PATHOLOGY OF THE REPIRATORY
SYSTEM
part I
OBJECTIVES:
By the end of these series of lecture on respiratory system pathology the students
would be able to:
1- define the pathogenesis and the pathological features of the most common tumor
like and tumor (benign and malignant) conditions of the upper respiratory tract
including: allergic nasal polyp, angiofibroma, nasopharyngeal carcinoma, laryngeal
tumors including: vocal cord nodule, laryngeal papilloma and laryngeal carcinoma.
2- describe atelectasis of the lung and its classification.
3- define adult respiratory distress syndrome and its causes and pathological features.
4- define (the pathogenesis and the pathological features) and list obstructive
pulmonary disease: asthma, emphysema, chronic bronchitis and broncheactasis.
5- describe the pathogenesis, types and pathological features of diffuse interstitial
lung diseases.
6- define and list the granulomatous lung diseases.
7- identify the pathogenesis and pathological features of pulmonary infections.
8- outline the pathogenesis and the pathological features of pulmonary tuberculosis.
9- list and classify the most important lung tumors describing the pathogenesis and
pathological features, with clinical presentations including paraneoplastic syndrome
descriptions.
10- define diseases of the pluera and list the most common neoplasms of the pleura.
THE UPPER RESPIRATORY
TRACT
Allergic nasal polyp
Not true neoplasms. They are associated with inflammation
and allergy. Generally, they are multiple (bunch of grapes),
and nearly always bilateral.
Microscopically:
composed of loose mucoid stroma and mucous glands
covered by respiratory epithelium which often shows foci of
squamous metaplasia. They are infiltrated by lymphocytes,
plasma cells, mast cells, neureophils and eosinophils.
Benign tumors of the Nose and Nasal Cavity:
ANGIOFIBROMA
It occurs almost exclusively in males.
It is androgen dependent.
It presents as polypoidal mass that bleeds severely on
manipulation.
Microscopically:
Composed of matrix of blood vessels and fibrous tissue stroma
which may be loose and edematous or dense acellular and highly
collagenized.
The vessels range from capillary size which are particularly
common at the growing edge of the tumor, they have got plump
endothelial cells.
Larger venous size vessels are located at the base of the lesion.
Malignant Tumors:
NASOPHARYNGEAL CARCINOMA
This rare neoplasm has a strong epidemiologic links to
EBV
& a high
frequency in
China
.
These facts raise the possibility of
viral oncogenesis
on a background of
genetic susceptibility.
The cancers are either
squamous cell carcinoma
(keratinizing or
nonkeratinizing) or
undifferentiated carcinoma
. The latter is the most
common and the one most closely linked with EBV.
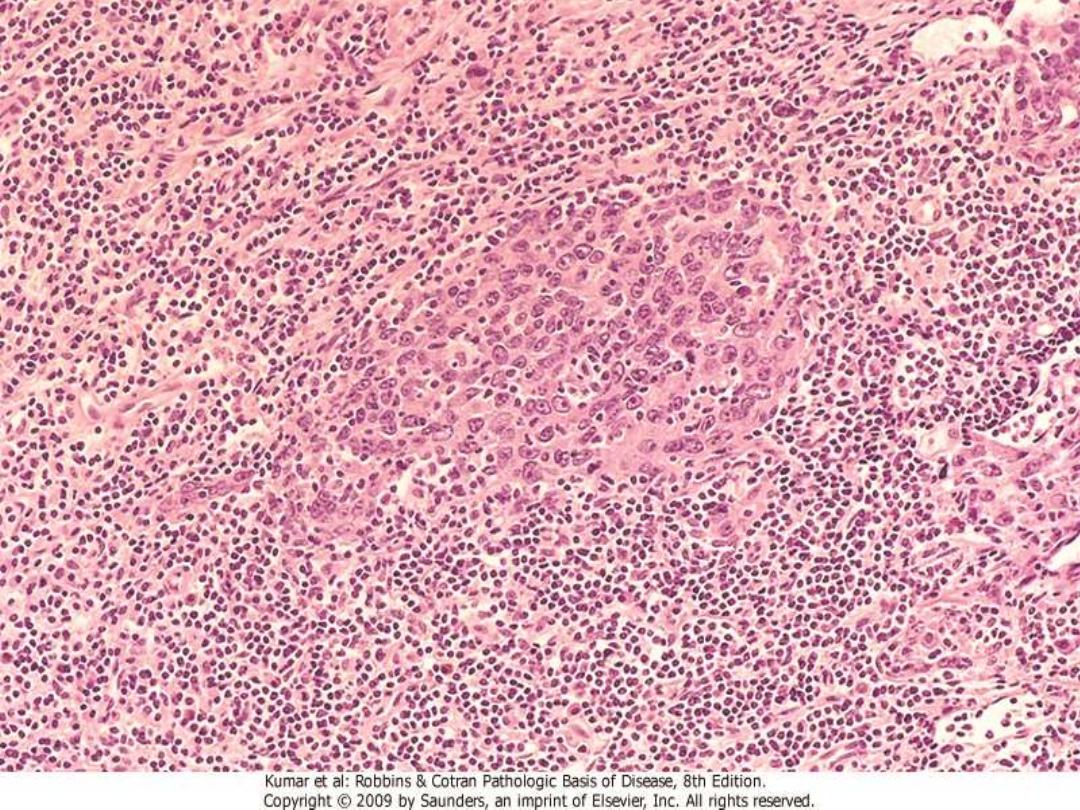
In nasopharyngeal carcinomas a striking infiltration of mature
lymphocytes can often be seen. These neoplasms are therefore referred
to as
"lymphoepitheliomas,"
although the lymphocytes are not part of
the neoplastic process.
Nasopharyngeal carcinomas invade locally, spread to cervical lymph
nodes, and then metastasize to distant sites.
They are, however,
radiosensitive
, and 5-year survival rates of 50% are
reported for even advanced cancers.
LARYNGEAL TUMORS
Benign Lesions
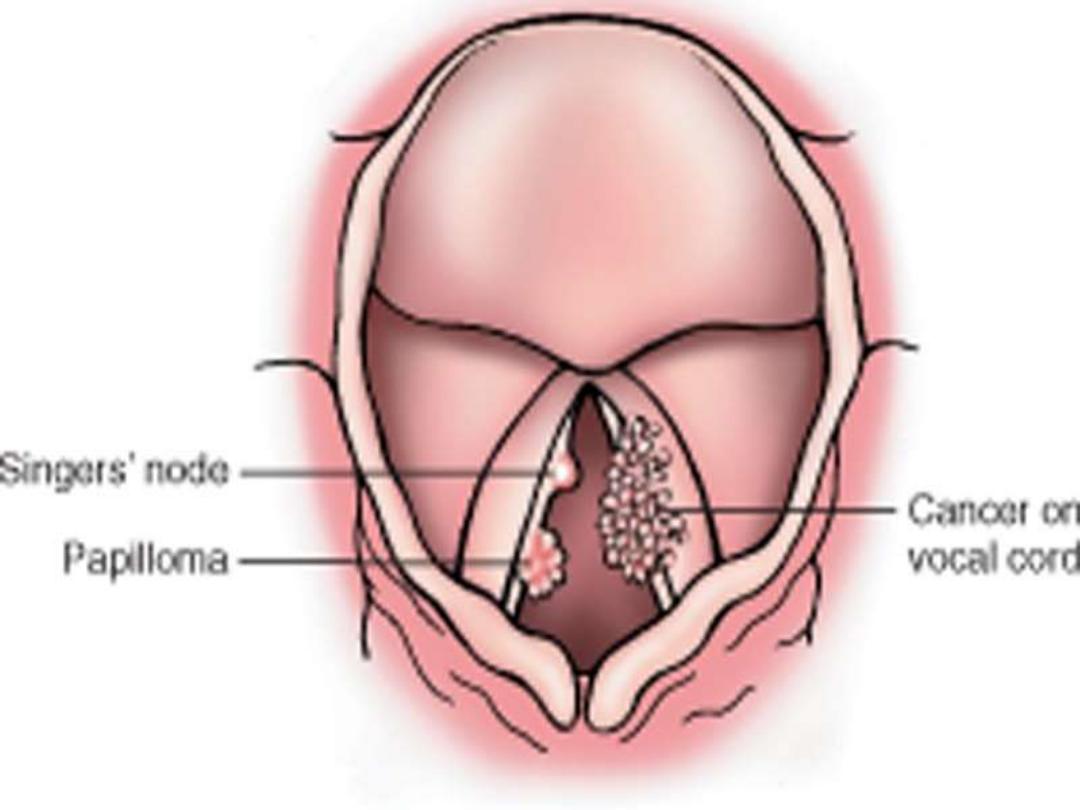
Vocal cord nodules ("polyps")
are smooth protrusions (usually less than
0.5 cm in diameter) located, most often, on
the true vocal cords
. The nodules
are composed of fibrous tissue and covered by stratified squamous mucosa.
These lesions occur chiefly in
heavy smokers or singers (singer's nodes)
,
suggesting that they are the result of chronic irritation or voice abuse.
Laryngeal papilloma (squamous papilloma)
of the larynx is a benign
neoplasm, usually on the
true vocal cords
, that forms a soft, raspberry-like
excrescence rarely more than 1 cm in diameter.
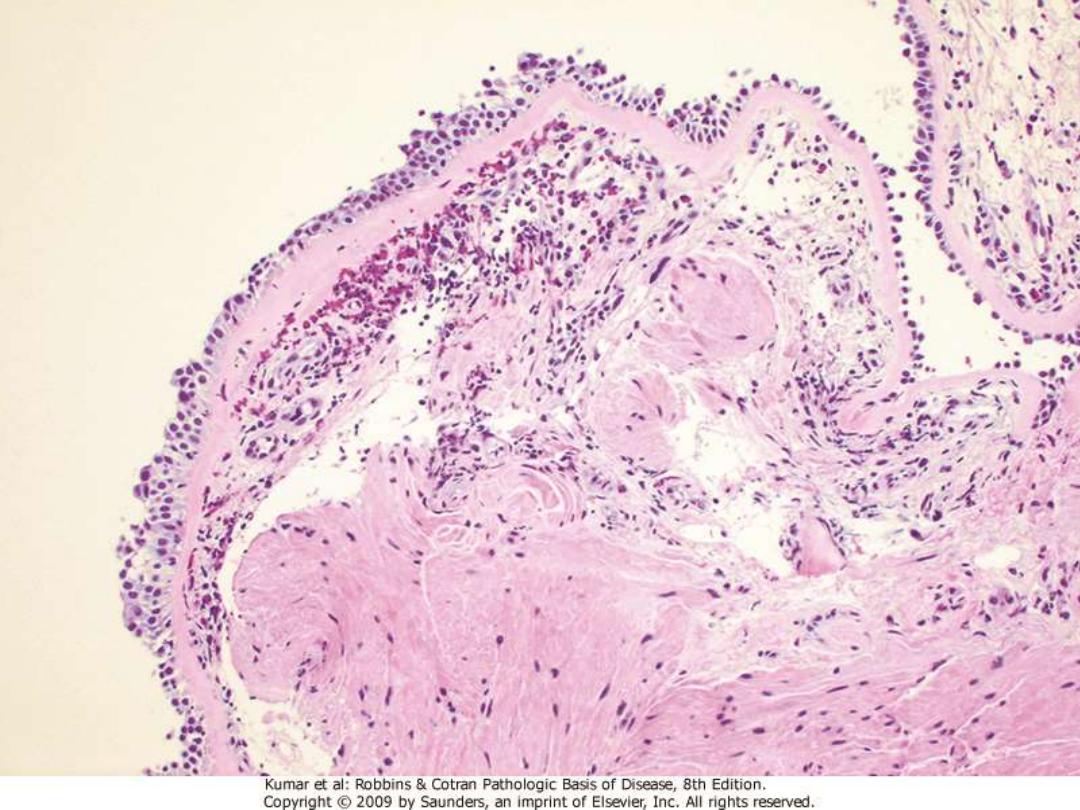
Microscopically
, it consists of
multiple, slender, finger-like projections supported by central fibrovascular
cores and covered by benign, stratified squamous epithelium.
