Dr. Rabah
Lec. 8
HEPATIC DISEASES
Wed. 6 / 4/ 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Hepatic diseases Dr. Rabah
6-4-2016
1
Hepatic diseases
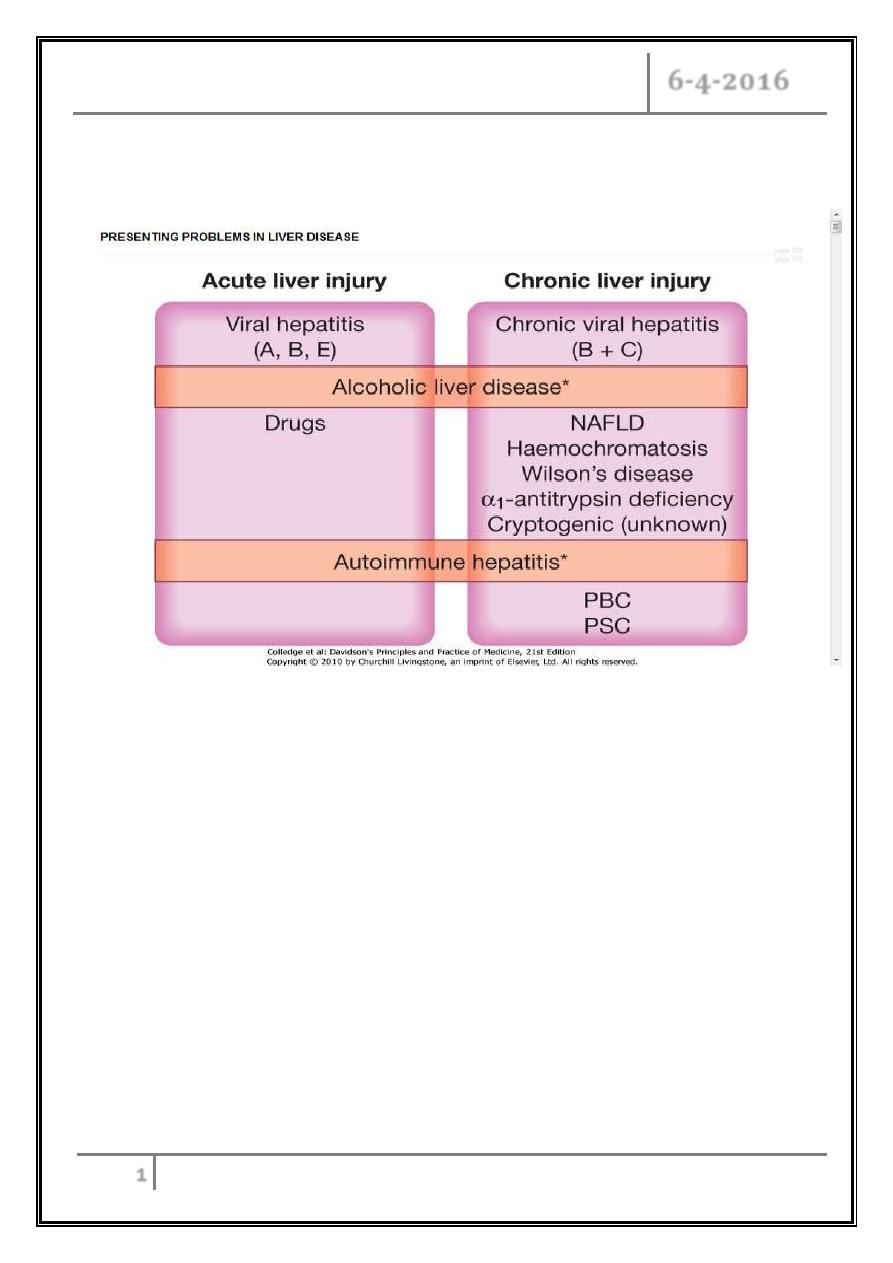
Hepatic injury
May be either:
Acute liver injury which may present with non-specific symptoms of fatigue and
abnormal LFTs, or with jaundice and acute liver failure.
