Dr. Salim Al- Rubaiee
Lec. 7
GONADS – PART 1
Wed. 13 / 4 / 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Gonads – Part 1 Dr. Salim Al- Rubaiee
13-4-2015
1
Gonads – part 1
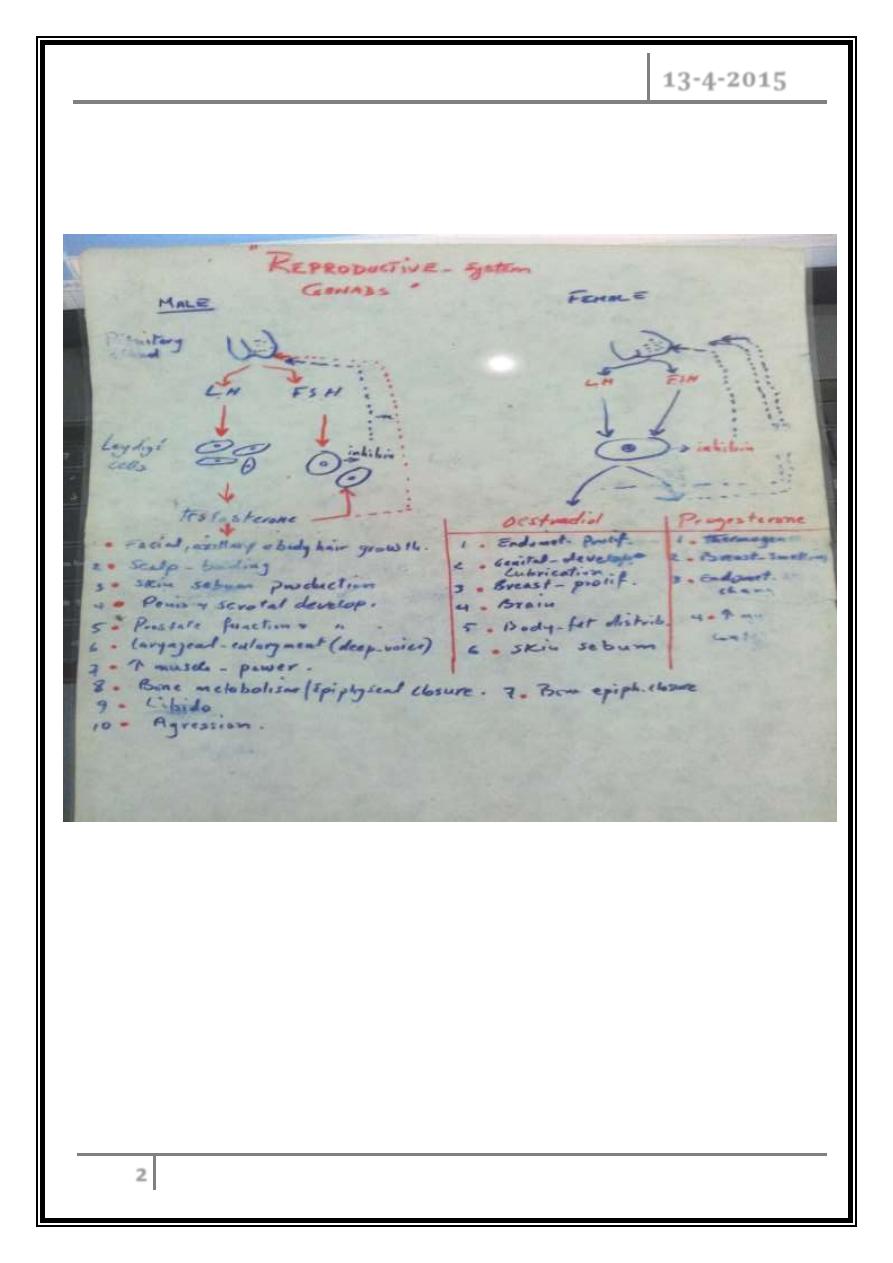
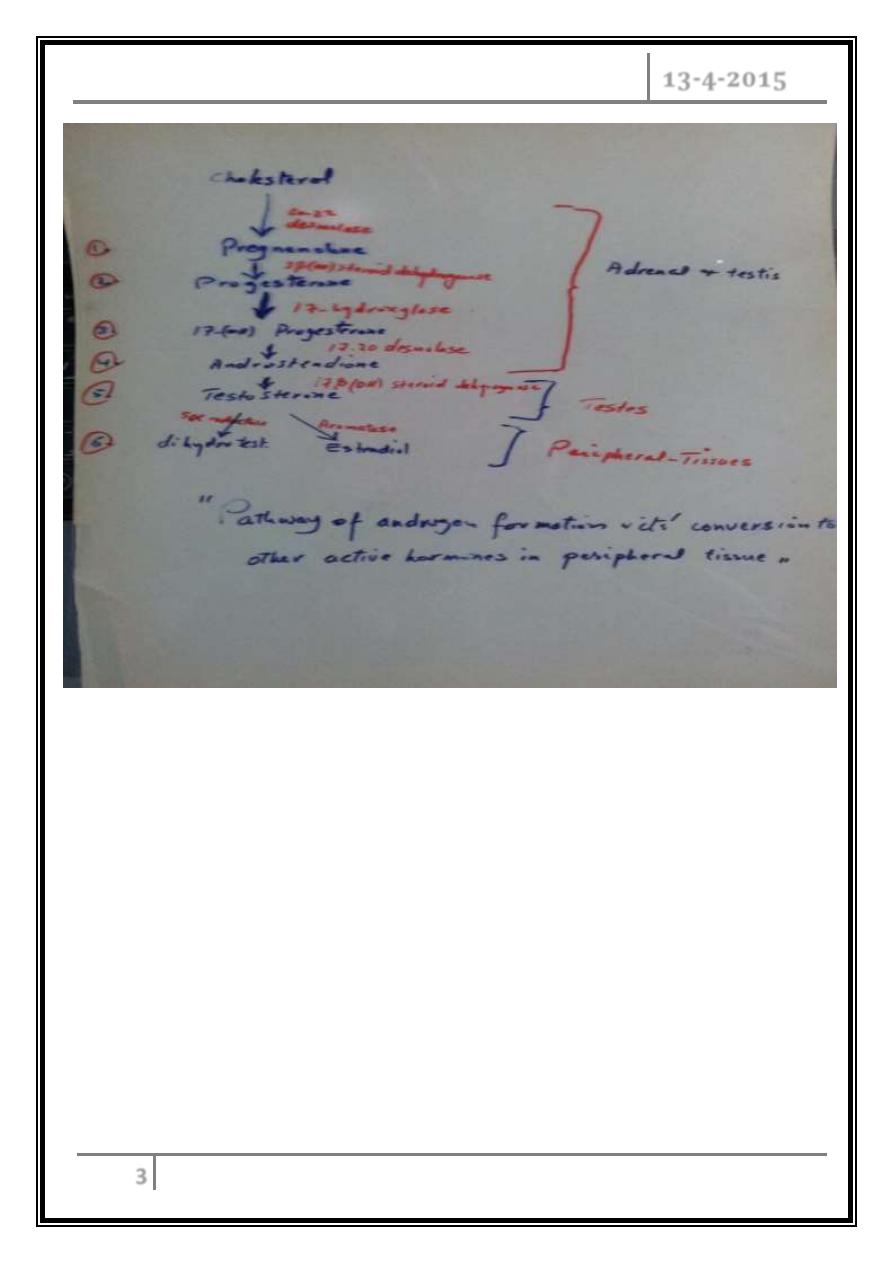
Male’s gonads
Human life is an active male androgenic activity interacting with female
estrogenic activity producing fertilized ovum leading to genotypic and
phenotypic criteria in their off springs
Male androgenic and female estrogenic act. are at risk for variety of pathologic
disorders.
