Dr. Manal
Lec. 3
ADRENAL GLAND
HYPERFUNCTION
Tues. 15 / 3 / 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
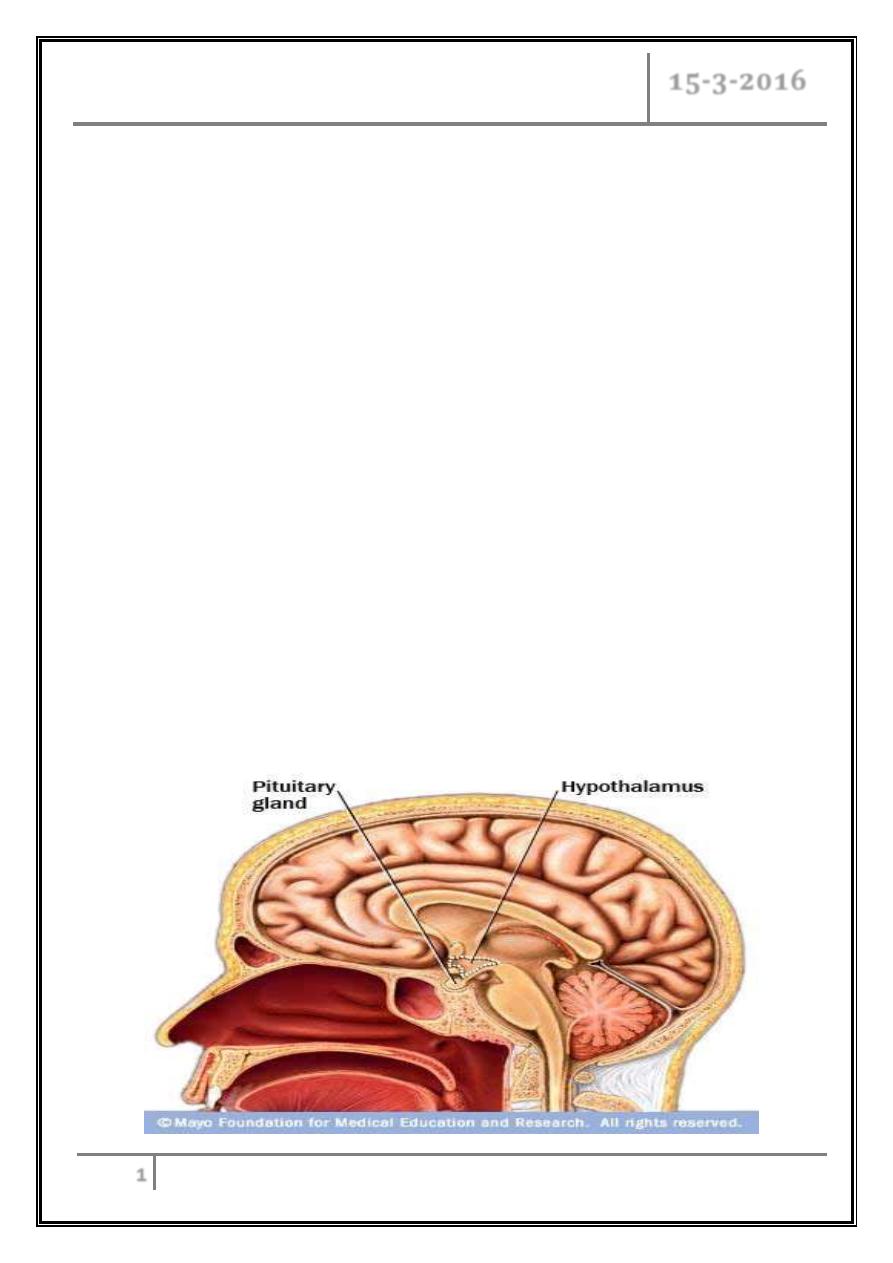
Adrenal gland hyperfunction Dr. Manal
15-3-2016
1
Adrenal gland hyperfunction
Objectives
At the end of this lecture, the student should be able to:
Define Cushing’s syndrome.
Recognize the etiology of Cushing’s syndrome.
Describe the clinical features and complication of Cushing’s disease.
Outline the diagnosis and treatment options.
Classify hyperaldosteronism.
Describe clinical features of Conn’s syndrome.
State diagnosis and treatment.
CASE SCENARIO
A 28 y old unmarried female presented with weight gain, bruising easily,
menstrual irregularity and striae. On examination she is hypertensive. Her blood tests
reveal hypokalemia.
