Baghdad College of Medicine / 4
th
grade
Student’s Name :
Dr. Mohanned Al-Fallouji
Lec. 4
Cervical Lymph Nodes
Thurs. 3 / 3 / 2016
DONE BY : Ali Kareem
مكتب اشور
لالستنساخ
2015 – 2016
Cervical LNs Dr. Mohanned Al-Fallouji
3-3-2016
2
©Ali Kareem 2015-2016
Cervical Lymph Nodes
Objectives
1- To reveal details of Cervical LNs’ Surgical Anatomy.
2- To know the causes of Lymphadenopathy.
3- To handle enlarged Supraclavicular LN management.
4- How to diagnose the Cervical Lymphadenopathy.
5- How to treat Tuberculous Lymphadenopathy.
Cervical LNs Dr. Mohanned Al-Fallouji
3-3-2016
3
©Ali Kareem 2015-2016
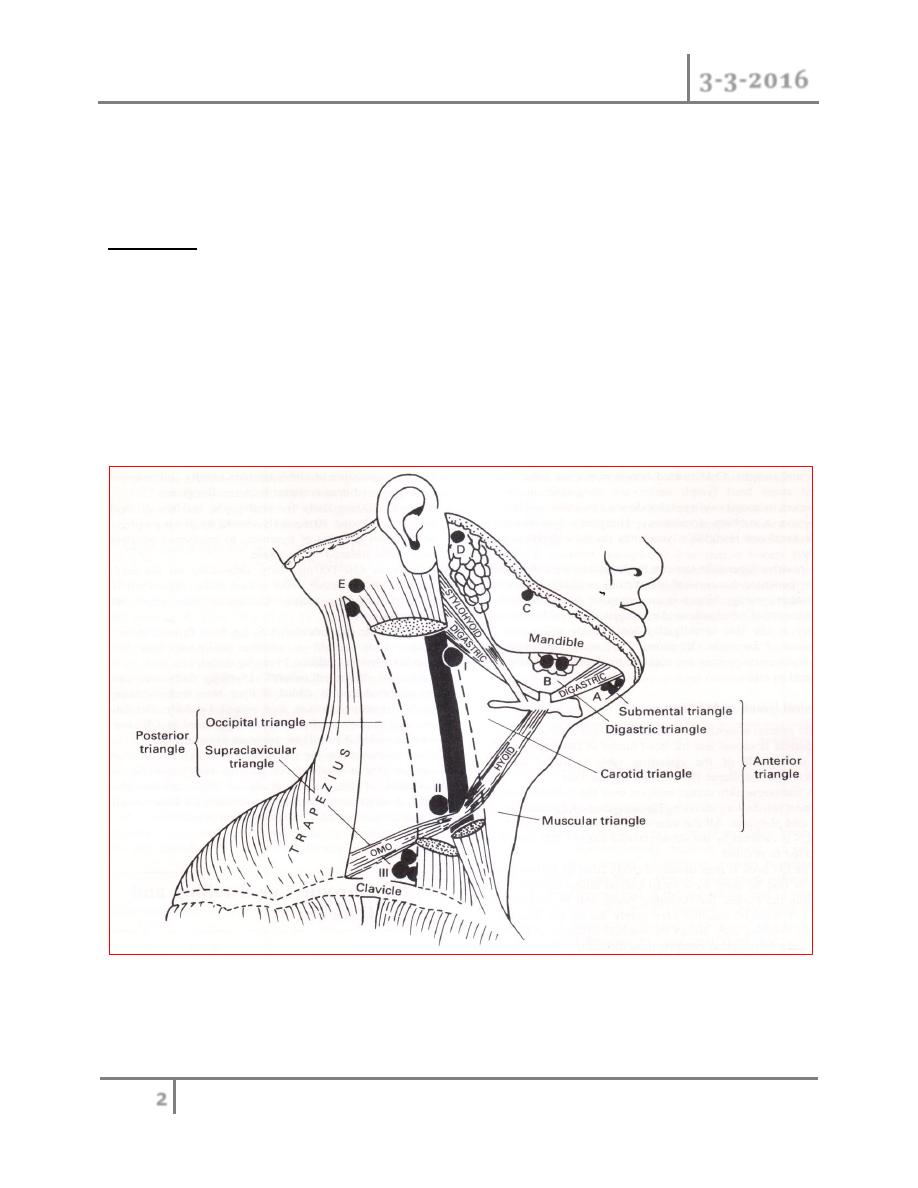
Surgical Anatomy
Cervical Lymph Nodes :
The human body contains about 800 lymph nodes (LN), of which 300 are
located in the neck.
