Dr. Muayad Abbas
Lec. 3
Gall Bladder & Biliary
Tree
Mon. 9 / 11 / 2015
DONE BY : Ali Kareem
مكتب اشور لالستنساخ
2015 – 2016

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
2
Gall bladder and biliary tree
Anatomy
Gall bladder is a pear-shaped structure
7.5–12 cm long,
With a normal capacity of about 35–50 ml
The anatomical divisions are a fundus, a body and a neck that terminates in
a narrow infundibulum
The cystic duct is about 3 cm in length.
Its lumen is usually 1–3 mm in diameter.
The cystic duct joins the common hepatic duct in 80% of cases, in
supradudenal portion
It may extend down into the retroduodenal or even retropancreatic part of
the bile duct before joining.(low insertion)
The cystic duct may join the right hepatic duct or even a right hepatic
sectorial duct
The common hepatic duct is usually less than 2.5 cm long and is formed by
the union of the right and left hepatic ducts.
The common bile duct is about 7.5 cm long and is formed by the junction of
the cystic and common hepatic ducts.
CBD is divided into four parts :
•
The supraduodenal portion, about 2.5 cm long, running in the free edge of
the lesser omentum;
•
The retroduodenal portion;
•
The infraduodenal portion, which lies in a groove on the posterior surface of
the pancreas;

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
3
•
Tthe intraduodenal portion, which passes obliquely through the wall of the
second part of the duodenum, where it is surrounded by the sphincter of
Oddi, and terminates by opening on the summit of the ampulla of Vater.
The cystic artery, a branch of the right hepatic artery.
The most dangerous anomalies are where the hepatic artery takes a tortuous
course on the front of the origin of the cystic duct, or the right hepatic artery
is tortuous and the cystic artery short. The tortuosity is known as the
‘caterpillar turn’ or ‘Moynihan’s hump’
Lymphatics
The lymphatic vessels of the gall bladder (subserosal and submucosal) drain
into the cystic lymph node of Lund (the sentinel lymph node)
Surgical physiology
•
Bile, is composed of 97% water, 1–2% bile salts and 1% pigments,
cholesterol and fatty acids.
•
The liver excretes bile at a rate estimated to be approximately 40 ml h–1.
FUNCTIONS OF THE GALL BLADDER
1-Reservoir for bile.
During fasting, resistance to flow through the sphincter is high, and bile
excreted by the liver is diverted to the gall bladder. After feeding, the
resistance to flow through the sphincter of Oddi is reduced, the gall bladder
contracts, and the bile enters the duodenum.

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
4
These motor responses of the biliary tract are in part effected by the
hormone CCK.
2- concentration of bile by active absorption of water, sodium chloride and
bicarbonate 5–10 times.
3- secretion of mucus
approximately 20 ml is produced per day. With total obstruction of the cystic
duct in a healthy gall bladder, a mucocele developson account of this
function of the mucosa of the gall bladder.
RADIOLOGICAL INVESTIGATION OF THE BILIARY TRACT
Plain radiograph
1- Rradio-opaque gallstones in 10% of patients, the centre of a stone may
contain radiolucent gas in a triradiate or biradiate fissure, and this gives
rise to characteristic dark shapes on a radiograph – the ‘Mercedes-Benz’ or
‘seagull’ sign.
2- Calcification of the gall bladder, a so called ‘porcelain’ gall bladder
,PREMALIGNANT in up to 25% of patients. SO indication for
cholecystectomy.
3- Gas may be seen in the wall of the gall bladder (emphysematous
cholecystitis).
4- Gas in the biliary tree may be seen after endoscopic sphincterotomy or
surgical anastomosis
Investigation of the biliary tree
Ultrasound: stones and biliary dilatation
Plain radiograph: calcification
Magnetic resonance cholangiopancreatography: anatomy and stones

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
5
Multidetector row computerised tomography scan: anatomy, liver, gall
bladder and pancreas cancer
Radioisotope scanning: function
Endoscopic retrograde cholangiopancreatography: anatomy, stones and
biliary strictures
Percutaneous transhepatic cholangiography: anatomy and biliary
strictures
Endoscopic ultrasound: anatomy and stones
Ultrasonography
biliary calculi,
the size of the gall bladder,
the thickness of the gall bladder wall,
the presence of inflammation around the gall bladder,
the size of the common bile duct and, occasionally, the presence of stones
within the biliary tree.
show a carcinoma of the pancreas occluding the common bile duct.
In OBSTRUCTIVE JAUNDICE identify intra- and
Endoscopic ultrasonography :
It provides accurate imaging of the common bile duct and is particularly
useful in detecting stones within the bile ducts,choledocholithiasis.
In addition, it has been shown to be highly accurate in diagnosing and
stataging both pancreatic and periampullary cancers.
Radioisotope scanning
Technetium-99m (99mTc)-labelled derivatives of iminodiacetic acid (HIDA,
IODIDA) for biliary leak or iatrogenic biliary stricture