What is the most likely diagnosis?
Adrenal gland hyperfunction Dr. Manal
15-3-2016
2
Cushing’s syndrome
A multisystem disorder resulting from chronic exposure to inappropriately
elevated concentrations of free circulating glucocorticoids.
Incidence of 1–2 per 100,000 population per year.
Causes of Cushing's syndrome
Endogenous
ACTH- dependent Cushing‘s - F/ M (1:1)
- Cushing's disease.
- Ectopic ACTH syndrome (by bronchial or pancreatic carcinoid tumors,
small cell lung cancer, medullary thyroid carcinoma,
pheochromocytoma).
ACTH- independent Cushing‘s - F/ M (4:1)
- Adrenocortical adenoma, adrenocortical CA.
- Rare: primary pigmented nodular adrenal disease, ACTH-independent
massive adrenal hyperplasia.
Exogenous:
- ACTH treatment
- Glucocorticoid treatment
Pseudo-Cushing's syndrome:
Chronic activation of (HPA), usually mild and temporary.
- Major depressive disorder.
- Alcoholism.
- Obesity, PCOS.
- Obstructive sleep apnea.
Adrenal gland hyperfunction Dr. Manal
15-3-2016
3
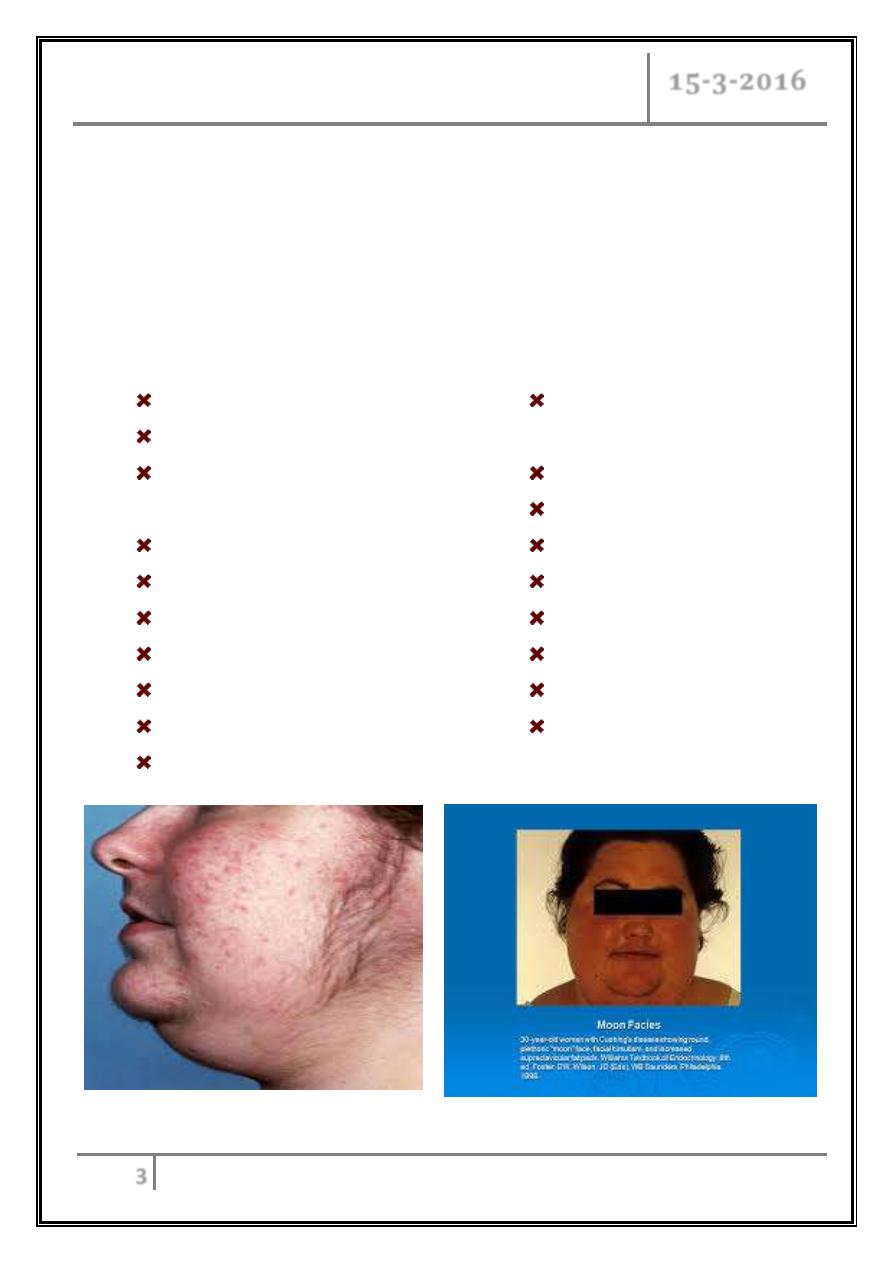
Cushing’s disease
o (ACTH- producing pituitary adenoma).