Papillomas are usually single in adults but are often multiple in children
, in
whom they are referred to as
recurrent respiratory papillomatosis (RRP),
since
they typically tend to recur after excision. These lesions are caused by
human
papillomavirus (HPV) types 6 and 11,
do not become malignant, and often
spontaneously regress at puberty.
A 28-year-old man who is a singer/songwriter has been experiencing hard
times for the past 3 years. He has played at a couple of clubs a night to
earn enough to avoid homelessness. He comes to the free clinic because he
has noticed that his voice quality has become progressively hoarser over
the past year. On physical examination: There are no palpable masses in
the head and neck area. He does not have a cough or significant sputum
production, but he has been advised on previous visits to give up smoking.
Which of the following is most likely to produce these findings?
(A) Croup
(B) Epiglottitis
(C) Reactive nodule
(D) Squamous cell carcinoma
(E) Squamous papillomatosis
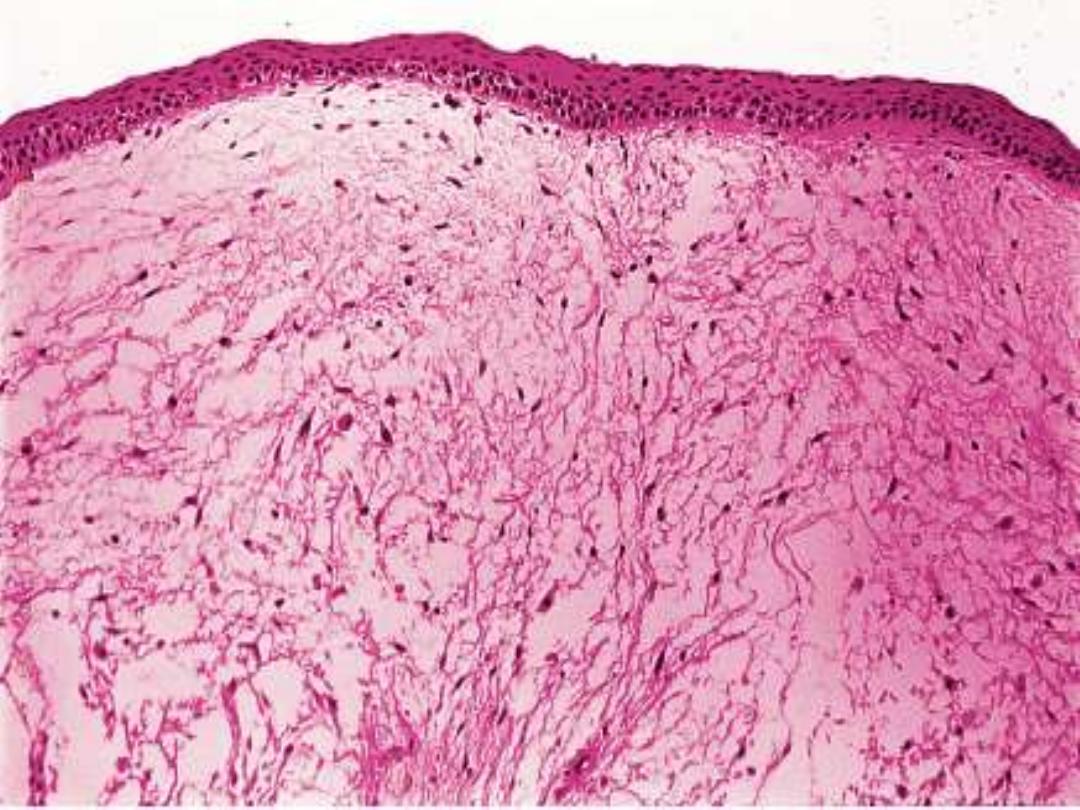
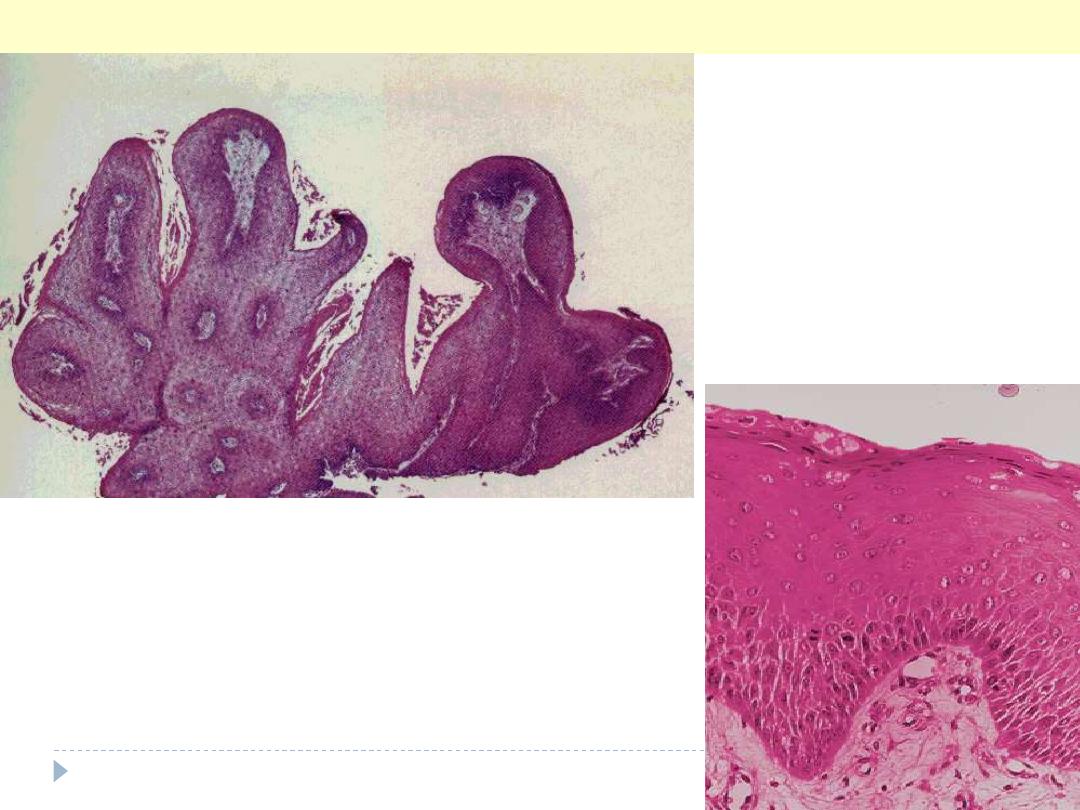
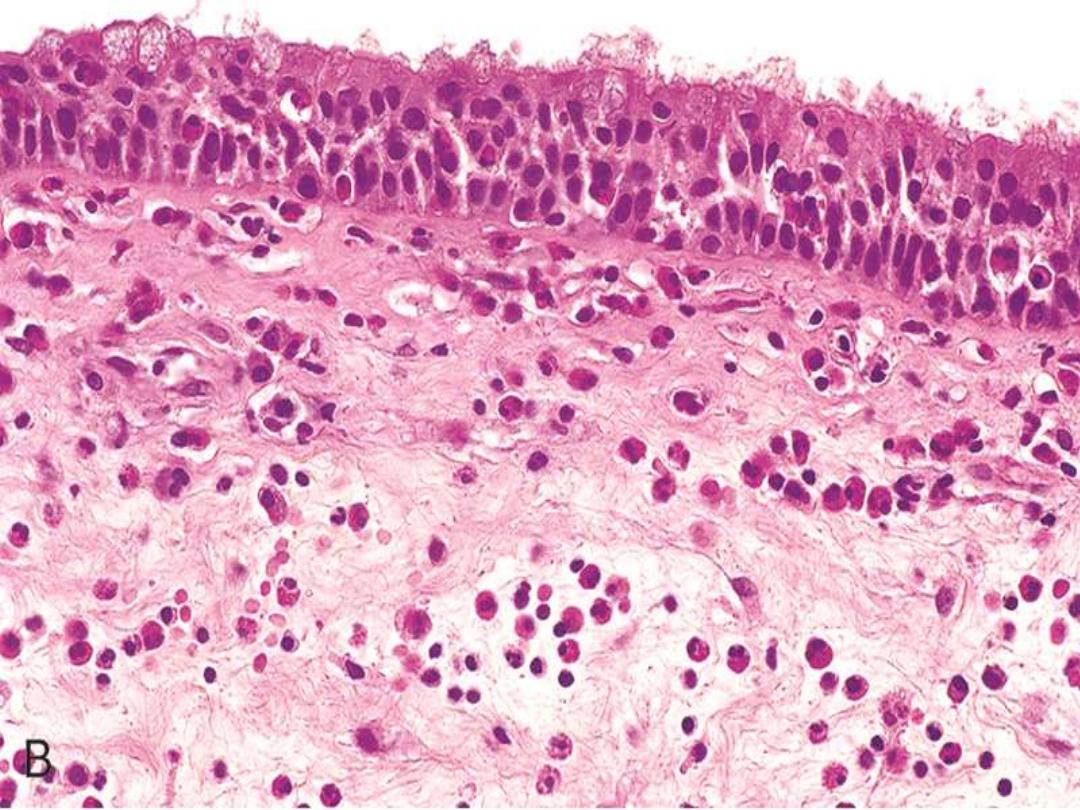
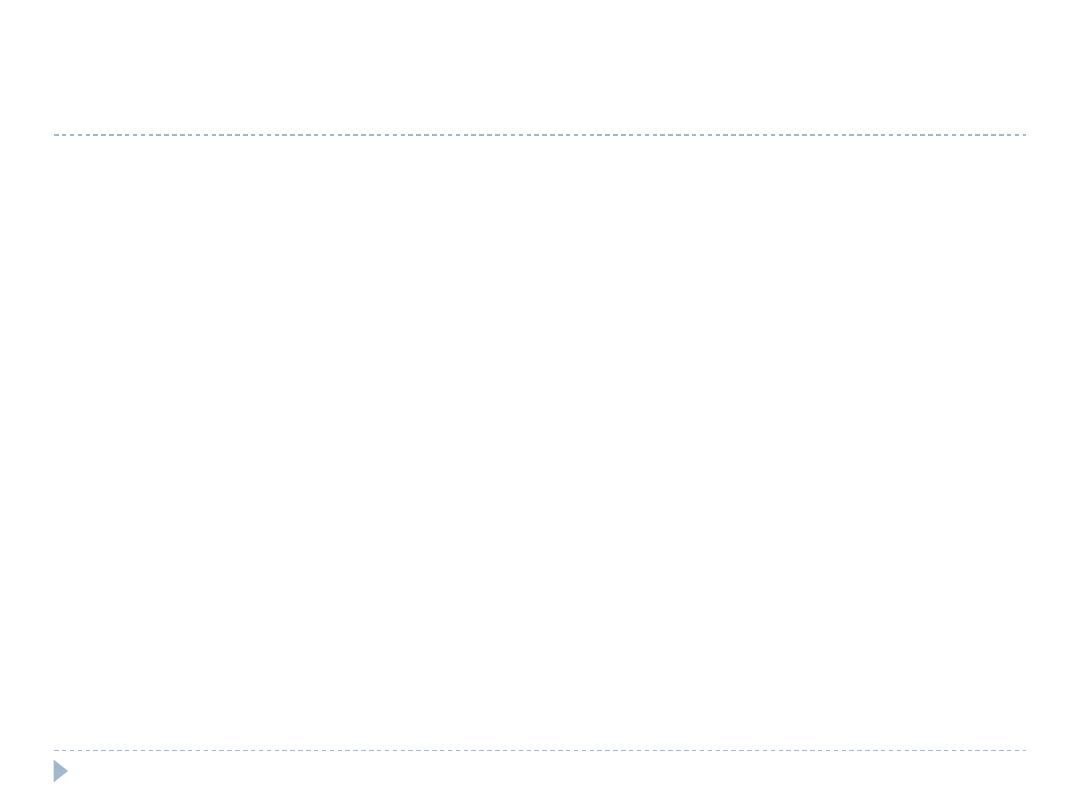
This multilayered benign-looking squamous epithelium is
arranged in a finger-like projections, each having a core of
vascularized connective tissue. The Rt. Photo is a higher power
showing the squamous epithelium cover of one of the papillae.
