
What are the most common causes of
Antepartum Hemorrhage ?

COMMON CAUSES
• Placenta Previa
• Placental Abruption
• Uterine Rupture
• Vasa Previa
• Bloody Show
• Coagulation Disorder
• Hemorrhoids
• Vaginal Lesion/Injury
• Cervical Lesion/Injury
• Neoplasia

Key point to Remember
• The pregnancy in which such bleeding occurs remains at
increased risk for a poor outcome even though the
bleeding soon stops and placenta previa appears to
have been excluded by sonography.

Placenta Previa
•
Defined as a placenta implanted in the lower segment
of the uterus, presenting ahead of the leading pole of
the fetus.
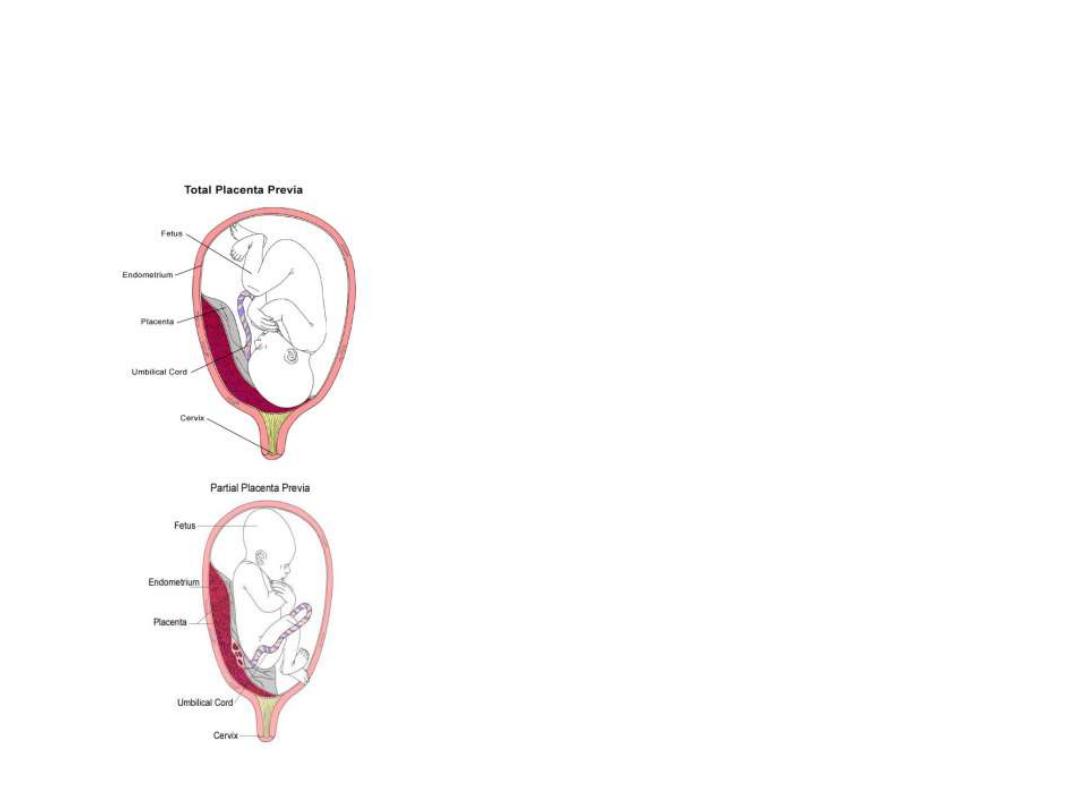
1. Total placenta previa
. The internal cervical os is covered
completely by placenta.
2. Partial placenta previa
. The internal os is partially covered by
placenta.
3. Marginal placenta previa
. The edge of the placenta is at the
margin of the internal os.
4. Low-lying placenta
. The placenta is implanted in the lower
uterine segment such that the placenta edge actually does not
reach the internal os but is in close proximity to it.
Placenta Previa
• Bleeding results from small
disruptions in the placental
attachment during normal
development and thinning of the
lower uterine segment

Placenta Previa
•
Incidence
about 1 in 300
•
Perinatal morbidity and mortality are
primarily related to the complications of
prematurity, because the hemorrhage is
maternal.

