Dr. Manal
Lec. 4
ADRENAL INSUFFICIENCY
Wed. 16 / 3 / 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Adrenal insufficiency Dr. Manal
16-3-2016
1
Adrenal insufficiency
Objectives
At the end of this lecture, the student should be able to:
Define adrenal insufficiency.
Recognize the causes of adrenal insufficiency.
Describe clinical presentation of Addison’s disease.
List the investigations and outline the management plan of Addison’s disease.
Describe the clinical features and treatment of adrenal crisis.
CASE SCENARIO
A 32-year-old woman with known hypothyroidism is admitted to hospital. Her
Blood pressure is 86/ 53 mmHg and her pulse 100 bpm. Investigations reveal:
- Serum sodium: 126 mmol/ L (137-144).
- Serum potassium 5.8 mmol/ L (3.5-4.9).
- Serum glucose 3.0 mmol/ L (3.0-6.0).
1- What is the most likely diagnosis?
2- What is the most appropriate investigation to confirm your diagnosis?
Definition
There is a decrease in the secretion of cortisol and/ or aldosterone.
Clinical suspicion is important because the presentation of AI may be insidious
and subtle.
Clinical diagnosis is frequently delayed or missed early
if unrecognized, may
present in a life-threatening crisis with acute cardiovascular collapse (adrenal
crisis).
Prevalence of well-documented, permanent adrenal insufficiency is 5 in 10,000
in the general population.
Adrenal insufficiency Dr. Manal
16-3-2016
2
Classification
Secondary (low ACTH)
Hypothalamic or pituitary disease:
- Chronic glucocorticoid excess (endogenous or exogenous).
- Pituitary tumors (active and inactive adenomas, carcinoma).
- Mass lesions affecting the hypothalamic-pituitary region:
craniopharyngioma, meningioma, metastases.
- Pituitary irradiation.
- Autoimmune hypophysitis.
- Pituitary apoplexy/ hemorrhage.
- Pituitary infiltration and infection (TB, actinomycosis, sarcoidosis,
histiocytosis X, Wegener's granulomatosis, metastases).
Primary adrenal insufficiency (high ACTH) (Addison’s disease)
Autoimmune:
- Isolated autoimmune adrenalitis (30- 40%).
- Polyglandular syndrome 1 &2 (60- 70%).
Infection: TB, HIV, CMV, cryptococcosis, histoplasmosis,
coccidioidomycosis.
AIDS.
Metastases.
Bilateral adrenalectomy.
Rare causes:
Lymphoma.
Adrenal hemorrhage in meningococcal sepsis (Waterhouse-Friderichsen
syndrome).
Amyloidosis, sarcoidosis.
Hemochromatosis.
Adrenal insufficiency Dr. Manal
16-3-2016
3
Imparied steriodiogensis
CAH.
Drugs (Mitotane, aminoglutethimide, etomidate, ketoconazole, suramin.
Addison’s diseAse
First discovered by Thomas Addison in 1855.
First described as an infection of the adrenal gland- most commonly TB.
Now instead of infection, its most commonly characterized by an autoimmune
destruction of the adrenal glands.
Epidemiology
Addison’s disease is a rare and chronic disease.
6-110 cases diagnosed per 100,000 in the world per year.
1.4 million deaths per year around the world.
Usually effects 30-50 year-olds, but can be seen in all ages.
Clinical Features
Signs and symptoms of glucocorticoid deficiency
- Fatigue, lack of energy.
- Anorexia, weight loss.
- Myalgia, joint pain.
- Fever.
- Anemia, lymphocytosis, eosinophilia.
- Slightly increased TSH (due to loss of feedback inhibition of TSH release).
- Hypoglycemia (more frequent in children).
- Low blood pressure, postural hypotension.
- Hyponatremia (due to loss of feedback inhibition of ADH release).
Adrenal insufficiency Dr. Manal
16-3-2016
4
Signs and symptoms caused by mineralocorticoid deficiency (primary AI
only)
- Abdominal pain, nausea, vomiting.