o Most common cause of Cushing’s syndrome (in 90%).
o F/M (4:1), more in male in pre-puberty cases.
o 3
rd
or 4
th
decade of life.
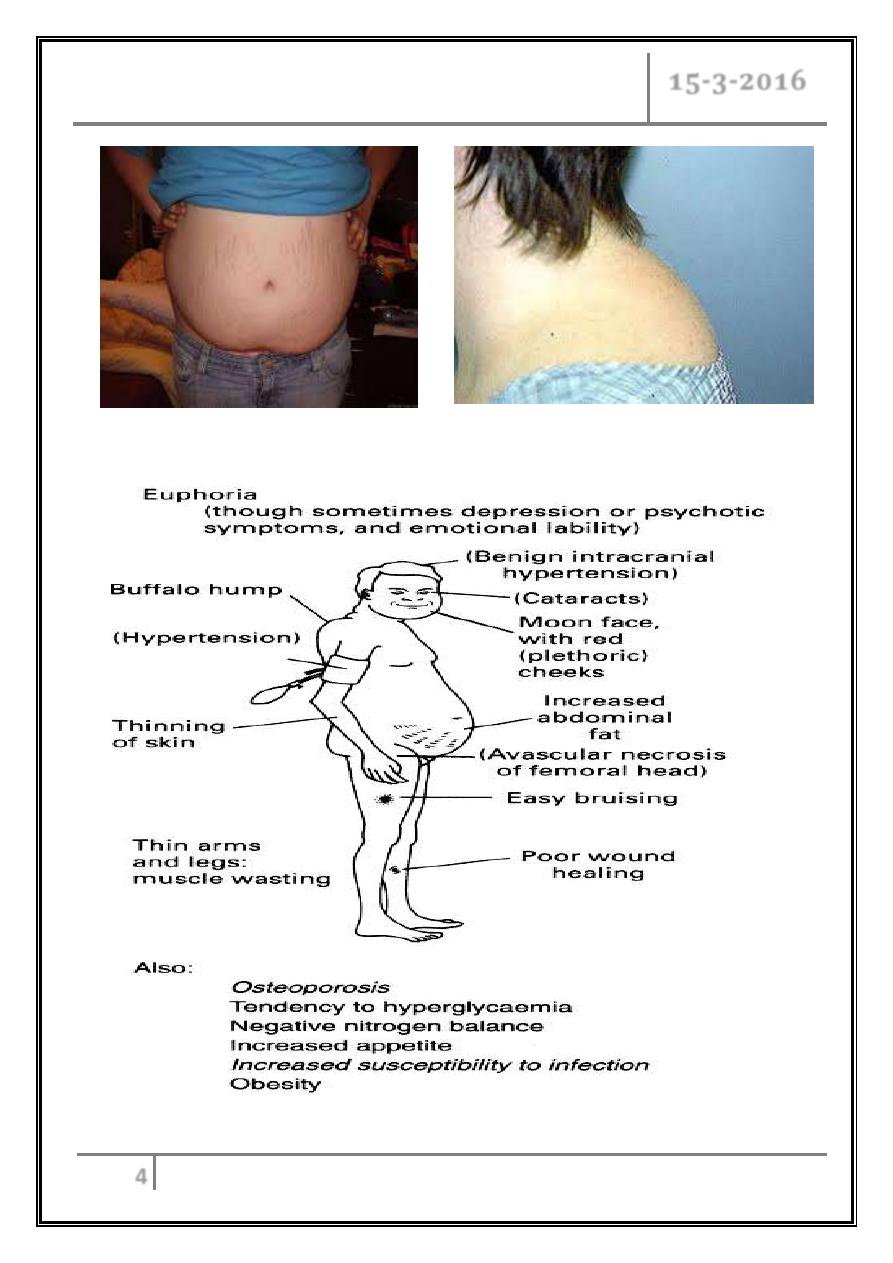
Clinical features
Truncal obesity.