Chronic liver injury which is defined as hepatic injury, inflammation and/ or
fibrosis occurring in the liver for more than 6 months. In the early stages
patients can be asymptomatic with abnormal LFTs. With more severe liver
damage, however, the presentation can be with jaundice, portal hypertension or
other signs of cirrhosis.
Hepatic diseases Dr. Rabah
6-4-2016
2
Severity Acute liver injury Chronic liver injury
Mild/ moderate Abnormal LFTs Abnormal LFTs
Severe Jaundice Cirrhosis ± portal hypertension
Very severe Acute liver failure Chronic liver failure
Jaundice
Ascites
Hepatic encephalopathy
Portal hypertension + variceal bleeding
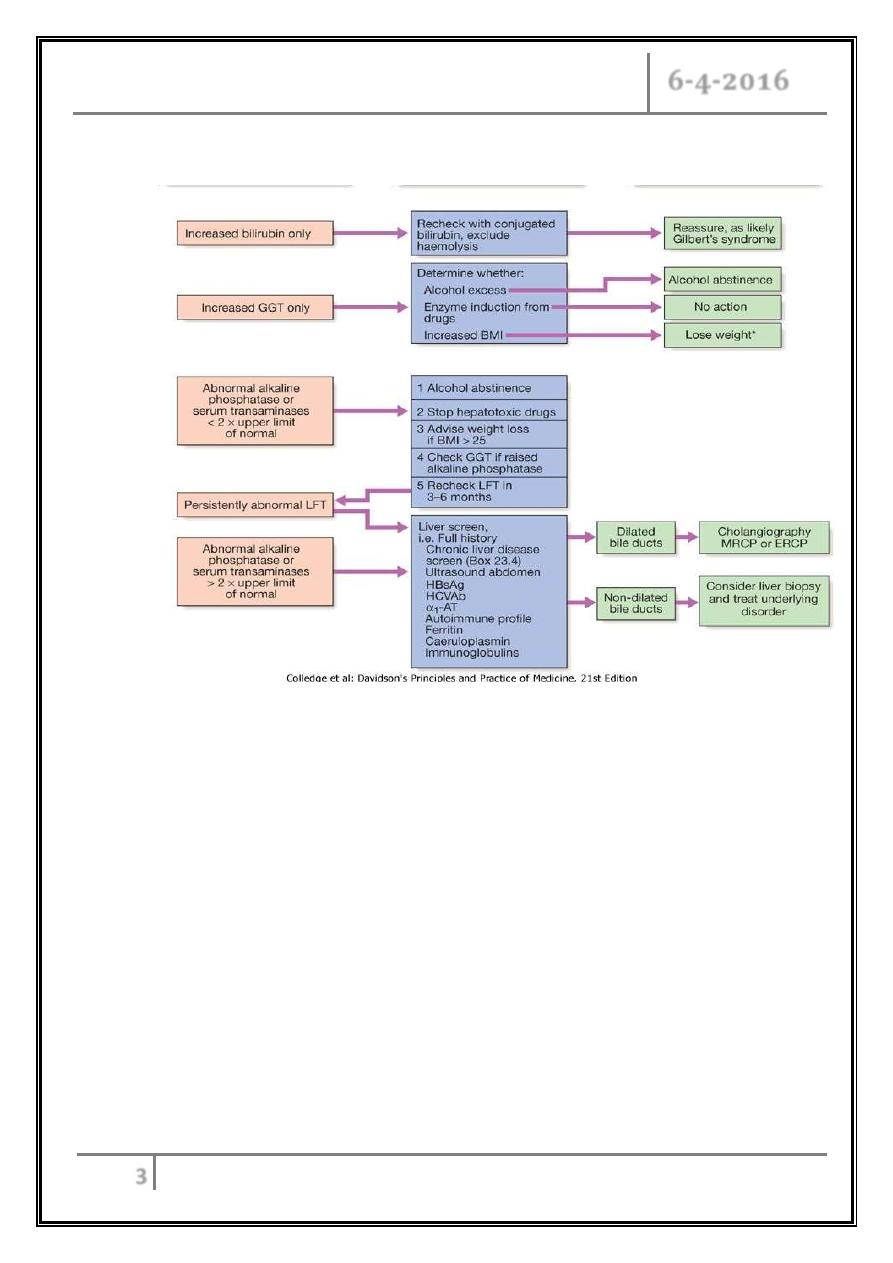
Abnormal liver function tests
Common causes of elevated serum transaminases
Minor elevation (< 100 U/ L):
- Chronic hepatitis B and C.