- Dizziness, postural hypotension.
- Salt craving.
- Low blood pressure, postural hypotension.
- Increased serum creatinine (due to volume depletion).
- Hyponatremia.
- Hyperkalemia.
Signs and symptoms caused by adrenal androgen deficiency
- Lack of energy.
- Dry and itchy skin (in women).
- Loss of libido (in women).
- Loss of axillary and pubic hair (in women).
Other signs and symptoms
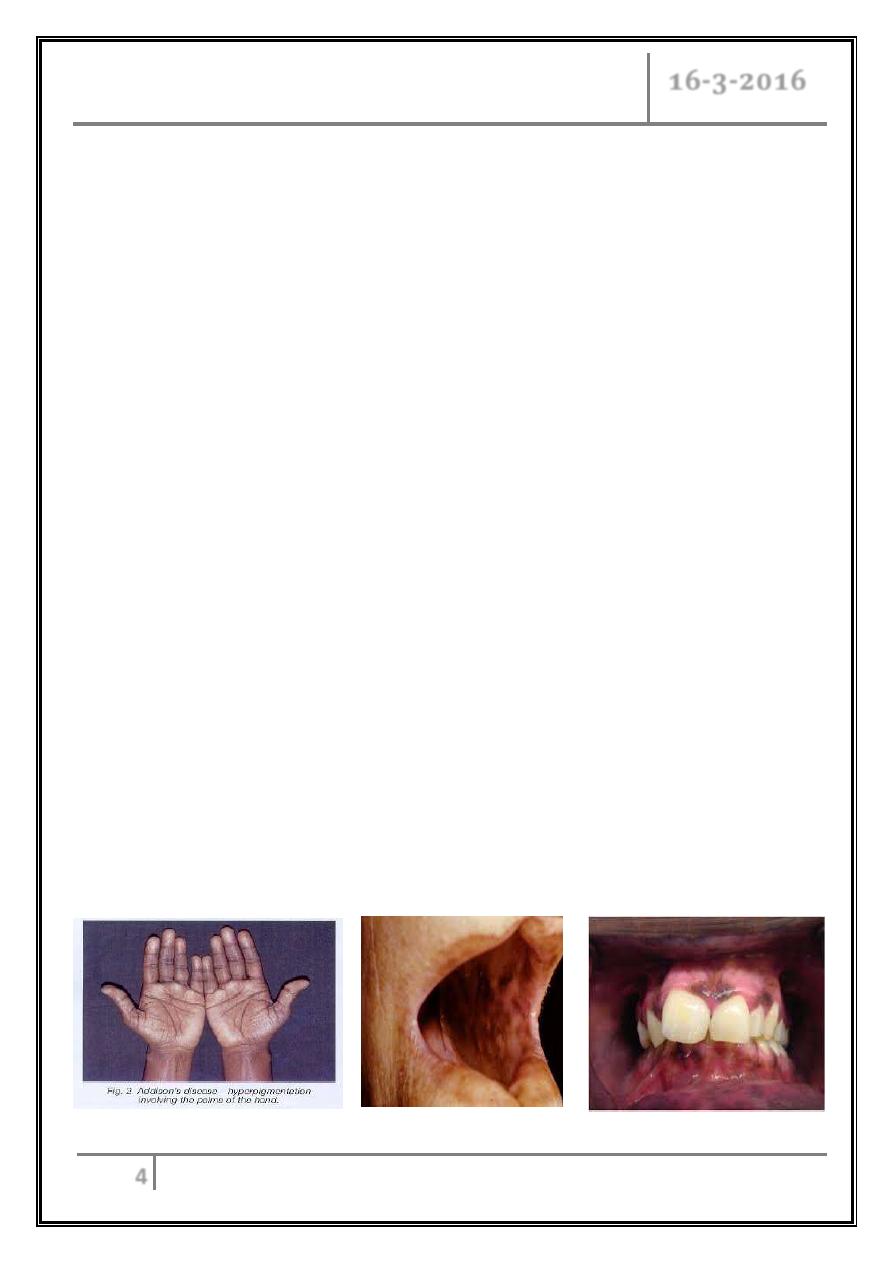
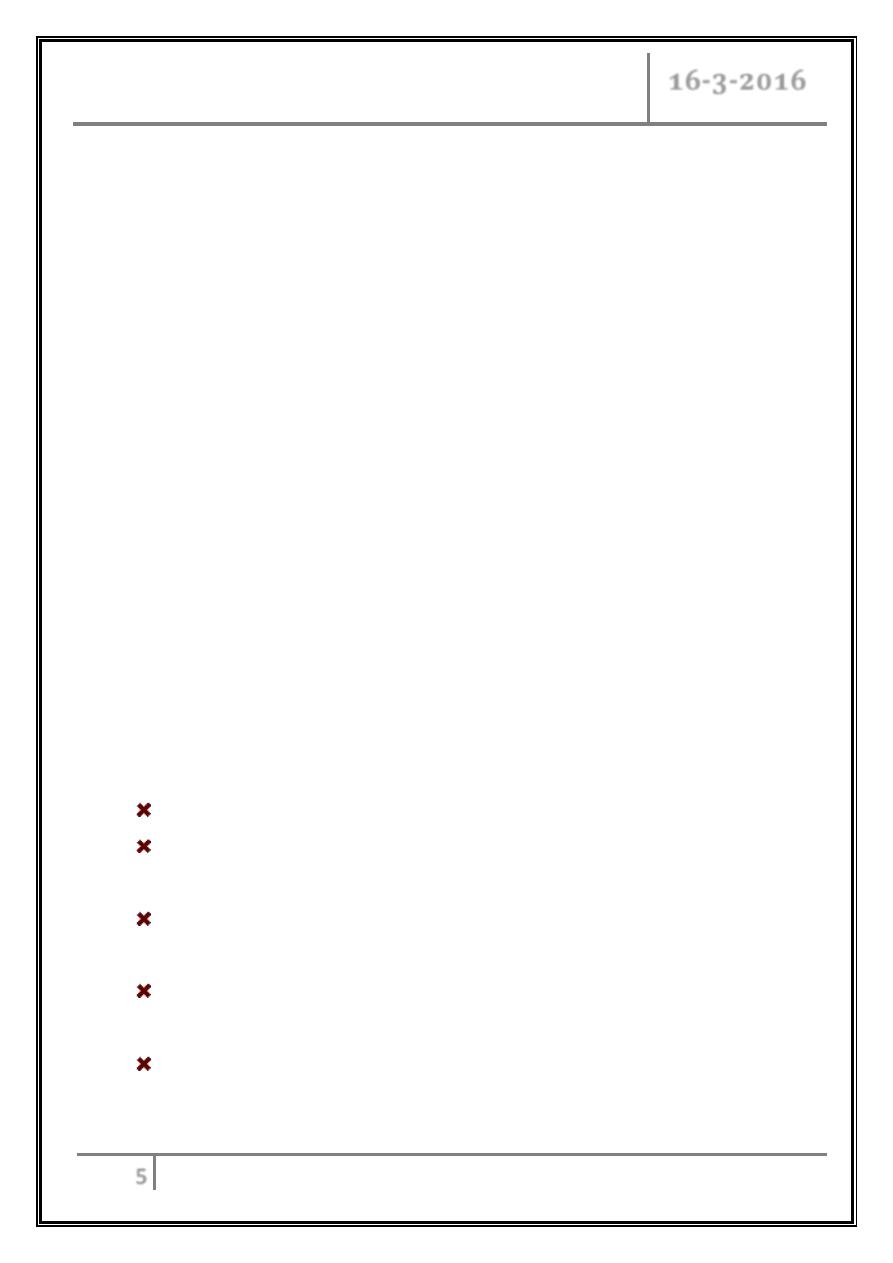
