Dr. Khalid A. Al- Khazraji
Lec. 6
PEPTIC ULCER DISEASE
Tues. 1 / 3 / 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Peptic ulcer disease Dr. Khalid A. Al- Khazraji
1-3-2016
1
Peptic ulcer disease
Ulcer: is a disruption of the mucosal integrity of the stomach and/or duodenum
leading to a local defect or excavation due to active inflammation.
DUs: occur in D1 in more than 95% with about 90% located within 3 cm of
pylorus. They are usually equal or less than 1 cm in diameter, occasionally
reach 3-6 cm (giant ulcer).
GUs: can represent a malignancy in contrast to DUs. The benign GU often
found distal to the junction between the antrum and the acid secretory mucosa
Pathophysiology
DU: H. Pylori and NSAID-induced injury account for the majority of DUs.
GU: as in DUs, the majority of GUs can be attributed to either H. Pylori or
NSAID-induced mucosal damage.
H. Pylori and acid peptic disorders: gastric infection with the bacterium H.
Pylori accounts for the majority of PUD.
Pathophysiology
The particular end result of H.pylori infection (gastritis, PUD, gastric MALT
lymphoma, gastric cancer) is determined by a complex interplay between bacterial
and host factors
1- Bacterial factors: H.pylori is able to facilitate gastric residence, induce mucosal
injury, and avoid host defense. A specific region of the bacterial genome, the
pathogenicity island, encodes the virulence factors Cag A and pic B. Vac A also
contributes to pathogenicity, though it not encoded within the pathogenicity
island.
Peptic ulcer disease Dr. Khalid A. Al- Khazraji
1-3-2016
2
Urease allows the bacteria to reside in the acidic stomach, generating NH3
which can damage epithelial cells. H. pylori makes proteases and
phospholipases that break down the glycoprotein lipid complex of the mucous
gel, thus reducing the efficacy of this first line of mucosal defense.
2- Host factors: the inflammatory response to H. pylori includes recruitment of
neutrophils, lymphocytes (T and B), macrophages, and plasma cells. The
pathogen leads to local injury leading to cell death (apoptosis), moreover,
bacterial strains that encode cag-PAI can introduce Cag A into host cells,
leading to further cell injury and activation of cellular pathways involved in
cytokine production.
Clinical features
History:
- Abdominal pain: is common in GI disorders including DU and GU, but poor
predictive value for presence of either a DU or GU.
- Up to 10% of patients with the NSAID-induced mucosal disease can present
with complications (bleeding or perforation and obstruction).
- Epigastric pain occurs as a burning or gnawing discomfort, and can be
present in both GU and DU.
- The typical pain pattern in DU occurs minutes to 3 h after a meal and
frequently relieved by food or antacids.
- Pain that awakes the patient from sleep (between midnight and 3 A.M.) is
the most discriminating symptom with 2 thirds of DU patients describing this
complaint.
- The pain pattern in GU patients may be different from that in DU patients
where discomfort may actually be precipitated by food.
- Nausea and weight loss occur more commonly in GU patients.
Peptic ulcer disease Dr. Khalid A. Al- Khazraji
1-3-2016
3
- Vomiting: is infrequent but often relieves pain, while persistent daily
vomiting suggests gastric outlet obstruction.
- Anorexia may occur.
Physical examination:
- Epigastric tenderness is the most frequent finding.
- Tachycardia and orthostasis suggest dehydration secondary to vomiting or
active GI blood loss.
- A severely tender, boardlike abdomen suggests a perforation.
Differential diagnosis
Non-ulcer dyspepsia.
GERD.
Biliary tract disease.
Pancreatitis.
Coronary and/ or mesenteric vascular insufficiency.
Intra-abdominal neoplasms.
Functional bowel syndrome.
Inflammatory bowel disease.
Investigations
1-
Endoscopy
- Most sensitive and specific approach for examining the upper GI tract.
- Direct visualization of mucosa, helpful in identifying too small or atypical
lesions detected by radiography, and taking a tissue biopsy to rule out
malignancy (GU) or H. pylori.
- Determine if the ulcer is a source of bleeding.
- DU is almost never malignant and does not required biopsy.
- GU must always require biopsy in most circumstances, because it’s
occasionally malignant.
Peptic ulcer disease Dr. Khalid A. Al- Khazraji
1-3-2016
4
- Biopsy urease test.
-
Endoscopy is indicated in all patients with “alarm symptoms”.