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
6
TYPES OF CHOLANGIOGRAPH
o Oral cholecystography and intravenous cholangiography
historical interest
discarded
replaced by more accurate imaging modalities
o Percutaneous transhepatic cholangiography
o Endoscopic retrograde cholangiopancreatography
o Peroperative cholangiography
o Operative biliary endoscopy(choledochoscopy)
o Postoperative T-tube cholangiography
GALLSTONES (CHOLELITHIASIS)
Gallstones are the most common biliary pathology.
10–15% of the adult population in the USA.
asymptomatic in the majority (> 80%).
Approximately 1–2% of asymptomatic patients will develop symptoms
requiring cholecystectomy per year,
cholecystectomy one of the most common operations performed by general
surgeons.
Etiology and types of gall stones
Three main types:
cholesterol,
pigment (brown/black)
mixed stones. ,
o Cholesterol or mixed stones contain 51–99% pure cholesterol plus an
admixture of calcium salts, bile acids, bile pigments and phospholipids.

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
7
o The process of gallstone formation is complex
o Obesity,
o high-calorie diets and
o Certain medications can increase the secretion of cholesterol and
supersaturate the bile, increasing the lithogenicity of bile.
o Abnormal emptying of the gall bladder may promote the aggregation of
nucleated cholesterol crystals; hence, removing gallstones without removing
the gall bladder inevitably leads to gallstone recurrence.
o Pigment stone Less than 30% cholesterol.
o There are two types – black and brown.
o Black stones are largely composed of an insoluble bilirubin pigment
polymer mixed with calcium phosphate and calcium bicarbonate.
o Overall, 20–30% of stones are black.
o Black stones accompany haemolysis, usually hereditary spherocytosis or
sickle cell disease.
o For unclear reasons, patients with cirrhosis have a higher instance of
pigmented stones.
o Brown pigment stones contain calcium bilirubinate, calcium palmitate and
calcium stearate, as well as cholesterol.
o Brown stones are rare in the gall bladder.
o They form in the bile duct and are related to bile stasis and infected bile.
o Brown pigment stones are also associated with the presence of foreign
bodies within the bile ducts such as endoprosthesis stents) or parasites such
as Clonorchis sinensis and Ascaris lumbricoides
Clinical presentation
80% asymptomatic
Right upper quadrant or epigastric pain,
may radiate to the back.
colicky,
more often is dull and constant.
dyspepsia,

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
8
flatulence, food intolerance, particularly to fats,
some alteration in bowel frequency.
Biliary colic
Biliary colic is typically present in 10–25% of patients. This is described as
a severe right upper quadrant pain that ebbs and flows for minutes to hours
associated with nausea and vomiting
Jaundice may result if a stone migrates from the gall bladder and obstructs
the common bile duct.
Rarely, a gallstone can lead to bowel obstruction (gallstone ileus).
Acute cholecystitis
When symptoms do not resolve, but progress to continued pain
with fever and leucocytosis,
Effects and complications of gall stones
In the gallbladder
o Biliary colic
o Acute cholecystitis
o Chronic cholecystitis
o Empyema of the gall bladder
o Mucocele
o Perforation
In the bile ducts
o Biliary obstruction
o Acute cholangitis
o Acute pancreatitis
In the intestine
o Intestinal obstruction (gallstone ileus)
Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
9
Differential diagnosis of cholecystitis
Common
o Appendicitis
o Perforated peptic ulcer
o Acute pancreatitis
Uncommon
o Acute pyelonephritis
o Myocardial infarction
o Pneumonia – right lower lobe
Ultrasound scan aids diagnosis
Uncertain diagnosis – do CT scan
Diagnosis
history
physical examination with
confirmatory radiological studies
In the acute phase,
the patient may have right upper quadrant tenderness that is exacerbated
during inspiration by theexaminer’s right subcostal palpation (Murphy’s
sign).
A positive Murphy’s sign suggests acute inflammation and may be
associated with a leucocytosis and moderately elevated liver function test
A mass may be palpable as the omentum walls off an inflamed gall bladder.
Fortunately, in the majority of cases, this process is limited by the stone
slipping back into the body of the gall bladder and the contents of the gall
bladder escaping by way of the cystic duct. This achieves adequate drainage
of the gall bladder and enables the inflammation to resolve.
If resolution does not occur, an empyema of the gall bladder may result. The
wall may become necrotic and perforate, with the development of localised
peritonitis. The abscess may then perforate into the peritoneal cavity with a
septic peritonitis – however, this is uncommon, because the gall bladder is
usually localised by omentum around the perforation.

