Hepatic diseases
Hepatic diseasesHepatic injury
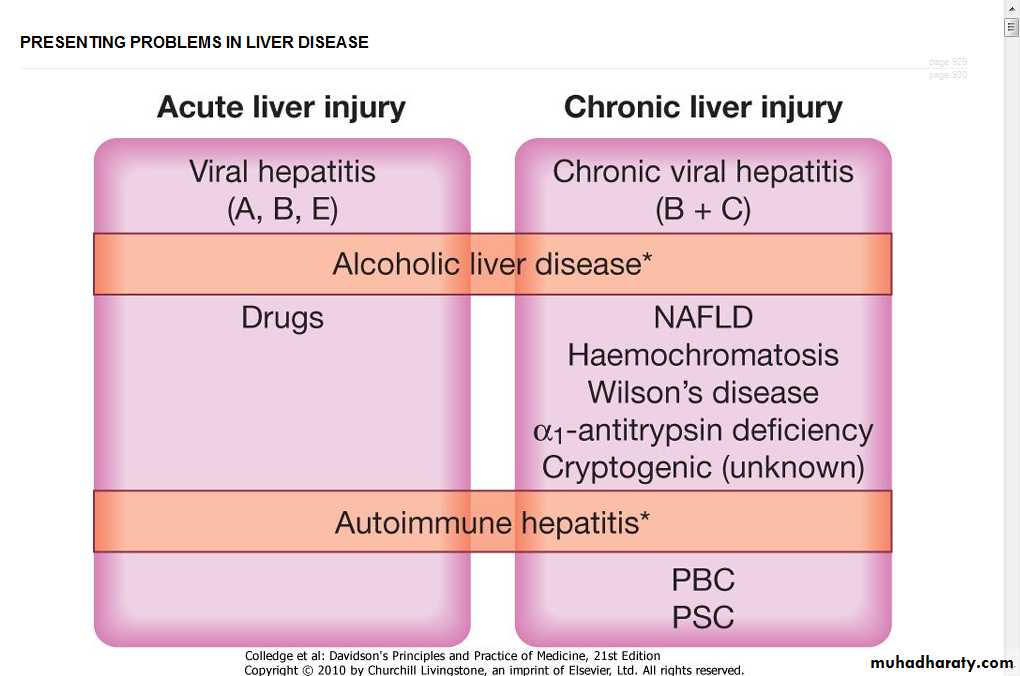
may be eitherAcute liver injury may present with non-specific symptoms of fatigue and abnormal LFTs, or with jaundice and acute liver failure.
Chronic liver injury is defined as hepatic injury, inflammation and/or fibrosis occurring in the liver for more than 6 months. In the early stages patients can be asymptomatic with abnormal LFTs. With more severe liver damage, however, the presentation can be with jaundice, portal hypertension or other signs of cirrhosis
Hepatic injury
Severity Acute liver injury Chronic liver injuryMild/moderate Abnormal LFTs Abnormal LFTs
Severe Jaundice cirrhosis ± portal hypertension
Very severe Acute liver failure Chronic liver failure
Jaundice
Ascites
Hepatic encephalopathy
Portal hypertension+ variceal bleeding
Abnormal liver function tests Common causes of elevated serum transaminases
Minor elevation (< 100 U/L)
Chronic hepatitis B and CHaemochromatosis
Fatty liver disease
Moderate elevation (100-300 U/L) As above plus:
Alcoholic hepatitis
Non-alcoholic steatohepatitis
Autoimmune hepatitis
Wilson's disease
Major elevation (> 300 U/L)
Drugs (e.g. paracetamol)
Acute viral hepatitis
Autoimmune liver disease
Ischaemic liver
