Non traumatic urological emergencies
Dr. Mohammed Bassil1
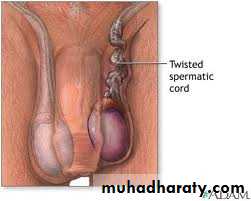
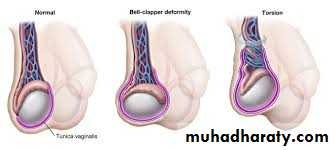
Testicular torsion is a twist of the spermatic cord, resulting in strangulation of the blood supply to the testis.
most frequently between the ages of 10 and 30 (peak incidence 13–15years of age), but any age group may be affected.
Torsion of the testis and testicularappendages
2
There is a sudden onset of severe pain in the hemiscrotum.
and is often associated with nausea.There is sometimes a history of minor trauma to the testis.
Some patients report previous episodes with spontaneous resolution of the pain.
The torted testis is usually moderately swollen and very tender to the touch.
History and examination
3
It may be high riding compared to the contralateral testis and may lie in a horizontal position due to twisting of the cord.
Thecremasteric reflex is nearly always absent.
History and examination
4
Epididymoorchitis.
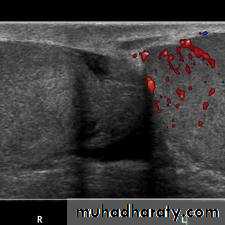
torsion of a testicular appendage.Color Doppler ultrasound .
radionuclide scanning .
In many hospitals these tests are not readily available and the diagnosis is based on symptoms and signs.
Differential diagnosis and investigations
5
6
Scrotal exploration should be undertaken as a matter of urgency since delay in relieving the twisted testis results in permanent ischemic damage to the testis, causing atrophy, loss of hormone and sperm production, and, as the testis undergoes necrosis and the blood–testis barrier breaks down, an autoimmune reaction against the contralateral testis (sympathetic orchidopathy).
Surgical management
7Bilateral testicular fixation should always be performed since the bellclapper abnormality that predisposes to torsion often occurs bilaterally.
Manual detorsion may be attempted in the emergency room while awaiting surgery. Occasionally, the induction of anesthesia will reduce spasm and promote spontaneous detorsion—in both of these instances,
bilateral orchiopexy should still be performed to prevent recurrence.
Surgical management
8
The appendix testis and the appendix epididymis can undergo infarction, causing pain that mimics a testicular torsion.
The “blue dot” sign is the typical physical finding for appendix testis infarction. At scrotal exploration they are easily removed with scissors or electrocautery.
If these diagnoses are confirmed radiographically , analgesics may be given and surgical exploration is unnecessary.
Infarction of testicular appendages
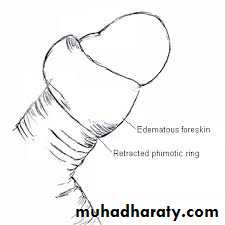
9is when the uncircumcised foreskin is retracted under the glans penis and the foreskin becomes edematous, and cannot be pulled back over the glans into its normal anatomical position.
Paraphimosis is usually painful. The foreskin is edematous and a small area of ulceration of the foreskin may have developed.
Paraphimosis
10
11
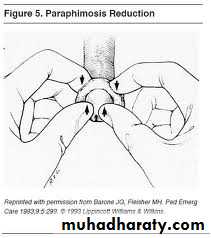
The best initial maneuver for manually reducing paraphimosis is to forcefully squeeze the edematous prepuce for several minutes. Then the skin may be manipulated distally with the fingers of both hands as the glans is pressed down with the thumbs.
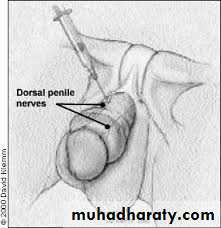
If this fails, the traditional surgical treatment is a dorsal slit under general anesthetic or ring block. A longitudinal incision is made in the tight band of constricting tissue and the foreskin pulled back over the glans.
Treatment
12
Fournier gangrene is a necrotizing fasciitis of the genitalia and perineum primarily affecting males and causing necrosis and subsequent gangrene of infected tissues.
Fournier gangrene
13
Culture of infected tissue reveals a mixed polymicrobial infection with aerobic (E. coli, enterococcus, Klebsiella) and anaerobic organisms (Bacteroides, Clostridium, microaerophilic streptococci).
Fournier gangrene
14
Conditions predisposing to the development of Fournier gangrene include diabetes, local trauma to the genitalia and perineum (e.g., zipper injuries to the foreskin, periurethral extravasation of urine following traumatic catheterization or instrumentation of the urethra), and surgical procedures such as circumcision.
Presentation
15
A fever is usually present, the patient looks very ill, with marked pain in the affected tissues, and the developing sepsis may alter the patient’s mental state. The genitalia and perineum are edematous.
and on palpation of the affected area, tenderness and crepitus may be present, indicating presence of subcutaneous gas produced by gas-forming organisms.
Presentation
16As the infection advances, blisters (bullae) appear in the skin and, within a matter of hours, areas of necrosis may develop on the genitalia and perineum that spread to involve adjacent tissues (e.g., the lower abdominal wall).
The condition advances rapidly—hence its alternative name of spontaneous fulminant gangrene of the genitalia.
Presentation
17The diagnosis is a clinical one and is based on awareness of the condition and a high index of suspicion. CT will demonstrate areas of subcutaneous areas of necrosis and gas.
Diagnosis
18Do not delay. While IV access is obtained, blood taken for culture, IV fluids started, and oxygen administered, broad-spectrum antibiotics are given to cover both gram-positive and gram-negative aerobes and anaerobes.
debridement of necrotic tissue (skin, subcutaneous fat) can be carried out. Extensive areas of tissue may have to be removed.
but it isunusual for the testes or deeper penile tissues to be involved.
Treatment
19Priapism is prolonged and often painful erection in the absence of a sexual stimulus, lasting >4–6 hours, which predominantly affects the corpus cavernosa.
Priapism
20Low-flow (ischemic) priapism
It manifests as a painful, rigid erection, with absent or low cavernosal blood flow. Ischemic priapism beyond 4 hours requires emergency intervention.Blood gas analysis shows hypoxia and acidosis
Classification
21
High-fl ow (nonischemic) priapism
This is usually post-traumatic in nature and does not require emergent intervention. It is due to unregulated arterial blood flow.presenting with a semi-rigid, painless erection.
Blood gas analysis shows similar results to arterial blood.
22
Ischemic priapism of >4 hours implies a compartment syndrome and requires decompression of the corpora cavernosa. Aspiration of blood from corpora ± intracavernosal injection of A1-adrenergic selective agonist are performed every 5–10 minutes until detumescence occurs.
High-fl ow priapism
Early stages may respond to a cool bath or icepack.
Delayed presentations require arteriography and selective embolization of the internal pudendal artery.
Complications
These include fibrosis and impotence.