Dr. Khalid A. Al- Khazraji
Lec. 7
ACUTE UPPER GI
BLEEDING
Wed. 2 / 3 / 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Acute upper GI bleeding Dr. Khalid A. Al- Khazraji
2-3-2016
1
Acute upper gastrointestinal bleeding
Epidemiology
The most common gastrointestinal emergency.
Overall incidence is approximately 100 hospitalizations per 100 000 adults per
year.
The incidence among men is approximately double than that among women.
Rate increases markedly with age.
Mortality rate is 5-12%.
Clinical features
The two cardinal features are:
1- Haematemesis: bloody vomitus; either fresh & bright red, or older and “coffee-
ground” in character.
2- Melaena: passage of black, tarry, foul-smelling stools.
Following a bleed from the upper GI tract, unaltered blood can appear per
rectum, but the bleeding must be massive and is almost always accompanied by shock.
The passage of dark blood and clots without shock is always due to lower GI bleeding.
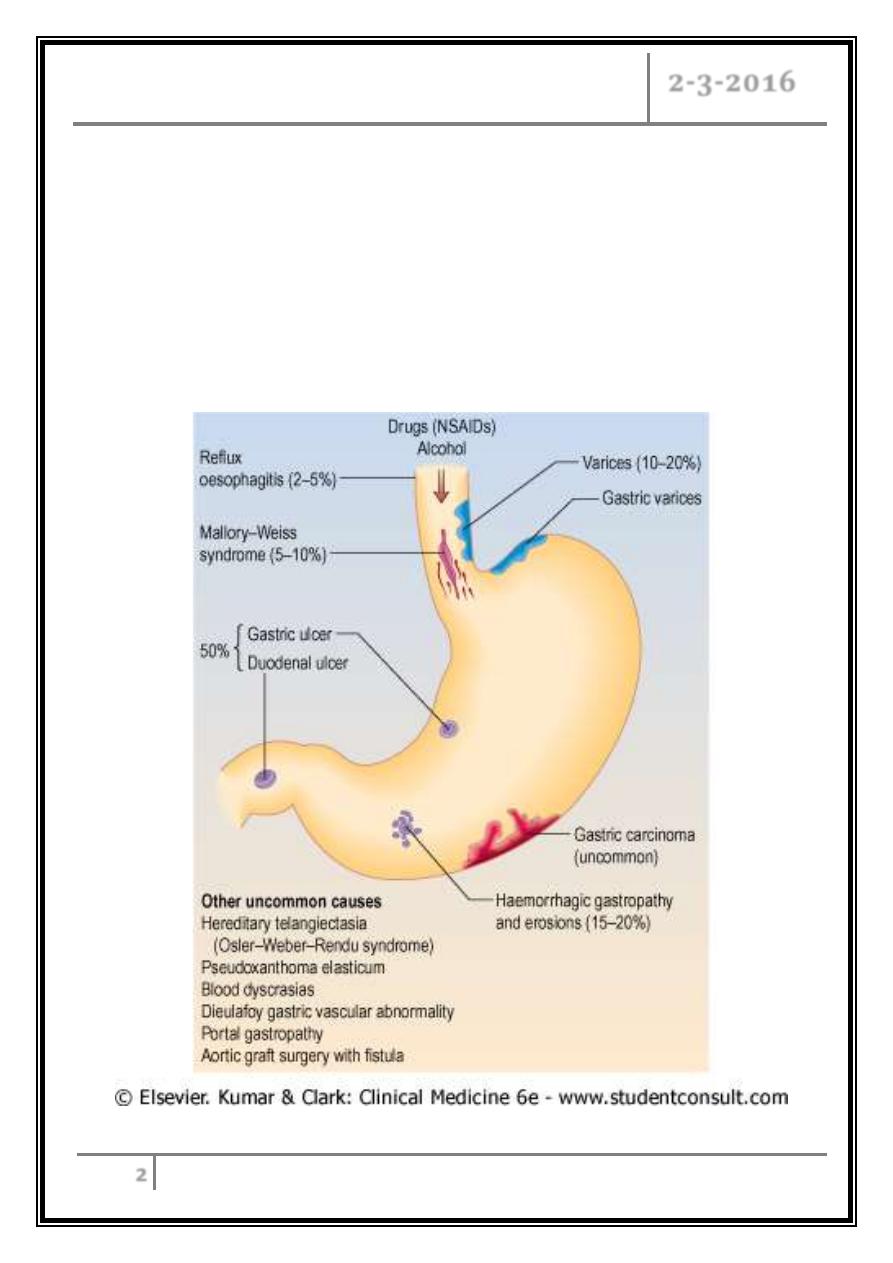
Aetiology
Common causes:
1- Peptic ulcer 35-50%.