Placenta Previa
•
Etiology
:
– Advancing
maternal age
–
Multiparity
–
Multifetal gestations
–
Prior cesarean delivery
–
Smoking
– Prior placenta previa

Placenta Previa
• The most characteristic event in placenta previa
is painless hemorrhage.
• This usually occurs near the end of or after the
second trimester.
• The initial bleeding is rarely so profuse as to
prove fatal.
• It usually ceases spontaneously, only to recur.

Placenta Previa
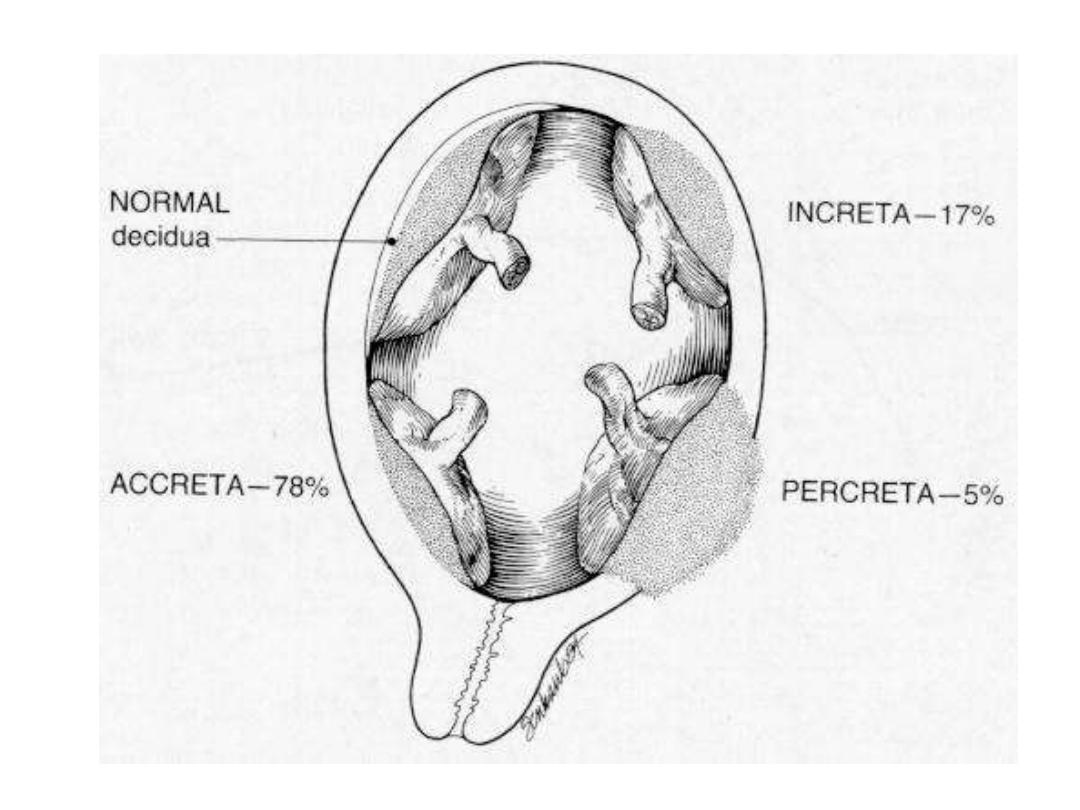
• Placenta previa may be associated with
placenta accreta
,
placenta increta
or
percreta.
• Coagulopathy is rare with placenta previa.

Placenta Previa
•
Diagnosis.
– Placenta previa or abruption should always be suspected in
women with uterine bleeding during the latter half of pregnancy.
– The possibility of placenta previa should not be dismissed until
appropriate evaluation, including sonography, has clearly proved
its absence.
– The diagnosis of placenta previa can seldom be established
firmly by clinical examination. Such examination of the cervix
is never permissible unless the woman is in an operating
room with all the preparations for immediate cesarean
delivery, because even the gentlest examination of this sort
can cause torrential hemorrhage.