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
10
A palpable, non-tender gall bladder (Courvoisier’s sign)
. This usually results from a distal common duct obstruction secondary to a
peripancreatic malignancy.
Rarely, a non-tender, palpable gall bladder results from complete
obstruction of the cystic duct with reabsorption of the intraluminal bile salts
and secretion of uninfected mucus secreted by the gall bladder epithelium,
leading to a mucocele
Treatment
•
Most authors would suggest that it is safe to observe patients with
asymptomatic gallstones, with cholecystectomy only being performed for
those patients who develop symptoms or complications of their gallstones.
Prophylactic cholecystectomy
In diabetic patients,
Congenital haemolytic anaemia
Those due to undergo bariatric surgery for morbid obesity,
Because increased risk of complications from gallstones.
o For patients with biliary colic or cholecystitis, cholecystectomy is the
treatment of choice in the absence of medical contraindications.
o The timing of surgery in acute cholecystitis remains controversial.
o early intervention,
o others suggest that a delayed approach is preferable
Conservative treatment followed by cholecystectomy
more than 90% of cases, the symptoms of acute cholecystitis subside with
conservative measures.
Nonoperative treatment is based on four principles:

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
11
1- Nil per mouth (NPO) and intravenous fluid administration.
2- Administration of analgesics.
3- Administration of antibiotics.
As the cystic duct is blocked in most instances, the concentration of
antibiotic in the serum is more important than its concentration in bile. A
broadspectrum antibiotic effective against Gram-negative aerobes is most
appropriate (e.g. cefazolin, cefuroxime or gentamicin).
4- Subsequent management. When the temperature, pulse and other physical
signs show that the inflammation is subsiding, oral fluids are reinstated
followed by regular diet.
Ultrasonography is performed to ensure
o no local complications have developed
o the bile duct is of a normal size and
o no stones are contained in the bile duct.
Cholecystectomy may be performed on the next available list, or the patient
may be allowed home to return later when the inflammation has completely
resolved.
Conservative treatment must be abandoned if the pain and tenderness
increase; depending on the status of the patient, operative intervention and
cholecystectomy should be performed
If the patient has serious comorbid conditions, a percutaneous
cholecystostomy can be performed under ultrasound control, which will
rapidly relieve symptoms.
A subsequent cholecystectomy is usually required
Routine early operation
some surgeons advocate urgent operation as a routine measure in cases of
acute cholecystitis. Provided that :
The operation is undertaken within 5–7 days of the onset of the attack,
the surgeon is experienced and excellent operating facilities are available,
BUT conversion rate in laparoscopic cholecystectomy is five times higher in
acute than in elective surgery.

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
12
If an early operation is not indicated, one should wait approximately 6
weeks for the inflammation to subside before proceeding to
operate.(INTERVAL CHOLECYSTECTOMY)
EMPYEMA OF THE GALL BLADDER
The gall bladder filled with pus.
it may be a sequel of acute cholecystitis or the result of a mucocele
becoming infected.
The treatment is drainage and, later, cholecystectomy.
Acalculous cholecystitis
o Acute and chronic inflammation of the gall bladder can occur in the absence
of stones and give rise to a clinical picture similar to calculous cholecystitis.
o Acute acalculous cholecystitis is seen particularly in
o patients recovering from major surgery (e.g. coronary artery bypass),
o trauma and burns.
o In these patients, the diagnosis is often missed, and the mortality rate is
high.
CHOLECYSTECTOMY
Preparation for operation
o Full blood count
o Renal profile and liver function tests
o Prothrombin time
o Chest X-ray and electrocardiogram (if over 45 years or medically indicated)
o Antibiotic prophylaxis
o Deep vein thrombosis prophylaxis
o Informed consent