2- Gastric erosions 10-20%.
3- Esophagitis (usually with hiatus hernia) 5%.
4- 4-Varices 5-15%.
5- Vascular malformation 2%.
6- Mallory - Weiss tears 5%.
7- Cancer of stomach or esophagus 5%.
Acute upper GI bleeding Dr. Khalid A. Al- Khazraji
2-3-2016
2
Other uncommon causes:
1- Hereditary telangiectasia (Osler-Weber-Rendu syndrome).
2- Pseudoxanthoma elasticum.
3- Blood dyscrasias.
4- Dieulafoy gastric vascular abnormality.
5- Portal gastropathy.
6- Aortic graft surgery with fistula.
Causes
Acute upper GI bleeding Dr. Khalid A. Al- Khazraji
2-3-2016
3
Clinical assessment
Haematemesis is red with clots when bleeding is profuse, or black (coffee
grounds) when less severe.
Intravascular volume depletion
Hypotension
Syncope
Symptoms of anaemia suggest chronic bleeding.
Approximately 85% of patients stop bleeding spontaneously within 48 hours.
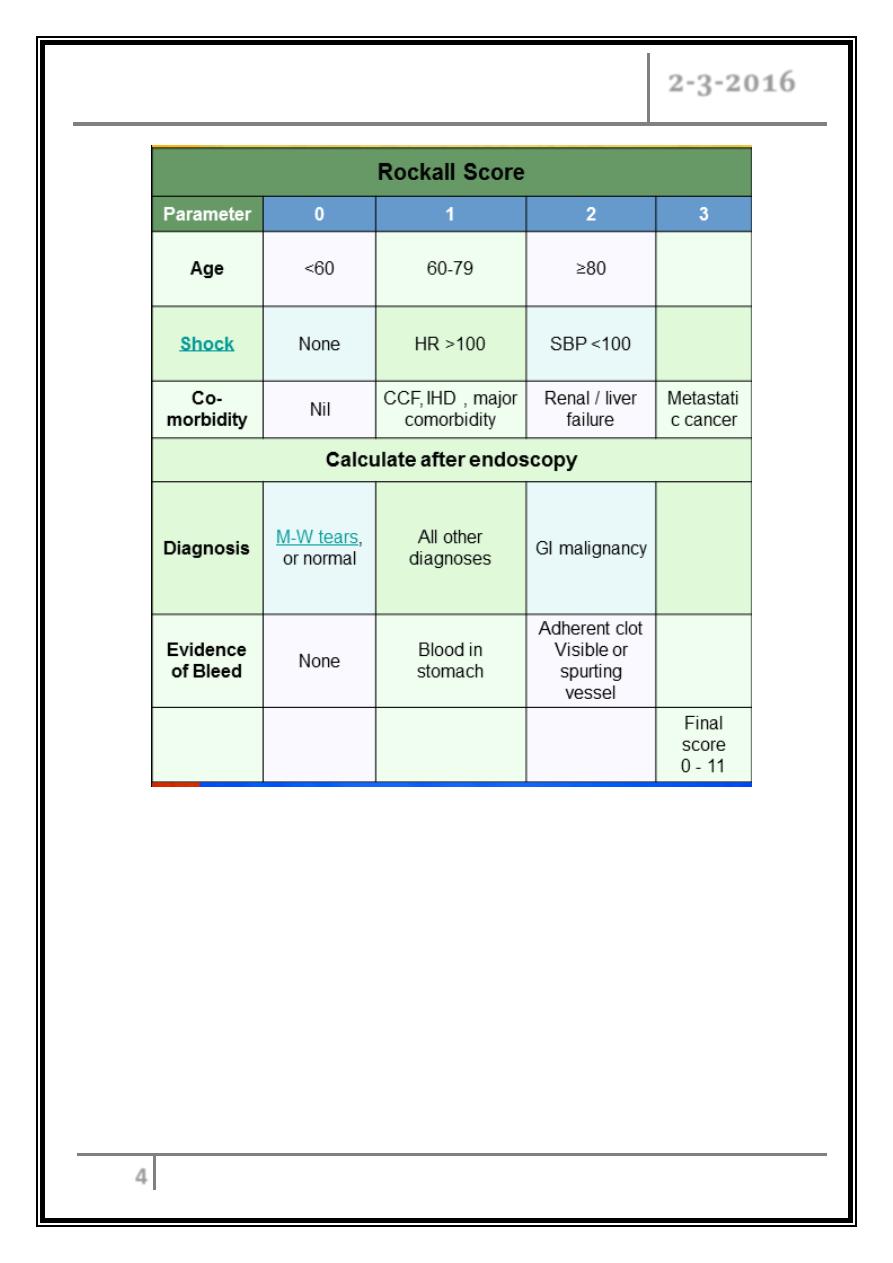
Factors affects the risk of rebleeding and death:
- Age.
- Evidence of co-morbidity.
- Shock.
- Endoscopic diagnosis.
- Ulcer with active bleeding.
- Clinical signs of chronic liver disease.
Acute upper GI bleeding Dr. Khalid A. Al- Khazraji
2-3-2016
4
Management
The goals of management:
First the patient’s hemodynamic status must rapidly assessed & resuscitative
measures initiated.
Only then should next steps in management be undertaken: determine the source
of hemorrhage, stop the bleeding and prevent recurrent rebleeding.
Acute upper GI bleeding Dr. Khalid A. Al- Khazraji
2-3-2016
5
Immediate management
1- History and examination. Note co-morbidity.
2- Monitor pulse and BP half-hourly.
3- Take blood for: Hb, electrolytes, urea, liver biochemistry, coagulation screen,
group and cross-match.
4- IV access (2 large-bore I.V. cannulae). Central line if brisk bleeding.
5- Give blood transfusion/colloid if necessary.
Indications for blood transfusions are:
A- Shock.
B- Hb less than 10 g/dL.
6- Oxygen.
7- Urgent endoscopy in shocked patients/ liver disease.
8- Continue to monitor pulse and BP.
9- Re-endoscope for continued bleeding/ hypovolemia.
10- Surgery if bleeding persists.
Indication for urgent endoscopy:
1- Large initial bleed.
2- Patients with resting hypotension or orthostatic change.
3- Repeated hematemesis or bloody nasogastric.
4- Requiring blood transfusions.