Toxins (e.g. Amanita phalloides poisoning)
Flare of chronic hepatitis B
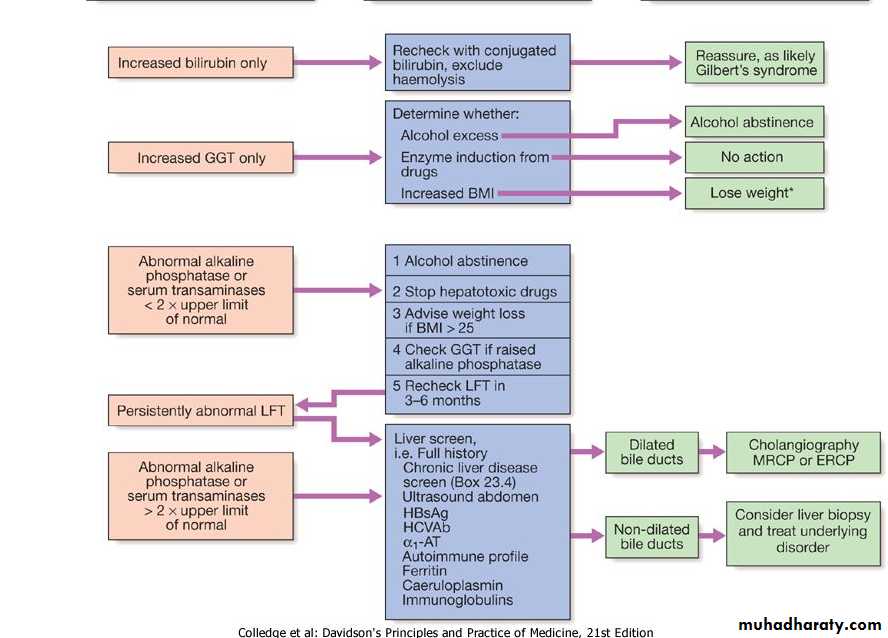
Management of abnormal liver function test
Jaundice
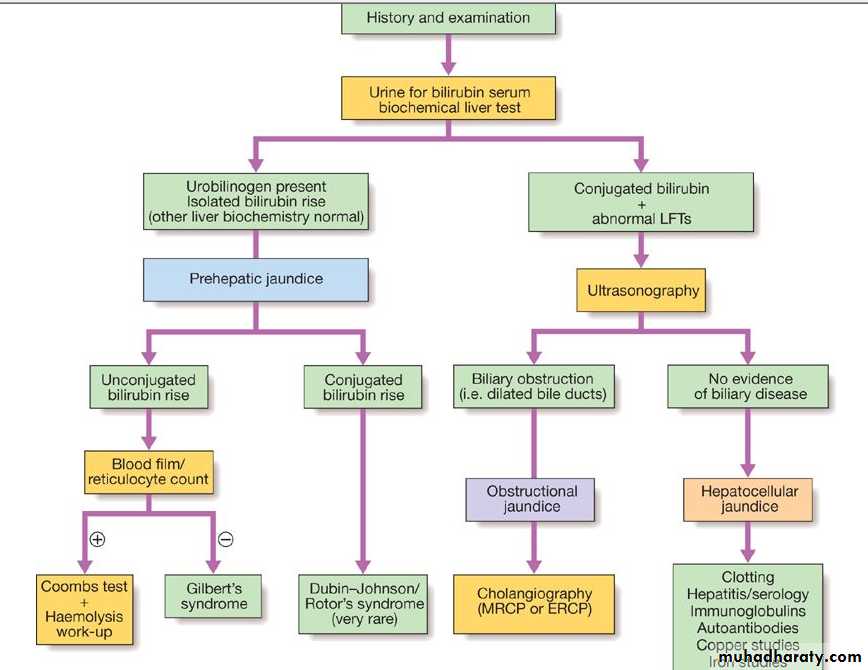
Jaundice is usually detectable clinically when the plasma bilirubin exceeds 50 μmol/L (∼3 mg/dL).The causes of jaundice overlap with the causes of abnormal LFTs
In a patient with jaundice it is useful to consider whether the cause might be pre-hepatic, hepatic or post-hepatic
Pre-hepatic jaundice
characterised by an isolated raised bilirubinhaemolysis
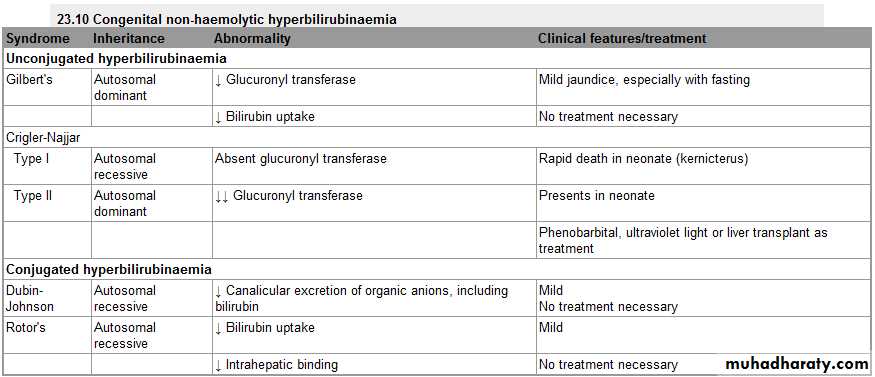
congenital hyperbilirubinaemia,
The most common form of non-haemolytic hyperbilirubinaemia is Gilbert's syndrome, an inherited disorder of bilirubin metabolism
Obstructive (cholestatic)
Obstructive (cholestatic) jaundice may be caused by:intrahepatic cholestasis : failure of hepatocytes to initiate bile flow
Extrahepatic obstruction of bile flow in the bile ducts
Ultrasound evaluation is indicated in all cases to determine whether there is evidence of mechanical obstruction and dilatation of the biliary tree
Management of cholestatic jaundice depends on the underlying cause of the cholestasis and is discussed in detail in the relevant sections below.