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
13
Laparoscopic cholecystectomy
o Serious complications of laparoscopic cholecystectomy fall into two major
areas:
access complications
bile duct injuries.
If either a visceral or a bile duct injury is suspected, conversion to an open
technique isrecommended by most surgeons.
Open cholecystectomy
For patients in whom a laparoscopic approach is not indicated or in whom
conversion from a laparoscopic approach is required, an open
cholecystectomy is performed.
Golden rules in case of difficulty
When the anatomy of the triangle of Calot is unclear, blind dissection
should stop.
Bleeding adjacent to the triangle of Calot should be controlled by pressure
and not by blind clipping or clamping.
When there is doubt about the anatomy, a ‘fundus-first’ or ‘retrograde’
cholecystectomy dissecting on the gall bladder wall down to the cystic duct
can be helpful.
If the cystic duct is densely adherent to the common bile duct and there is the
possibility of a Mirizzi syndrome (a gallstone ulcerating through into the
common duct), the infundibulum of the gall bladder should be opened, the
stone removed and the infundibulum oversewn.
A cholecystostomy is rarely indicated but, if necessary,
stones should be extracted, and a large Foley catheter (14F) placed in the
fundus of the gall bladder with a direct track externally.

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
14
By so doing, should stones be left behind in the gallbladder, these can be
extracted with a choledochoscope.
Indications for choledochotomy
o In a situation in which sophisticated preoperative imaging or peroperative
cholangiography is not available,
o the traditional indications for choledochotomy, which are:
1- palpable stones in the common bile duct;
2- jaundice, a history of jaundice or cholangitis;
3- a dilated common bile duct;
4- abnormal liver function tests, in particular a raised alkaline phosphatase.
Late symptoms after cholecystectomy
o In 15% of patients, cholecystectomy fails to relieve the symptoms for which
the operation was performed. ‘post-cholecystectomy’ syndrome.
o problems are usually related to the preoperative symptoms and are
continuation of those symptoms. Full investigation should be undertaken to
confirm the diagnosis
o presence of a stone in the common bile duct,