About 150 are in the Mesentery.
The lymphatic drainage of the head and neck is arranged into superficial
and deep.
The superficial group has 2 'circles‘:
The inner circle
The outer circle.
The Superficial Lymph Nodes comprise following elements.
Outer circle of nodes from chin to occiput is made up of :
A. The submental nodes : three or four nodes lie just beneath the chin. They
drain the tip of the tongue. floor of the mouth lingual and labial gum. They
drain into the submandibular group but a few efferents pass direct to the
jugulo-omohyoid node.
B. The submandibular nodes drain a wide area from the centre of the
forehead. nose and nearby cheek. upper lip and the anterior two-thirds of
the tongue, floor of mouth and gums. They receive lymph from the upper
and lower teeth, from the anterior half of the nasal cavity and from the
frontal and maxillary and middle and anterior ethmoidal sinuses. Most of
the submandibular nodes drain into the jugulo-omohyoid node; a few drain
into the jugulo-diagastric node.
C. Buccal and mandibular nodes: a small node lies isolated on the baccinator
muscle, another on the lower border of the mandible at the anterior border
of the masseter. They drain part of the cheek and lower eyelid. Their
efferents pass to the jugulo-digastric node.

Cervical LNs Dr. Mohanned Al-Fallouji
3-3-2016
4
©Ali Kareem 2015-2016
D. Pre-auricular nodes: these lie on and within the parotid gland: one or two
are subcutaneous. The subcutaneous nodes drain the skin of the temple and
vertex. forehead and eyelids. pinna and external acoustic meatus.These
drain through the deep cervical fascia into supraclavicular nodes. The deep
nodes receive from the back of the orbit, from the infratemporal fossa, and
from the parotid gland itself. They drain into the deep members of the deep
group.
E. Occipital nodes: these drain the posterior part of the scalp and auricle.
The efferents pass to the supraclavicular nodes.
The inner circle lies within the surrounding larynx, trachea, and pharynx.
It comprises pre-tracheal, para-tracheal and retro-pharyngeal LNs.
The pre-tracheal LNs drain the lower larynx, trachea and thyroid isthmus.
The retro-pharyngeal LNs drain the soft palate, posterior parts of hard palate
and nose, as well as the pharynx itself.
Tonsils, lingual tonsil, palatine tonsil and adenoids sometimes called inner ring
of waldeyer. These then drain into the Deep Cervical LNs.
Deep Cervical Lymph Nodes :
found around the internal jugular vein from the base of the skull to the root of the
neck. They are formed of 3 groups:
I.
The jugulo-digastric node lies below the posterior belly of the digastric
between the angle of the mandible and
the anterior border of
sternomastoid.
II.
The jugulo-omohyoid node lies above the inferior belly of the omohyoid,
behind the jugular vein.
Cervical LNs Dr. Mohanned Al-Fallouji
3-3-2016
5
©Ali Kareem 2015-2016
III.
The supraclavicular lymph nodes extend behind the
border of
sternomastoid into the posterior triangle. Lymph from the deep cervical
nodes is collected into the jugular lymph trunk.
This joins the thoracic duct on the left side: on the right side, it usually opens
independently into the internal jugular or brachiocephalic vein.