Squamous cell papilloma larynx
Malignant Lesions
Carcinoma of the Larynx
Carcinoma of the larynx most commonly occurs after age
40 years
and is more
common in men
(7: 1)
than in women.
Nearly all cases occur in
smokers,
and
alcohol and asbestos
exposure may also
play roles.
The vast majority (95%) are
squamous cell carcinomas.
The tumor develops mostly on the
vocal cords (glottic tumors),
but it may arise
above the cords
(supraglottic)
or below the cords
(subglottic).
They begin as
in situ lesions
that later appear as pearly gray, wrinkled plaques
on the mucosal surface, ultimately ulcerating and fungating.
As expected with lesions arising from recurrent exposure to environmental
carcinogens, adjacent mucosa may demonstrate squamous cell hyperplasia with
foci of dysplasia, or even carcinoma in situ.
Clinically there is persistent
hoarseness.
Supraglottic cancers have a worse prognosis than glottic tumors because of their
earlier metastasis to regional (cervical) lymph nodes. The subglottic tumors, like
the supraglottic ones, tend to remain clinically silent, & thus usually present as
advanced disease.
With surgery, radiation, or combined therapeutic treatments, only one third die
of the disease.
The usual cause of death is infection of the distal respiratory passages or
widespread metastases and cachexia.
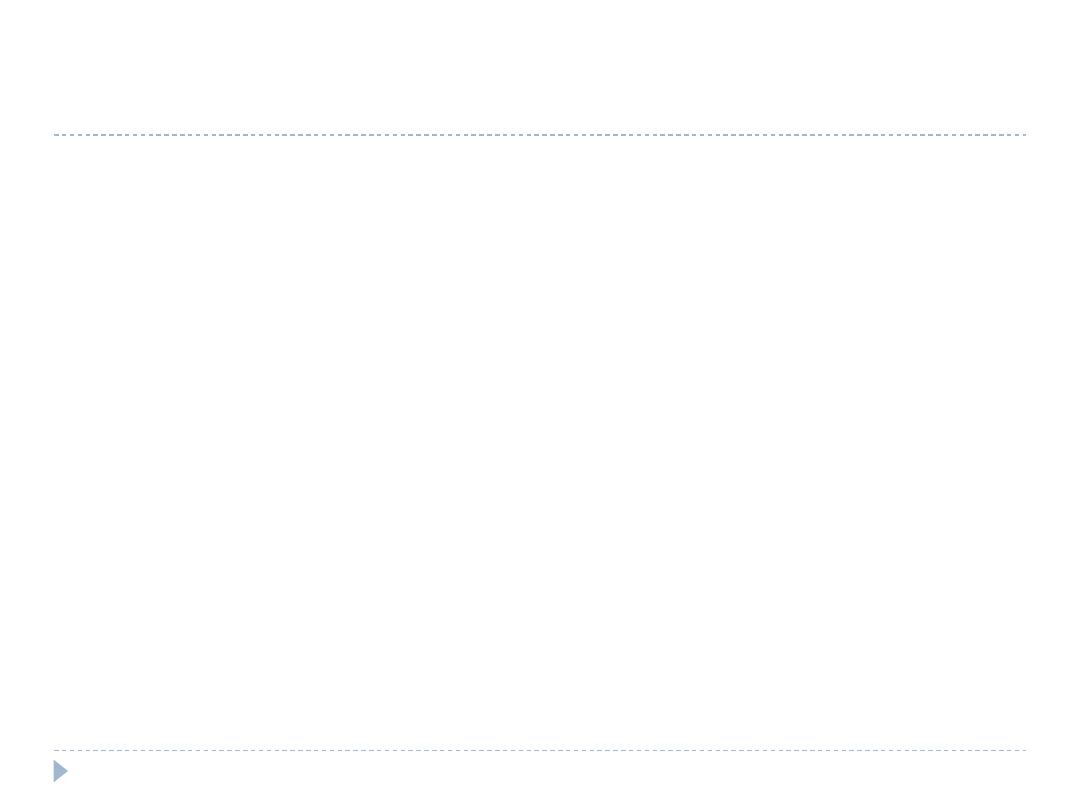
Transglottic Infraglottic Supraglottic
A 70-year-old man who has experienced increasing
hoarseness for almost 6 months has recently had an episode
of hemoptysis. On physical examination, no lesions are noted
in the nasal or oral cavity. There is a firm, nontender anterior
cervical lymph node. The lesion shown in the figure is
identified by endoscopy. The patient undergoes biopsy,
followed by laryngectomy and neck dissection. Which of the
following etiologic factors most likely played the greatest role
in the
development of this lesion?
(A) Human papillomavirus infection
(B) Type I hypersensitivity
(C) Smoking tobacco
(D) Repeated bouts of aspiration
(E) Epstein-Barr virus infection
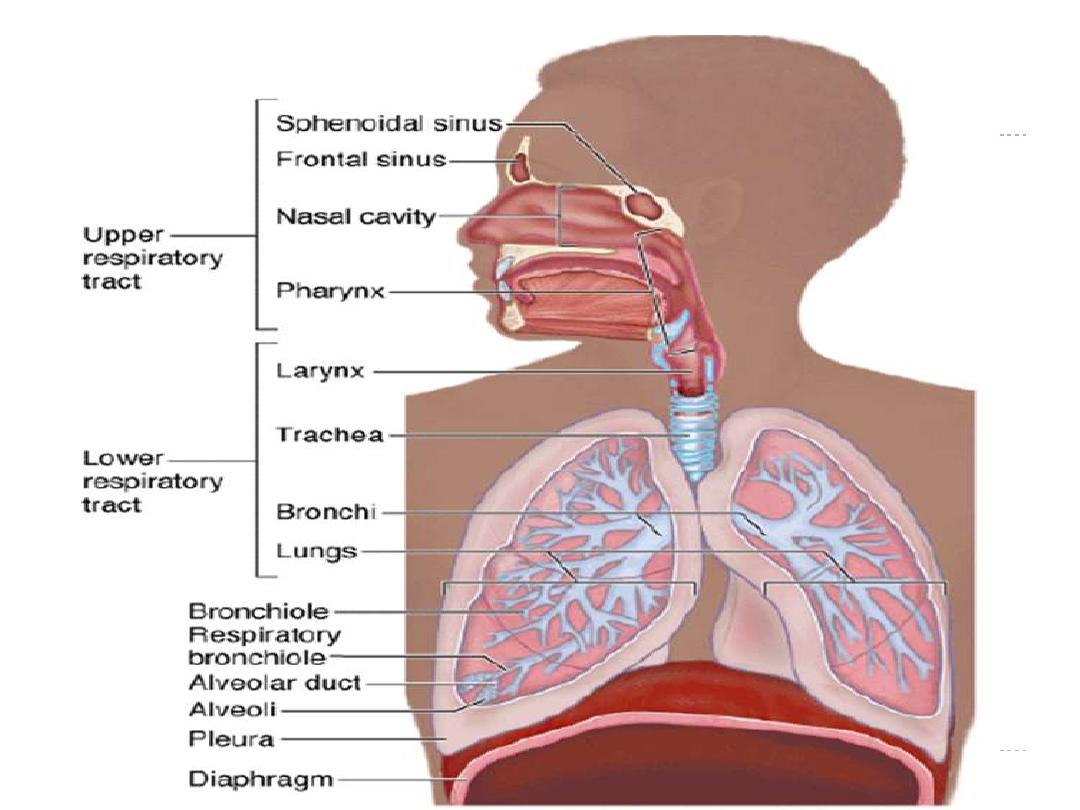
THE LUNG
ATELECTASIS (COLLAPSE)
is loss of lung volume caused by inadequate expansion of
airspaces; this leads to shunting of inadequately oxygenated blood
from pulmonary arteries into veins, thus giving rise to hypoxia.
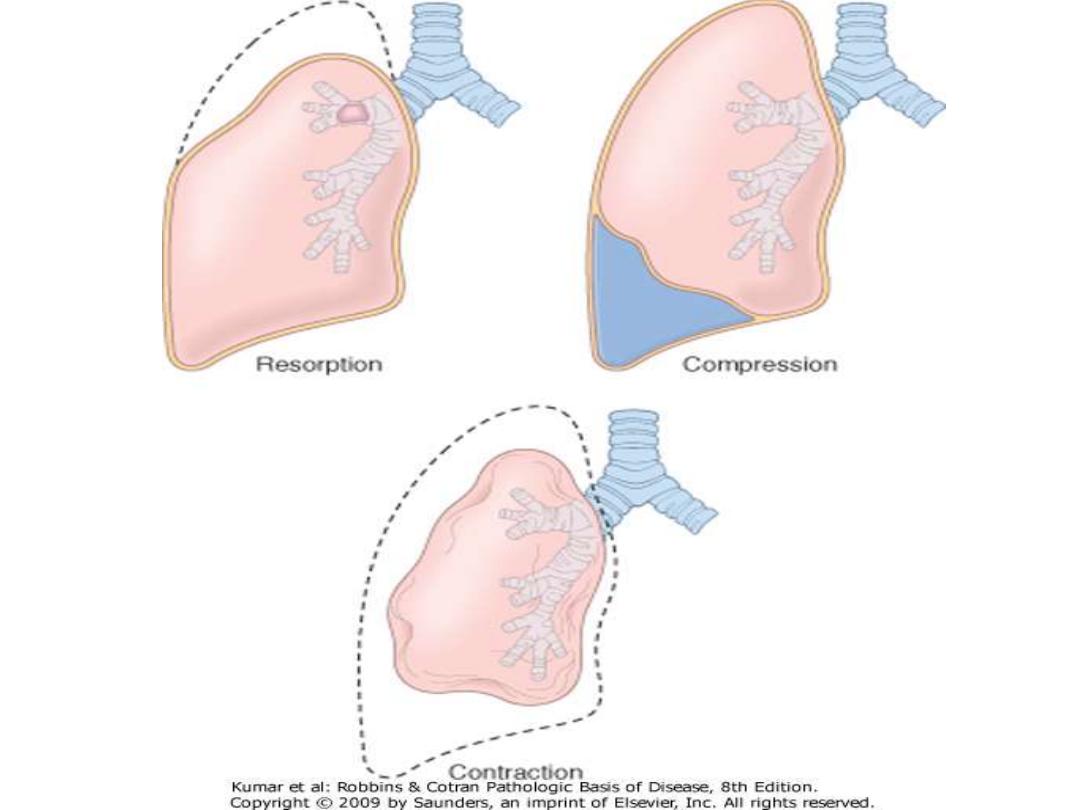
Pathogenetically atelectasis is classified into three forms
1.
Resorption atelectasis
complicating obstruction.
The air already present distally gradually becomes absorbed, and alveolar
collapse follows.
Depending on the level of airway obstruction, an entire lung, a complete
lobe, or a segment may be involved.
A mucous or muco-purulent plug is the most common cause of such
obstruction for
e.g. following surgical operations or bronchial asthma,
bronchiectasis, chronic bronchitis, or the aspiration of foreign bodies,
particularly in children.
2. Compression atelectasis
is usually due to mechanical compression of the lung by pleural
distension as in pleural effusion (congestive heart failure) or
pneumothorax.
Basal atelectasis
is another example & is due to elevated diaphragm as
that occurs in bedridden patients, in those with ascites, and during and
after surgery.
3. Contraction atelectasis
occurs in the presence of focal or generalized pulmonary fibrosis or
pleural fibrosis; in these situations there is interference with expansion
and an increase in elastic recoil during expiration.
Atelectasis (except contraction type) is reversible and should be treated
quickly to prevent hypoxemia and infection of the collapsed lung.