Placenta Previa
• The simplest and safest method of placental localization
is provided by
transabdominal sonography.
•
Transvaginal ultrasonography
has substantively
improved diagnostic accuracy of placenta previa.
• MRI
• At 18 weeks, 5-10% of placentas are low lying. Most
‘migrate’ with development of the lower uterine segment.
Placenta Previa
Management
• Admit to hospital
•
NO VAGINAL EXAMINATION
• IV access
• Placental localization
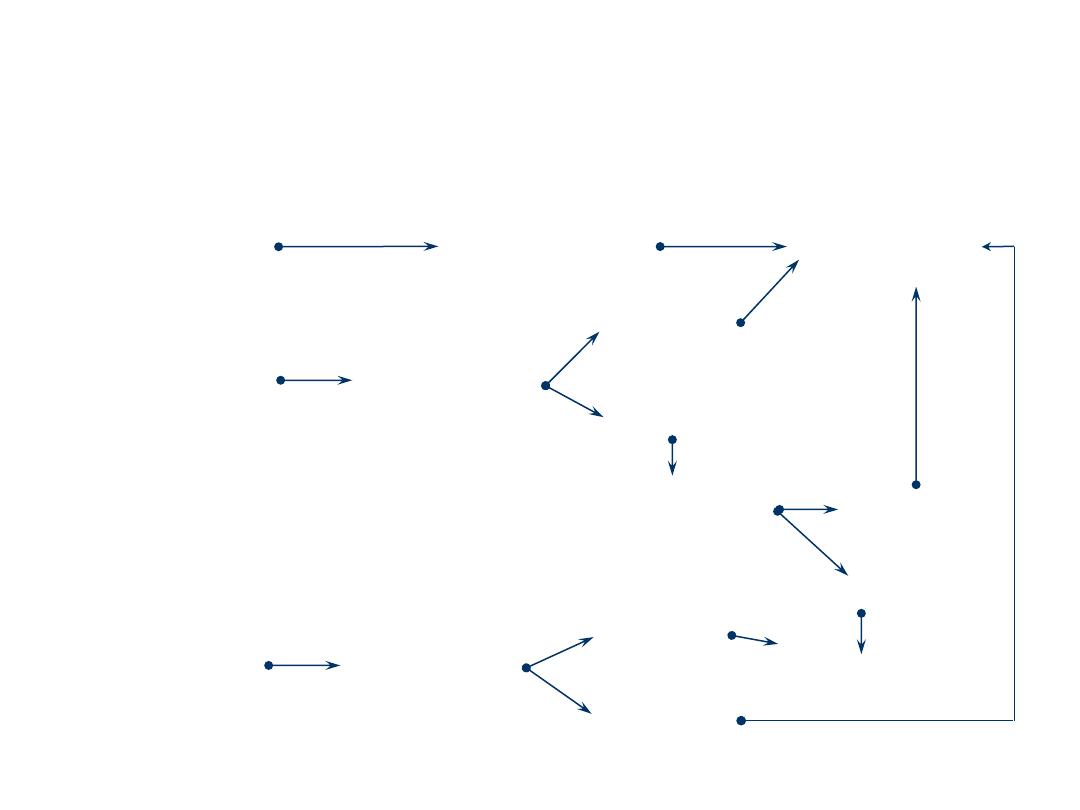
Placenta Previa
Management
Severe
bleeding
Caesarean
section
Moderate
bleeding
Gestation
>34/52
<34/52
Resuscitate
Steroids
Unstable
Stable
Resuscitate
Mild
bleeding
Gestation
<36/52
Conservative
care
>36/52

Placenta Previa
Management
• Delivery is by Caesarean section
• Occasionally Caesarean hysterectomy
necessary.