Causes of cervical lymphadenopathy
1- Infection
o Acute pyogenic (tonsillitis, dental extraction, middle ear infections,
parotitis, scalp infections)
o Chronic
Non-specific (viral infection)
Specific
Glandular fever (infectious mononucleosis, EBV
infection)
Tuberculosis
Syphilis
Toxoplasmosis
Cat scratch fever
2- Neoplastic
o Metastatic secondary tumours from primary tumours of : squamous
carcinoma of nasopharynx, skin of head, neck, chest, and abdomen.
o Primary tumours :
Hodgkin's lymphoma (adult)
Non-Hodgkin's lymphoma (elderly)
Leukaemia (usually children and young adults)
3- Miscellaneous Sarcoidosis
Cervical LNs Dr. Mohanned Al-Fallouji
3-3-2016
6
©Ali Kareem 2015-2016
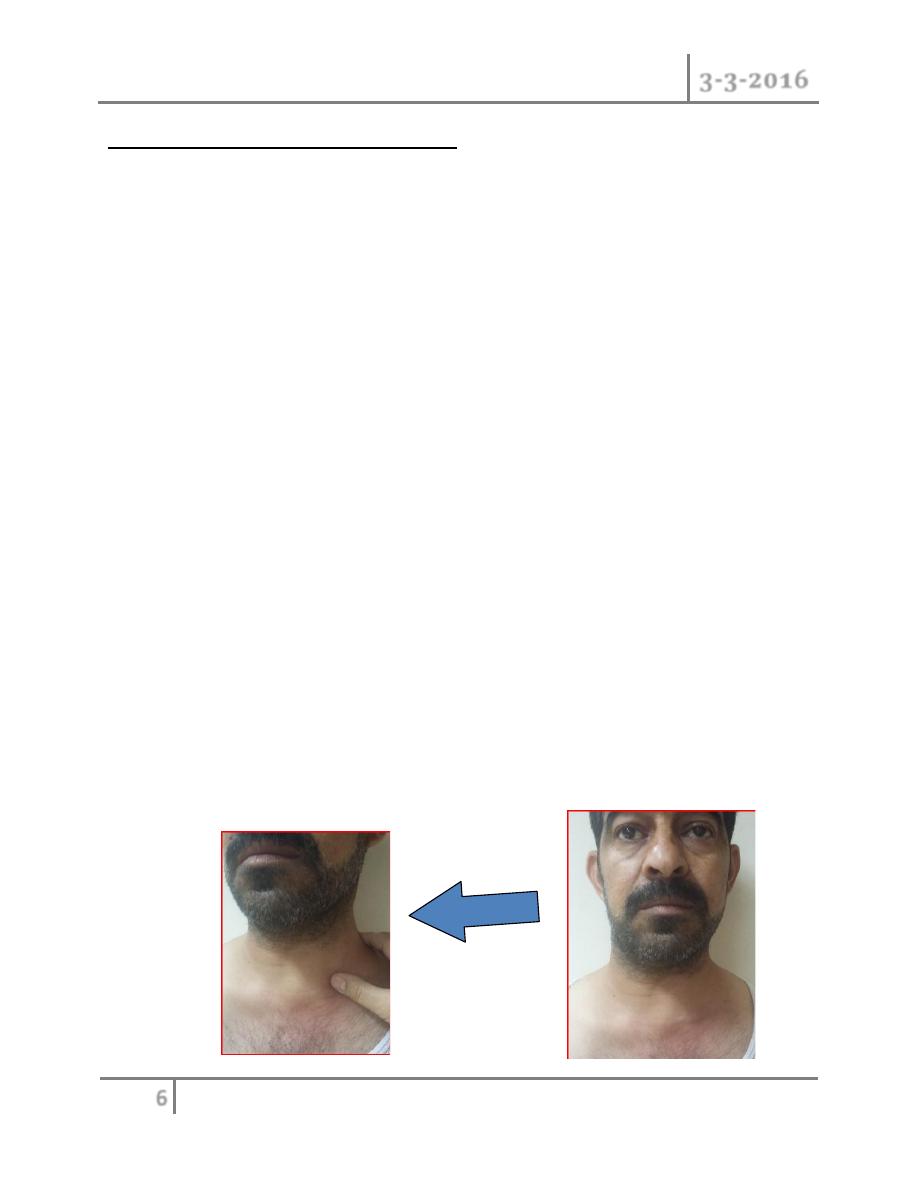
Enlarged Supraclavicular Lymph Nodes
Take the name of the German pathologist Virchow (1821-1902): the classical
enlarged supraclavicular LN (of Virchow) following metastasis from underlying
gastric carcinoma is termed Troisier's sign (named after a French professor of
pathology, 1844-1919).