A 7-year-old boy accidentally inhales a small peanut,
which lodges in one of his bronchi. A chest x-ray
reveals the mediastinum to be shifted toward the
side of the obstruction. Which of the following
pulmonary abnormalities is most likely present in
this boy?
a. Absorptive atelectasis
b. Compression atelectasis
c. Contraction atelectasis
d. Patchy atelectasis
e. Hyaline membrane disease

ADULT RESPIRATORY DISTRESS
SYNDROME (ARDS)
(previously “Shock lung”) is “progressive
respiratory insufficiency caused by diffuse alveolar damage”
The clinical setting associated with ARDS include
A. Respiratory
1. Diffuse infections (viral, bacterial)
2. Aspiration
3. Inhalation (toxic gases, near drowning)
4. O
2
therapy
B. Non-respiratory
1. Sepsis (septic shock)
2. Trauma (with hypotension)
3. Burns
4. Pancreatitis
5. Ingested toxins (e.g. paraquat)
There is an acute onset of dyspnea, hypoxemia (refractory to O
2
therapy), and
radiographic bilateral pulmonary infiltrates (noncardiogenic pulmonary edema).
The condition may progress to multisystem organ failure.
Pathogenesis
In ARDS there is damage to alveolar capillary membrane by endothelial
&/or epithelial injury. This leads to three consequences
1. Increased vascular permeability (endothelial damage)
2. Loss of diffusion capacity of the gases
3. Widespread surfactant deficiency (damage to type II pneumocytes).
Nuclear factor κB,
is suspected of tilting the balance in favor of pro-
inflammatory rather than anti-inflammatory mediators, which causes
the endothelial damage.
This leads to fluid accumulation.
Following the insult, there is increased synthesis of a potent neutrophil
chemotactic and activating agent
IL-8 & TNF
by pulmonary
macrophages.
The recruited, activated neutrophils release oxidants, proteases, etc.
that cause damage to the alveolar epithelium leading to loss of
surfactant that interferes with alveolar expansion.
Gross features:
in the acute phase the lungs are dark red, airless, and heavy.
Microscopic features:
The histologic reflection of ARDS in the lungs is known as
diffuse alveolar damage.
Early stage is characterized by
Capillary congestion and stuffing by neutrophils
Necrosis of alveolar epithelial cells
Interstitial and intra-alveolar edema and sometimes hemorrhage
The presence of
hyaline membranes is characteristic
.
They particularly line the distended alveolar ducts & consist of fibrin admixed
with necrotic epithelial cells.
Overall, the picture is very similar to that seen in
respiratory distress syndrome
in the newborn.
Organizing stage is characterized by
Marked regenerative proliferation of type II pneumocytes
Organization of the fibrin exudates.
This eventuates in intra-alveolar fibrosis.
Marked fibrotic thickening of the alveolar septa.
The prognosis of ARDS
is gloomy and
mortality rates are around 60%
despite improvements in
supportive therapy.
However, in most patients who survive the acute insult normal
respiratory function returns.
Alternatively,
diffuse interstitial fibrosis occurs with permanent
impairment of respiratory function.
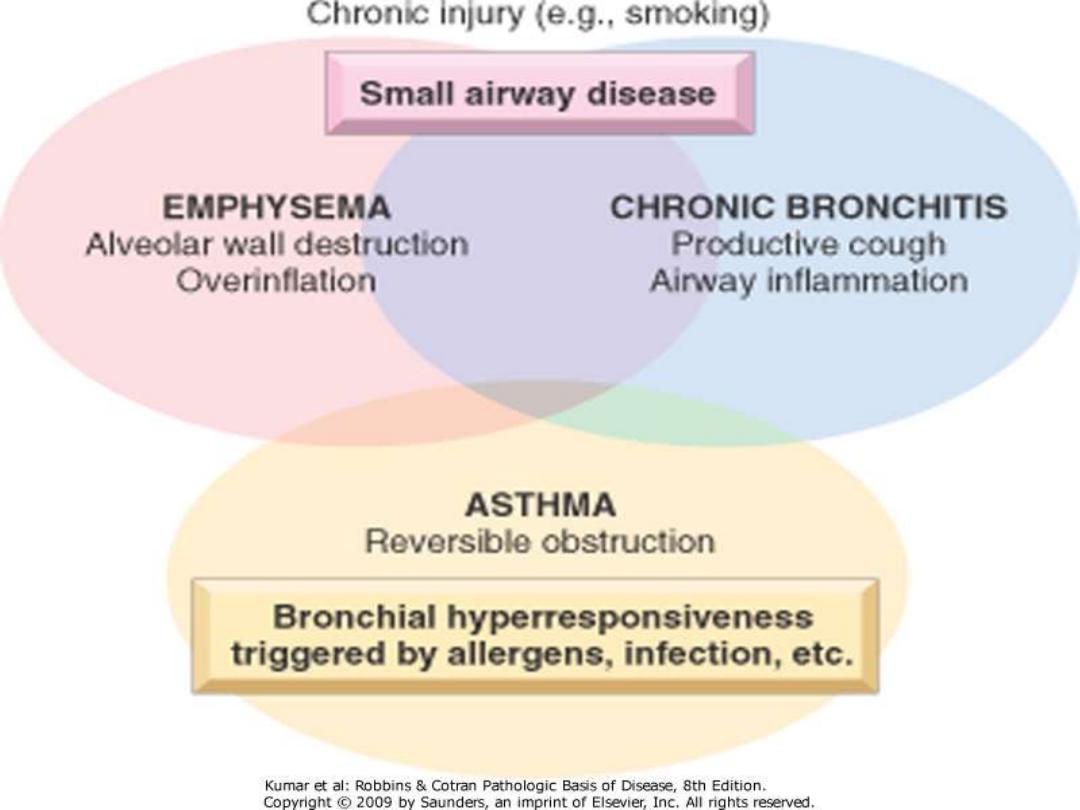
OBSTRUCTIVE PULMONARY DISEASE
Under this heading come four entities
1. Emphysema
2. Chronic bronchitis
3. Asthma
4. Bronchiectasis
Although chronic bronchitis may exist without emphysema, and pure
emphysema may occur (with inherited α
1
-antitrypsin deficiency), the two
diseases usually coexist.
This is because long-term cigarette smoking is a common underlying
agent in both disorders.
Emphysema and chronic bronchitis are often clinically grouped together
under the term
chronic obstructive pulmonary disease (COPD),
which is
one of the leading causes of death.
The irreversibility of airflow obstruction of COPD distinguishes it from
asthma (reversible obstruction)
EMPHYSEMA
is defined as
"abnormal permanent enlargement of the airspaces distal to the
terminal bronchioles, accompanied by destruction of their walls without
obvious fibrosis".
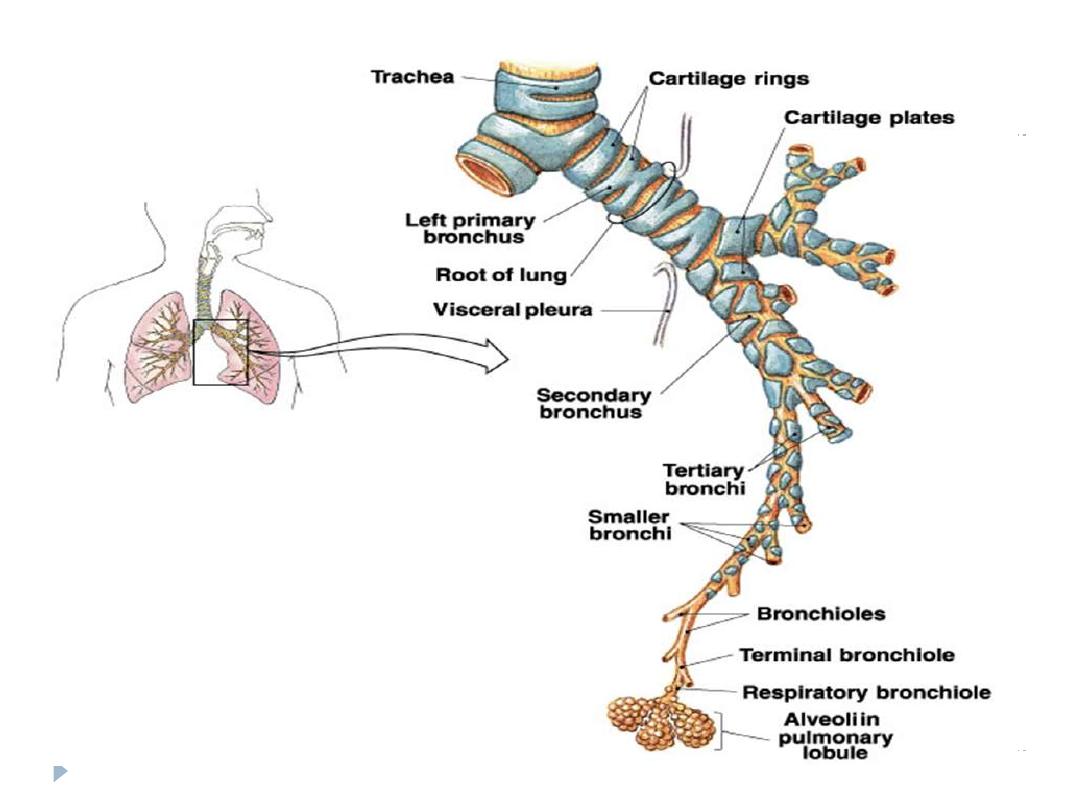
Classification of Emphysema
is according to its anatomic distribution
within the lobule; the acinus is the structure distal to terminal bronchioles,
and a cluster of 3 to 5 acini is called a lobule. There are four major types of
emphysema:
1. Centriacinar
2. Panacinar
3. Distal acinar
4. Irregular
Only the first two cause clinically significant airway obstruction, with
centriacinar emphysema being about 20 times more common than
panacinar disease.
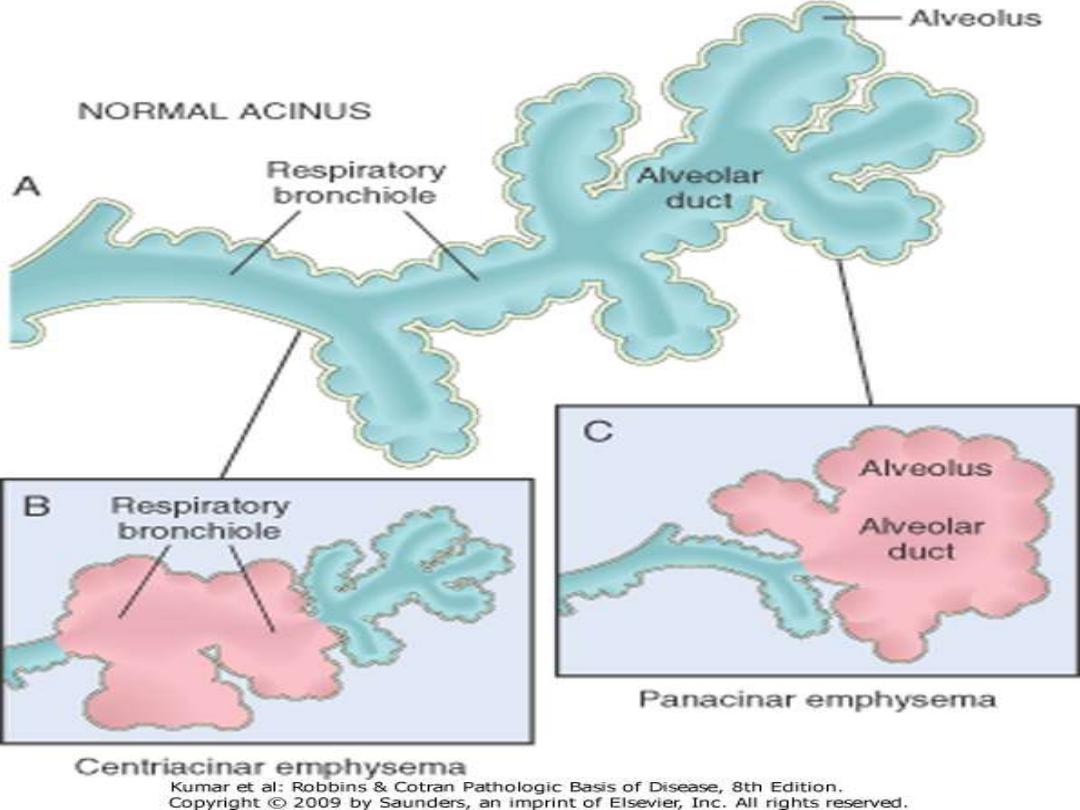
Centriacinar (Centrilobular) Emphysema:
the central parts of the
acini i.e.
the respiratory bronchioles
are affected, while distal alveoli are
spared. The lesions are more common and severe in the
upper lobes
.