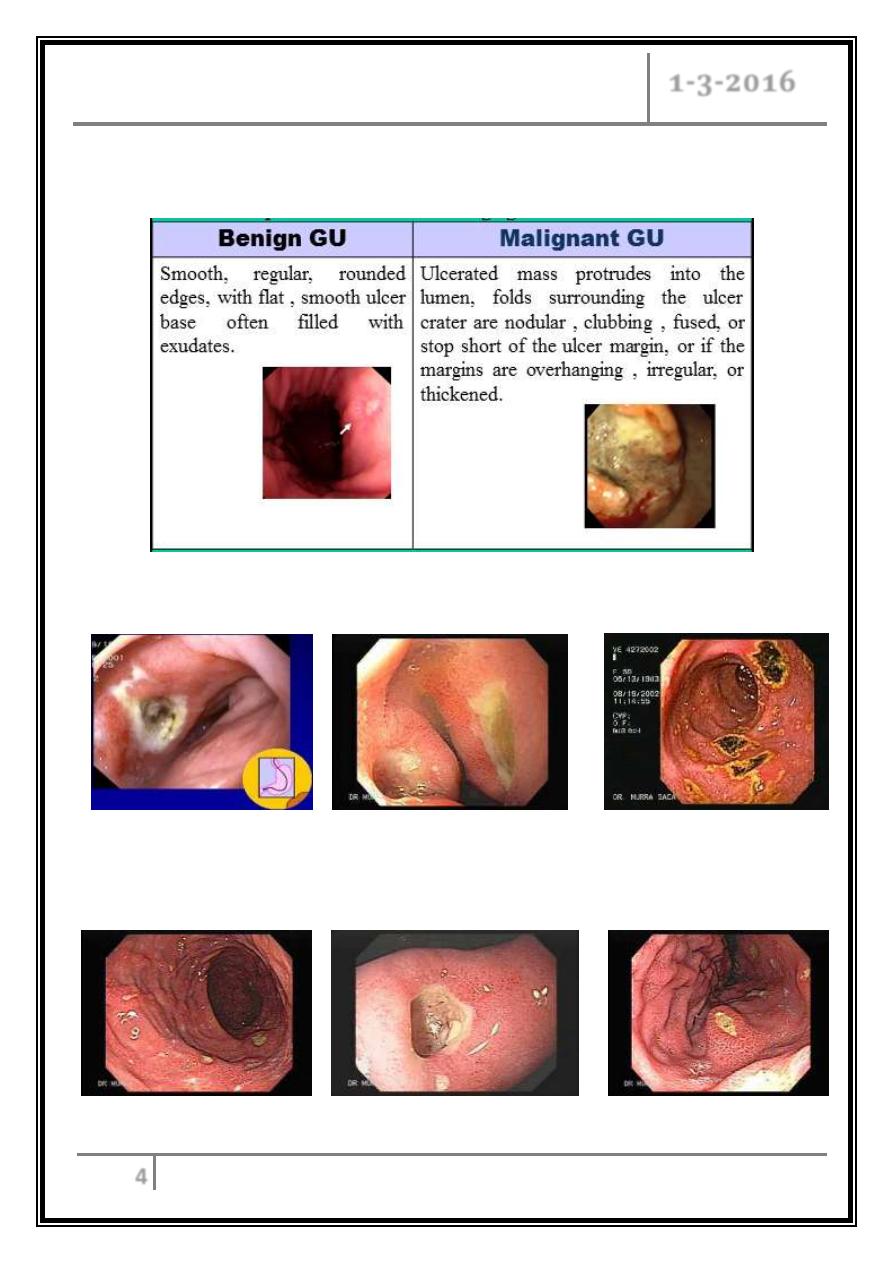
Endoscopic differentiation of benign gastric ulcer from cancer
DU Kissing DUs Multiple DUs
Multiple GUs GU GU
Peptic ulcer disease Dr. Khalid A. Al- Khazraji
1-3-2016
5
2-
Non–invasive methods:
- Serology: detect IgG, used in diagnosis and epidemiological studies, sensitive
(90%) & specific (83%).
-
13
C-urea breath test: quick and reliable test, sensitive (97%) & specific
(96%). This test is suitable for testing for eradication of the organism.
- Stool antigen test: sensitive (97.6%) & specific (96%). This test is useful in
the diagnosis of H.pylori infection and for monitoring efficacy of eradication
therapy.