o Enlarged supraclavicular LN is of great surgical interest. since it is
usually due to neoplastic lesions more than infective ones (the commonest
cause of infective enlargement of supraclavicular lymph nodes is
pulmonary tuberculosis).
o While most upper limb infection can cause epitrochlear and axillary LN
enlargement, infection of the middle finger and dorsum of the hand passes
directly into the supraclavicular LNs.
o Other causes of enlargement include bronchogenic carcinoma (Pancoast
tumor), breast carcinoma, thyroid carcinoma(wrongly called ectopic
thyroid), oesophageal carcinoma, pharyngolaryngeal carcinoma,
Hodgkin's and non-Hodgkin's lymphoma. pancreatic carcinoma and
testicular carcinoma (particularly choriocarcinoma). Hypernephroma can
also give rise to enlarged supraclavicular nodes.
o Superficial and Deep cervical lymph nodes ultimately drain into
supraclavicular lymph nodes. So any enlargement of these glands (due to
infections or neoplasms in the head and neck and upper limbs) will result
in enlargement of the supraclavicular lymph nodes. Enlargement of
supraclavicular may be part of a generalised lymphadenopathy due to
leukemia, lymphoma and AIDS.
Cervical LNs Dr. Mohanned Al-Fallouji
3-3-2016
7
©Ali Kareem 2015-2016
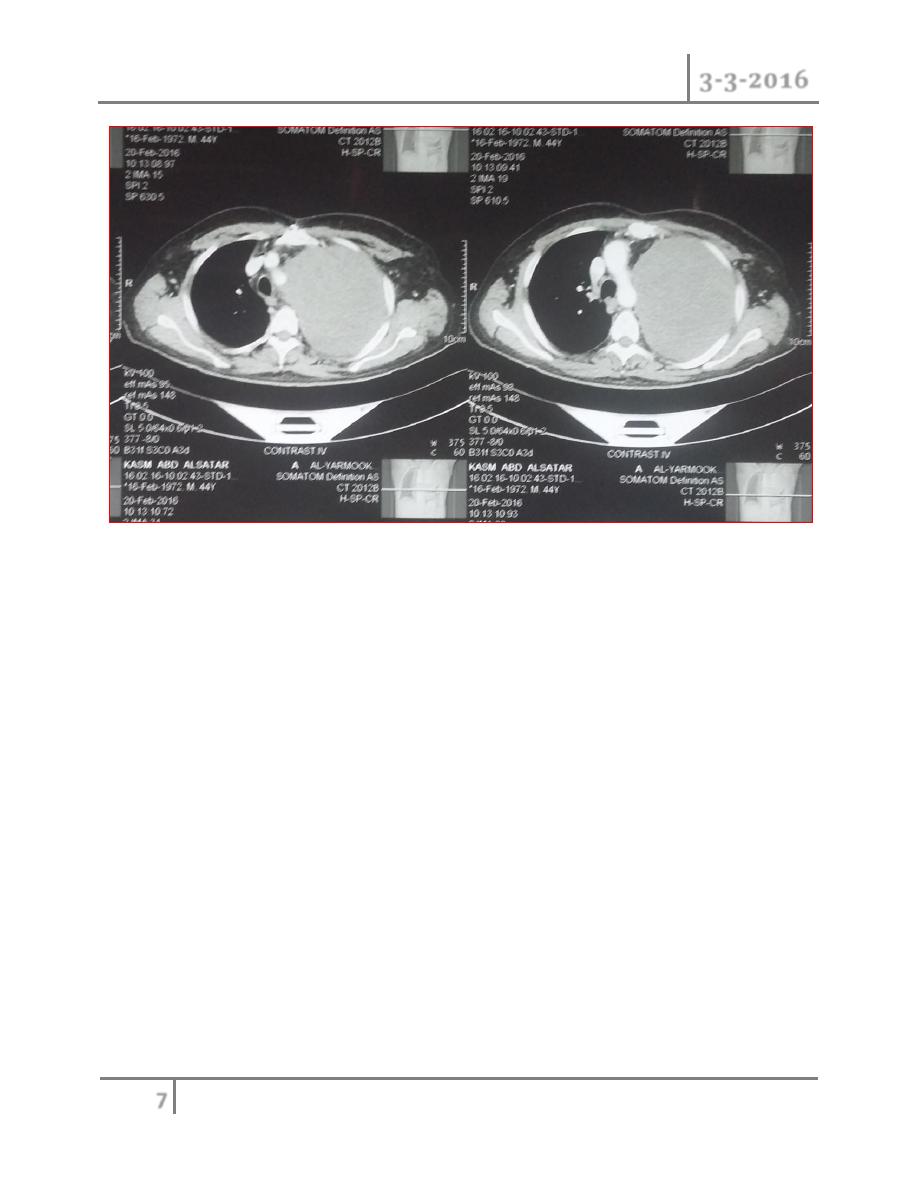
Diagnosis of a Cervical Swelling (due to Lymph Node enlargement)