This
type is most commonly associated with cigarette smoking.
Panacinar (Panlobular) Emphysema:
the acini are uniformly
enlarged from the level of the respiratory bronchiole to the terminal blind
alveoli . It tends to occur more commonly in the
lower lobes
and is
the type
that occurs in α
1
-antitrypsin deficiency.
Distal Acinar (Paraseptal) Emphysema:
the distal part of the acinus
is primarily involved especially adjacent to the pleura and the lobular
connective tissue septa. Characteristically, there are
multiple, adjacent,
enlarged airspaces up to 2 cm or more in diameter, sometimes forming
cystic structures referred to as bullae.
This type of emphysema probably
underlies many of the cases of spontaneous pneumothorax in young adults.
Irregular Emphysema:
the acinus is irregularly involved; it is
associated with
scarring.
Pathogenesis of centriacinar & panacinar forms of
emphysema
These are thought to arise as a result of
imbalances of
protease-antiprotease and oxidant-antioxidant .
The protease-antiprotease imbalance hypothesis is
supported by the enhanced tendency of emphysema
development in patients with
genetic α1-antitrypsin
deficiency, which is aggrvated by smoking.
α1-Antitrypsin, is a major inhibitor of proteases
(particularly elastase) secreted by neutrophils during
inflammation.
Emphysema seems to result from the destructive effect of
high protease activity in subjects with low antiprotease
action.
Smoking seems to play a decisive role in the pathogenesis of
emphysema
1.
It causes accumulation of neutrophils & macrophages within the
alveoli through its
direct chemoattractant effects
and through the
reactive oxygen species contained in it. These activate the
transcription factor
NF-κB
, which switches on genes that encode
TNF
and IL-8.
These, in turn, attract and activate more neutrophils. Accumulated
active neutrophils release their granules, which are rich in a variety of
proteases (
elastase, proteinase, etc
.) that result in tissue damage.
2. Smoking also
enhances elastase activity in macrophages;
this elastase is
not inhibited by α
1
-antitrypsin; additionally, it can digest this
antiprotease.
3. Tobacco smoke contains
abundant reactive oxygen free radicals,
which
deplete the antioxidant mechanisms, thereby inciting tissue damage.
A secondary consequence of oxidative injury is inactivation of native
antiproteases, resulting in "functional" α
1
-antitrypsin deficiency even in
patients without enzyme deficiency
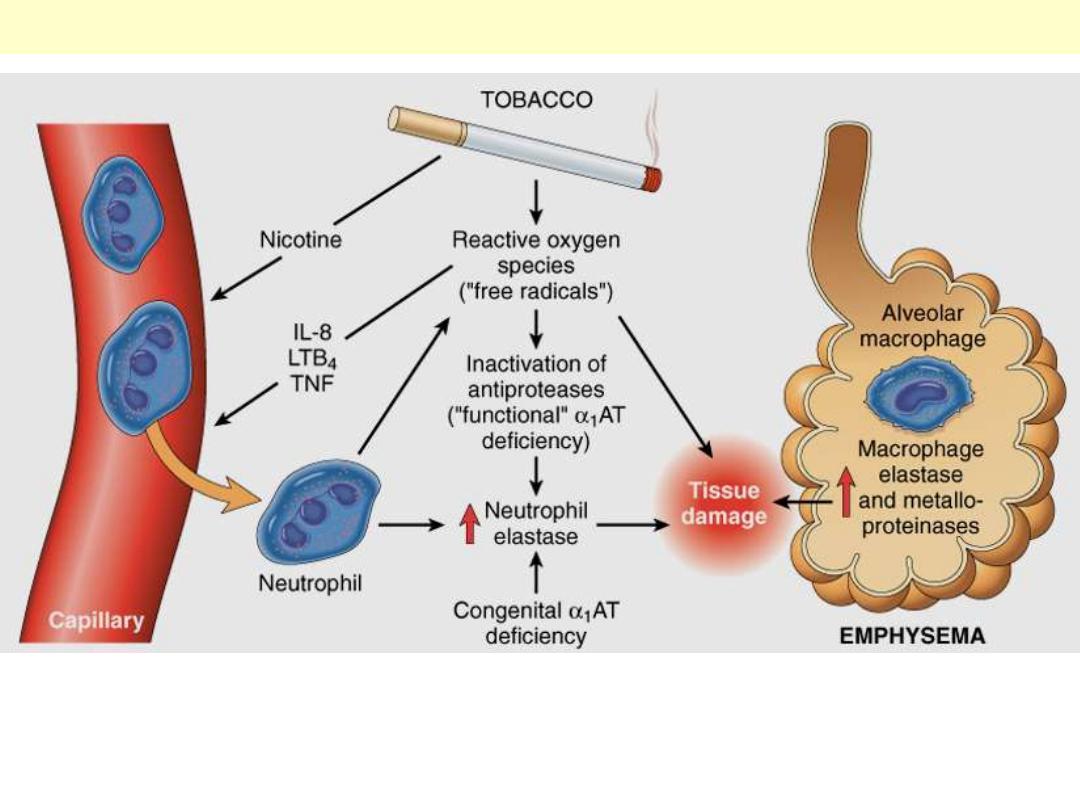
The protease-antiprotease imbalance and oxidant-antioxidant imbalance are additive in their effects
and contribute to tissue damage. α1-Antitrypsin (α1AT) deficiency can be either congenital or
"functional" as a result of oxidative inactivation. See text for details. IL-8, interleukin 8; LTB4,
leukotriene B4; TNF, tumor necrosis factor.
Pathogenesis of emphysema
Gross features
The diagnosis and classification of emphysema depend on the gross
appearance of the lung.
Panacinar emphysema produces pale, voluminous lungs that obscure
the heart at autopsy.
In centriacinar emphysema the lungs are less voluminous and deeper
pink. Generally, in this type the upper two-thirds of the lungs are more
severely affected.
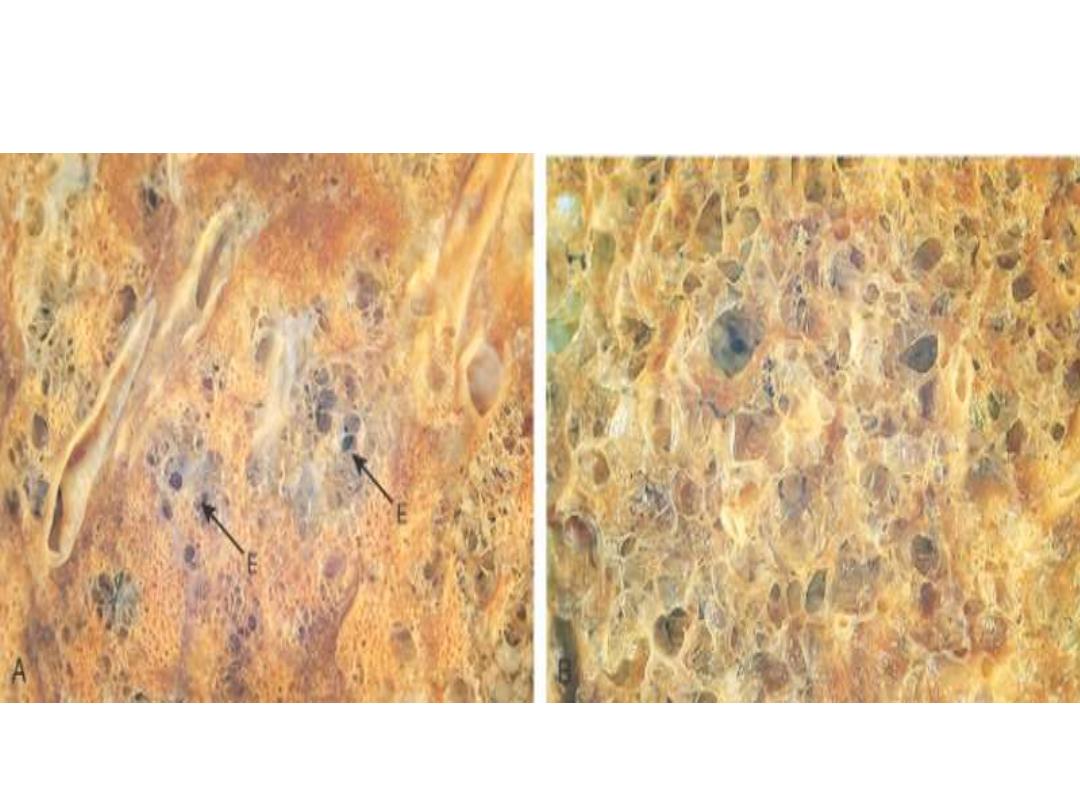
Microscopic features
There is thinning and destruction of alveolar walls.
With advanced disease, adjacent alveoli coalesce, creating large
airspaces.
The capillaries within alveolar walls are reduced in number due to
stretching.
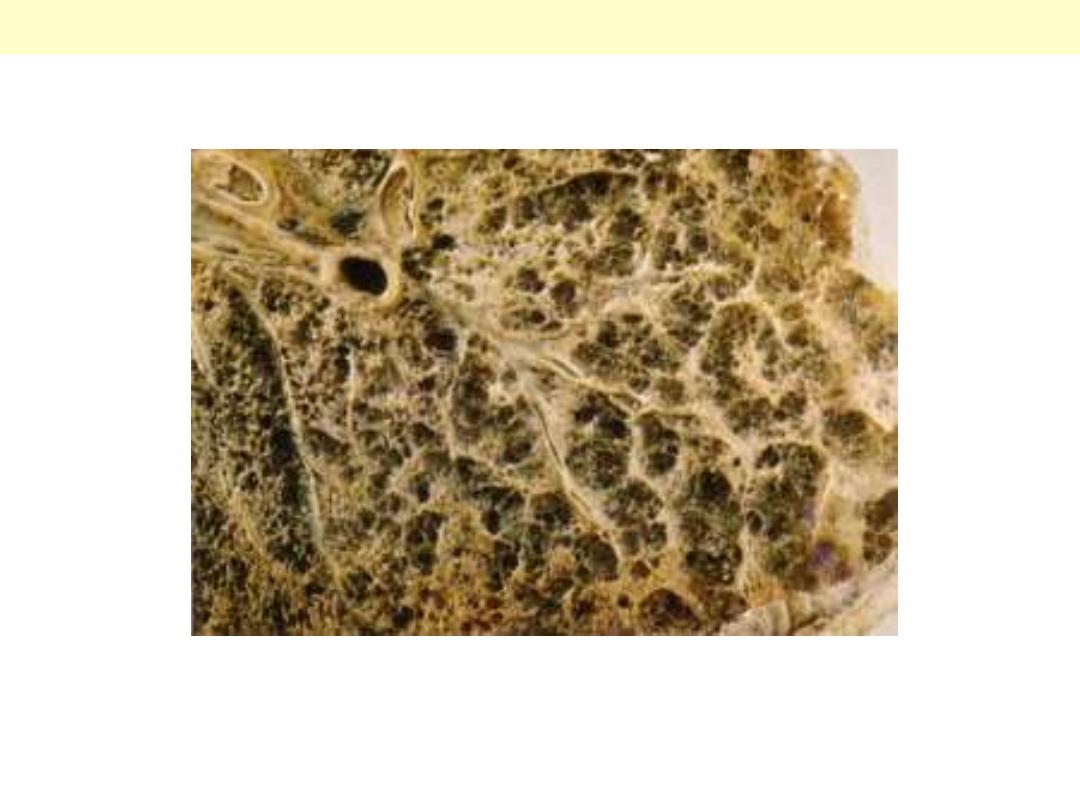
There is severe diffuse involvement of the acini; the whole acinus is markedly
dilated.