Assessments of testicular functions
Hx & C/F then investigations:
Hormonal essay: testesterone, prolactin, LH/FSH, and gonadotrophic hormone.
Urine 17-ketosteroids.
Seminal fluid analysis: volume, sperm count, liquefaction, morphology, activity,
any pus cells or RBC.
Gonadotropin stimulation test and response (HCG injection 2000 IU I.M. per 4
days then check testosterone level one day before the initial dose and after the
4
th
dose).
Testicular biopsy ( rarely indicated )
Hypogonadism
Primary
Idiopathic.
Autoimmune (Schmidts 2 )
Chemical – alcoholism
Infection: viral (mumps-orchitis), TB, brucellosis & pyogenic.
Infiltrative: LL, lymphoma, seminomas, haemochromatosis.
Traumatic.
Genetic: Klinefelter’s disease (XXY), myotonia–congenita.
Systemic illness: liver cirrhosis, sickle disease.
Drugs: narcotics, spironolactone.
Gonads – Part 1 Dr. Salim Al- Rubaiee
13-4-2015
2
Secondary
Sheehan’s syndrome.
Kalmann’s syndrome.
Gonads – Part 1 Dr. Salim Al- Rubaiee
13-4-2015
3
Impotence
A. With decrease libido:
- Hypogonadism.
- Depression.
B. With normal libido: psychological (anxiety)
- Ischemic (atheroma).
- Neuropathic (DM, alcohol, D.S).
- Drugs (β-blockers, thiazides).
Gonads – Part 1 Dr. Salim Al- Rubaiee
13-4-2015
4
Workup of such cases includes:
Hx.
C/E (local and systemic).
Investigation:
1. FBS.
2. HbA1C.
3. Hormone (testosterone, LH-FSH & prolactin).
4. In Cushing’s syndrome: Dex. supp. test.
5. Further rare investigations:
- Nocturnal tumescence- monitoring.
- Intracavernosal inj. of papaverine / PGE1 to test the adequacy of blood
supply.
- Int. pudendal art. angiography.
- Tests for autonomic N.S functions.
- Tests for P.N conduction.
Treatment
1. Treat the cause when possible.
2. Supportive:
a. Sildenafil (Viagra 50,100 mg) - it is a phosphodiesterase inhibitor
(cardiac, IHD & arrhythmias)
b. Self-administerted intracavernosal or urethral PGE1.
c. Prosthetic-implants (fixed-rod, inflatable-reservoir - availability ???,
Cost ???)
Gonads – Part 1 Dr. Salim Al- Rubaiee
13-4-2015
5
Hirsutism
A. Without virilization:
1. Idiopathic (familial).
2. PCOS (hypertension, obesity, primary amenorrhea, cyst by ultrasound &
infertility)
- LH.
- FSH.
- LH/FSH = 2.5: 1.
- 20% testosterone & prolactin.
B. With virilization:
1. Exogenous androgen abuse.
2. Adrenal tumor, C.A.H.
3. Overian tumors (arrhenoblastomas, ovarian rest tumor)
Rapid onst
Investigated by:
o Abdominal CT scan.
o Hormonal study (high androgens but not supp. by dex. or estrogen), and low
LH-FSH.
Rx of the cause
Gynecomastia
Gynecomastia is enlargement of the gland tissue of the male breast. During
infancy, puberty, and in middle-aged to older men, gynecomastia can be common.
Gynecomastia must be distinguished from pseudogynecomastia, which refers to
the presence of fat deposits in the breast area of obese men. True gynecomastia results
from growth of the glandular, or breast tissue, which is present in very small amounts
in men.
Gonads – Part 1 Dr. Salim Al- Rubaiee
13-4-2015
6
What causes gynecomastia?