Placental Abruption
• Defined as the premature separation of the
normally implanted placenta.
• The Latin
abruptio placentae
, means "rending
asunder of the placenta
• Occurs in 1-2% of all pregnancies
• Perinatal mortality rate associated with placental
abruption was 119 per 1000 births compared
with 8.2 per 1000 for all others.
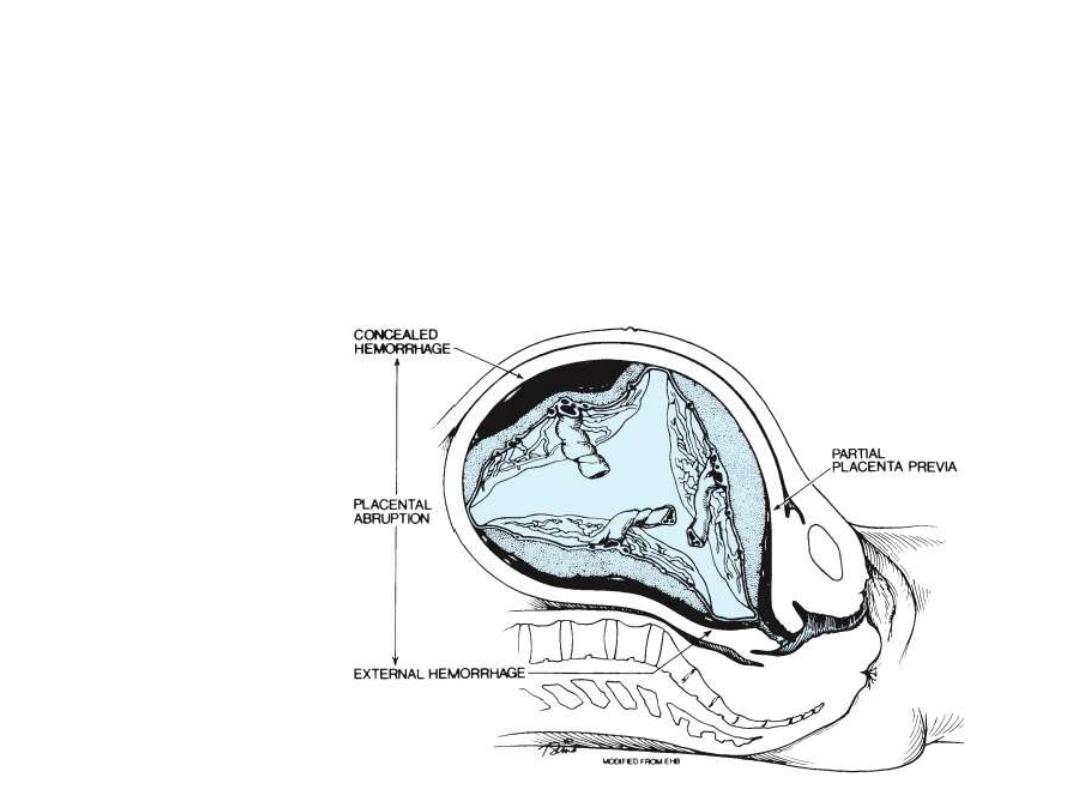
Placental Abruption
•
external hemorrhage
•
concealed hemorrhage
•
Total
•
Partial

Placental Abruption
• What are the risk factors for placental
abruption?

Placental Abruption
• Increased age and parity
• Preeclampsia
• Chronic hypertension
• Preterm ruptured
membranes
• Multifetal gestation
• Hydramnios
• Cigarette smoking
• Thrombophilias
• Cocaine use
• Prior abruption
• Uterine leiomyoma
• External trauma
The primary cause of placental abruption is unknown, but
there are several associated conditions.

