13/3/2016
Operative Intervention in Obstetrics
Dr. Raghad
1
BY:TAHER ALI TAHER
Operative Intervention in Obstetrics
Caesarean Section:
Caesarean section refers to an operation that is performed to deliver a
baby via the trans-abdominal route.
Indications for caesarean section:
Past obstetric history:
Previous classical C/S.
Interval pelvic floor or anal sphincter repair.
Previous severe shoulder dystocia with significant neonatal
injury.
Current pregnancy events:
Significant fetal disease likely to lead to poor tolerance of
labor.
Mono-amniotic twins.
Placenta previa.
Obstructing pelvic mass.
Active primary herpes at onset of labor.
Intra-partum events:
Acute fetal compromise in the first stage.
Maternal disease for which delay in delivery may
compromise the safety of the mother.
Absolute cephalo-pelvic disproportion (brow presentation,
etc)
There are many other indications for C/S.
Preparations for caesarean section:
Full informed consent must always be obtained prior to operation,
supra-pubic shaving, bladder should be emptied, foly's catheter is
inserted and remains per operatively, premedication with antacid is
standard, and all patients being transferred to theatre must be in the left
lateral position with a wedge under the right buttock (to prevent supine
hypotension and fetal distress). The operating table must be kept in a
left lateral tilt position until after the delivery. Thrombo-prophylaxis
13/3/2016
Operative Intervention in Obstetrics
Dr. Raghad
2
BY:TAHER ALI TAHER
should be considered for all patients and prophylactic antibiotic should
be given.
Operative Procedure:
Skin incision either: * supra-pubic transverse incision (pfannenstiel
incision commonly used): has the advantage of improved cosmetic
results, decreased analgesic requirements and thus less postoperative
pulmonary compromise and superior wound strength,
Or * midline vertical incision which provides greater ease of access to
the pelvic and intra-abdominal organs and may be enlarged more
easily, may be indicated in extreme maternal obesity, or suspected
other intra-abdominal pathology.
Uterine incisions: either * transverse lower segment uterine incision
is used in more than 90% of C/S due to:
Ease to repair.
Reduced blood loss.
Lower incidence dehiscence or rupture in subsequent pregnancies
Or * vertical upper segment uterine incision which is indicated in
certain situation because:
It is difficult to repair.
Associated with severe bleeding.
More incidence of rupture in subsequent pregnancies.
Indications of classical uterine incision:
Lower segment fibroid.
Lower segment dense adhesions.
Placenta previa with large vessels in the lower segment.
Transverse lie with back down and prolapsed arm.
PPROM associated with poor lower segment and transverse
lie
Conjoined twins
C/S in the presence of cervical carcinoma.
Post-mortem C/S.
Other types of uterine incisions are U-shape, J-shape, or modified
classical incision (lower segment vertical) incisions.
After delivering the baby, placenta and membranes should be
delivered by continuous cord traction.
13/3/2016
Operative Intervention in Obstetrics
Dr. Raghad
3
BY:TAHER ALI TAHER
Uterine closure: either in single layer or in double layer, with good
heamostasis. Closure with double layer is preferred as it is
associated with less scar dehiscence in subsequent pregnancies.
Complications of ceasarean section:
Intra-operative:
Anesthetic complication (e.g. atelactasis).
Urinary tract damage (bladder and ureteric injury).
Bowel injury.
Hemorrhage: due to vascular injury like uterine artery injury, or
due to uterine atony or placenta previa. There are many
maneuvers that may be employed to manage such cases rang
from bimanual compression, infusion of oxytocin, applying
compression sutures to the more radical but life saving
hysterectomy.
Caesarean hysterectomy.