Gynecomastia results from an imbalance in hormone levels in which levels of
estrogen (female hormones) are increased relative to levels of androgens
(male hormones). Gynecomastia that occurs in normally-growing infant and
pubertal boys that resolves on its own with time is known as physiologic
gynecomastia.
All individuals, whether male or female, possess both female hormones
(estrogens) and male hormones (androgens). During puberty, levels of these
hormones may fluctuate and rise at different levels, resulting in a temporary
state in which estrogen concentration is relatively high. Studies regarding the
prevalence of gynecomastia in normal adolescents have yielded widely
varying results, with prevalence estimates as low as 4% and as high as 69%
of adolescent boys. These differences probably result from variations in what
is perceived to be normal and the different ages of boys examined in the
studies.
Gynecomastia caused by transient changes in hormone levels with growth
usually disappears on its own within six months to two years. Occasionally,
gynecomastia that develops in puberty persists beyond two years and is
referred to as persistent pubertal gynecomastia.
A number of conditions that cause gynecomastia includes:
Malnutrition and re-feeding (recovery from malnutrition) have both been
shown to create a hormonal environment that may lead to gynecomastia.
Similarly, cirrhosis of the liver alters normal hormone metabolism and may
lead to gynecomastia.
Gonads – Part 1 Dr. Salim Al- Rubaiee
13-4-2015
7
Disorders of the male sex organs (testes) can result in decreased testosterone
production and relatively high estrogen levels, leading to gynecomastia.
These disorders may be genetic, such as Klinefelter's syndrome, or acquired
due to trauma, infection, reduced blood flow, or aging. Testicular cancers
may also secrete hormones that cause gynecomastia.
Other conditions that are associated with an altered hormonal environment in
the body and may be associated with gynecomastia are chronic renal failure
and hyperthyroidism. Rarely, cancers other than testicular tumors may
produce hormones that can cause gynecomastia.
A number of drugs that cause gynecomastia includes:
Spironolactone: a diuretic that has anti-androgenic activity.
Calcium channel blockers, used to treat hypertension (such as nifedipine).
ACE inhibitor drugs for hypertension (captopril, enalapril).
Some antibiotics (for example, isoniazid, ketoconazole , and metronidazole)
Anti-ulcer drugs (such as ranitidine, cimetidine, and omeprazole).
Anti-androgen or estrogen therapies for prostate cancer.
Methyldopa.
Highly active anti-retroviral therapy (HAART) for HIV disease, which may
cause fat redistribution leading to pseudogynecomastia or, in some cases,
true gynecomastia.
Digitoxin.
Diazepam.
Drugs of abuse (for example, alcohol, marijuana, and heroin) and lavender
oil and tea tree oil, when used in skin-care products, have been associated
with gynecomastia.
Gonads – Part 1 Dr. Salim Al- Rubaiee
13-4-2015
8
What are the risk factors for gynecomastia?
Normally-developing pubertal males may be at risk for gynecomastia that is
part of the normal developmental process. Other risk factors include aging, since
aging may promote decreases in testosterone production that can cause
gynecomastia. The risk factors for developing gynecomastia related to specific
diseases and conditions (such as cirrhosis of the liver) are the same risk factors that
predispose to those conditions. Taking certain medications (see above) may
increase the risk of developing gynecomastia.
What are the symptoms of gynecomastia?
The primary symptom of gynecomastia is enlargement of the male breasts. As
mentioned before, gynecomastia is the enlargement of glandular tissue rather
than fatty tissue. It is typically symmetrical in location with regard to the
nipple and may have a rubbery or firm feel. Gynecomastia usually occurs on
both sides but can be unilateral in some cases. The enlargement may be
greater on one side even if both sides are involved. Tenderness and sensitivity
may be present, although there is typically no severe pain.
The most important distinction with gynecomastia is differentiation from male
breast cancer, which accounts for about 1% of overall cases of breast cancer.