Placental Abruption
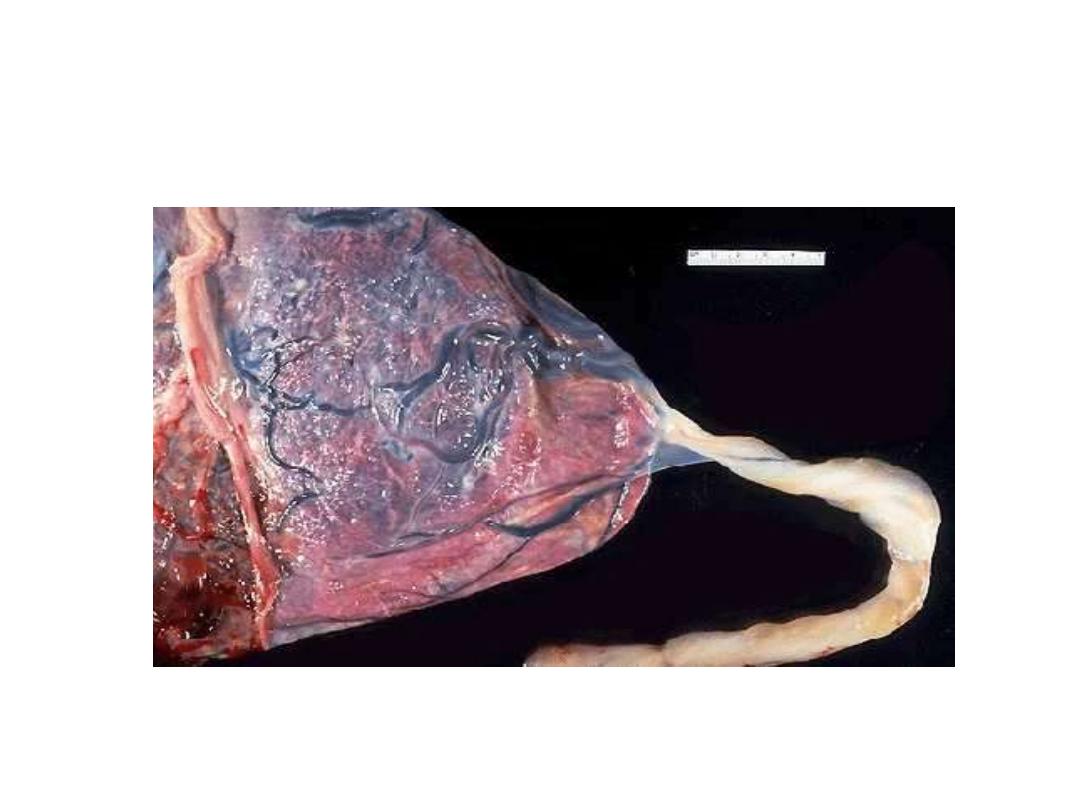
•
Pathology
– Placental abruption is initiated by hemorrhage
into the decidua basalis.
– The decidua then splits, leaving a thin layer
adherent to the myometrium.
– development of a decidual hematoma that leads
to separation, compression, and the ultimate
destruction of the placenta adjacent to it.

Placental Abruption
• Bleeding with placental abruption is almost
always maternal.
• Significant fetal bleeding is more likely to be
seen with traumatic abruption.
• In this circumstance, fetal bleeding results from
a tear in the placenta rather than from the
placental separation itself.

Placental Abruption
• The hallmark symptom of placental abruption is pain
which can vary from mild cramping to severe pain.
• A firm, tender uterus and a possible sudden increase in
fundal height on exam.
• The amount of external bleeding may not accurately
reflect the amount of blood loss.
• Importantly, negative findings with ultrasound
examination do not exclude placental abruption.
Ultrasound only shows 25% of abruptions.

Placental Abruption
•
Shock
•
Consumptive Coagulopathy
•
Renal Failure
•
Fetal Death
•
Couvelaire Uterus

Placental Abruption
•
Management:
Treatment for placental abruption varies
depending on gestational age and the status of the
mother and fetus.
– Admit
– History & examination
– Assess blood loss
• Nearly always more than revealed
– IV access, X match, DIC screen
– Assess fetal well-being
– Placental localization

Uterine Rupture
• Reported in 0.03-0.08% of all delivering women, but
0.3-1.7% among women with a history of a uterine
scar (from a C/S for example)
• 13% of all uterine ruptures occur outside the
hospital
• The most common maternal morbidity is
hemorrhage
• Fetal morbidity is more common with extrusion

Uterine Rupture
• Classic presentation includes vaginal bleeding,
pain, cessation of contractions, absence/
deterioration of fetal heart rate, loss of station of
the fetal head from the birth canal, easily
palpable fetal parts, and profound maternal
tachycardia and hypotension.
• Patients with a prior uterine scar should be
advised to come to the hospital for evaluation of
new onset contractions, abdominal pain, or
vaginal bleeding.