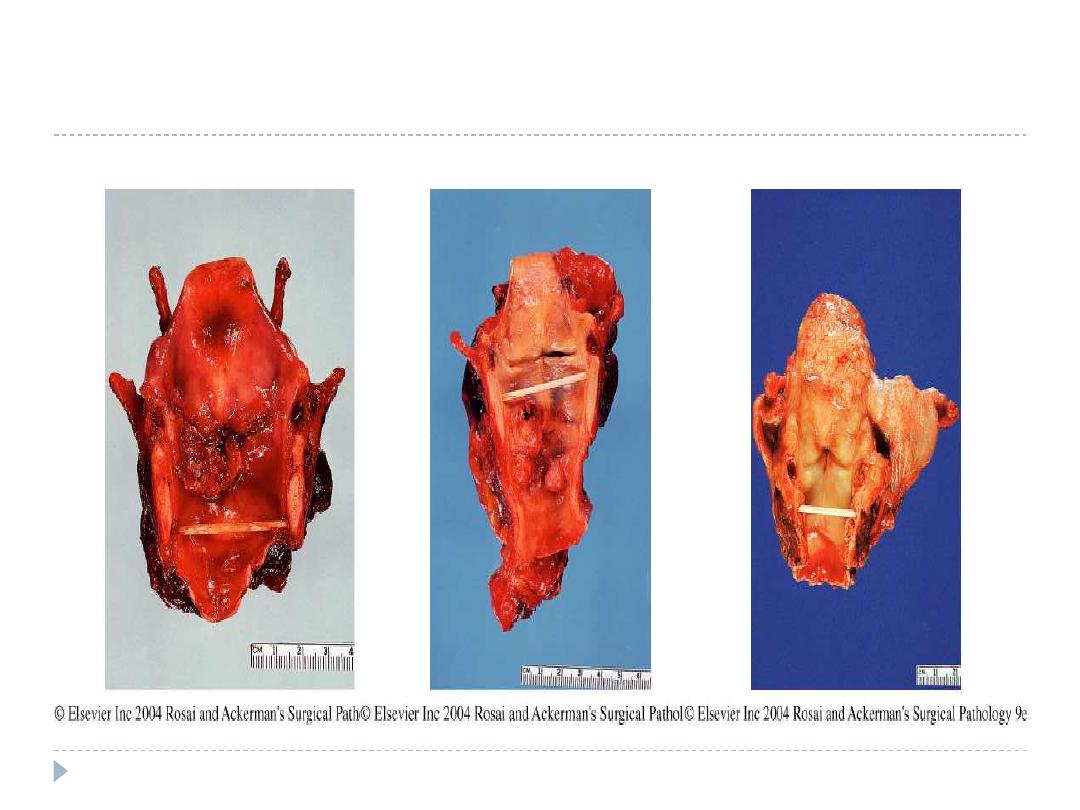
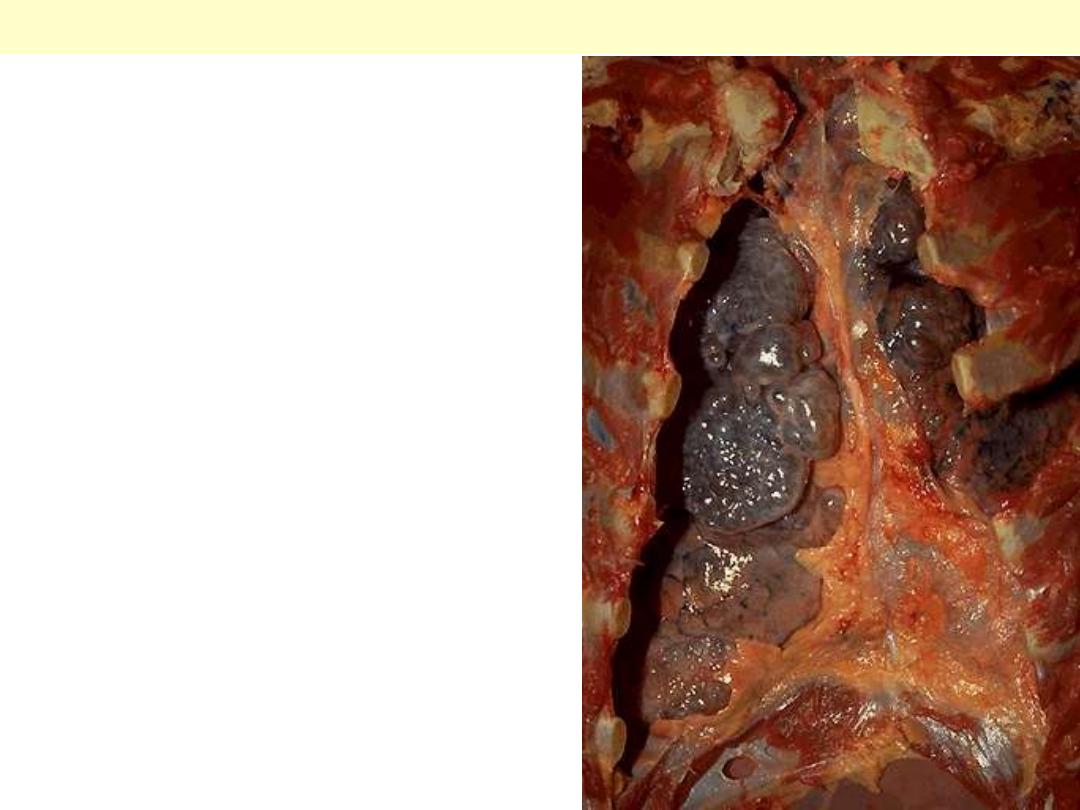
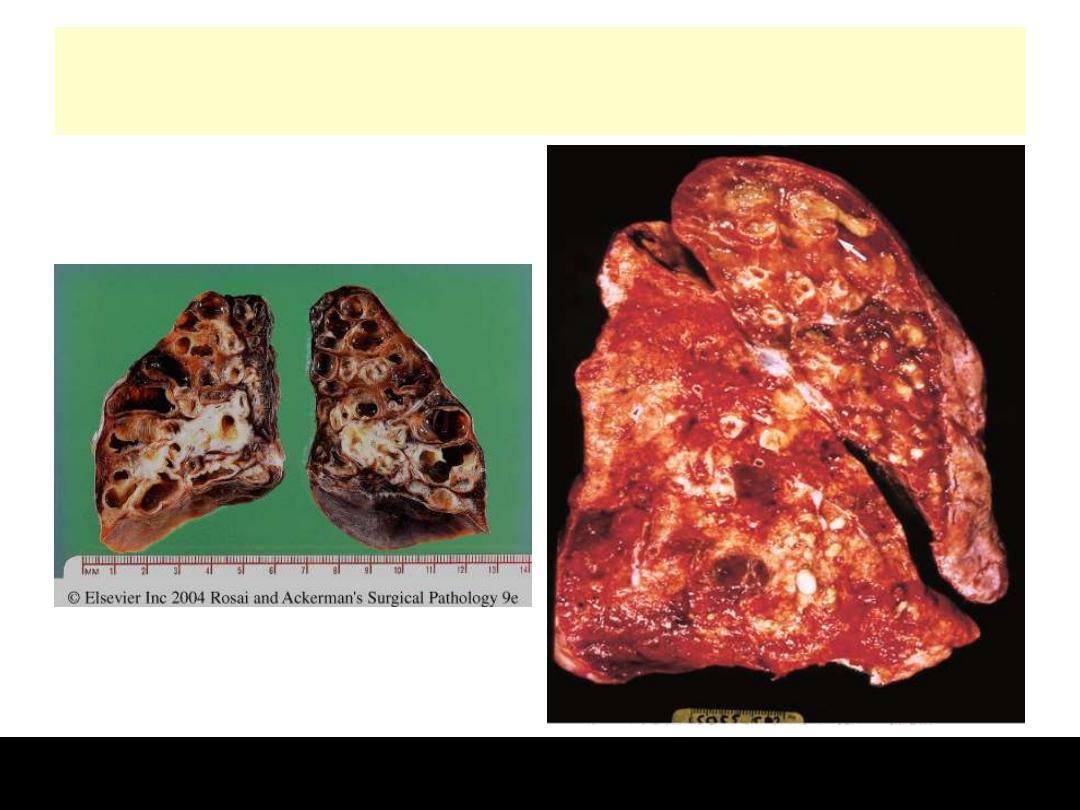
Panacinar emphysema
The 'substance' of the lung has been almost
completely lost. When such lungs are
removed from the body they are soft and
can often be squeezed into a small ball. The
pathology can be demonstrated by inflating
the intact lung by running formalin into the
main bronchus, allowing it to float in
formalin for 48 hours for fixation, then
slicing it with a long, sharp knife. As the
lung is cut, the formalin runs out of the
emphysematous spaces but the holey organ
can be examined by immersing the slices in
water, as was done for this photograph.
Pan-acinar destructive emphysema – severe emphysema.
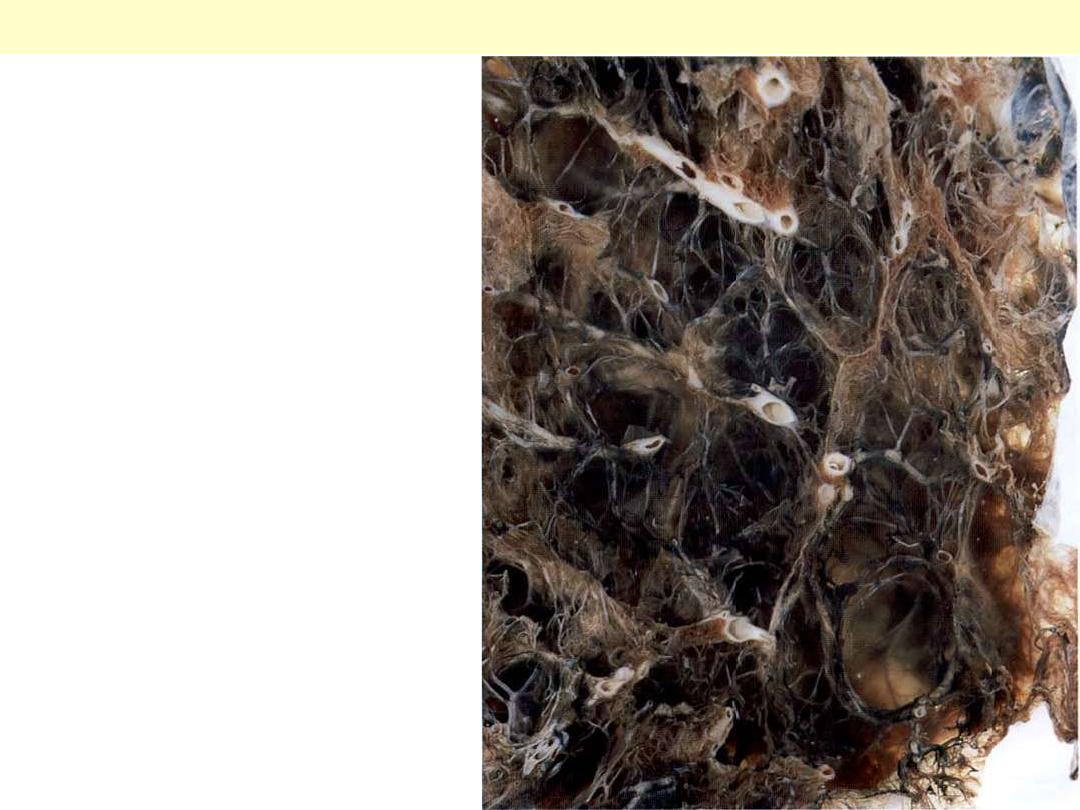
The chest cavity is opened at autopsy to reveal
numerous large bullae apparent on the surface of the
lungs in a patient dying with emphysema. Bullae are
large dilated airspaces that bulge out from beneath
the pleura. Emphysema is characterized by a loss of
lung parenchyma by destruction of alveoli so that
there is permanent dilation of airspaces.