Causes of cholestatic jaundice
Intrahepatic
Primary biliary cirrhosis
Primary sclerosing cholangitis
Alcohol
Drugs
Cystic fibrosis
Severe bacterial infections
Hepatic infiltrations (lymphoma, granuloma, amyloid, metastases)
Pregnancy
Inherited cholestatic liver disease, e.g. benign recurrent intrahepatic cholestasis
Chronic right heart failure
Extrahepatic
CarcinomaAmpullary
Pancreatic
Bile duct (cholangiocarcinoma)
Liver metastases
Choledocholithiasis
Parasitic infection
Traumatic biliary strictures
Chronic pancreatitis
Clinical features and complications of cholestatic jaundice
Early features
Jaundice
Dark urine
Pale stools
Pruritus
Late features
Malabsorption (vitamins A, D, E and K)
Weight loss
Steatorrhoea
Osteomalacia
Bleeding tendency
Xanthelasma and xanthomas
Cholangitis
Fever
Rigors
Pain (if gallstones are present)
Hepatocellular jaundice
Hepatocellular jaundice results from an inability of the liver to transport bilirubin across the hepatocyte into the bile, occurring as a consequence of parenchymal liver disease.both unconjugated and conjugated bilirubin in the blood increase.
Hepatocellular jaundice can be due to acute or chronic liver injury (features of acute or chronic liver disease may be detected clinically).
increases in transaminases (AST, ALT), but increases in other LFTs, including cholestatic enzymes (GGT, ALP) may occur due edema of the inflammation
Acute liver failure
Acute liver failure is an uncommon but serious syndrome.The presentation is with mental changes progressing from confusion to stupor and coma, and a rapidly progressive deterioration in liver function within 8 weeks of onset of the precipitating illness, in the absence of evidence of pre-existing liver disease
Pathophysiology
Cerebral edema
Portosystemic shunt of toxins
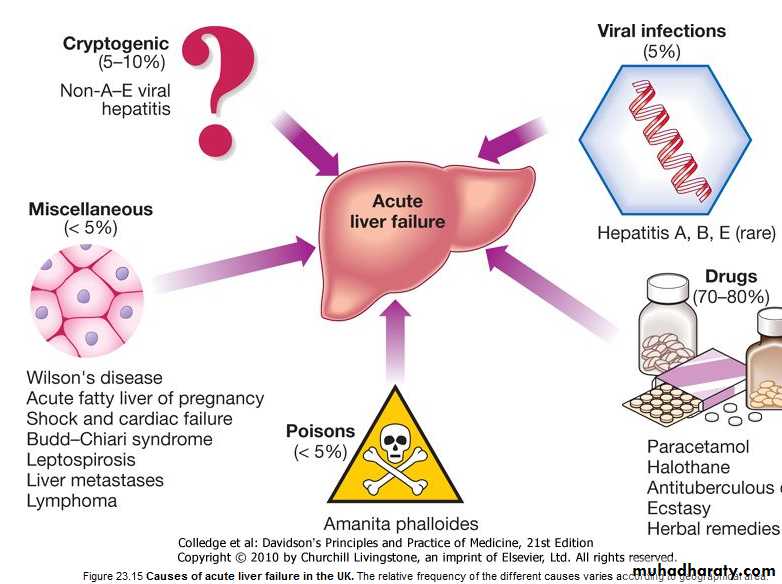
causes
Any cause of liver damage can produce acute liver failure, provided it is sufficiently severe.Acute viral hepatitis is the most common cause world-wide,
paracetamol toxicity is the most frequent cause.