What are the risk factors
associated with uterine rupture?
Uterine Rupture
• Excessive uterine
stimulation
• Hx of previous C/S
• Trauma
• Prior rupture
• Previous uterine surgery
• Multiparity
• Non-vertex fetal
presentation
• Shoulder dystocia
• Forceps delivery

Uterine Rupture
• Management: Emergent laparotomy

Vasa Previa
• Rarely reported condition in which the fetal
vessels from the placenta cross the entrance to
the birth canal.
• Incidence varies, but most resources note
occurrence in 1:3000 pregnancies.
• Associated with a high fetal mortality rate (50-
95%) which can be attributed to rapid fetal
exsanguination resulting from the vessels
tearing during labor

Vasa Previa
•
There are three causes typically noted
for vasa previa:
1. Bi-lobed placenta
2. Velamentous insertion of the umbilical cord
3. Succenturiate (Accessory) lobe
Vasa Previa

Vasa Previa

Vasa Previa
• Risk Factors:
– Bilobed and succenturiate placentas
– Velamentous insertion of the cord
– Low-lying placenta
– Multiple gestation
– Pregnancies resulting from in vitro fertilization
– Palpable vessel on vaginal exam

Vasa Previa
• Management:
– When vasa previa is detected prior to labor, the baby
has a much greater chance of surviving.
– It can be detected during pregnancy with use of
transvaginal sonography.
– When vasa previa is diagnosed prior to labor, elective
caesarian is the delivery method of choice.

Kleihauer-Betke Test
• Is a blood test used to measure the
amount of fetal hemoglobin transferred
from a fetus to the mother's bloodstream.
• Used to determine the required dose of Rh
immune globulin.
• Used for detecting fetal-maternal
hemorrhage.

Apt test
• The test allows the clinician to determine whether the
blood originates from the infant or from the mother.
– Place 5 mL water in each of 2 test tubes
– To 1 test tube add 5 drops of vaginal blood
– To other add 5 drops of maternal (adult) blood
– Add 6 drops 10% NaOH to each tube
– Observe for 2 minutes
– Maternal (adult) blood turns
yellow-green-brown;
fetal blood
stays
pink.
– If fetal blood, deliver STAT.

Initial management of APH
• Admit
• History
• Examination
•
NO PV
• Nurse on side
• IV access/ resuscitate
• Clotting screen
• Cross match
• Kleihauer-Betke test
• Apt test
• CTG
• Observation
• Placental localization
• Speculum examination
when placenta previa
excluded
• Anti-D if Rh-negative

Diagnosis of Antepatrm Hemorrhage
• Painless vaginal bleeding after 24w.?
• Symptoms and sings:
-shock -bleeding may be precipitated by
intercourse
-relaxed uterus -normal fetal condition
-fetal presentation not in the pelvis/ lower uterine
pole feels empty.
• Dg: Placenta previa

• Vaginal bleeding after 24 w,intermitent,or
constant abdominal pain?
• Symptoms and sings:
-Shock -tense/tender uterus
-decreased /absent fetal movements.
-fetal distress/absent fetal heart sound.
Dg: Abruptio placentae.
( R/O co-exciting PIH)
• Bleeding(intra-abdominal and/or vaginal)?
• Sever abdominal pain(may decreas after
rupture)?
• Previous uterine scar?
- shock -abdominal distention/free fluid.
-abnormal uterine contour -tender abdomin
-easily palpable fetal parts -rapid maternal puls
-absent fetal movements and FHS
Dg: Ruptured uterus

• Mild vaginal bleeding after 24 w(mild)?
• Symptoms and sings:
-clinically stable
-fetal assessment showed fetal distress
that can not be explained by the mild bleeding.
Dg : Vasa previa

Complications of placenta previa
-shock
-postpartum hemorrhage
- Women with placenta previa are at high
risk for PPH and placenta accreta/increta;
a common finding is at the site of a
previous cesarean section

Complications of abruptio placentae
• Maternal shock
• Fetal death
• Uterine atony
• Amniotic fluid embolism
• Caogulopathy( 30%)
• Renal failure
The principal cause of maternal death is renal
failure due to prolonged hypotension .
Don not underestimate the amount of the
hemorrhage

Management
• General rules:
-call for help
-remember that mother and the neonate
require evaluation and intervention if needed