Acute upper GI bleeding Dr. Khalid A. Al- Khazraji
2-3-2016
6
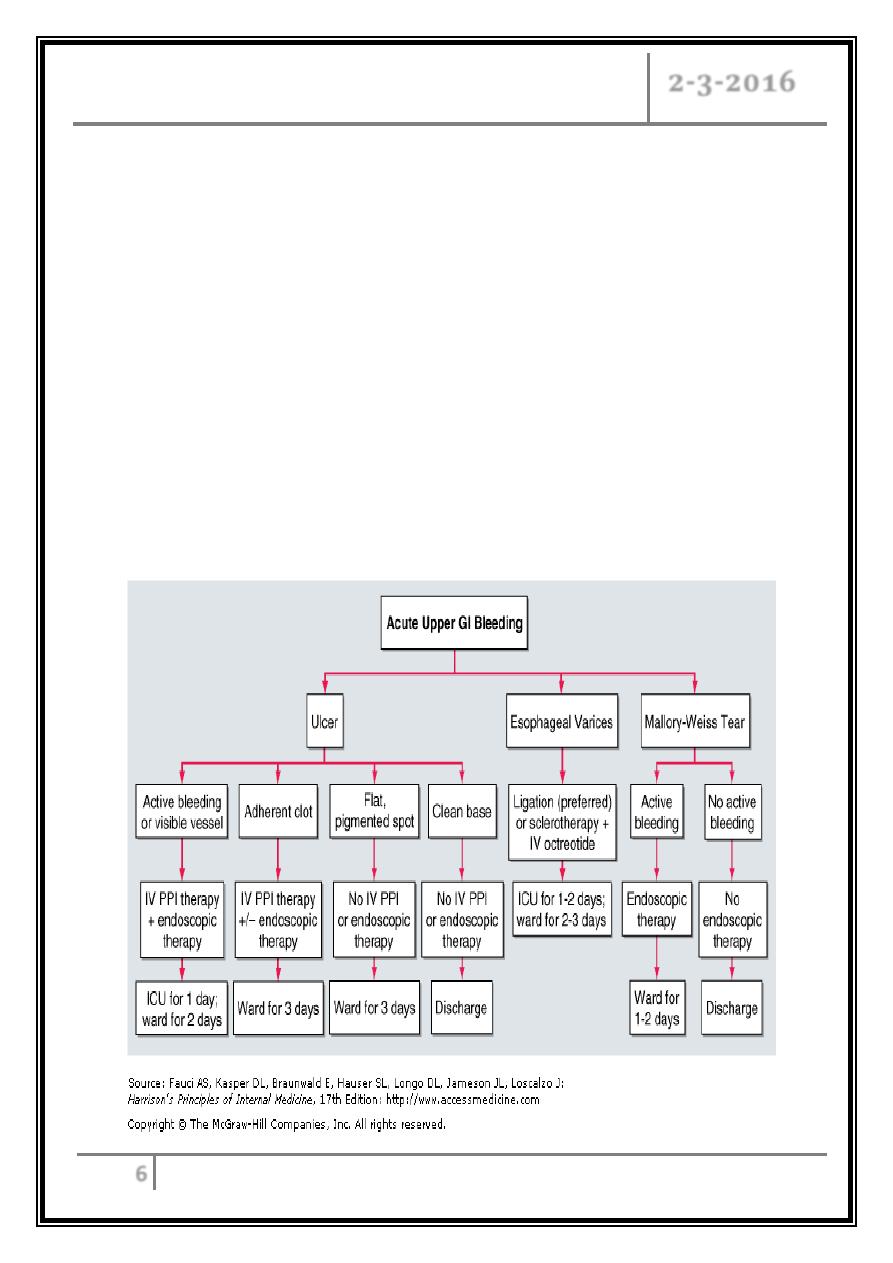
o Endoscopy
Can detect the cause of bleeding in 80% or more of cases.
At first endoscopy:
- Varices treated with banding, or sclerosing.
- Bleeding ulcer treated with two haemostatic methods (injection with
adrenaline ,& thermal coagulation), or by endoscopic clipping
- Take antral biopsy for H. pylori.
o Drug therapy
After diagnosis at endoscopy, give I.V. omeprazole 80 mg followed by 8
mg/h 72 hours to all ulcer patients as it reduces the rebleeding rates and the
need for surgery.
H2-receptor antagonists are of no value.