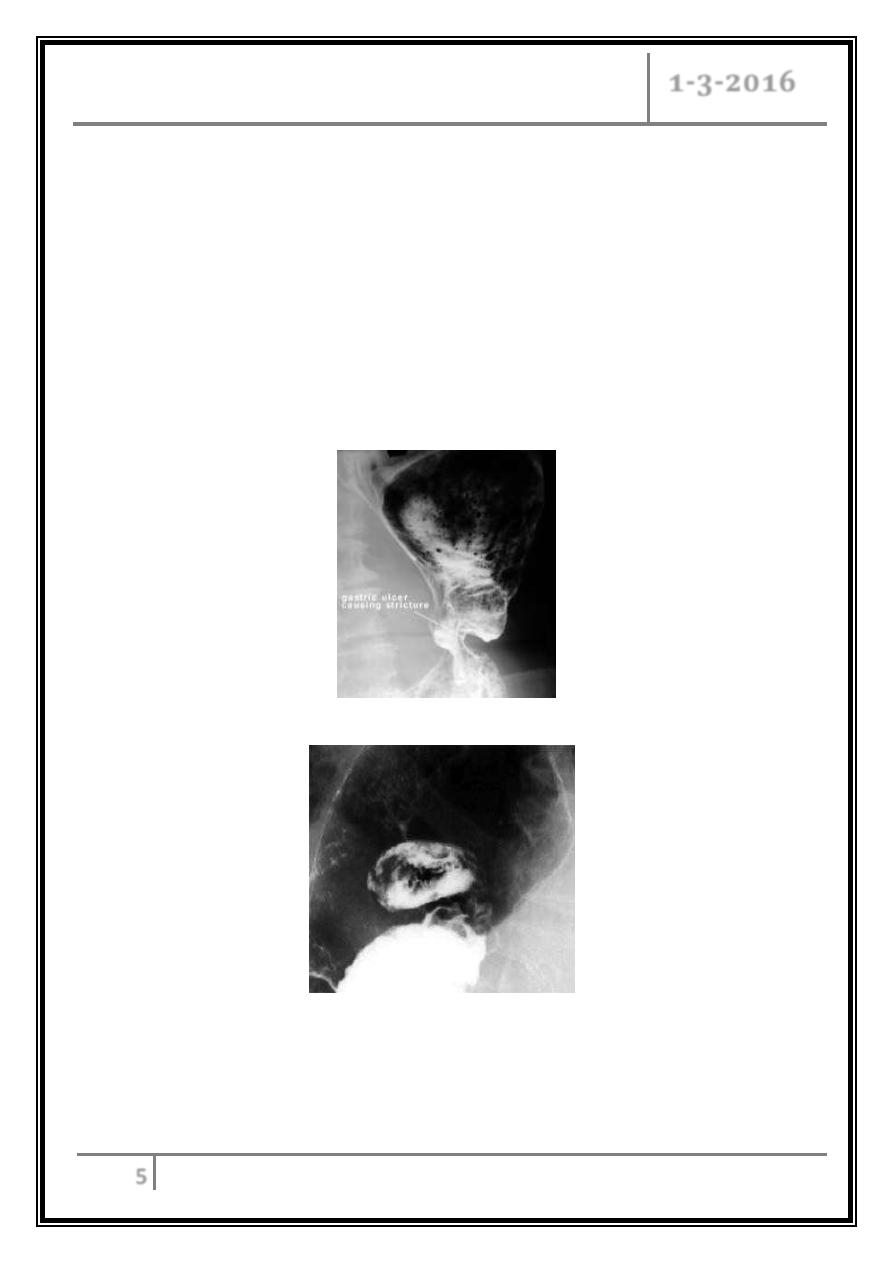
Gastric ulcer - body of the stomach
A 5-cm ulcer crater in the lesser curve of the stomach is depicted en
face. The filling defects in the ulcer crater are caused by a blood clot
from recent bleeding.
Peptic ulcer disease Dr. Khalid A. Al- Khazraji
1-3-2016
6
Treatment
The goals of the ulcer therapy:-
o Relieve symptom.
o Heal the ulcer.
o Cure H.pylori and Prevent recurrence.
Acid neutralizing/ inhibitory drugs
Antacids
- Neutralization of secreted acid with antacids constituted the main form of
therapy for peptic ulcers.
- They are now rarely, if ever, used as the primary therapeutic agent but
instead are often used by patients for symptomatic relief of dyspepsia.