First aid management
• Insert 2 wide bore cannulae
• Blood for CBC,crossmatch
• Immediately star iv crystalloid solutions
• Provide 100% oxygen via mask
• Warm the women
• Insert Foley catheter
• Monitor blood pressure and pulse/ 5 min
• Monitor urine output /hour

Indications of when to terminate
pregnancy
• Women in labour
• Bleeding is heavy(evidente or hidden)
manifested by shock
• Gestational age equals or more 37 w
• There is fetal distress
• There is IUFD and /or fatal congenital
anomalies by US

When to use conservative management
• Bleeding is light or has stopped AND
• The fetus is alive AND
• The fetus is premature.
• Cases of abruptio placentae which are
diagnosed only on US examination, with
no clinical finding( no bleeding, no shock,
no tender or tonically contracted uterus)

In abruptio placentae:
• When the clinical diagnosis is clear
• Or in the presence of acute fetal
distress:…. Do not waste your time for US
examination.
• US is neither sensitive nor specific
diagnosis modality in abruptio placentae
50
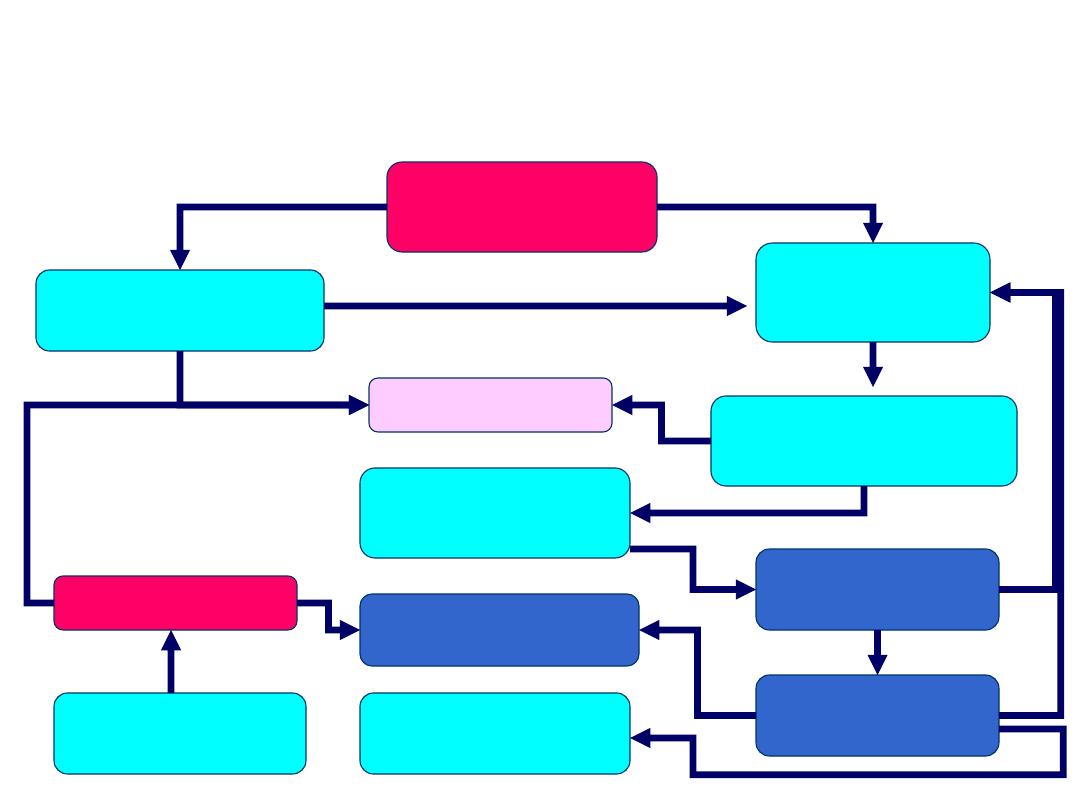
Placental
migration
Bleeding
C/Section
Expectant
management
Management of Placenta praevia in a
Pregnancy of viable gestational age
Fetal distress
Bleeding
Fetal lung maturity
Sono assessment
q 3-4 weeks
Complete
resolution
Trial of labor
(low-lying only)
Double set-up
Trial of labor
+
-
-
+
+
-
+
- -
+
+
-