- Haemochromatosis.
- Fatty liver disease.
Moderate elevation (100-300 U/ L): As above plus:
- Alcoholic hepatitis.
- Non-alcoholic steatohepatitis.
- Autoimmune hepatitis.
- Wilson's disease.
Major elevation (> 300 U/ L):
- Drugs (e.g. paracetamol).
- Acute viral hepatitis.
- Autoimmune liver disease.
- Ischaemic liver.
- Toxins (e.g. Amanita phalloides poisoning).
- Flare of chronic hepatitis B.
Hepatic diseases Dr. Rabah
6-4-2016
3
Management of abnormal liver function test
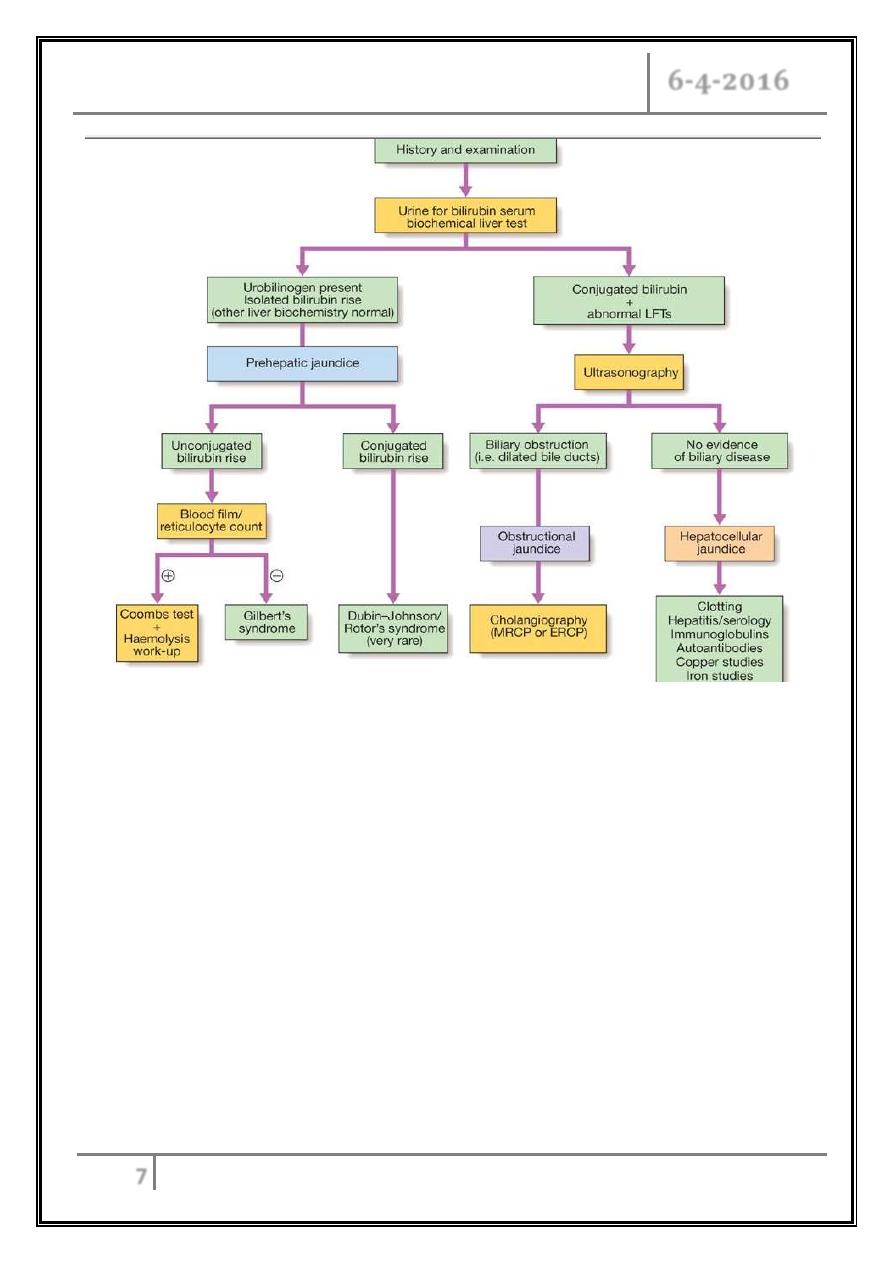
Jaundice
Jaundice is usually detectable clinically when the plasma bilirubin exceeds 50
μmol/ L (
∼
3 mg/ dL).