Acute liver failure occurs occasionally with other drugs as anti TB
toxins as Amanita phalloides (mushroom) poisoning
pregnancy
Wilson's disease
shock
extensive malignant disease of the liver.
In 10% of cases the cause of acute liver failure remains unknown
Clinical features
Cerebral disturbance (hepatic encephalopathy) is the cardinal manifestation of acute liver failure,in the early stages this can be mild and episodic.
The initial clinical features are often subtle and include reduced alertness and poor concentration, progressing through behavioural abnormalities such as restlessness and aggressive outbursts, to drowsiness and coma .
Cerebral oedema may occur due to increased intracranial pressure causing unequal or abnormally reacting pupils, fixed pupils, hypertensive episodes, bradycardia, hyperventilation, profuse sweating, local or general myoclonus, focal fits or decerebrate posturing.
Papilloedema occurs rarely and is a late sign.
general symptoms include weakness, nausea and vomiting.
Right hypochondrial discomfort is an occasional feature.
Clinical features
The patient is usually jaundiced.Occasionally, death may occur in fulminant cases of acute liver failure before jaundice develops.
Fetor hepaticus can be present.
The liver is usually of normal size but later becomes smaller.
Hepatomegaly is unusual and, in the presence of a sudden onset of ascites, suggests venous outflow obstruction as the cause (Budd-Chiari syndrome).
Splenomegaly is uncommon and never prominent.
Ascites and oedema are late developments
Clinical features
hepatic encephalopathy clinically grade
Grade 1 Poor concentration, slurred speech, slow mentation, disordered sleep rhythm
Grade 2 Drowsy but easily rousable, occasional aggressive behaviour, lethargic
Grade 3 Marked confusion, drowsy, sleepy but responds to pain and voice, gross disorientation
Grade 4 Unresponsive to voice, may or may not respond to painful stimuli, unconscious
Investigations
The prothrombin time rapidly becomes prolonged as coagulation factor synthesis fails; this is the laboratory test of greatest prognostic value and should be carried out.increase plasma bilirubin reflects the degree of jaundice.
Increase Plasma aminotransferase and is not helpful in determining prognosis.
Plasma albumin remains normal unless the course is prolonged.
Percutaneous liver biopsy is contraindicated because of the severe coagulopathy,.
Investigations
Investigations to determine the cause of acute liver failureToxicology screen of blood and urine
HBsAg, IgM anti-HBc
IgM anti-HAV
Anti-HEV, HCV, cytomegalovirus, herpes simplex, Epstein-Barr virus
Ceruloplasmin, serum copper, urinary copper, slit-lamp eye examination
Autoantibodies: ANF, ASMA, LKM
Immunoglobulins
Ultrasound of liver and Doppler of hepatic veins
prognosis
Prothrombin time > 100 secondsor
Any three of the following:
Jaundice to encephalopathy time > 7 days
Age < 10 or > 40 years
Indeterminate or drug-induced causes
Bilirubin > 300 μmol/L (≅ 17.6 mg/dL)
Prothrombin time > 50 seconds
or
encephalopathy grade 3 or 4
Management
should be treated in intensive care unitConservative treatment aims to maintain life in the hope that hepatic regeneration will occur
Nutrition IV glucose 300 g
Decrease IC pressure by manitol
Bowel steralization by neomyscine or metronidazol
Lactulose laxative
Infection treatment
Regular electrolyte check
Specific treatment
N-acetylcysteine therapy may improve outcome, particularly in patients with acute liver failure due to paracetamol poisoning.
Liver transplantation is an increasingly important treatment option for acute liver failure,
Complications of acute liver failure
Encephalopathy and cerebral oedema
Hypoglycaemia
Metabolic acidosis
Infection (bacterial, fungal)
Renal failure
Multi-organ failure (hypotension and respiratory failure)
Monitoring in acute liver failure
NeurologicalIntracranial pressure monitoring
Conscious level
Cardiorespiratory
Pulse
Blood pressure
Central venous pressure
Respiratory rate
Fluid balance
Hourly output (urine, vomiting, diarrhoea)
Input: oral, intravenous
Blood analyses
Arterial blood gases
Peripheral blood count (including platelets)
Sodium, potassium, HCO3-, calcium, magnesium
Creatinine, urea
Glucose (2-hourly in acute phase)
Prothrombin time
Infection surveillance
Cultures: blood, urine, throat, sputum, cannula sites
Chest X-ray
Temperature