o a stone in the cystic duct stump
o or operative damage to the biliary tree.
o best DIAGNOSED by
MRCP or ERCP.
o The latter has the added advantage that, if a stone is found in the common
bile duct, it can be removed.
Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
15
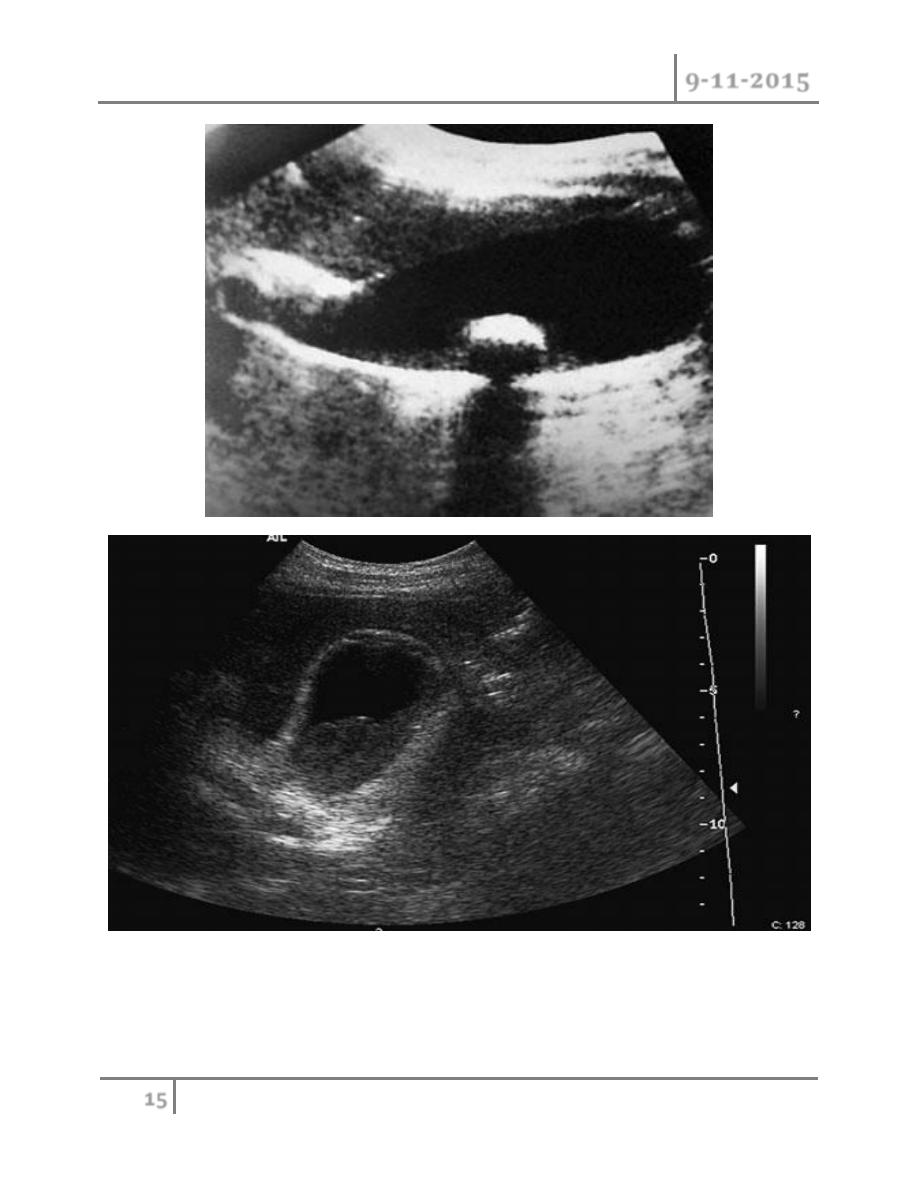
Cholecystitis. Ultrasound demonstrates pericholecystic fluid (thin arrow), gall
bladder wall (thick arrow) and biliary sludge
Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
16
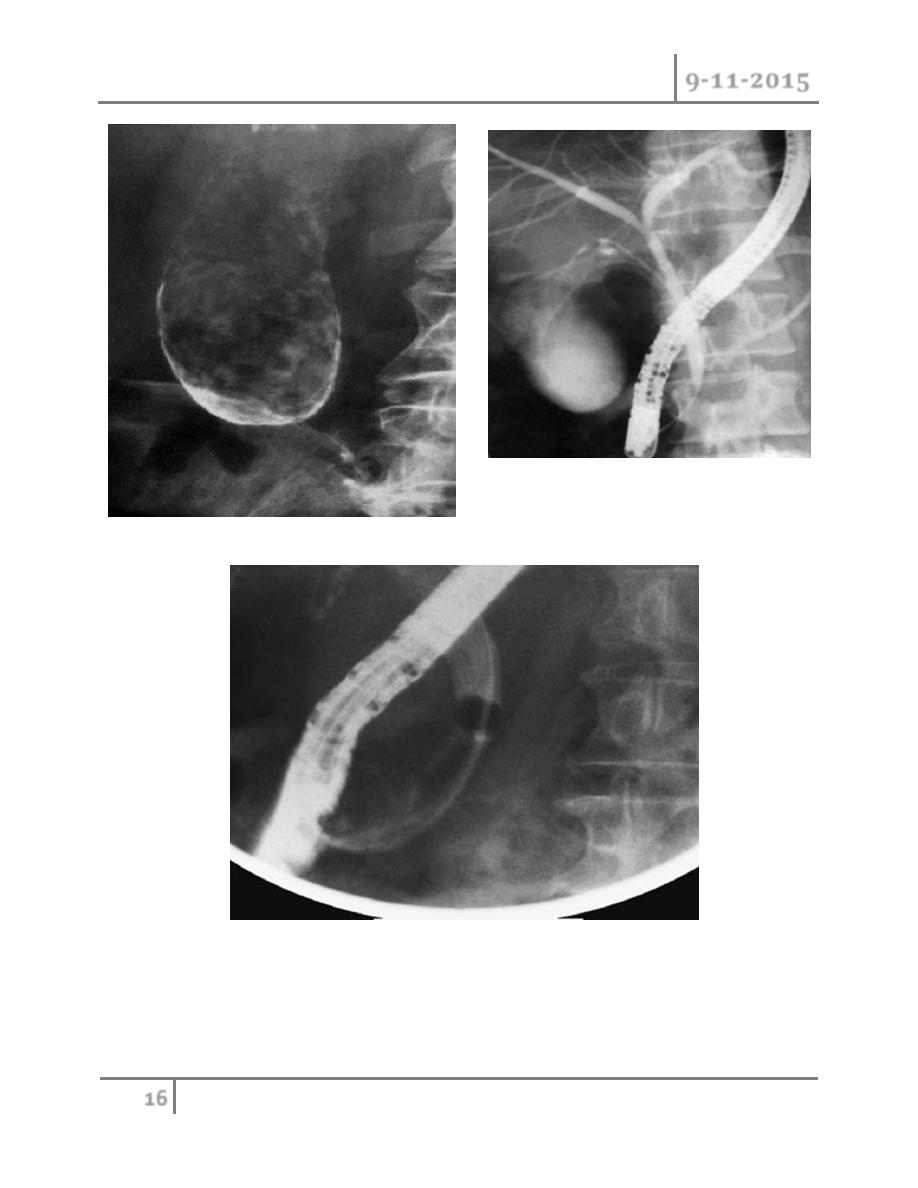
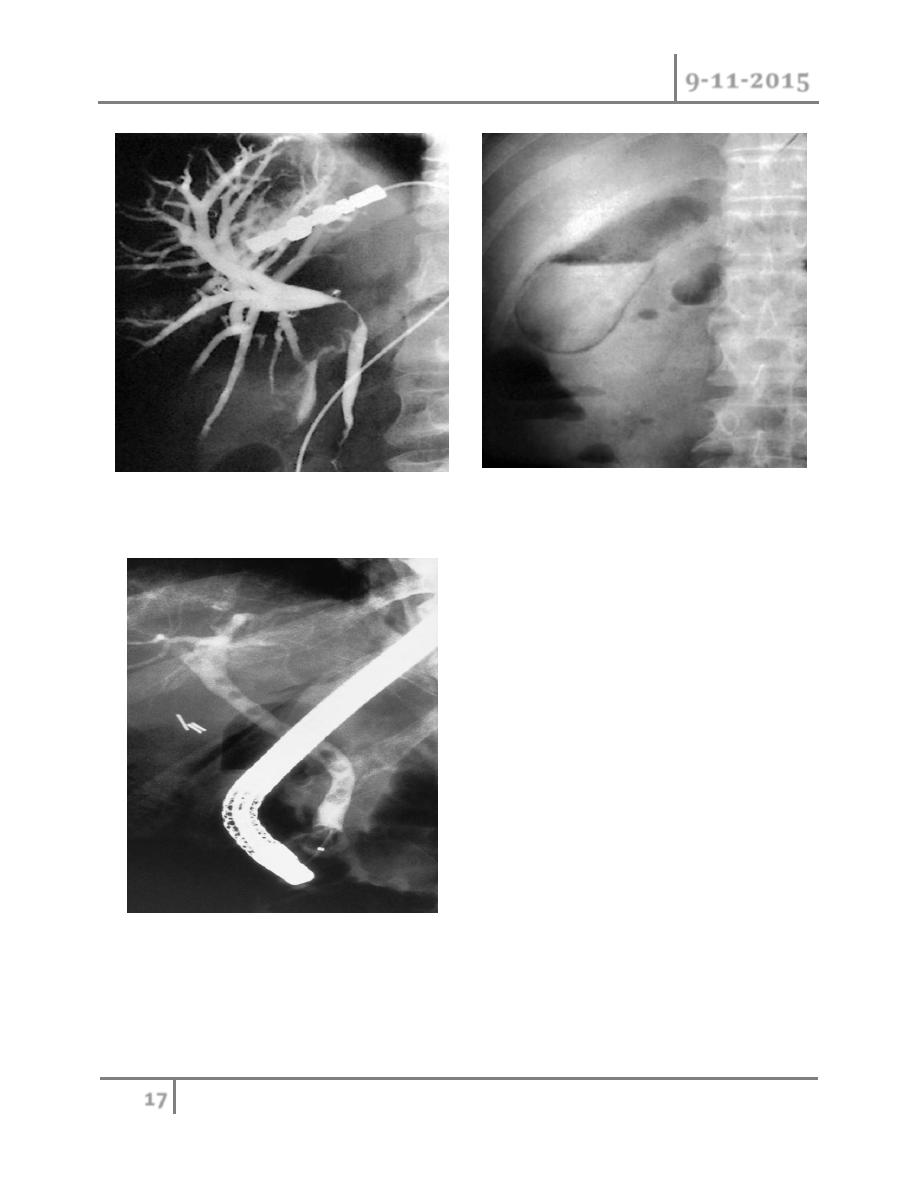
NORMAL ERCP
Endoscopic retrograde cholangiopancreatography
demonstrating stone obstructing the common bile duct (arrow
Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
17
Transhepatic cholangiogram showing a stricture
of the common hepatic duct
Gas in the gall bladder and gall bladder wall
(Clostridium perfringens). Emergency surgery is
indicated.
Endoscopic retrograde
cholangiopancreatography: the
patient presented with jaundice 4 days after
laparoscopic cholecystectomy.
The bile duct contained multiple stones

Gall bladder & Biliary tree Dr. Muayad Abbas
9-11-2015
18
END…
Done by
Ali Kareem