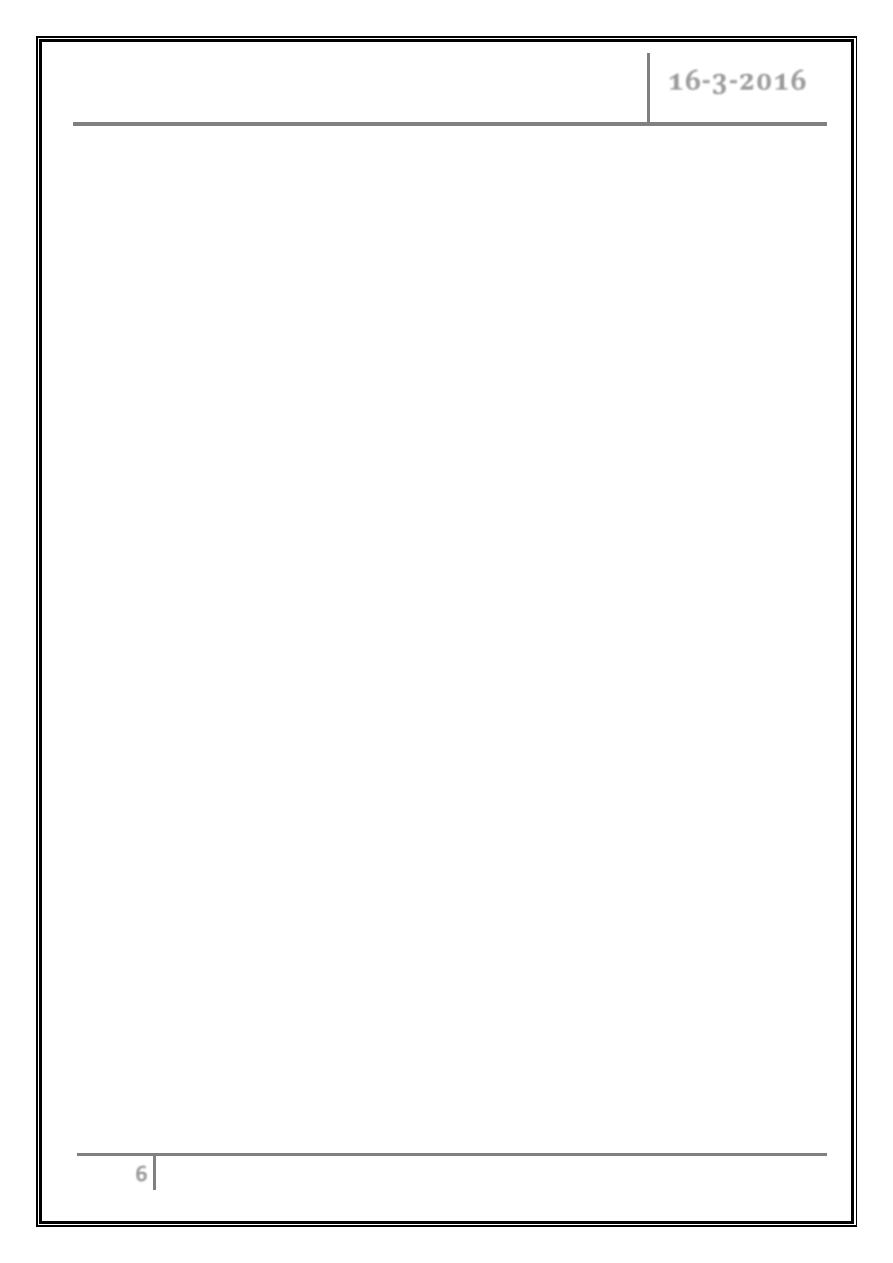
- Hyperpigmentation (primary AI only) [due to excess of pro-
opiomelanocortin (POMC)–derived peptides].
- Alabaster-colored pale skin (secondary AI only) (due to deficiency of
POMC-derived peptides).