Advanced emphysema
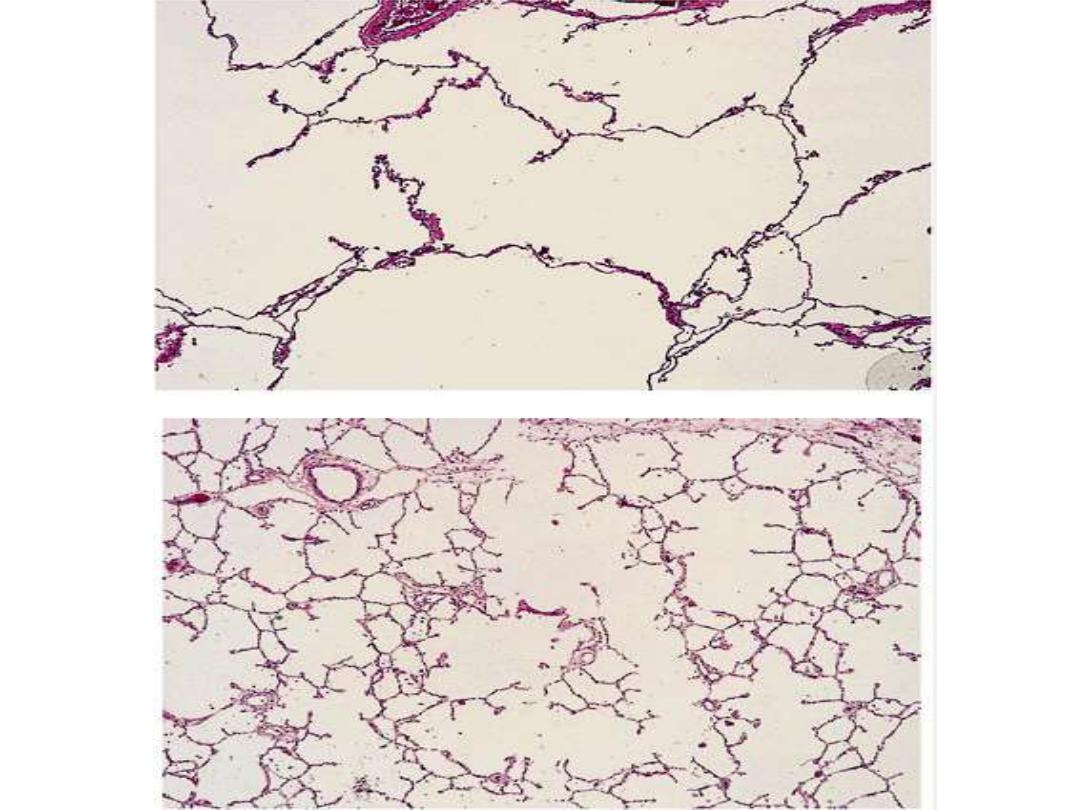
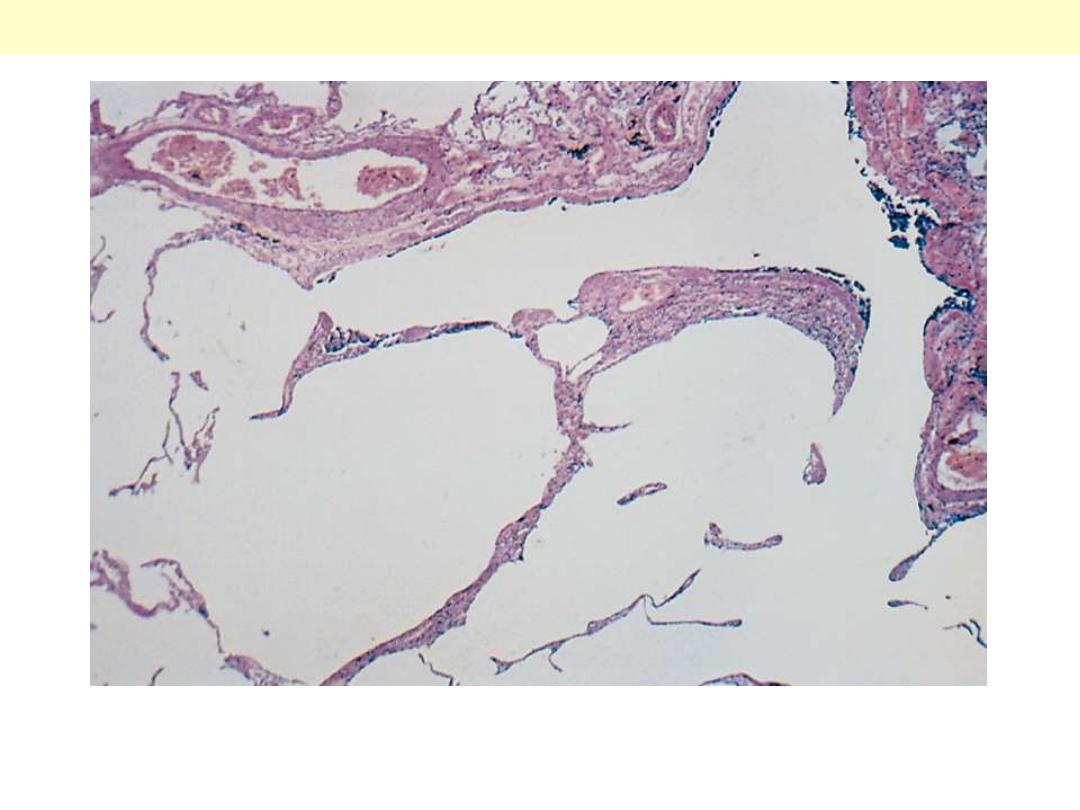
There is marked enlargement of airspaces, with thinning and
destruction of alveolar septa.
Pulmonary emphysema
Course & prognosis
With the loss of elastic tissue in the surrounding alveolar septa, there is
reduced radial traction on the small airways.
As a result, they tend to collapse during expiration-an important cause
of chronic airflow obstruction in severe emphysema.
The patient is
barrel-chested and dyspneic
, with obviously prolonged
expiration.
Hyperventilation is prominent thus gas exchange is adequate and blood
gas values are relatively normal i.e. there is no cyanosis.
Patients with emphysema and chronic bronchitis usually have less
prominent dyspnea and respiratory drive, so they retain carbon
dioxide, become hypoxic, and are often cyanotic.
The eventual outcome of emphysema is the gradual development of
secondary pulmonary hypertension,
arising from both hypoxia-induced
pulmonary vascular spasm and loss of pulmonary capillary surface
area from alveolar destruction and stretching.
Death from emphysema is related to either pulmonary failure, or right-
sided heart failure (cor pulmonale).
Conditions Related to Emphysem
a
Several conditions resemble but are not really emphysema, these include
a.
Compensatory emphysema
refers to dilation of alveoli in
response to
loss of lung substance
elsewhere, as in residual
lung tissue after surgical removal of a diseased lung or lobe.
b. Obstructive overinflation:
the lung expands because air is
trapped within it. A common cause is
subtotal obstruction
by a
tumor or foreign object, & mucous plugs in asthmatic patients. It
can be a life-threatening emergency if the affected portion extends
sufficiently to compress the remaining normal lung.
c. Bullous emphysema
refers to any form of emphysema that
produces
bullae (spaces >1 cm in diameter).
They represent
localized accentuations of one of the four forms of emphysema
, are
most often subpleural that with rupture leads to pneumothorax.
d. Mediastinal (interstitial) emphysema
signifies the entrance of air into the
connective tissue of the
lung, mediastinum, and subcutaneous tissue.
It may spontaneous as with a sudden increase in intra-
alveolar pressure (associated with vomiting or violent
coughing) that causes a tear, with dissection of air into the
connective tissue.
It is also likely to occur in
patients on respirators who have
partial bronchiolar obstruction or in persons who suffer a
perforating injury (e.g., a fractured rib).
When the interstitial air enters the subcutaneous tissue, the
patient may blow up like a balloon, with marked swelling of
the head and neck.
CHRONIC BRONCHITIS
is common among cigarette smokers
and in smog-ridden cities. The diagnosis of chronic bronchitis is clinical; it
is defined as
"a persistent productive cough for at least 3 consecutive months
in at least 2 consecutive years."
Pathogenesis
The distinctive feature of this disease is
hypersecretion of mucus
,
beginning in the
large airways
.
Although the single most important cause is
cigarette smoking
, other air
pollutants, such as
sulfur dioxide and nitrogen dio
xide, may contribute.
These environmental irritants induce
hypertrophy of mucous glands
in
the trachea and main bronchi and a
marked increase in mucin-secreting
goblet cells in the surface epithelium of smaller bronchi and bronchiole
s.
In addition, these irritants cause inflammation with infiltration of
CD8+
T
cells, macrophages, and neutrophils.
Microbial infection is often present but has a
secondary role,
chiefly by
maintaining the inflammation.
Airflow obstruction in chronic bronchitis results from :
1. Small airway disease,
(chronic bronchiolitis) induced by goblet cell
metaplasia with mucus plugging of the bronchiolar lumen, inflammation,
and bronchiolar wall fibrosis
2. Coexistent emphysema:
while small airway disease is important in the
early and mild airflow obstruction, chronic bronchitis with significant
airflow obstruction is almost always complicated by emphysema.
Gross features
The mucosal lining of the larger airways is usually hyperemic and
edematous. It is often covered by a layer of mucus or mucopurulent
secretions.
The smaller bronchi and bronchioles may also be filled with similar
secretions.
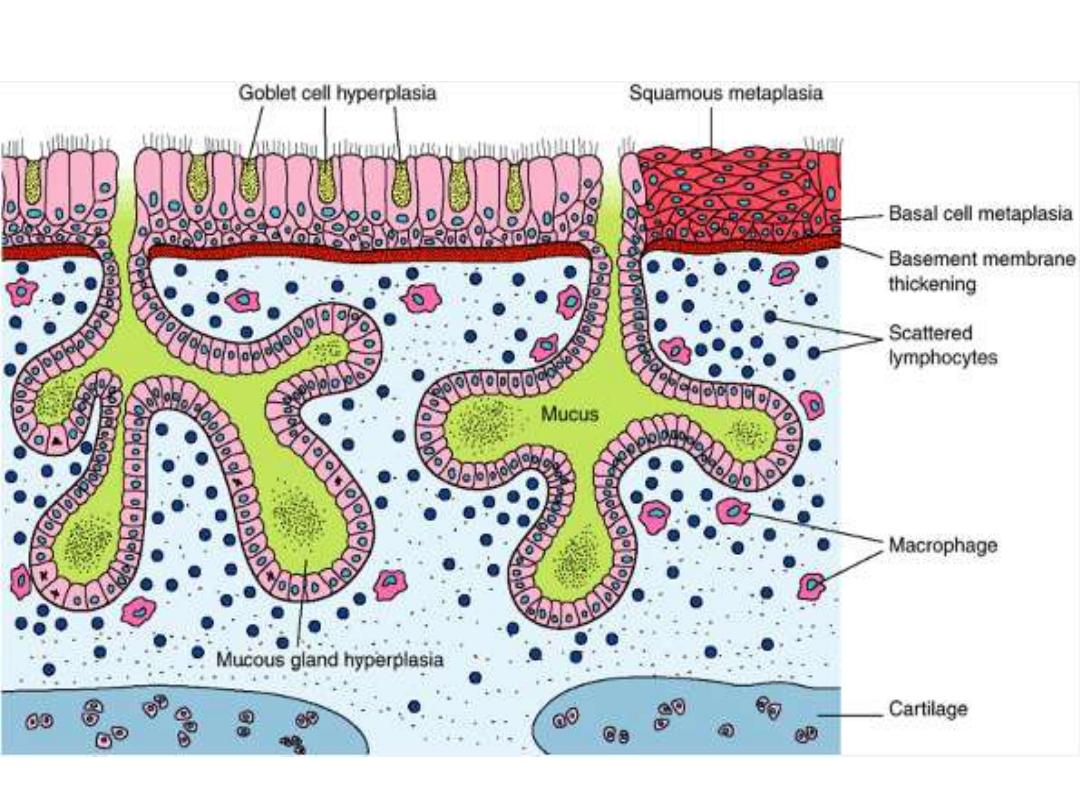
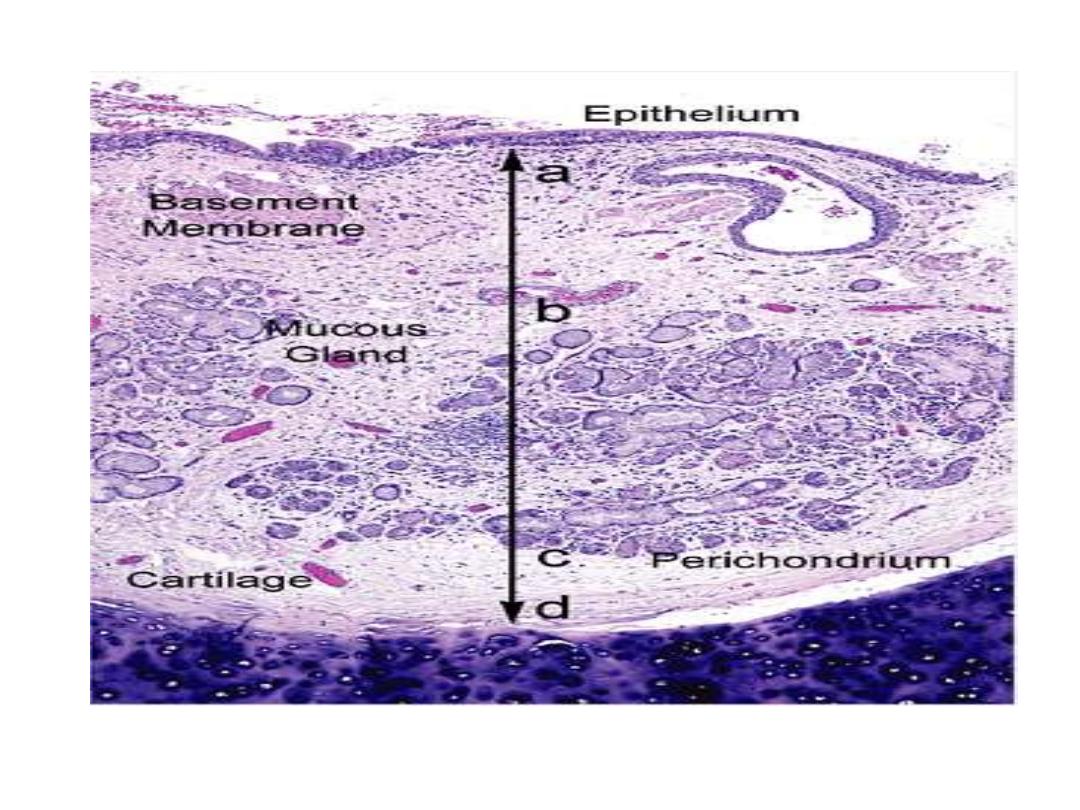
The lumen of the bronchus is above. Note the marked thickening of the mucous gland layer
(approximately twice normal) and squamous metaplasia of lung epithelium.
