
suspected metastasis from a distant primary site.
Adrenal gland biopsy
o Never biopsy an adrenal mass until phaeochromocytoma has been
biochemically excluded
o The indication for adrenal gland biopsy is to confirm adrenal gland
metastasis
Treatment
o Non-functioning adrenal tumour greater than 4 cm in diam- eter and
smaller tumours that increase in size over time should undergo surgical
resection. Non-functioning tumours smaller than 4 cm should be followed-up
after 6, 12 and 24 months by imaging (MRI) and hormonal evaluation.
Adrenal metastases
o One-third of patients with malignant disease .
o Most common primary tumours are breast, lung, renal, gastric, pancreatic,
ovarian and colorectal cancer.
o In selected circumstances an adrenalectomy is appropriate, for example if it
is the sole site of metastatic disease.
Adrenocortical carcinoma
Pathology :
o Differentiation between benign and malignant adrenal tumours is
challenging.
o Tumors size,
o The presence of necrosis or haemorrhage and microscopic features such as
capsular or vascular invasion.

Adrenal Glands Dr. Muayad Abbas
10-3-2016
6
©Ali Kareem 2015-2016
o Macroscopic features are commonly multinodularity and heterogeneous
structure with haemorrhage and necrosis.
Clinical presentation
o
60 per cent of patients present with evidence of cortisol excess (Cushing’s
syndrome)
o Patients with non-func- tioning tumours frequently complain of abdominal
discomfort or back pain caused by large tumours.
o Adrenal tumours secreting more than one hormone in excess, or
feminising/masculanising steroids are likely to be malignant.
Diagnosis
o Measurements of DHEAS, cortisol and catecholamines to exclude a
phaeochro- mocytoma and a dexamethasone suppression test
o MRI and CT are equally effective in imaging adrenocortical carcinoma
o MRI angiography is useful to exclude tumour thrombus in the vena cava
o CT scan of the lungs is recommended
Staging
o The World Health Organization classification of 2004 is based on the
McFarlane classification and defines four stages:
o Tumours <5 cm (stage I)
o or >5 cm (stage II),
o Locally invasive tumours (III) or
o Tumours with distant metastases(IV)
o Functioning tumours tend to do worse than non-functioning, but have the
advantage of a serum marker which can be used for follow up and disease
monitoring.

Adrenal Glands Dr. Muayad Abbas
10-3-2016
7
©Ali Kareem 2015-2016
Treatment
o Complete tumour resection (R0) is associated with favourable survival
and should be attempted whenever possible.
o In order to prevent tumour spillage and implantation metastases, the
capsule must not be damaged.
o En bloc resection with removal of locally involved organs is often
required and in case of tumour thrombus in the vena cava thrombectomy
is needed.
o Laparoscopic adrena lectomy is associated with a high incidence of local
recurrence and cannot be recommended
o Tumors debulking plays a role in functioning tumours to control hormone
excess
o Patients can be treated postoperatively with mitotane alone or in
combination with etoposide, doxorubicin and cisplatin.
o Adjuvant radiotherapy may reduce the rate of local recurrence
o Restaging every three months is required as the risk of tumour relapse is
high.
Prognosis
o Stage I or II disease -five-year survival rate of 25 per cent
o Stage III and stage IV disease - five- year survival rates of 6 and 0 per cent,
respectively.
Phaeochromocytoma and paraganglioma
Definition
o Tumours of the adrenal medulla and sympathetic gan-glia which are derived
from chromaffin cells and which produce catecholamines.
Aetiology
o In total, 4 per cent of incidentalomas are phaeochromocytomas
Adrenal Glands Dr. Muayad Abbas
10-3-2016
8
©Ali Kareem 2015-2016
o Sporadic phaeochromocytomas occur around the fourth decade whereas
patients with hereditary forms are diagnosed earlier.
o
10 per cent tumour’
o 10 per cent of tumours are inherited,
o 10 per cent are extra-adrenal,
o 10 per cent are malignant, 10 per cent are bilateral
o 10 per cent occur in children.