The causes of jaundice overlap with the causes of abnormal LFTs.
In a patient with jaundice it is useful to consider whether the cause might be
pre-hepatic, hepatic, or post-hepatic.
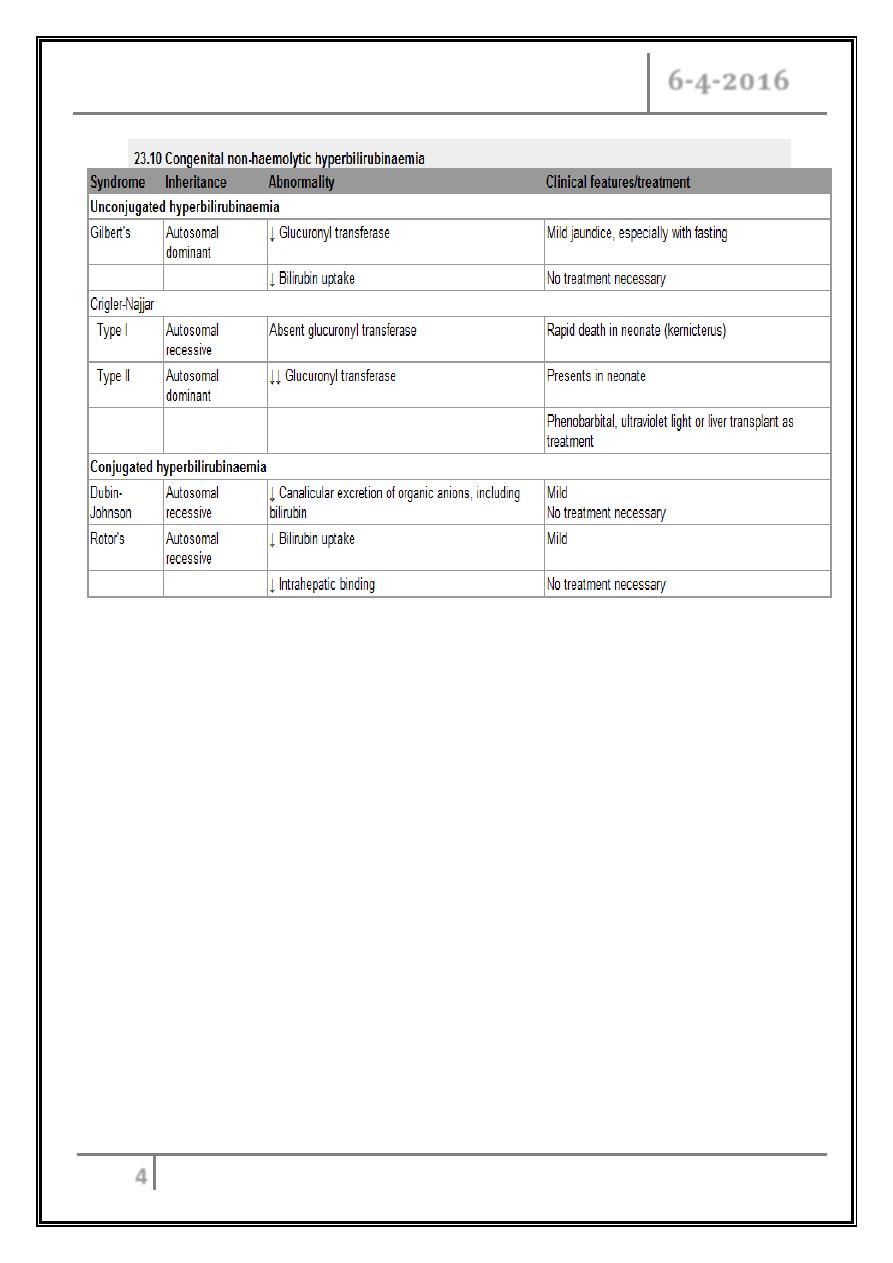
Pre-hepatic jaundice
Characterised by an isolated raised bilirubin.
