Dr. Nadia Aziz
C.A.B.C.M.
Department of community medicine
Medical college, Baghdad University

1-Define what is food intoxication.
2-describe types of food poisoning.
3-discuss clinical features, diagnosis, occurrence &
measures of control of food intoxication.
Including foodborne
intoxications
and foodborne
infections
, are terms applied to illnesses acquired
through
consumption of contaminated food
also include those caused by
chemical contaminants
such as heavy metals and organic compounds.
The more frequent causes are:
1)
Toxins
elaborated by bacterial growth
in the food
before consumption
Like : Clostridium botulinum, Staphylococcus aureus and
Bacillus cereus
or in the
intestines
Clostridium perfringens
2) bacterial, viral, or parasitic infections (brucellosis,
Escherichia coli, hepatitis A, salmonellosis and infection
with vibrios etc…)
3) toxins produced by harmful
algal
species (ciguatera
fish poisoning, paralytic, neurotoxic, diarrhoeic or
amnesic shellfish poisoning).
Foodborne disease outbreaks are recognized by the
occurrence of
illness within usually
short time period
(a few hours to a
few weeks)
after a meal, among
individuals who have consumed
foods in common.
Prompt and thorough
laboratory evaluation
of cases
and implicated foods is essential.
Single cases of foodborne disease are
difficult to
identify
unless, as in botulism, there is a
distinctive
clinical syndrome
.
Ultimately, prevention depends on
educating food
handlers
about proper practices in cooking and
storage of food and personal hygiene.
1. Keep Clean.
2. Separate raw and cooked.
3. Cook thoroughly.
4. Keep food at safe temperatures.
5. Use safe water and raw materials.
An intoxication (not an infection) of
abrupt
severe
nausea
,
vomiting , cramps,
and
prostration,
often accompanied by diarrhea and sometimes with
subnormal temperature and lowered blood pressure.
Deaths are
rare
illness commonly lasts only a day or two
In outbreak:
Recovery of staphylococci (10
5
/g of food) on
culture
media
Detection of
enterotoxin
from food item.
Absence of staphylococci on culture from heated food
does not rule out the diagnosis
A
Gram stain
of the food may disclose the organisms
that have been heat killed.
Isolation of organisms from
stools
or
vomitus
of 2 or
more ill persons
Several enterotoxins of Staphylococcus aureus,
stable at
boiling temperature.
Staphylococci produce the toxins at levels of water
activity too low for the growth of many bacteria.
Occurrence
About
25%
of people are
carriers
of this pathogen.
Reservoir
Humans
in most instances; occasionally
cows
with
infected udders, as well as dogs and fowl.
Ingestion
of a food containing staph enterotoxin like
salad dressings
, sandwiches,
meat
products & cheese.
When these foods remain at room temperature for
several hours before being eaten, toxin-producing
staphylococci multiply and elaborate the
heat-stable
toxin.
Organisms may be of
human origin
from purulent
discharges of an infected finger or eye, abscesses, acne
form eruptions, nasopharyngeal secretions,
or of
bovine origin
, such as contaminated milk or milk
products, especially cheese.
Incubation period
30 minutes
to 8 hours, usually
2–4 hours
.

A. Preventive measures:
1)
Educate
food handlers about:
(a) Strict food
hygiene
,
sanitation
and cleanliness of
kitchens, proper
temperature control
, hand washing,
cleaning of fingernails
(b) The
danger
of working with exposed skin, nose or
eye
infections
and uncovered wounds.

2)
Reduce food-handling time
(from initial preparation to
service), no more than 4 hours at ambient temperature.
(above 60°C) or cold (below 4°C) in shallow containers and
covered.
3) Temporarily
exclude people
with boils, abscesses and
other purulent lesions of hands, face or nose from food
handling.

B. Control of patient, contacts and the immediate
environment:
1) Report to local health authority: Class 4.
Control is of outbreaks, single cases are rarely identified.
2) Specific treatment: Fluid replacement when indicated
An
intestinal
disorder characterized by sudden onset of
colic
followed by
diarrhea
,
nausea
is common.
Generally a mild disease of
short duration
, 1 day or less,
rarely fatal
in healthy people.
Outbreaks of severe disease with
high case-fatality
rates
associated with a
necrotizing enteritis
In outbreak :
Diagnosis is confirmed by demonstration of
Clostridium perfringens in anaerobic
cultures
of
food
(10
5
/g) or patients’
stool
(10
6
/g).
Detection of
enterotoxin
in patients’ stool also confirms
the diagnosis.
Infectious agent
Type A strains
of C. perfringens (C. welchii)
cause typical food poisoning outbreaks
Type C strains
cause necrotizing enteritis.
Reservoir
GI tract of healthy people and animals (cattle, fish,
pigs and poultry).