o Careful history and meticulous physical examination can give the
diagnosis in the majority of cases. Complete ENT examination of
postnasal space, oral cavity, oropharynx and fibreoptic laryngoscopy.
Examine other sites (axilla, epitrochlear, inguinal, spleen, and liver).
o Lymph nodes are tender and hot with evidence of infection (of the
respiratory tract and mouth). Cold matted lymph nodes are tuberculous.
o Fixed stony-hard lymph nodes are metastatic in origin.
o However, in lateral painless swellings that do not move with swallowing
and have a rubbery consistency, Hodgkin's lymphoma (in adults) and
non-Hodgkin's lymphoma (in the elderly) is most likely.
o High ESR, Chest x-ray findings can be confirmed by Positive tuberculin
test can be diagnostic for tuberculosis in any patient with a cervical lymph
node swelling. Past infection with Eptein-Barr virus plays a role in some
Hodgkin’s lymphoma patients.
o Fine needle aspiration cytology biopsy is an important diagnostic tool, in
the presence of an experienced cytologist.
Cervical LNs Dr. Mohanned Al-Fallouji
3-3-2016
8
©Ali Kareem 2015-2016
o Cervical lymph node biopsy is the last investigative tool which will solve
the problems of diagnosis. CT scan, ultrasound, radioactive isotope scan,
and positron emission tomography (PET) may be required to elucidate the
nature of cervical swelling, staging, assessment of response, and direction
of treatment..