Acute upper GI bleeding Dr. Khalid A. Al- Khazraji
2-3-2016
7
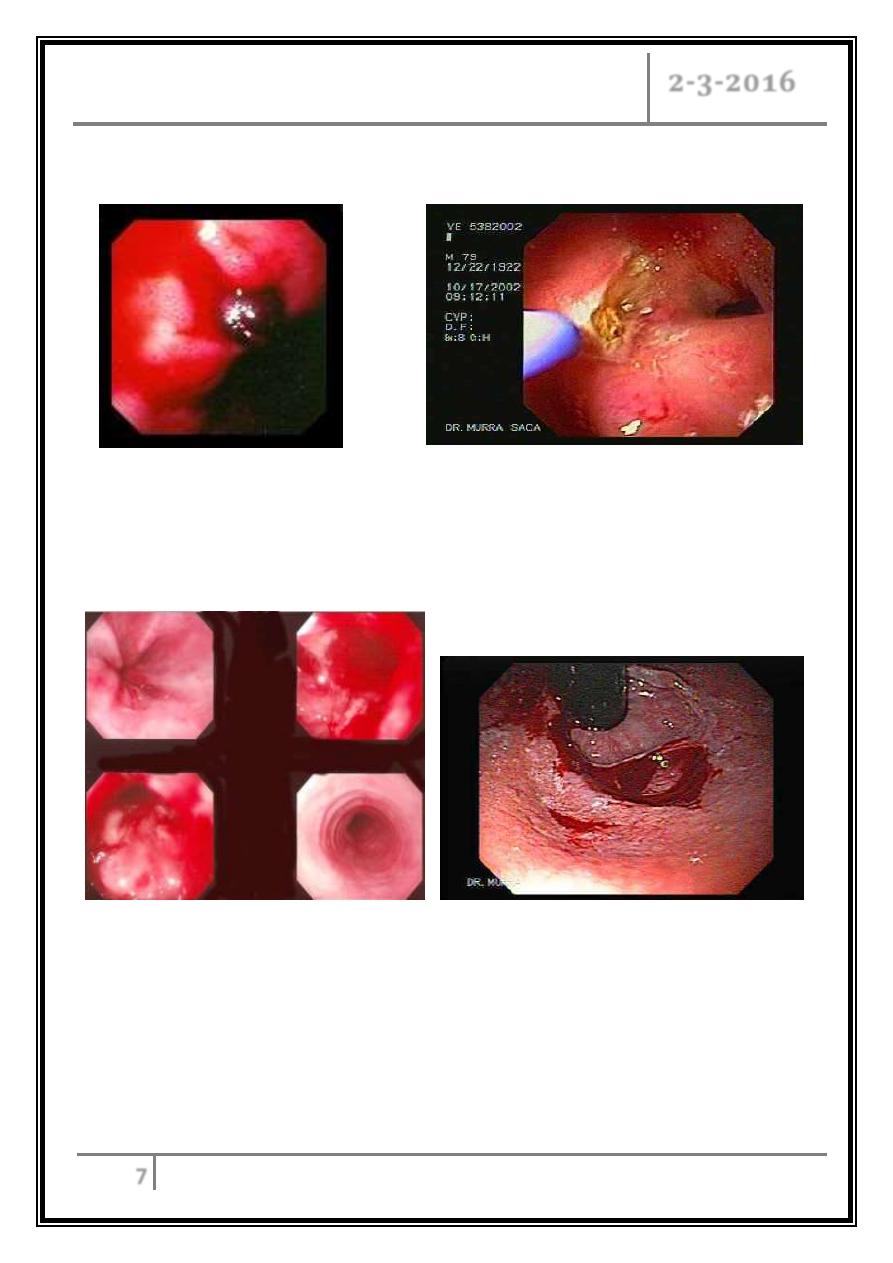
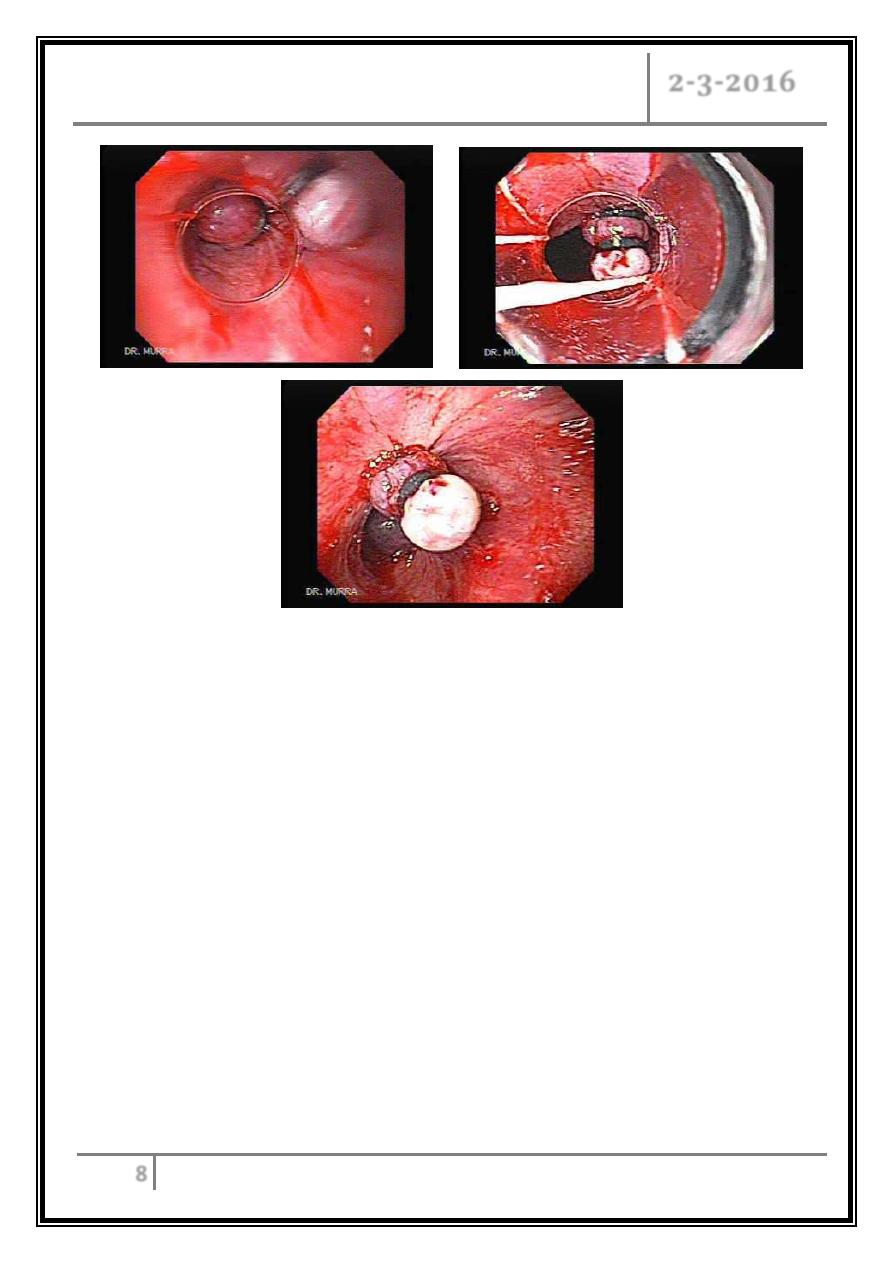
Atlas
DU with clot Therapy with Argon photocoagulation of
vessels of DU
Mallory-Weiss syndrome
Acute upper GI bleeding Dr. Khalid A. Al- Khazraji
2-3-2016
8
Variceal banding
… End …