Haemolysis.
Congenital hyperbilirubinaemia.
The most common form of non-haemolytic hyperbilirubinaemia is Gilbert's
syndrome, an inherited disorder of bilirubin metabolism.
Hepatic diseases Dr. Rabah
6-4-2016
4
Obstructive (cholestatic)
Obstructive (cholestatic) jaundice may be caused by:
- Intrahepatic cholestasis: failure of hepatocytes to initiate bile flow.
- Extrahepatic obstruction of bile flow in the bile ducts.
Ultrasound evaluation is indicated in all cases to determine whether there is
evidence of mechanical obstruction and dilatation of the biliary tree.
Management of cholestatic jaundice depends on the underlying cause of the
cholestasis and is discussed in detail in the relevant sections below.
Hepatic diseases Dr. Rabah
6-4-2016
5
Causes of cholestatic jaundice
o Intrahepatic
- Primary biliary cirrhosis.
- Primary sclerosing cholangitis.
- Alcohol.
- Drugs.
- Cystic fibrosis.
- Severe bacterial infections.
- Hepatic infiltrations (lymphoma, granuloma, amyloid, metastases).
- Pregnancy.
- Inherited cholestatic liver disease, e.g. benign recurrent intrahepatic
cholestasis.
- Chronic right heart failure.
o Extrahepatic
- Carcinoma.
Ampullary.
Pancreatic.
Bile duct (cholangiocarcinoma).
Liver metastases.
- Choledocholithiasis.
- Parasitic infection.
- Traumatic biliary strictures.
- Chronic pancreatitis.
Hepatic diseases Dr. Rabah
6-4-2016
6
Clinical features and complications of cholestatic jaundice
Early features
- Jaundice.
- Dark urine.
- Pale stools.
- Pruritus.
Late features
- Malabsorption (vitamins A, D, E and K).
Weight loss.
Steatorrhoea.
Osteomalacia.
Bleeding tendency.
- Xanthelasma and xanthomas.
Cholangitis
- Fever.
- Rigors.
- Pain (if gallstones are present).
Hepatocellular jaundice
Hepatocellular jaundice results from an inability of the liver to transport
bilirubin across the hepatocyte into the bile, occurring as a consequence of
parenchymal liver disease.
Both unconjugated and conjugated bilirubin in the blood increase.
Hepatocellular jaundice can be due to acute or chronic liver injury (features
of acute or chronic liver disease may be detected clinically).
Increases in transaminases (AST, ALT), but increases in other LFTs,
including cholestatic enzymes (GGT, ALP) may occur due edema of the
inflammation.
Hepatic diseases Dr. Rabah
6-4-2016
7
Acute liver failure
Acute liver failure is an uncommon but serious syndrome.
The presentation is with mental changes progressing from confusion to stupor
and coma, and a rapidly progressive deterioration in liver function within 8
weeks of onset of the precipitating illness, in the absence of evidence of pre-
existing liver disease.
Pathophysiology:
- Cerebral edema.
- Portosystemic shunt of toxins.