Moon face.
Fat deposits (supraclavicular
fossa and buffalo hump).
HTN.
Hirsutism.
Amenorrhea and impotence.
Depression.
Thin skin.
Easy bruising.
Hypercoagulation.
Purplish wide abdominal
striae.
Proximal muscle weakness.
Osteoporosis.
Diabetes Mellitus.
Avascular necrosis.
Wound healing impaired.
Pysch. symptoms.
Hyperpigmentation.
Hypokalemic alkalosis.
Adrenal gland hyperfunction Dr. Manal
15-3-2016
4
Adrenal gland hyperfunction Dr. Manal
15-3-2016
5
Ectopic ACTH
All the previous symptoms but…
Ectopic dominated by :
- Hypokalemic alkalosis (dominant feature).
- Fluid retention.
- HTN.
- Glucose intolerance.
- Steroid psychosis.
Absence of other features may be explained by more sudden onset by acquired
ACTH from tumor.
Complications of Cushing's if untreated
Diabetes.
HTN.
Osteoporotic fractures and avascular necrosis.
Infections.
Psychosis.
Screening test
Overnight dexamethasone suppression test (1 mg at 11 pm, cortisol measured at
8-9 am) plasma cortisol> 50 nmol/ L, or
24 hour urine free cortisol increased > 50 microgram/ day, or
Midnight plasma or salivary cortisol > 130 nmol/ L.