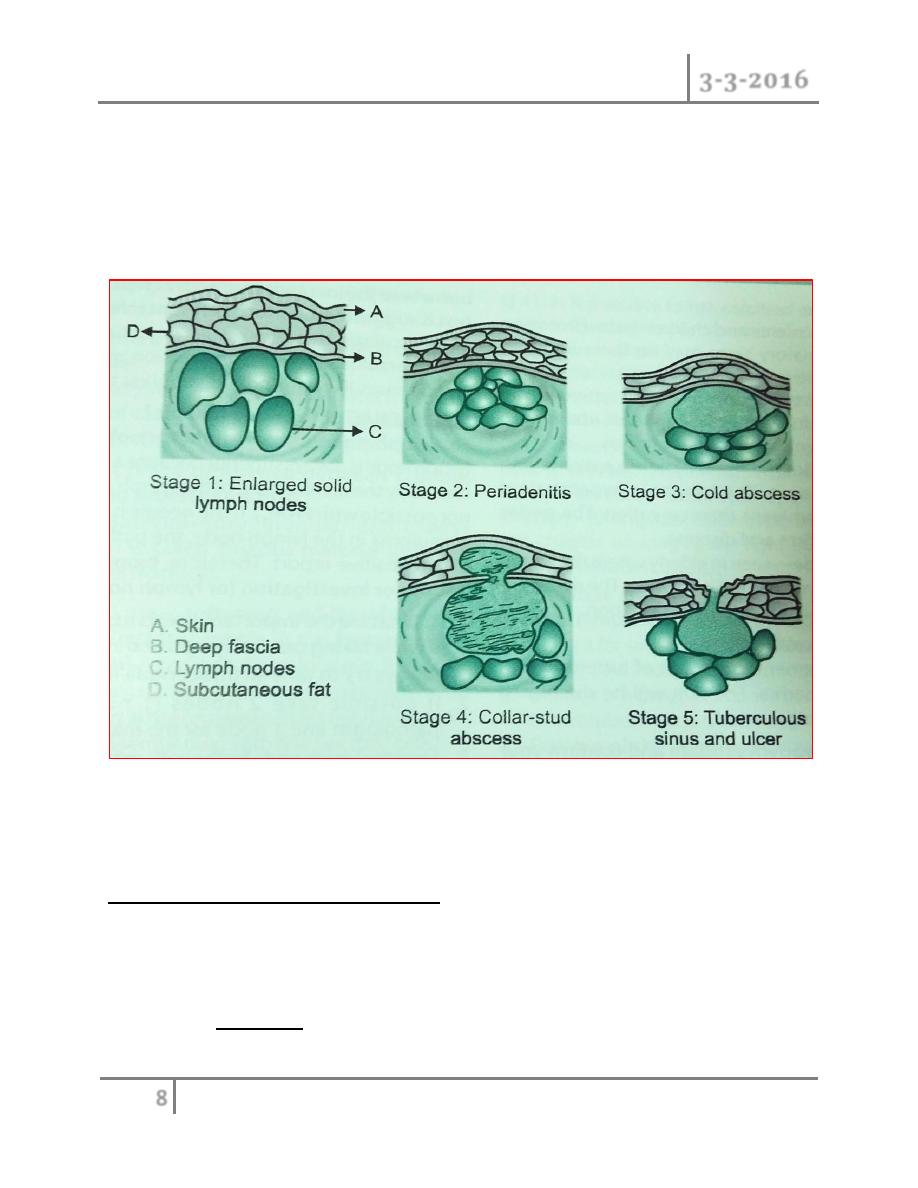
Tuberculosis lymphadenitis stages in order
Treatment of tuberculosis: in 2 phases
Initial phase for 2 months. At least 3 drugs are used to reduce the
population of viable bacteria rapidly and to prevent the emergence of drug-
resistant bacteria.
o Drugs are: Isoniazid 300 mg daily for adults(for children 10 mg/k
daily). Pyridoxine 10mg daily should be given prophylactically from
Cervical LNs Dr. Mohanned Al-Fallouji
3-3-2016
9
©Ali Kareem 2015-2016
the start of treatment to counteract peripheral neuropathy induced by
isoniazid .
o Rifampicin 450 mg daily, depending on the adult's body weight
whether under or over 50 kg respectively (for children 10 mg/kg
daily). Rifampicin may cause liver dysfunction.
o Pyrazinamide (bactericidal) 1.5-2 g daily depending on an adult's
body weight whether under or over 50 kg respectively(for children 35
mg/kg daily).
o Additional drugs: ethambutol (15 mg/kg daily: can cause colour
blindness) is added if drug resistance is thought likely. Streptomycin
(i.m. injection of 1 g daily; can cause oto- and nephrotoxicity) is
now rarely used in UK, but it may be added if bacilli are resistant to
isoniazid.
Continuation phase for 4 months. Two drugs, isoniazid and rifampicin(for
a total of six months each), are the key components of the second phase of
any antituberculosis regimen. Longer treatment may be necessary for bone
and joint infections, for meningitis, or for resistant organisms.
END OF THIS LECTURE …