o Hereditary phaeochromocytomas occur in several tumour syndromes:
o Multiple endocrine neoplasia type 2 (MEN 2):
o Familial paraganglioma (PG) syndrome:
o von Hippel–Lindau (VHL) syndrome:
o Neurofibromatosis (NF) type 1:
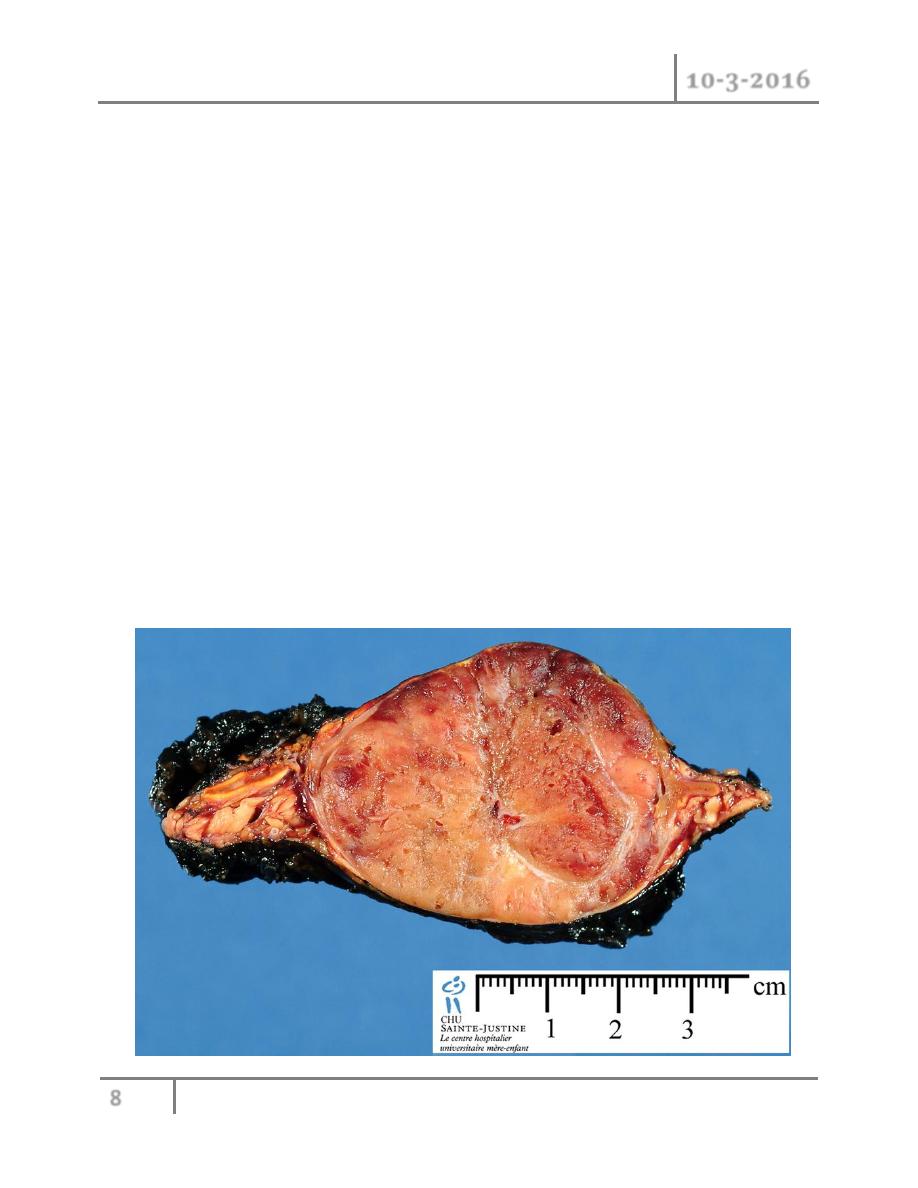
Pathology
o greyish-pink on the cut surface and are usually highly vascularised. Areas of
haemorrhage or necrosis are often observed

Adrenal Glands Dr. Muayad Abbas
10-3-2016
9
©Ali Kareem 2015-2016
o The differentiation between malignant and benign tumours is difficult,
except if metastases are present.
o An increased PASS (phaeo- chromocytoma of the adrenal gland scale
score), a high number of Ki-67-positive cells, vascular invasion or a
breached capsule all lean more towards malignant rather than benign.
o Phaeochromocytomas may also produce calcitonin, ACTH, vasoactive
intestinal polypeptide (VIP) and parathyroid hor- mone-related protein
(PTHrP).