False Positives
Severe depression.
Severe stress.
Estrogen (pregnancy or oral CP).
Morbid obesity.
Adrenal gland hyperfunction Dr. Manal
15-3-2016
6
False negatives
Phenytoin/phenobarbital/rifampin (accelerated metabolism of dexamethasone).
Confirmatory test
Low dose dexamethasone suppression test:
o Dexamethasone 0.5 mg q 6 x 48 hours,
o plasma cortisol > 50 nmol/L,
Or
o Measure urine cortisol during the last 24 hours (urine free cortisol >40
micrograms/ d).
Differential diagnosis
ACTH levels may distinguish ACTH-independent (adrenal or exogenous
glucocorticoids) from ACTH-dependent (pituitary, ectopic ACTH).
ACTH-independent - low ACTH to<5 pg/ ml.
ACTH-dependent - ACTH normal or high> 15pg/ml.
In addition, ectopic ACTH levels are usually 8x higher than pituitary caused
ACTH secreting adenomas.
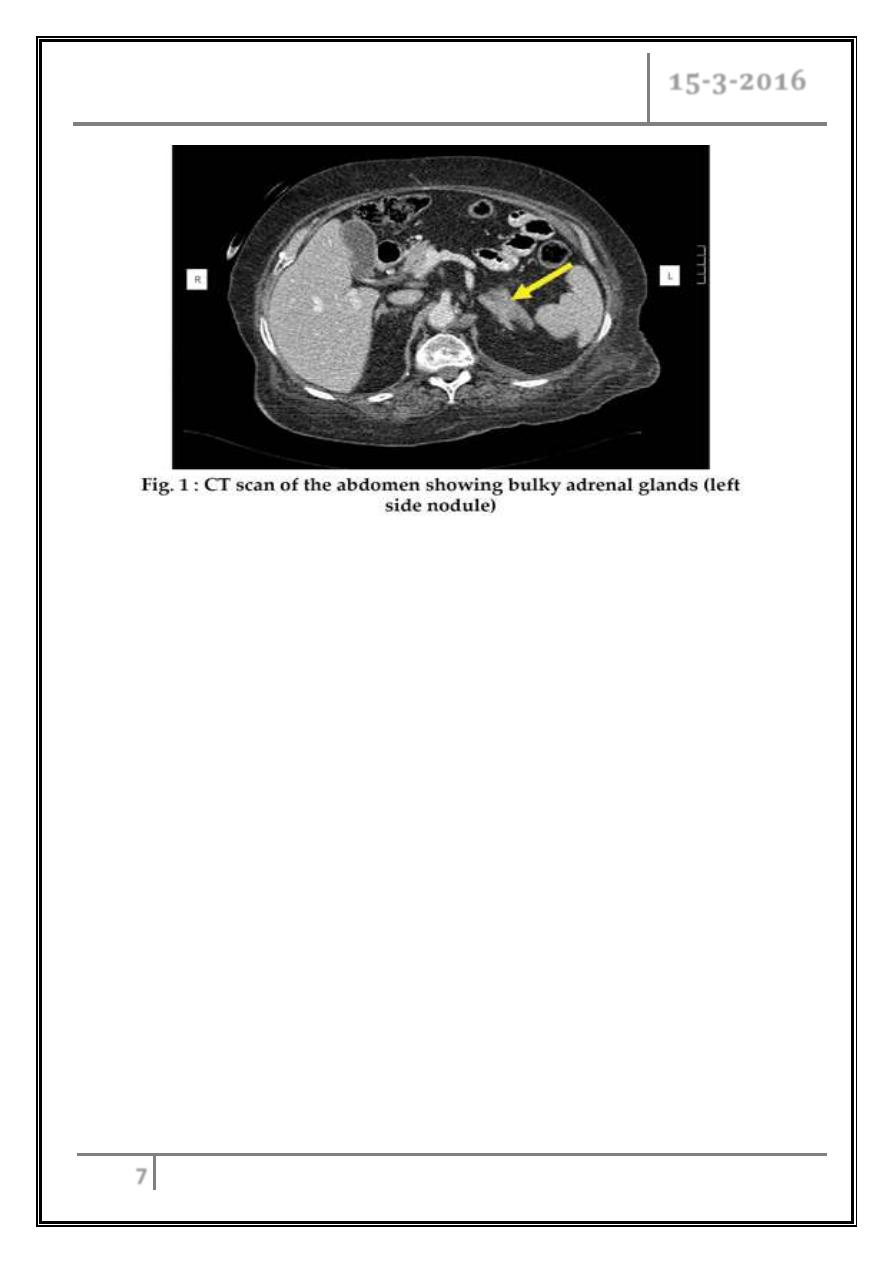
ACTH-independent
CT adrenals:
Bilateral micronodular or macronodular hyperplasia or unilateral adrenal
mass (adrenal tumor workup).
Adrenal gland hyperfunction Dr. Manal
15-3-2016
7
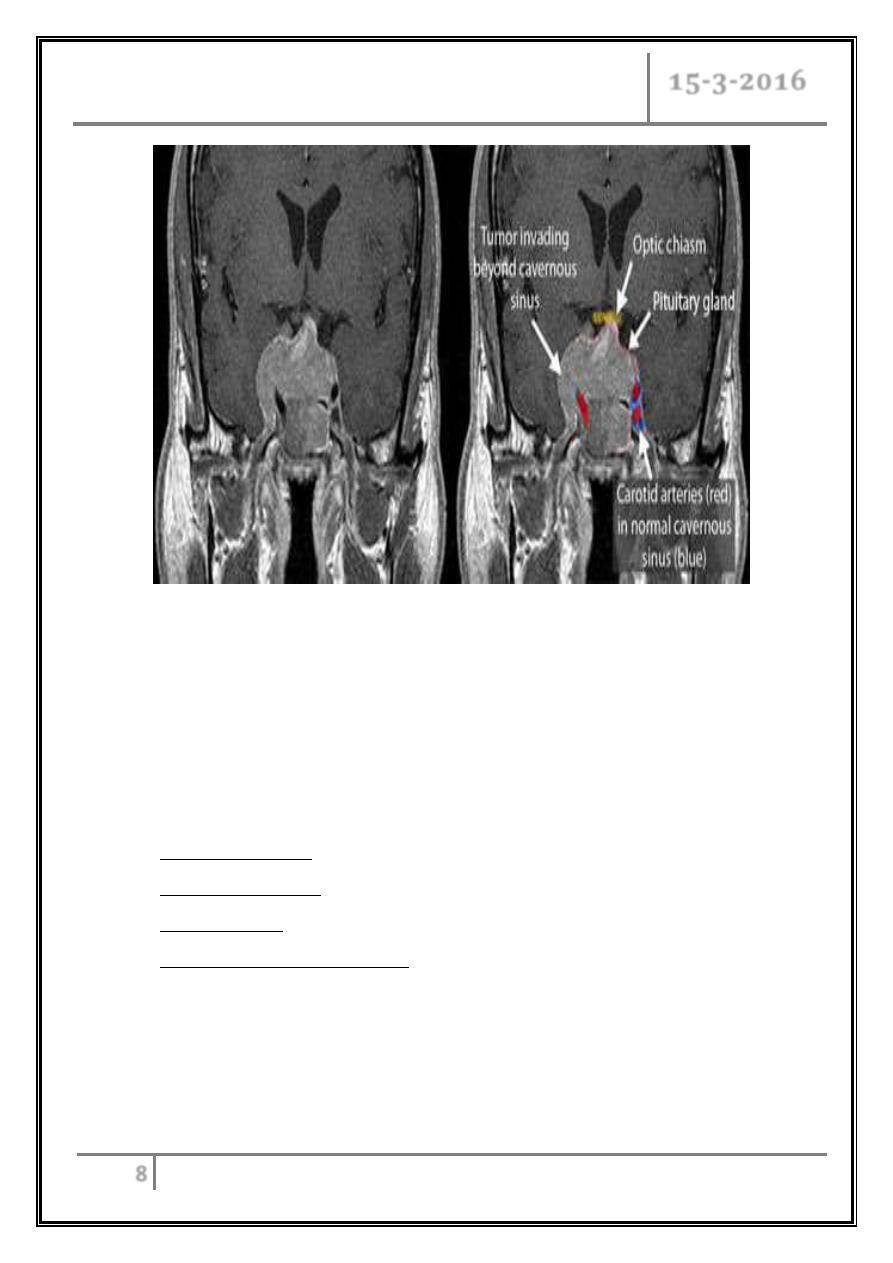
ACTH-dependent
MRI pituitary.