Ingestion
of food containing soil or feces and then held
under conditions that permit multiplication of the
organism.
Almost all outbreaks are associated with inadequately
heated or reheated
Meats.
Spores survive normal cooking temperatures
Incubation period
From
6
-
24
hours, usually 10–12 hours.
An intoxication characterized by:
sudden
onset of
nausea
and
vomiting
in others by
colic
and
diarrhea
.
Illness generally persists
no longer than 24 hours
and
is rarely fatal.
In outbreak, diagnosis is confirmed through
cultures
of suspected
food
(more than 10
5
- 10
6
organisms per
gram of food).
Enterotoxin
testing is valuable but may
not be widely
available.
Bacillus cereus, an
aerobic spore
former.
Two enterotoxins have been identified:
1-Heat stable
causing
vomiting
, is produced in food
when B. cereus levels reach 10
5
colony /g of food.
2-Heat labile
causing
diarrhea
, formed in the small
intestine of the human host.
Reservoir
A
ubiquitous
organism in soil and environment
Mode of transmission
Ingestion
of food kept at ambient temperatures after
cooking.
Outbreaks associated with vomiting have been most
commonly associated with
cooked rice
.
Incubation period
From
0.5
to
6
hours in cases where
vomiting
is the
predominant symptom
From
6
to
24
hours where
diarrhea
predominates.
Preventive measures
:
Foods
should not remain at ambient temperature after
cooking
Human botulism is a
serious
but
relatively rare
intoxication caused by potent
preformed toxins
produced by Clostridium botulinum.
There are 3 forms of botulism:
1- foodborne (the classic form)
2-wound
3-intestinal (infant and adult) botulism.
All types share the
flaccid paralysis
that results from
botulinum neurotoxin.
Foodborne botulism is a
severe
intoxication resulting
from ingestion of
preformed toxin
present in
contaminated food.
The characteristic early symptoms and signs are:
Marked fatigue, weakness
and
Vertigo
, usually followed by
Blurred vision
,
dry mouth
, and difficulty in swallowing
and speaking.
Vomiting
, diarrhea, constipation and abdominal swelling
may occur.
Neurological symptoms
always
descend
through the body
Paralysis
of breathing muscles can cause loss of breathing
and death.
There is no fever and no loss of consciousness.
The case-fatality rate is
5%–10%.
Infant botulism has in some cases been associated with
ingestion of honey
contaminated with botulism spores.
It may cause an estimated
5%
of cases of
sudden infant
death syndrome (SIDS).
demonstration of botulinum
toxin
in
serum
,
stool
,
gastric
aspirate
or
incriminated food
, or through
culture
of C.
botulinum from
gastric aspirate
or
stool
of the patients
Clostridium botulinum, a
spore-forming anaerobic
bacillus, isolated from soil, seafood and meat from
marine mammals.
Toxin is produced in
canned
, low acid or alkaline foods.
Toxin is
destroyed by boiling
Reservoir
Spores,
ubiquitous
in soil, honey & in the intestinal
tract of animals.
Incubation period
usually within
12–36
hours
1) Report to local health authority: Class 2
2) Specific treatment: Intravenous administration of 1
vial of polyvalent (AB or ABE) botulinum
antitoxin
as
soon as possible,
Antibiotics
do not improve
the course of the disease.
A bacterial disease manifested by:
Acute
enterocolitis
,
headache
,
abdominal pain
,
diarrhea
,
nausea
and sometimes
vomiting
.
Dehydration
, especially among infants or in the elderly,
may be severe.
Fever
is almost always present.
Deaths are uncommon, except in the very
young
, the very
old,
the
debilitated
and the
immunosuppressed
.
Salmonella isolated from
feces
during acute stages of
enterocolitis.
In the recently proposed nomenclature for Salmonella
the agent formerly known as S. typhi is called S.
enterica
Salmonella enterica serovar Typhimurium (commonly
S.
Typhimurium
) and
Salmonella enterica serovar Enteritidis (
S. Enteritidis
)
are the most commonly reported
Occurrence
Worldwide,
contaminated food
, mainly of
animal
origin
, is the predominant mode of transmission.
The incidence rate of infection is highest in infants and
young children.
person-to-person spread can also occur
Reservoir
Domestic
and
wild
animals, including poultry, swine, cattle,
rodents and pets such as iguanas, turtles, chicks, dogs and
cats; also humans, i.e. patients,
convalescent carriers
Chronic carriers are rare in humans
but prevalent in animals and birds.
Ingestion
of the organisms in food from
infected animals
or
contaminated by feces
of an infected animal or
person. This includes
eggs
, raw
milk
, contaminated
water,
meat
& poultry.
Maternity units with infected (at times
asymptomatic
)
infants, are sources of further spread.
Incubation period
From
6
to
72
hours, usually about 12–36 hours.
Period of communicability
Throughout the course of infection.
A temporary carrier
state occasionally continues for
months, especially in infants.
Increased by:
Achlorhydria
, antacid treatment, gastrointestinal surgery,
broad-spectrum antibiotherapy, neoplastic disease,
immunosuppressive treatment and other
debilitating
conditions
including malnutrition.