Adrenal insufficiency Dr. Manal
16-3-2016
5
Acute adrenal insufficiency
Occurs after a prolonged period of nonspecific complaints.
More frequently observed in patients with primary AI.
Postural hypotension may progress to hypovolemic shock.
Adrenal insufficiency may mimic features of acute abdomen with abdominal
tenderness, nausea, vomiting, and fever.
In some cases, decreased responsiveness, progressing to stupor and coma.
Addisonian Crisis:
o Severely low blood pressure (shock).
o Hyperkalemia.
o Hyponatremia.
o Hypoglycemia.
o Hypercalcemia.
o Unexplained fever, diarrhea, vomiting.
o Coma and death.
o Precipitated by infection, surgery or intercurrent disease.
Management of Addisonian crisis
It is a medical emergency.
I.V. fluid (normal saline 1 L/ h with continuous cardiac monitoring and 10%
dextrose).
Hydrocortisone 100 mg bolus followed by 100–200 mg hydrocortisone over
24 h infusion or I.V. doses until GI symptoms improve then start oral therapy.
Mineralocorticoid replacement can be initiated once the daily hydrocortisone
dose has been reduced to < 50 mg.
Treat precipitating cause.
Adrenal insufficiency Dr. Manal
16-3-2016
6
Diagnosis of AI
Determined by low level of adrenal hormone after stimulation with synthetic
ACTH hormone tetracosactide
Short test:
- 250 micrograms of tetracosactide or cosyntropin (ACTH 1-24), I.M.
or I.V. injection.
- Blood cortisol levels at 0, 30, and 60 min.
- ACTH at 0 min.
- Normal is 500–550 nmol/ L (18–20 µg/ dL) 30–60 minutes after
ACTH stimulation.
For Ddx:
- Plasma ACTH, renin, aldosterone.
- Adrenal autoantibody.
- MRI pituitary.
- CT or MRI of adrenals.
CBC.
Blood Ca and glucose.
Thyroid function test.
CXR.
HIV test.
Serum Na and K.
Adrenal insufficiency Dr. Manal
16-3-2016
7
Insulin tolerance test (ITT):
Administration of regular insulin 0.1 U/ kg I.V. (dose should be lower if
hypopituitarism is likely), and collection of blood samples at 0, 30, 60, and
120 minutes for glucose, cortisol, and growth hormone (GH), if also
assessing the GH axis.
Oral or I.V. glucose is administered after the patient has achieved
symptomatic hypoglycemia (usually glucose < 40 mg/ dL).
A normal response is defined as a cortisol > 20 µg/ dL and GH > 5.1µg/ L.
It is contraindicated in patients with DM, coronary disease, cerebrovascular
disease, or seizure disorders.
Treatment
Replacement ( always need glucocorticoids and usually mineralcorticoid
therapy).
Hydrocortison orally 15 mg at morning and 5 mg at evening.
Doses change according to lifestyle:
- Doubling the routine oral dose in the case of intercurrent illness with fever.
- I.V. hydrocortisone injection at a daily dose of 100 mg in cases of prolonged
vomiting, surgery, or trauma.
Have to carry emergency injection of hydrocortisone and card/bracelet
indentifying their condition.
Mineralocorticoid replacement in primary AI (100–150 g fludrocortisone). The
adequacy of treatment can be evaluated by measuring BP, sitting and standing
to detect a postural drop indicative of hypovolemia, serum Na, k, and plasma
renin should be measured regularly.
Adrenal insufficiency Dr. Manal
16-3-2016
8
Adrenal androgen replacement is an option in patients with lack of energy, and
in women with loss of libido.
- It can be achieved by once-daily administration of 25–50 mg DHEA.
Treatment is monitored by measurement of DHEAS, androstenedione, and
testosterone.
References
Davidson’s Principles of Internal Medicine 20
th
Edition.
Harrison’s Principles of Internal Medicine 18
th
Edition.
… END …