CRH test (ACTH increase>40% at 15- 30 min & cortisol > 20% at 45- 60
min after CRH 100 µg I.V.).
High dose DEX test (cortisol suppression > 50 % after q6h 2 mg DEX for 2
days).
-
Positive (Cushing’s disease)
- Negative test (Ectopic ACTH)
- Equivocal
inferior petrosal sinus sampling
(Petrosal/ peripheral ACTH ratio > 2 at baseline, > 3 at 2-5 min after
CRH 100 µg I.V.)
Inferior petrosal sinus sampling
-
Positive (Cushing’s disease).
- Negative (locate and remove ectopic ACTH source).
Adrenal gland hyperfunction Dr. Manal
15-3-2016
8
Treatment
Trans-sphenoidal surgery.
Pituitary radio-therapy.
Bilateral or unilateral adrenalectomy.
Medical therapy.
Treatment according to pathology:
Cushing’s disease: transphenoidal resection of pituitary adenoma.
Adrenal neoplasms: resection.
Ectopic ACTH: resection if possible.
Bilateral adrenal hyperplasia: may need adrenalectomies (lifelong
glucocorticoid and mineralcorticoid replacement).
Adrenal gland hyperfunction Dr. Manal
15-3-2016
9
‘Medical’ Adrenalectomy
Medications that inhibit steroidogenesis
Ketoconazole (600 to 1200 mg/ day) inhibits cortisol synthesis by a direct
action on the P450 cytochrome enzyme.
Metyrapone, blocks the 11-ß hydroxylase enzyme (exacerbates female
virilization)(2-3 g/ day).
Mitotane (2-3 g/ day) - has a cytotoxic effect on both normal and malignant
tissue.
Aminoglutethinide (1g/ day).
Ocreotide, major side effect is adrenal insufficiency, therefore start at lowest
dose and titrate.