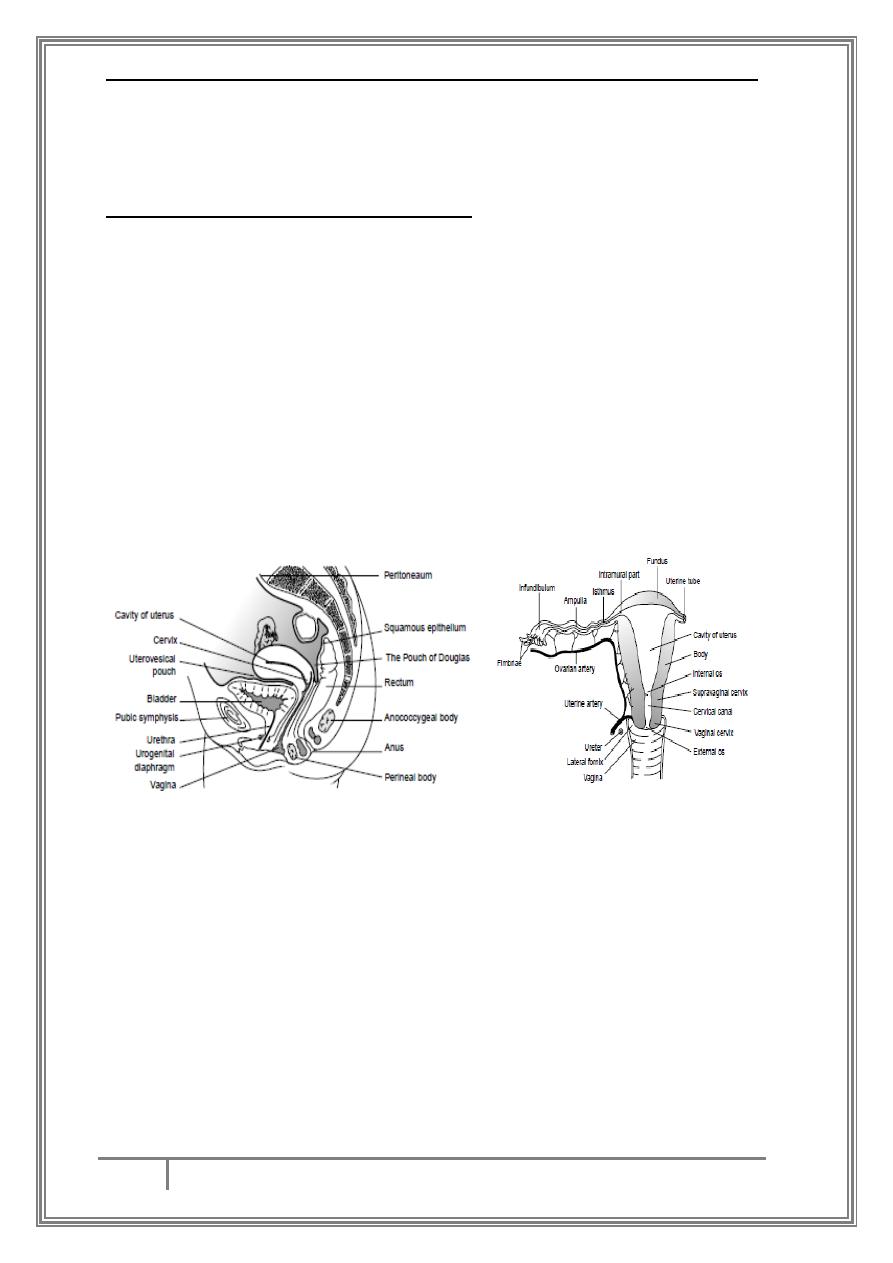
anatomy of female genital tract association between ureter and uterine artery
Postoperative complication:
Increased incidence of post partum hemorrhage.
Endometritis.
Chest infection.
Urinary tract infection.
Wound infection.
Mendelssohn's syndrome and aspiration pneumonia.
DVT and pulmonary embolism.
Increase incidence of placenta previa and placenta accreta in
subsequent pregnancies.
Delayed contact with baby.
13/3/2016
Operative Intervention in Obstetrics
Dr. Raghad
4
BY:TAHER ALI TAHER
Caesarean hysterectomy:
This is usually undertaken as a life saving procedure and as a
last resort, but should not be left too late in order to reduce
maternal morbidity and mortality.
Indications:
Uncontrollable maternal hemorrhage usually occurring
with placenta accretas.