Clinical features
o catecholamine excess and are typically intermittent.
o 90 per cent of patients with the combination of headache, palpitations and
sweating have a phaeochromocytoma.
o Paroxysms may be precipitated by physical training, induction of general
anaesthesia and numerous drugs and agents (contrast media, tricyclic anti-
depressive drugs, metoclopramide and opiates).
o Hypertension may occur continuously, be intermittent or absent
o A subset of patients are asymptomatic.
Diagnosis
o Determination of adrenaline and noradrenaline breakdown products,
metanephrine and normetanephrine level, in a 12- or 24-hour urine
collection.
o Determination of plasma-free metanephrine and normetanephrine levels
also has a high sensitivity
o Biochemical tests should be performed at least twice.
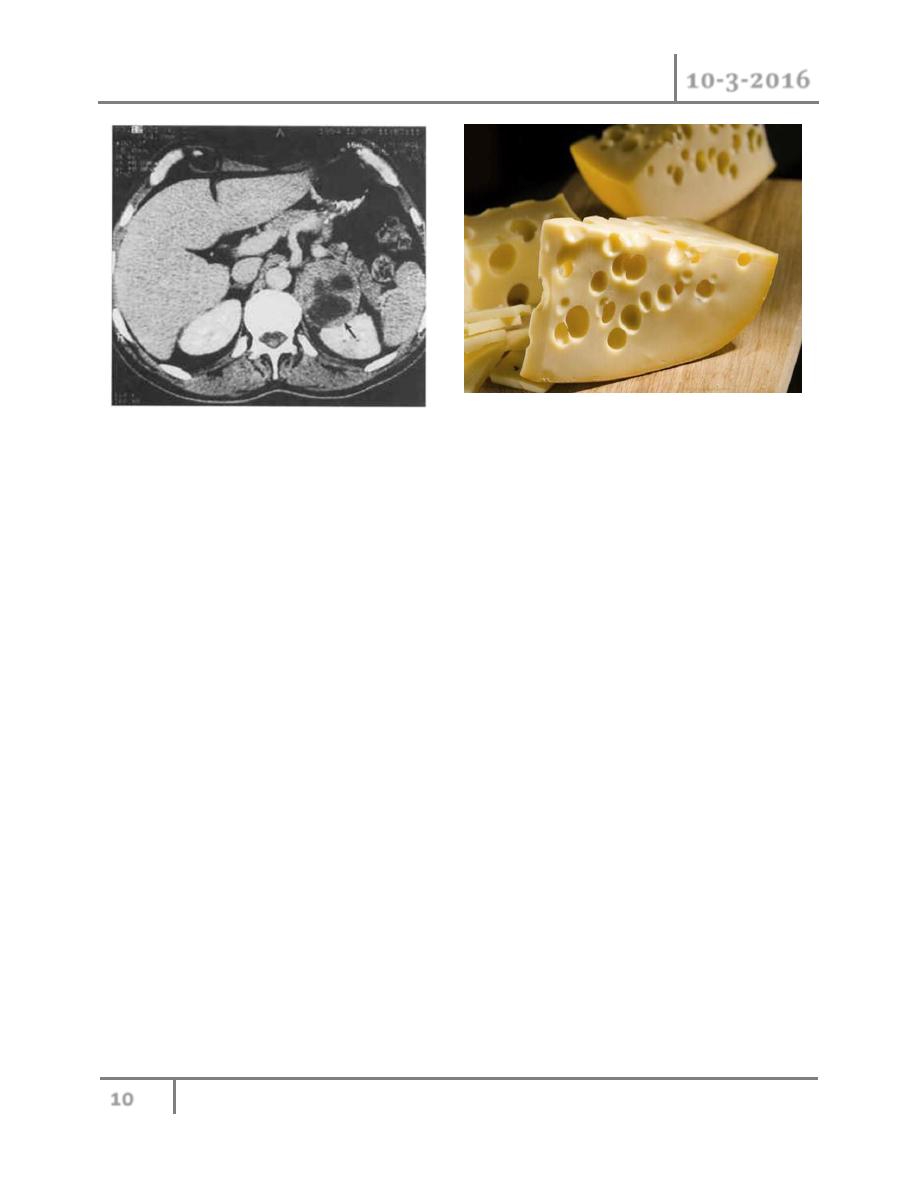
o Locali- sation of the phaeochromocytoma. MRI is preferred because
contrast media used for CT scans can provoke paroxysms. Classically,
phaeochromocytomas show a ‘Swiss cheese’ con- figuration.
