
Epidemiology of Chronic
Obstructive Pulmonary
Disease (COPD)
Asst Prof Dr Faris Al Lami
MBChB MSc PhD FFPH

Objectives
At the end of this lecture the student should be
able to:
•
Define COPD
•
Identify the Global burden of COPD
•
Identify the risk factors of COPD
•
Define methods of diagnosing COPD at
population level
•
Identify preventive methods

•
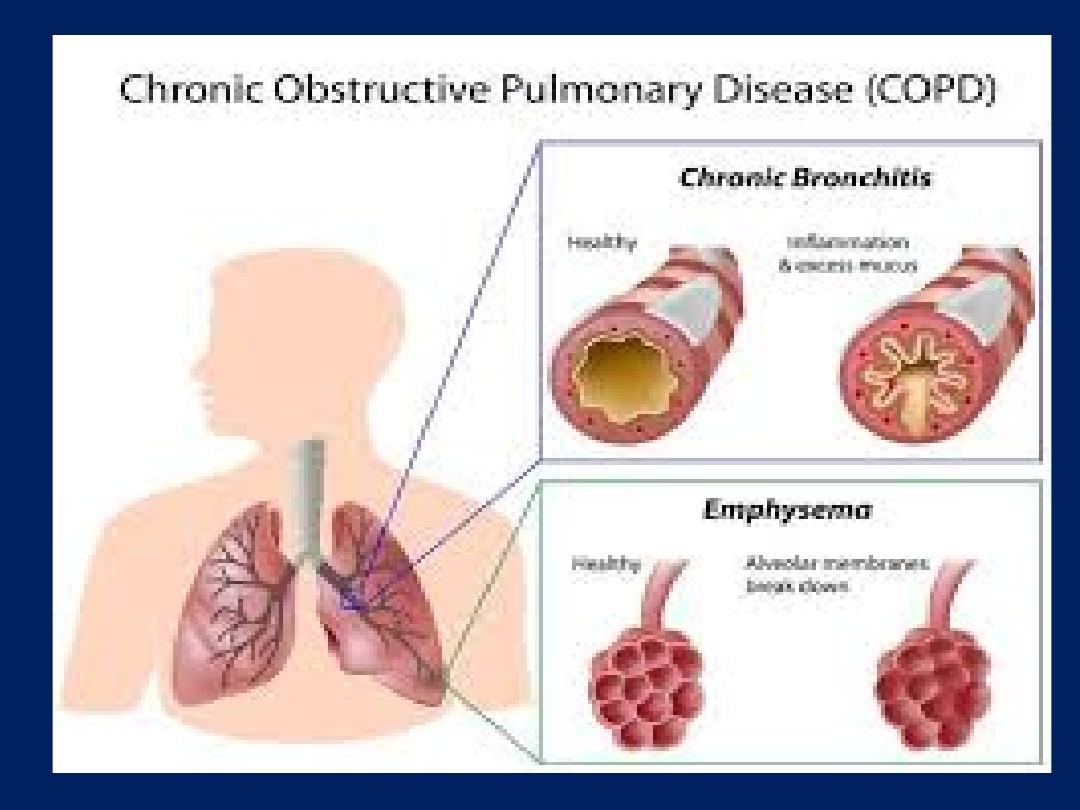
WHO define COPD as a lung ailment characterized by a
persistent blockage of airflow from the lungs
•
COPD is a mixture of small airways disease (chronic
bronchitis) and parenchymal destruction (emphysema)
•
COPD is:
Life-threatening
Progressive
Not fully reversible
Under-diagnosed lung disease
But
Preventable and Treatable

•
A clinical symptoms of COPD are: dyspnea, chronic
cough and sputum production for at least 3 months in
each of two consecutive years
•
Diagnosis is confirmed by Spirometry via the presence
of a
post-bronchodilator FEV1/FVC% < 70%

•
Worldwide, COPD remains a major public health problem
•
It is one of the 10 leading causes of mortality
•
It is projected to rank the
5
th
leading cause of death in
2020
•
In terms of Disability Adjusted Life Years, (DALYs), COPD
ranks
13
th
•
COPD kills on average one person every 10 seconds.
•
COPD burden projected to increase because of continued
exposure to risk factors and population aging

•
COPD encompasses:
o
Chronic obstructive bronchitis
(with
obstruction of small airways) and
o
Emphysema
(with enlargement of air
spaces and destruction of lung
parenchyma, loss of lung elasticity, and
closure of small airways)