Cancer is usually confined to one side, is not necessarily centered around the
nipple, feels hard or firm, and can be associated with dimpling of the skin,
retraction of the nipple, nipple discharge, and enlargement of the underarm
(axillary) lymph nodes.
Gonads – Part 1 Dr. Salim Al- Rubaiee
13-4-2015
9
How is gynecomastia diagnosed?
The definition of gynecomastia is the presence of breast tissue greater than
0.5 cm in diameter in a male. As previously discussed, gynecomastia is the
presence of true breast (glandular) tissue, generally located around the
nipple. Fat deposition is not considered to be true gynecomastia.
In most cases, gynecomastia can be diagnosed by a physical examination. A
careful medical history is also important, including medication and drug use.
If there is a suspicion of cancer, a mammogram may be ordered by a health
care practitioner. Further tests may be recommended to help establish the
cause of gynecomastia in certain cases. These can include blood tests to
examine liver, kidney, and thyroid function. Measurement of hormone levels
in the bloodstream may also be recommended in some cases.
What is the treatment for gynecomastia?
Gynecomastia, especially in pubertal males, often goes away on its own
within about six months, so observation is preferred over specific treatment in
many cases. Stopping any offending medications and treatment of underlying
medical conditions that cause gynecomastia are also mainstays of treatment.
Treatments are also available to specifically address the problem of
gynecomastia, but data on their effectiveness are limited, and no drugs have
yet been approved by the U.S. Food and Drug Administration (FDA) for
treatment of gynecomastia. Medications are more effective in reducing
gynecomastia in the early stages, since scarring often occurs after about 12
months. After the tissue has become scarred, medications are not likely to be
effective, and surgical removal is the only possible treatment.
Gonads – Part 1 Dr. Salim Al- Rubaiee
13-4-2015
10
Medications that have been used to treat gynecomastia
include:
o Testosterone replacement has been effective in older men with low levels of
testosterone, but it is not effective for me who have normal levels of the male
hormone.
o The selective estrogen receptor modulators (SERMs) tamoxifen and
raloxifene have been shown to reduce breast volume in gynecomastia,
although they are not able to entirely eliminate all the breast tissue. This type
of therapy is most often used for severe or painful gynecomastia.
o Aromatase inhibitors [such as anastrozole ] are a class of medication that
interferes with the synthesis of estrogen. While these drugs theoretically
should be able to reduce breast mass in gynecomastia, studies have failed to
show a significant benefit in treating gynecomastia.
What are the complications of gynecomastia?
Although pubertal gynecomastia typically regresses on its own, in rare cases
it may persist, requiring treatment. Gynecomastia that is present over the
long term (12 months or more) may undergo scarring (medically termed
fibrosis), making treatment with medications much more difficult if not
impossible to achieve a response.
Psychological consequences can occur if the breast enlargement is
pronounced or is a source of embarrassment.
Can gynecomastia be prevented?
Gynecomastia that occurs because of hormonal fluctuations with growth or
aging cannot be prevented. Gynecomastia related to medical conditions can only be
prevented to the extent that the underlying or responsible condition can be
prevented.
Gonads – Part 1 Dr. Salim Al- Rubaiee
13-4-2015
11
What is the outlook for gynecomastia?
Many cases of gynecomastia resolve without treatment, and medical
treatment is effective in reducing gynecomastia in many cases. For severe
cases or cases in which the breast tissue has become scarred, surgical
techniques can help restore normal appearance. Typically, gynecomastia is
not associated with long-term problems.
Men with gynecomastia have about a five-fold greater risk for developing
male breast cancer when compared with the general population. It is believed
that the gynecomastia itself is not a precancerous condition, but rather that
the hormonal changes (relative increase in estrogens, lower levels of
androgens) that produce gynecomastia in adult men also increase their risk
of developing breast cancer.
To be continued …