Adrenal Glands Dr. Muayad Abbas
10-3-2016
10
©Ali Kareem 2015-2016
o 123I-MIBG (metaiodobenzylguanidine) single-photon emission computed
tomography (SPECT) will identify about 90 per cent of primary tumours and
is essential for the detection of multiple extra-adrenal tumours and
metastases.
o PET scanning using FDG PET or DOPA PET is yet more sensitive in
detecting metastatic foci.
Treatment
o Laparoscopic resection is now routine in the treatment of
phaeochromocytoma.
o If the tumour is larger than 8–10 cm or radiological signs of malignancy are
detected, an open approach should be considered
Preoperative
o
Once a phaeochromocytoma has been diagnosed, an α-adrenoreceptor
blocker (phenoxybenzamine) is used to block catecholamine excess and its
consequences during surgery.
o WITH dequate medical pretreatment, the perioperative mortality rate has
decreased from 20–45 per cent to less than 3 per cent

Adrenal Glands Dr. Muayad Abbas
10-3-2016
11
©Ali Kareem 2015-2016
o A dose of 20 mg of phenoxybenzamine initially should be increased daily by
10 mg until a daily dose of 100–160 mg is achieved and the patient reports
symptomatic postural hypotension.
o
β-blockade is required if tachycardia or arrhythmias develop; this should
not be introduced until the patient is α-blocked.
o Special attention is required when the adrenal vein is ligated as a sudden
drop in blood pressure may occur.
o The infusion of large volumes of fluid or administration of noradrenaline
can be necessary to correct postoperative hypotension in the presence of
unopposed α-blockade.
Postoperative
o Patients should be observed for 24 hours in the intensive care or high
dependency unit as hypovolaemia and hypoglycaemia may occur.
o Lifelong yearly biochemical tests should be performed to identify recurrent,
metastatic or metachronous phaeochromocy- toma
Malignant phaeochromocytoma
o
o Approximately 10 per cent of phaeochromocytomas are malignant. This rate
is higher in extra-adrenal tumours (paragangliomas).
o The diagnosis of malignancy implies metastases of chromaffin tissue, most
commonly to lymph nodes, bone and liver.
o
Symptomatic treatment can be obtained with α-blockers.
o Mitotane should be started as adjuvant or palliative treatment. Treatment
with 131I-MIBG or combination chemotherapy has resulted in a partial
response in 30 per cent and an improvement of symptoms in 80 per cent of
patients.
o The natural history is highly variable with a five-year survival rate of less
than 50 per cent.

Adrenal Glands Dr. Muayad Abbas
10-3-2016
12
©Ali Kareem 2015-2016
Treatment
o Surgical excision is the only chance for cure.
o Even in patients with metastatic disease, tumour debulking can be
considered to reduce the tumour burden and to control the catecholamine
excess.
Ganglioneuroma
Definition
o A ganglioneuroma is a benign neoplasm that arises from neural crest tissue.
o Ganglioneuromas can occur in the adrenal medulla characterised by
mature sympathetic ganglion cells and Schwann cells in a fibrous stroma.
Clinical features
o all age groups
o more common before the age of 60.
o anywhere along the paravertebral sympathetic plexus and in the adrenal
medulla (30 per cent).
o Mostly identified incidentally by CT or MRI performed for other indications
Treatment
o Treatment is by surgical excision, laparoscopic when adrenalec- tomy is
indicated.
SURGERY OF THE ADRENAL GLANDS
o Since its introduction in the 1990s, laparoscopic or retrop- eritoneoscopic
adrenalectomy has become the ‘gold standard’ in the resection of adrenal
tumours, except for tumours with signs of malignancy.
o The mortality rate ranges from 0 to 2 per cent in specialised centres.

Adrenal Glands Dr. Muayad Abbas
10-3-2016
13
©Ali Kareem 2015-2016
o In the case of small, bilateral tumours or in patients with hereditary tumour
syndromes a subtotal resection is warranted, to avoid steroid dependence.
o An open approach should be considered if:
o radiological signs, distant metastases, large tumours (>8–10 cm) or a
distinct hor monal pattern suggest malignancy
o Laparoscopic adrenalectomy
END OF THIS LECTURE…