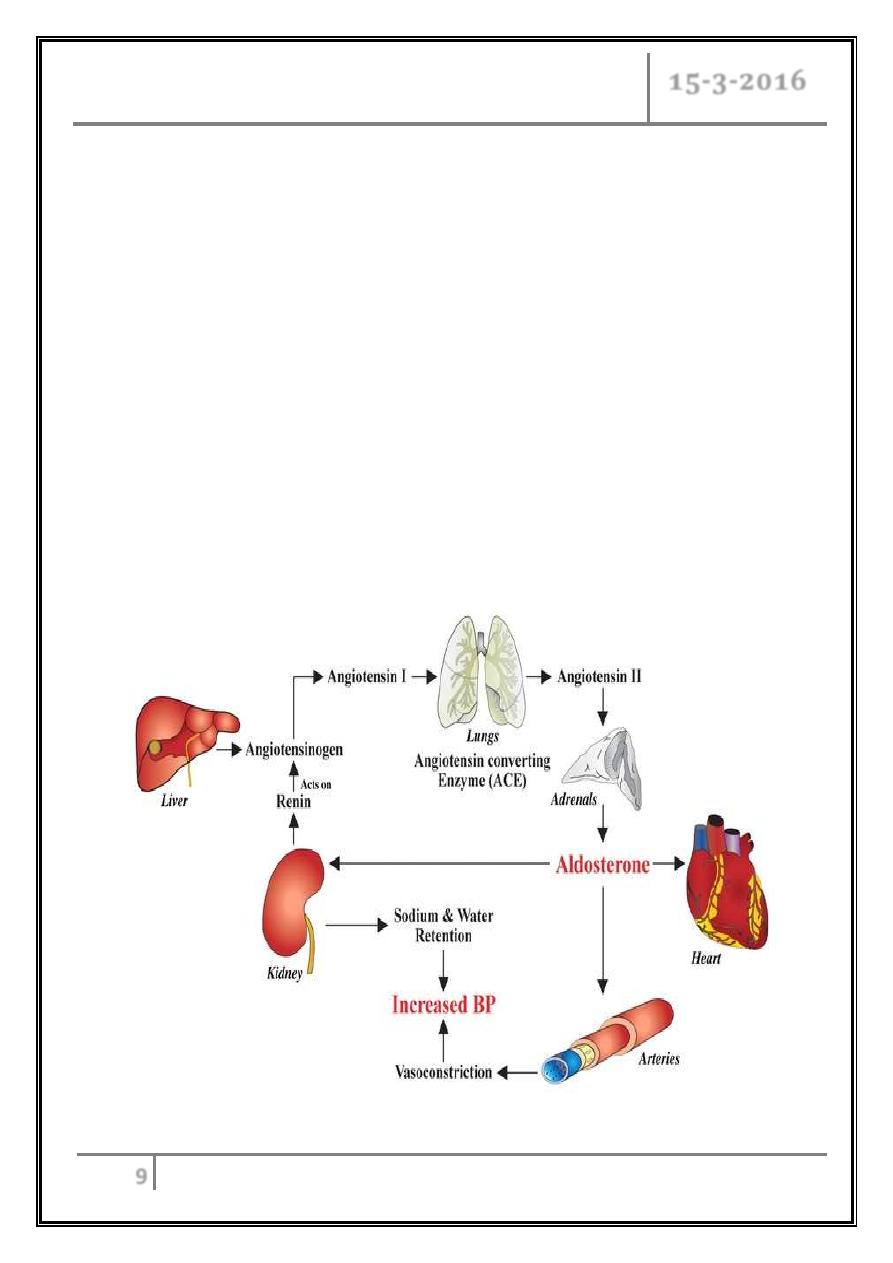
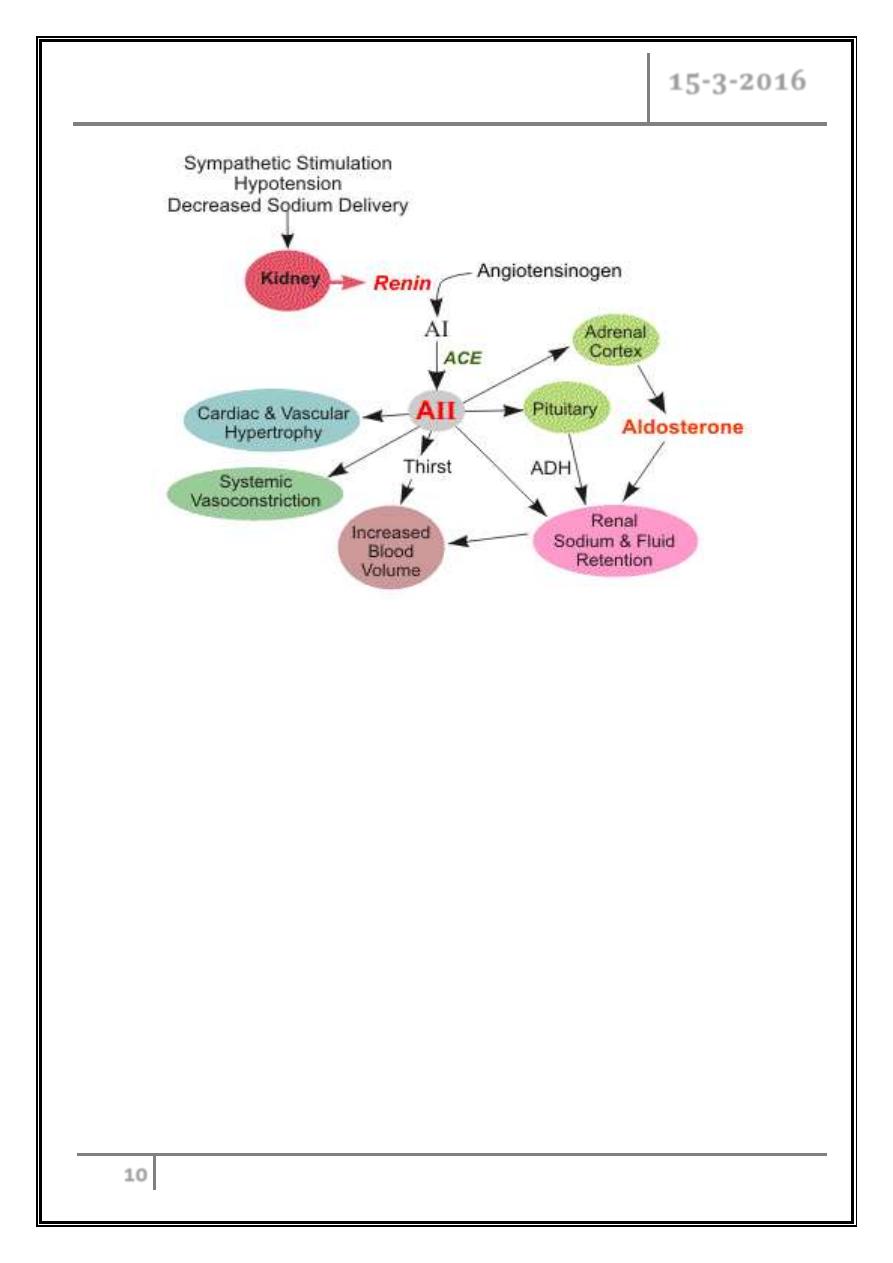
Mineralocorticoid Excess
Adrenal gland hyperfunction Dr. Manal
15-3-2016
10
Primary Hyperaldosteronism (high aldosterone and low renin)
Adrenal (Conn's) adenoma.
Bilateral (micronodular) adrenal hyperplasia.
Secondary hyperaldosteronism (high aldosterone and renin)
Diuretics, HF, liver F, NS, RAS.
Renin secreting renal tumor.
Low aldosterone and renin
Congenital adrenal hyperplasia (high DOC).
Liquorice misuse.
Liddle's syndrome.
Adrenal gland hyperfunction Dr. Manal
15-3-2016
11
Conn's syndrome
o An aldosterone-producing adrenal adenoma.
o Represents 5- 12% of hypertension causes.
o Peak age 30-50 years.
o Most patients are women.
Clinical features
Often asymptomatic.
Proximal muscle weakness to flaccid paralysis (because of low potassium
level).
Hypokalemic hypertension.
Leg edema due to sodium retention.
Investigations
Low K and high bicarbonate.
Upper normal Na.
Screening test: Aldosterone renin ratio > 750 pmol/ L: ng/ ml/ h and
aldosterone > 450 pmol/ L.
Confirmation of diagnosis: saline infusion (2 L saline over 4h I.V.), oral Na
test, fludrocortisone suppression test.