Uncontrollable uterine atony.
Uterine rupture.
Extension of a low transverse incision.
Leiomyoma preventing uterine closure and heamostasis.
Hematomas
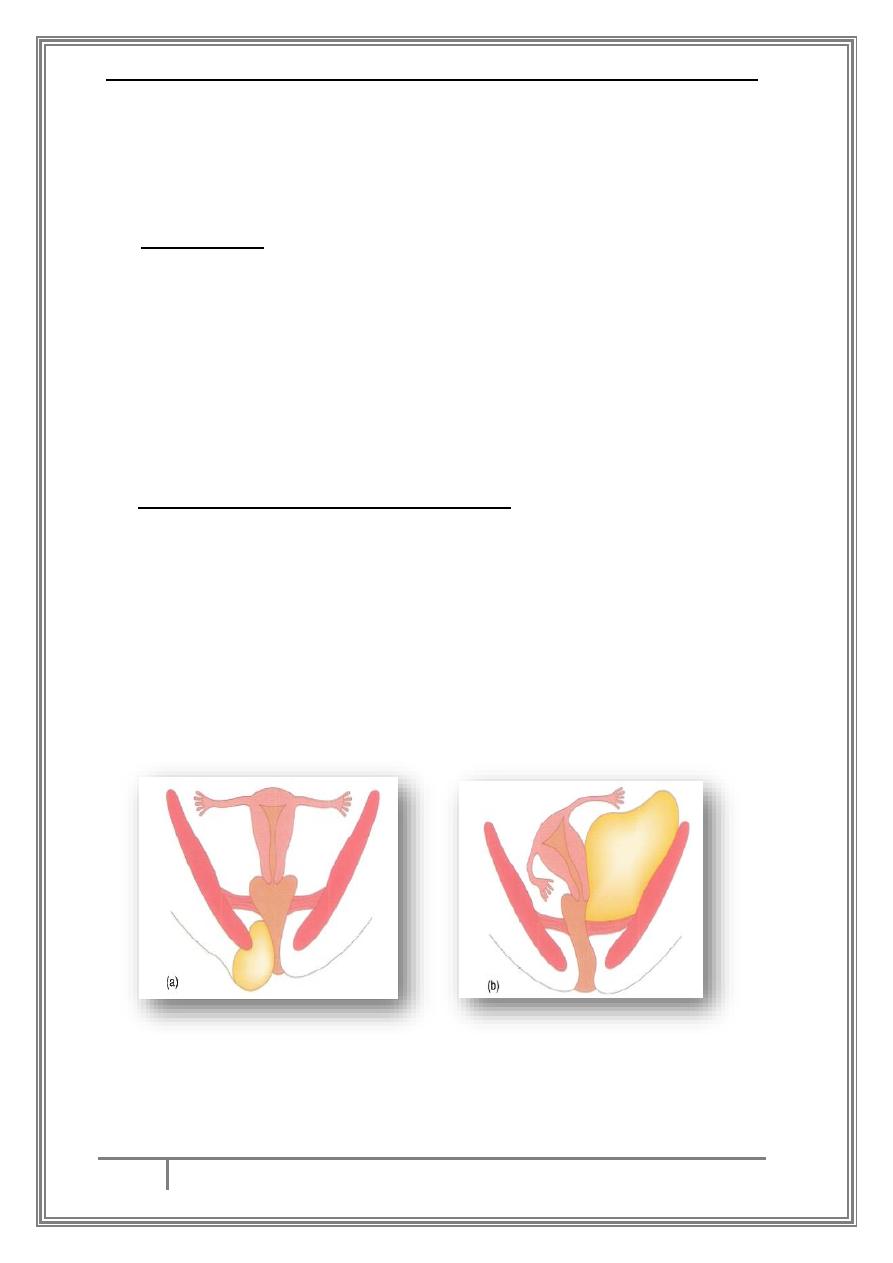
Vulval and paravaginal hematomas:
Definition:
Infra-levator hematoma: those that lie below the levator
muscle including vulval and perineal heamatomas, as well
as paravaginal hematomas and those occurring at the
ischiorectal fossa.