Hepatic diseases Dr. Rabah
6-4-2016
8
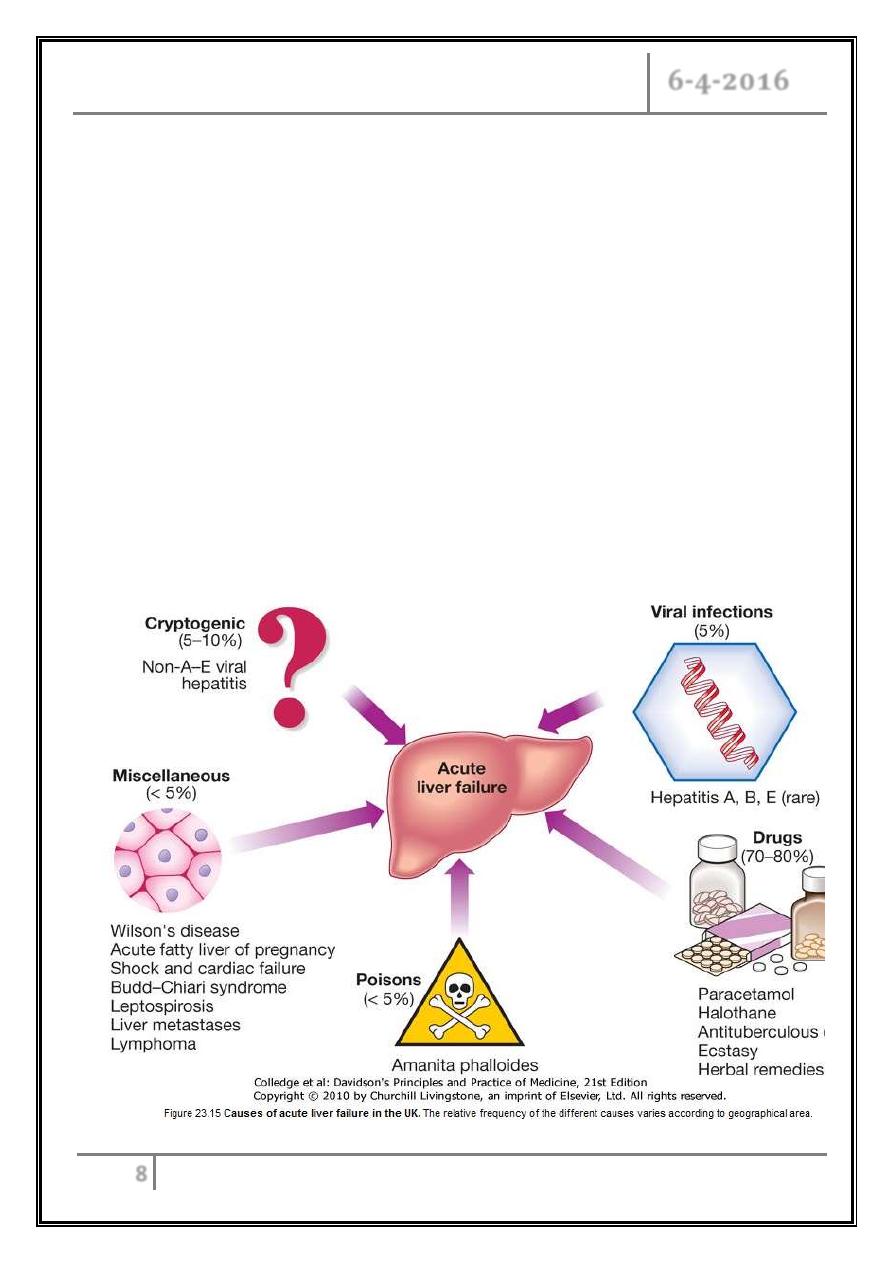
Causes
Any cause of liver damage can produce acute liver failure, provided it is
sufficiently severe.
Acute viral hepatitis is the most common cause world-wide.
Paracetamol toxicity is the most frequent cause.
Acute liver failure occurs occasionally with other drugs as anti TB.
Toxins as Amanita phalloides (mushroom) poisoning.
Pregnancy.
Wilson's disease.
Shock.
Extensive malignant disease of the liver.
In 10% of cases the cause of acute liver failure remains unknown.
Hepatic diseases Dr. Rabah
6-4-2016
9
Clinical features
Cerebral disturbance (hepatic encephalopathy) is the cardinal manifestation
of acute liver failure.
In the early stages this can be mild and episodic.
The initial clinical features are often subtle and include reduced alertness
and poor concentration, progressing through behavioural abnormalities such
as restlessness and aggressive outbursts, to drowsiness and coma.
Cerebral oedema may occur due to increased intracranial pressure causing
unequal or abnormally reacting pupils, fixed pupils, hypertensive episodes,
bradycardia, hyperventilation, profuse sweating, local or general myoclonus,
focal fits or decerebrate posturing.