•
Most patients with COPD have all 3 pathologic
conditions:
Chronic obstructive bronchitis
Emphysema
Mucus plugging
•
The relative extent of emphysema and obstructive
bronchitis within individual patients can vary
Epidemiology
•
Available information on COPD comes from developed
countries.
•
Accurate epidemiologic data on COPD are difficult and
expensive to collect
•
COPD Morbidity and Mortality are underestimated
because:
The disease is usually not diagnosed until it is clinically
apparent and moderately advanced.
The imprecise and variable definitions of COPD
COPD is more likely to be cited as a contributory than
an underlying cause of death, or may not be cited at
all.
Prevalence
The worldwide prevalence of COPD in 2002 was:
11.6/1,000 in men and 8.77/1,000 in women in all ages
Prevalence is Higher in:
–
Older adults
–
Countries where cigarette smoking is very common
–
Men than women
•
COPD is responsible for a significant part of
physician visits, emergency department visits,
hospitalizations and significant % of YLD
Risk Factors
•
Host Factors
1. Genes
•
Many genetic factors increase (or decrease) a person's
risk of developing COPD as of 1-α antitrypsin deficiency
2. Airway hyperresponsiveness
•
A complex disorders related to a number of genetic and
environmental factors
•
May develop after exposure to tobacco smoke or other
environmental insults

3. Lung Growth
•
Related to processes occurring during gestation, birth
weight, and exposures during childhood.
•
Reduced maximal attained lung function identify
individuals at increased risk for COPD
4. Sex
•
COPD prevalence and mortality were greater among
men than women, the difference getting narrower
(probably reflects changing patterns of tobacco smoking.
Exposures
1. Tobacco smoke
Cigarette smokers have a higher prevalence of:
Lung-function abnormalities
Respiratory symptoms
Greater annual rate of decline in FEV1
Higher death rates for COPD

•
Passive smoking may contribute to COPD by
increasing lungs' total burden of inhaled
particulates and gases.
•
Pipe and cigar smokers have more COPD than
non-smokers
•
Not all smokers develop COPD (Genetic factors
must modify each individual's risk)
•
Smoking during pregnancy may pose a risk for
the fetus, by:
Affecting lung growth and development in utero
Priming of the immune system.
2. Occupational dusts and chemicals
•
Intense or prolonged occupational dusts and
chemicals exposures (vapours, irritants, fumes)
can increase COPD risk (independent of cigarette
smoking).
•
Exposure to particulate matter, irritants, organic
dusts, and sensitizing agents can increase airway
hyperresponsiveness, especially in airways
already damaged by other occupational
exposures, cigarette smoke, or asthma.

3. Outdoor and indoor air pollution
•
High levels of urban air pollution are harmful to
persons with existing heart or lung disease.
•
Indoor air pollution from biomass fuel, burned for
cooking and heating in poorly vented dwellings, is a
risk factor for COPD.
•
The role of outdoor air pollution is unclear, but
appears to be small when compared with cigarette
smoking.

4. Infections
•
A history of severe childhood respiratory infection
has been associated with reduced lung function and
increased respiratory symptoms in adulthood.
5. Socioeconomic status
•
Inverse association with socioeconomic status.
•
It may reflects exposures to indoor and outdoor air
pollutants, crowding, poor nutrition, or other factors
related to socioeconomic status
Diagnosis
•
COPD should be considered in any patient with cough,
sputum production, or dyspnea and/or a history of
exposure to risk factors for the disease.
•
Diagnosis confirmed by: spirometry which measures
lung function and capacity.
•
Post-bronchodilator FEV1/FVC% < 70%
•
Chronic cough and sputum production often precede
the development of airflow limitation by many years
•
Not all individuals with cough and sputum production go
on to develop COPD.

•
Poorly reversible airflow limitation associated with other
diseases such as bronchiectasis, cystic fibrosis,
tuberculosis, or asthma
•
A low peak flow is consistent with COPD, but may not be
specific to COPD (other lung diseases and poor
performance during testing)
•
In many developing countries both TB and COPD are
common.
•
In all subjects with symptoms of COPD, TB should be
considered, especially in endemic areas.

Management
An effective COPD management plan includes
four components:
1) Assess and Monitor Disease
2) Reduce Risk Factors
3) Manage Stable COPD
4) Manage Exacerbations
Prevention
•
Avoidance of cigarette smoking or exposure to second hand
cigarette smoke
•
Eliminating occupational or vocational exposures that can
worsen lung function.
•
Because of the strong familial component of COPD, evaluating
children and siblings of never-smoking COPD patients may
provide opportunities for early intervention
•
Patients with asthma are at risk for developing COPD.
Monitoring of lung function and aggressive treatment of
underlying condition are recommended.

•
Pneumonia and influenza vaccines should be
given to COPD patients.
•
Those with COPD should also live a healthy
lifestyle by:
Exercising
Avoiding cigarette smoke and other air pollutants
Eating well
Pulmonary Rehabilitation

Qs