If still negative: abdominal CT (unilateral adrenal mass, bilateral
hyperplasia or normal adrenal morphology).
Adrenal vein catheterization to measure aldosterone.
Iodo- noncholesterol scanning.
Adrenal gland hyperfunction Dr. Manal
15-3-2016
12
Management
A. Unilateral adrenal adenoma and age < 40 y:
- Unilateral adrenalectomy preceded by medical treatment for few weeks.
- If > 40y and still surgery is indicated we depend on result of vein sampling
(if positive then surgery but if negative treat by drugs).
B. Bilateral adrenal hyperplasia:
- Spironolactone (Aldactone) up to 400mg/ d and amiloride (10- 40mg/ d).
References
Davidson’s Principles of Internal Medicine 20
th
Edition.
Harrison’s Principles of Internal Medicine 18
th
Edition.
… End …
Adrenal gland hyperfunction Dr. Manal
15-3-2016
13
Quiz
1- A cushinoid appearance would be an expected finding in all of the following
conditions EXCEPT:
a- Chronic alcohol abuse.
b- Pituitary microadenoma.
c- ACTH- secreting bronchial carcinoma.
d- Adrenocortical adenoma.
2- The typical clinical features of Conn's syndrome include all of the following
EXCEPT:
a- Hypertension.
b- Muscle weakness.
c- Hypokalemic alkalosis.
d- High aldosterone and high renin.