Papilloedema occurs rarely and is a late sign.
General symptoms include weakness, nausea and vomiting.
Right hypochondrial discomfort is an occasional feature.
The patient is usually jaundiced.
Occasionally, death may occur in fulminant cases of acute liver failure before
jaundice develops.
Fetor hepaticus can be present.
The liver is usually of normal size but later becomes smaller.
Hepatomegaly is unusual and, in the presence of a sudden onset of ascites,
suggests venous outflow obstruction as the cause (Budd-Chiari syndrome).
Splenomegaly is uncommon and never prominent.
Ascites and oedema are late developments.
Hepatic diseases Dr. Rabah
6-4-2016
10
Hepatic encephalopathy clinically grade:
- Grade 1 - Poor concentration, slurred speech, slow mentation, disordered
sleep rhythm.
- Grade 2 - Drowsy but easily rousable, occasional aggressive behaviour,
lethargic.
- Grade 3 - Marked confusion, drowsy, sleepy but responds to pain and
voice, gross disorientation.
- Grade 4 - Unresponsive to voice, may or may not respond to painful
stimuli, unconscious.
Investigations
The prothrombin time rapidly becomes prolonged as coagulation factor
synthesis fails; this is the laboratory test of greatest prognostic value and
should be carried out.
Increased plasma bilirubin reflects the degree of jaundice.
Increased plasma aminotransferase and is not helpful in determining
prognosis.
Plasma albumin remains normal unless the course is prolonged.
Percutaneous liver biopsy is contraindicated because of the severe
coagulopathy.
Investigations to determine the cause of acute liver failure
- Toxicology screen of blood and urine.
- HBsAg, IgM anti-HBc.
- IgM anti-HAV.
- Anti-HEV, HCV, cytomegalovirus, herpes simplex, Epstein-Barr virus.
- Ceruloplasmin, serum copper, urinary copper, slit-lamp eye examination.
- Autoantibodies: ANF, ASMA, LKM.
- Immunoglobulins.
- Ultrasound of liver and Doppler of hepatic veins.
Hepatic diseases Dr. Rabah
6-4-2016
11
Prognosis
o Prothrombin time > 100 seconds,
or
o Any three of the following:
- Jaundice to encephalopathy time > 7 days.
- Age < 10 or > 40 years.
- Indeterminate or drug-induced causes.
- Bilirubin > 300 μmol/ L (
≅
17.6 mg/ dL).
- Prothrombin time > 50 seconds.
or
o Encephalopathy grade 3 or 4.
Management
Should be treated in intensive care unit.
Conservative treatment aims to maintain life in the hope that hepatic
regeneration will occur.
Nutrition I.V. glucose 300 g.
Decrease IC pressure by mannitol.
Bowel steralization by neomyscine or metronidazole.
Lactulose laxative.
Infection treatment.
Regular electrolyte check.
Specific treatment.
N-acetylcysteine therapy may improve outcome, particularly in patients with
acute liver failure due to paracetamol poisoning.
Liver transplantation is an increasingly important treatment option for acute
liver failure.
Hepatic diseases Dr. Rabah
6-4-2016
12
Complications of acute liver failure
Encephalopathy and cerebral oedema.
Hypoglycaemia.
Metabolic acidosis.
Infection (bacterial, fungal).
Renal failure.
Multi-organ failure (hypotension and respiratory failure).
Monitoring in acute liver failure
Neurological
- Intracranial pressure monitoring.
- Conscious level.
Cardiorespiratory
- Pulse.
- Blood pressure.
- Central venous pressure.
- Respiratory rate.
Fluid balance
- Hourly output (urine, vomiting, diarrhoea).
- Input: oral, intravenous.
Blood analyses
- Arterial blood gases.
- Peripheral blood count (including platelets).
- Sodium, potassium, HCO
3-
, calcium, magnesium.
- Creatinine, urea.
- Glucose (2-hourly in acute phase).
- Prothrombin time.
Hepatic diseases Dr. Rabah
6-4-2016
13
Infection surveillance
- Cultures: blood, urine, throat, sputum, cannula sites.
- Chest X-ray.
- Temperature.
… End …