- The most commonly used agents are mixtures of aluminum hydroxide and
magnesium hydroxide.
- Aluminum hydroxide can produce constipation and phosphate depletion,
while magnesium hydroxide may cause loose stools.
- Many of the commonly used antacids (e.g. Maalox) have a combination of
both aluminum hydroxide and magnesium hydroxide in order to avoid
these side effects.
- Calcium carbonate and sodium bicarbonate are potent antacids with
varying levels of potential problems.
Peptic ulcer disease Dr. Khalid A. Al- Khazraji
1-3-2016
7
H
2
Receptor antagonists
- Four of these agents are presently available (cimetidine, ranitidine,
famotidine, nizatidine).
- Although each has a different potency, all will significantly inhibit basal
and stimulated acid secretion to comparable levels when used at
therapeutic doses.
- Dosing for cimetidine is 800 mg at bed time for treatment of active ulcer
with healing rate about 80% at 4 weeks.
- Comparable night-time dosing regimens are ranitidine 300 mg,
famotidine 40 mg, and nizatidine 300 mg.
Proton pump (H
+
, K
+
-ATPase) inhibitors
- Omeprazole, esomeprazole, lansoprazole, rabeprazole, and pantoprazole
are substituted benzimidazole derivatives that covalently bind and
irreversibly inhibit H
+
, K
+
-ATPase.
- Esomeprazole is the newest member.
- Omeprazole and lansoprazole are PPIs that have been used for the
longest time.
Cytoprotective agents
Sucralfate
- A complex sucrose salt in which the hydroxyl group have been substituted
by aluminum hydroxide and sulfate.
- It’s insoluble in water and becomes a viscous paste within the stomach
and duodenum, binding primarily to sites of active ulcerations.
Peptic ulcer disease Dr. Khalid A. Al- Khazraji
1-3-2016
8
Bismuth-containing preparations
- Colloidal bismuth subcitrate CBC and bismuth subsalicylate BSS are the
most widely used preparations.
- Potential mechanisms include ulcer coating, prevention of further pepsin/
HCl-induced damage; binding of pepsin, and stimulation of PGs,
bicarbonate and mucous secretion.
Prostaglandin analogues
- Standard therapeutic dose is 200 micro-gram qid
- Central role in maintaining mucosal integrity and repair.
Regimens recommended for eradication of H.Pylori infection
Triple therapies
- Bismuth subsalicylate 2 tabs qid, plus metronidazole 250 mg qid, plus
tetracycline 500 mg qid, or
- Ranitidine bismuth citrate 400 mg bid, plus tetracycline 500 mg bid, plus
clarithromycin or metronidazole 500 mg bid, or
- Omeprazole (lansoprazole) 20 mg bid (30 mg bid), plus clarithromycin
250 or 500 mg bid, plus metronidazole 500 mg bid or Amoxicillin 1 g bid.
Quadruple therapy
1- Omeprazole (lansoprazole) 20 mg bid (30 mg bid) daily.
2- Bismuth subsalicylate 2 tabs qid.
3- Metronidazole 250 mg bid.
4- Tetracycline 500 mg bid.
Peptic ulcer disease Dr. Khalid A. Al- Khazraji
1-3-2016
9
Recommendations for treatment of NSAID-related mucosal
injury
Active ulcer
- NSAID discontinued ------- H2 receptor antagonist or PPI.
- NSAID continued ------- PPI.
Prophylactic therapy ------- Misoprostol
------- PPI
------- Selective COX-2 inhibitor
H. pylori infection ------- eradication if active ulcer present or a past history
of peptic ulcer disease.
Indications for surgery in PU
Emergency:
1- Perforation.
2- Hemorrhage.
Elective:
1- Complications: e.g. gastric outflow obstruction.
2- Recurrent ulcer following gastric surgery.
Complications of gastric resection or vagotomy:
Dumping.
Bile reflux gastritis.
Diarrhea and maldigestion.
Weight loss.
Anemia.
Metabolic bone disease.
Gastric cancer.
Peptic ulcer disease Dr. Khalid A. Al- Khazraji
1-3-2016
10
Complications of PU
Hemorrhage.
Perforation: DU is perforated more commonly than GUs, usually into
peritoneal cavity, and into lesser sac also occurs. Surgery usually done to close
the perforation and drain the abdomen.
Gastric outlet obstruction: may be prepyloric, pyloric, or duodenal. Occurs due
to active ulcer with surrounding edema or healing ulcer with following scarring.
… End …