Supra-levator hematoma: spread upwards and outwards
beneath the broad ligament or partly downwards to bulge
into walls of the upper vagina. These also can also track
backwards into the retroperitoneal space.
(a)infra-levator hematoma, (b) supra-levator hematoma
Criteria used to define hematoma are hematomas>4cm in
diameter, the incidence is 1:1000 deliveries.
13/3/2016
Operative Intervention in Obstetrics
Dr. Raghad
5
BY:TAHER ALI TAHER
Causes:
The injury is frequently related to episiotomy, but in about 20% of
patients have intact perineum. Overall, half of the women who
develop genital hematoma do so following spontaneous delivery.
Diagnosis: although vulval hematoma is usually obvious, a
paravaginal hematoma may be missed, with no symptoms until
shock develops.
Management of infra-levator hematoma:
Management includes resuscitation and surgical evacuation.
If the hematoma<5cm and not expanding then observation
with icepacks and pressure dressing to limit its expansion,
and marking the edges of hematoma.
If hematoma>5cm or it is expanding, then surgical
evacuation is required by incising through vagina to
decrease scarring, ligation of bleeders is done. If no distinct
bleeders then a surgical drain or pack can be used.
Sub-peritoneal Hematoma:
Sub peritoneal hematomas (broad ligament) are much less
common than genital hematomas (1:20000) deliveries. They
follow spontaneous vaginal delivery, Caesarian section, or
forceps operations. More than 50 % of such hematomas are
diagnosed immediately, whereas the other half only presents
after 24 hrs. Symptoms and signs include lower abdominal
pain, vaginal bleeding, deviation of uterus to one side, and
hemodynamic instability.
Management of sub-peritoneal hematoma: a conservative
approach is recommended, with expectant management and
resuscitation. If it is not possible to maintain a stable
hemodynamic
state,
prompt
surgical
exploration
is
recommended and internal iliac artery or even hysterectomy
may be indicate.
13/3/2016
Operative Intervention in Obstetrics
Dr. Raghad
6
BY:TAHER ALI TAHER
Injuries to the cervix:
After vaginal delivery most of will have lacerations and/or
bruising of the cervix. Minor lacerations are extremely
common and not requiring suturing unless associated with
bleeding. So, bleeding that not appears to be arising from the
vagina or perineum with contracted uterus is an indication for
examining the cervix
Repair: for repairing a cervical tear, good visibility using right-
angle retractors is essential. Using two pairs of ring forceps
applied to the cervix at any one time, it is possible to inspect
the whole circumference accurately. Identification of the apex
of the tear is essential prior to repair. Deep lacerations and
particularly those involving the vaginal vault may extend to
bladder or laterally towards the uterine artery at the base of
broad ligament. Such deep lacerations need to be managed and
repaired in theatre under anesthesia.
Rarely
performed
but
important
operative
interventions:
Symphysiotomy: it is associated with subsequent maternal
morbidity such as pain in the symphysis pubis and groin.
Indication:
Cephalo-pelvic disproportion with a vertex presentation
and a living fetus (especially in rural areas when no
facilities to perform emergency C/S).
Trapped after-coming head of a breech vaginal delivery.
Last resort for shoulder dystocia.

13/3/2016
Operative Intervention in Obstetrics
Dr. Raghad
7
BY:TAHER ALI TAHER
Destructive operations:
These may be required where fetus is dead and where a vaginal
delivery is the only delivery that can be managed in that particular
situation or is the only route by which the mother wishes to be
delivered.
These include; craniotomy, perforation of the after-coming head
and decapitation.
Craniotomy: indicated for the delivery of a dead fetus with
obstructed labor in a cephalic presentation.
After-coming head: when the fetus is dead this can be managed by
craniotomy with perforation of the head through the occiput.
Where there is hydrocephalus CSF can be withdrawn by exposing
the spinal canal and passing a catheter into the canal and
decompress fetal head.
Decapitation: indicated in obstructed labor with shoulder
presentation and a dead fetus.
…THE END…