A. Preventive measures:
1) Educate all food handlers about the ways of proper
preparation & handling of food.
2)
Exclude individuals with diarrhea from food
handling
and from care of hospitalized patients, the
elderly and children.
Specific treatment:
rehydration
and electrolyte replacement Antibiotics may
not eliminate the carrier state
ciprofloxacin
is highly effective ampicillin or amoxicillin
may also be used.
Patients infected with
HIV may require lifelong treatment
to prevent Salmonella septicemia.
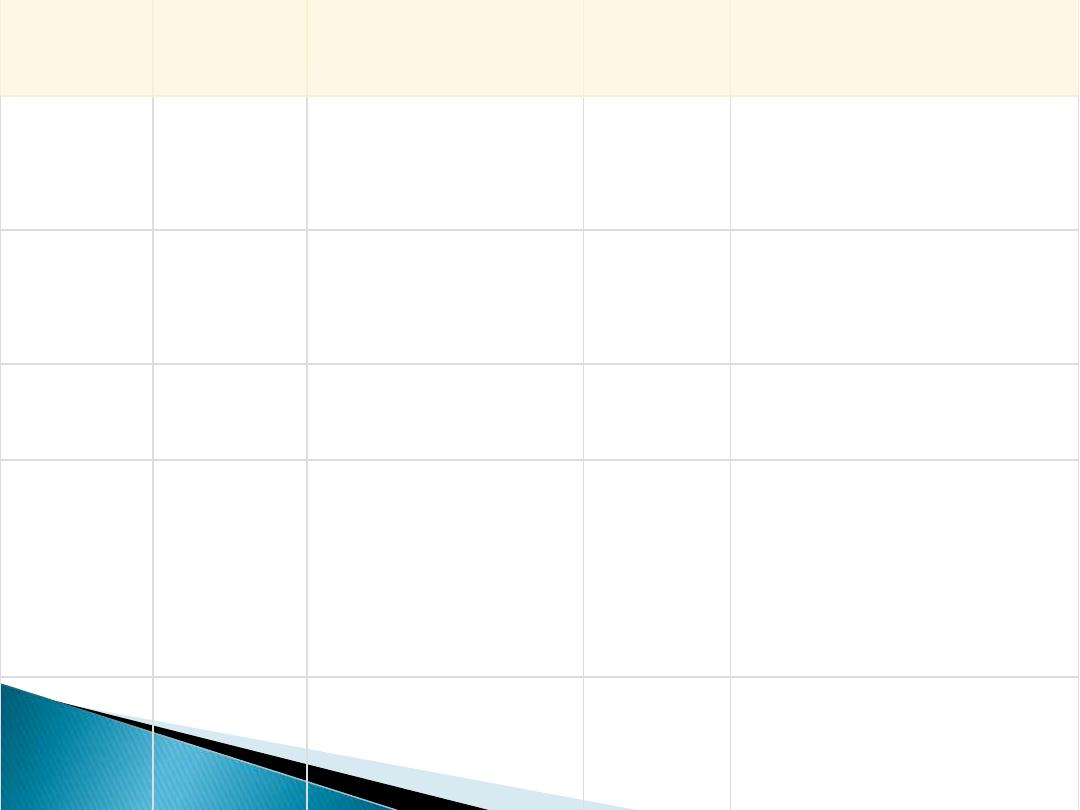
Organism
Incubation
period
Signs & Symptoms
Duration
Food Sources
Staphyloco
ccus aureus
30 min- 8
hrs
Sudden onset of
severe nausea and
vomiting.
24-48
hours
meats, egg, salads, cream
pastries
Clostridium
perfringens
8–24 hours Intense abdominal
cramps, watery
diarrhea
24
hours
Meats, poultry
Bacillus
cereus
6 -24 hrs
Abdominal cramps,
watery diarrhea,
24-48
hours
Cooked rice
Clostridium
botulinum
12-36
hours
Vomiting, diarrhea,
blurred vision,
muscle weakness,
respiratory failure
and death
Variable
Improperly canned foods,
especially home-canned
vegetables
Salmonella 6-72 hours Diarrhea, fever,
abdominal cramps,
vomiting
4-7 days
Eggs, poultry, meat,
unpasteurized milk or
juice, cheese

Thank you
&
Good Luck