Chronic bronchitis
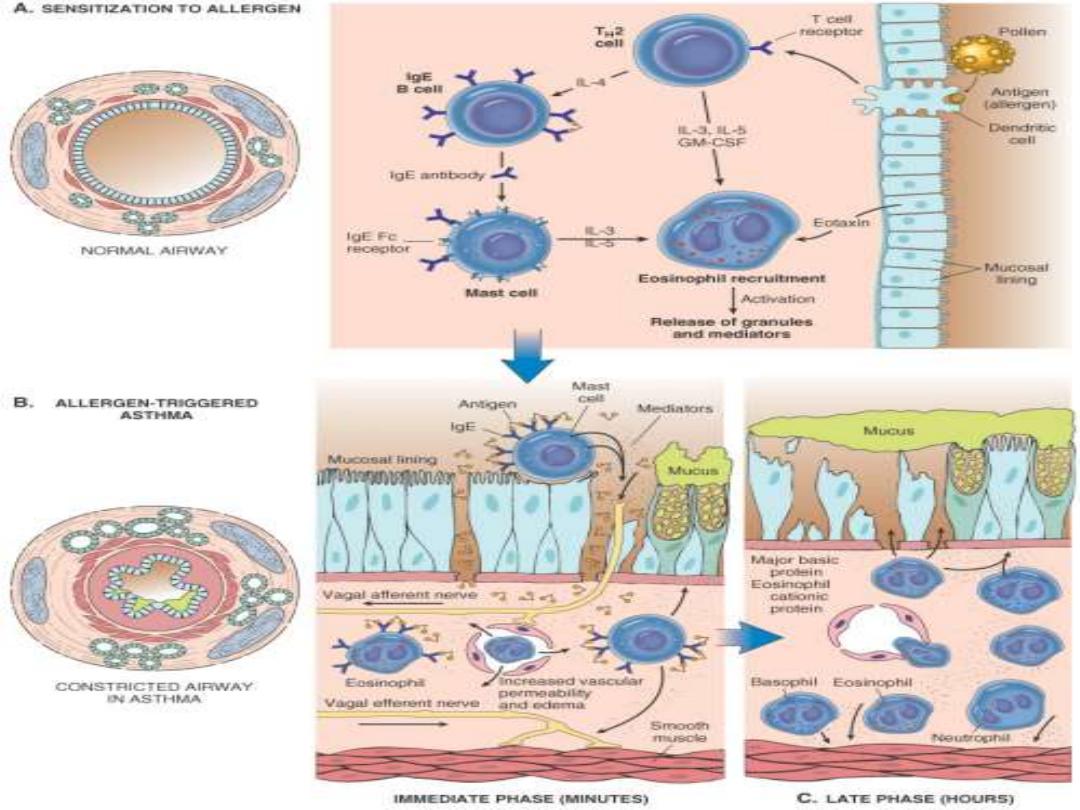
ASTHMA
is "a chronic inflammatory disorder of the airways that causes recurrent
attacks of breathlessness".
The inflammation seems to cause an increase in airway responsiveness
(bronchospasm) to a variety of stimuli, which would cause no such ill
effects in nonasthmatic individuals.
In two-thirds
of the cases, the disease is
"extrinsic" (atopic)
due to IgE and
T
H
2-mediated immune responses to environmental antigens.
In the remaining
one-third
, asthma is
"intrinsic" (non-atopic)
and is
triggered by
non-immune stimuli such as aspirin; pulmonary infections,
especially viral (common cold); psychological stress,
etc.
Pathogenesis
The major etiologic factors of asthma are
1. Genetic predisposition to type I hypersensitivity ("atopy"),
2. Airway inflammation
3. Bronchial hyper-responsiveness to a variety of stimuli.
The role of T
H
2:
the "atopic" form of asthma is associated with an excessive
T
H
2 reaction against environmental antigens. Three cytokines produced by T
H
2
cells are, in particular, responsible for most of the features of asthma;
1. IL-4 stimulates IgE production
2. IL-5 activates eosinophils
3. IL-13 stimulates mucus production
In addition, epithelial cells are activated to produce chemokines that recruit
more T
H
2 cells, eosinophils, & other leukocytes, thus amplifying the
inflammatory reaction.
The role of genetics:
in asthma the bronchial smooth muscle hypertrophy and
the deposition of subepithelial collagen may be the result of a genetically
inherited predisposition.
ADAM33
is one of the genes implicated.
The role of mast cells:
these are part of the inflammatory infiltrate & contribute by secreting
growth factors that
stimulate smooth muscle proliferation.
Atopic asthma,
which usually begins in childhood, is triggered by
environmental antigens (dusts, pollen, animal dander, and foods).
In the airways the inhaled antigens
stimulates induction of T
H
2-type
cells and release of interleukins IL-4 and IL-5
.
This leads to synthesis of
IgE
that binds to mucosal mast cells.
Subsequent exposure of IgE-coated mast cells to the same antigen
causes the release of chemical mediators.
In addition, direct stimulation of subepithelial vagal receptors provokes
reflex bronchocospasm.
These occur within minutes after stimulation thus called
acute, or
immediate, response.
Mast cells release other cytokines that cause the influx of other
leukocytes, including eosinophils. These inflammatory cells
set the stage
for the late-phase reaction, which starts
4 to 8 hours later.
The role of eosinophils
: these cells are particularly important in the late phase.
Their effects are mediated by
1. Major basic protein and eosinophil cationic protein, which directly damage
airway epithelial cells.
2. Eosinophil peroxidase causes tissue damage through oxidative stress.
3. Leukotriene C
4
, which contribute to bronchospasm.
Viral infections of the respiratory tract and inhaled air pollutants such as
sulfur dioxide increase airway hyper-reactivity in both normal & non-atopic
asthmatics. In the latter, however, the bronchial spasm is much more severe
and sustained. It is thought that virus-induced inflammation of the
respiratory mucosa renders the subepithelial vagal receptors more sensitive to
irritants.
The ultimate humoral and cellular mediators of airway obstruction are common
to both atopic and non-atopic variants of asthma, and hence they are treated in a
similar way.
Drug-Induced Asthma:
several drugs provoke asthma, aspirin being the
most striking example. Presumably,
aspirin inhibits the cyclooxygenase
pathway of arachidonic acid metabolism without affecting the lipoxygenase
route, thereby shifting the balance toward bronchoconstrictor leukotrienes.
Occupational Asthma:
this form is stimulated by fumes (epoxy resins,
plastics), organic and chemical dusts (wood, cotton, platinum), gases
(toluene), and other chemicals. Asthma attacks usually develop after repeated
exposure to the inciting antigen(s).
Pathologic features
Gross features:
in fatal cases, the lungs are overdistended because of
overinflation.
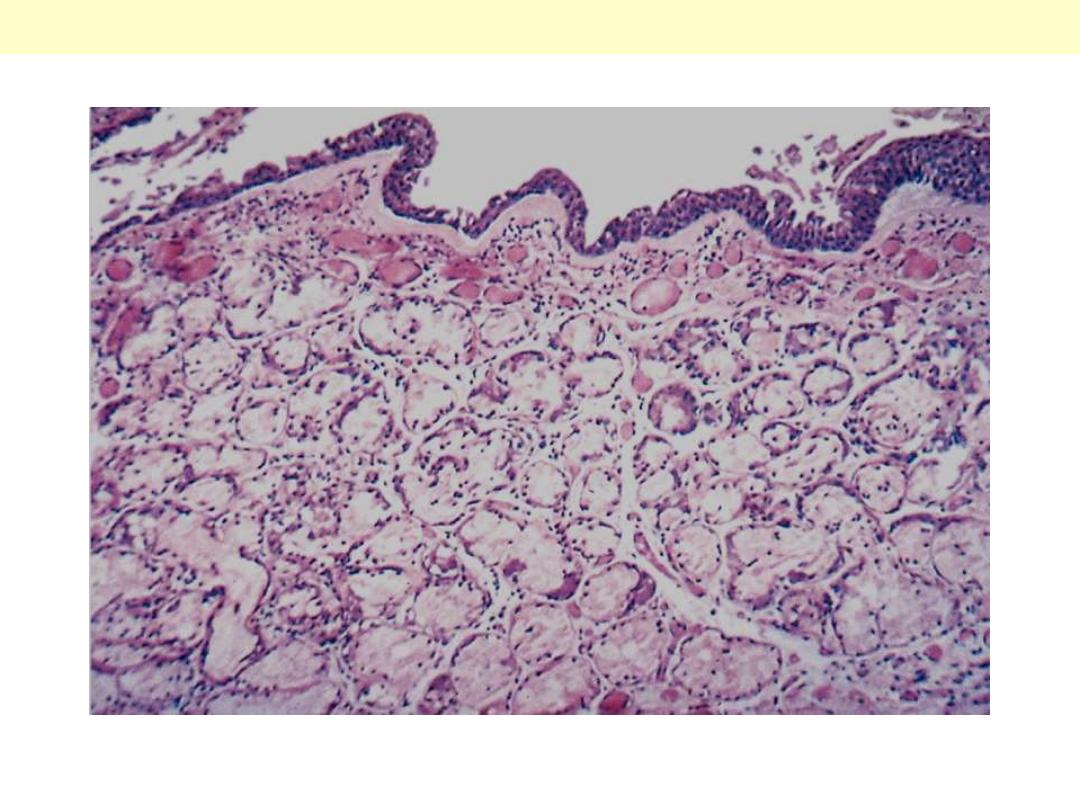
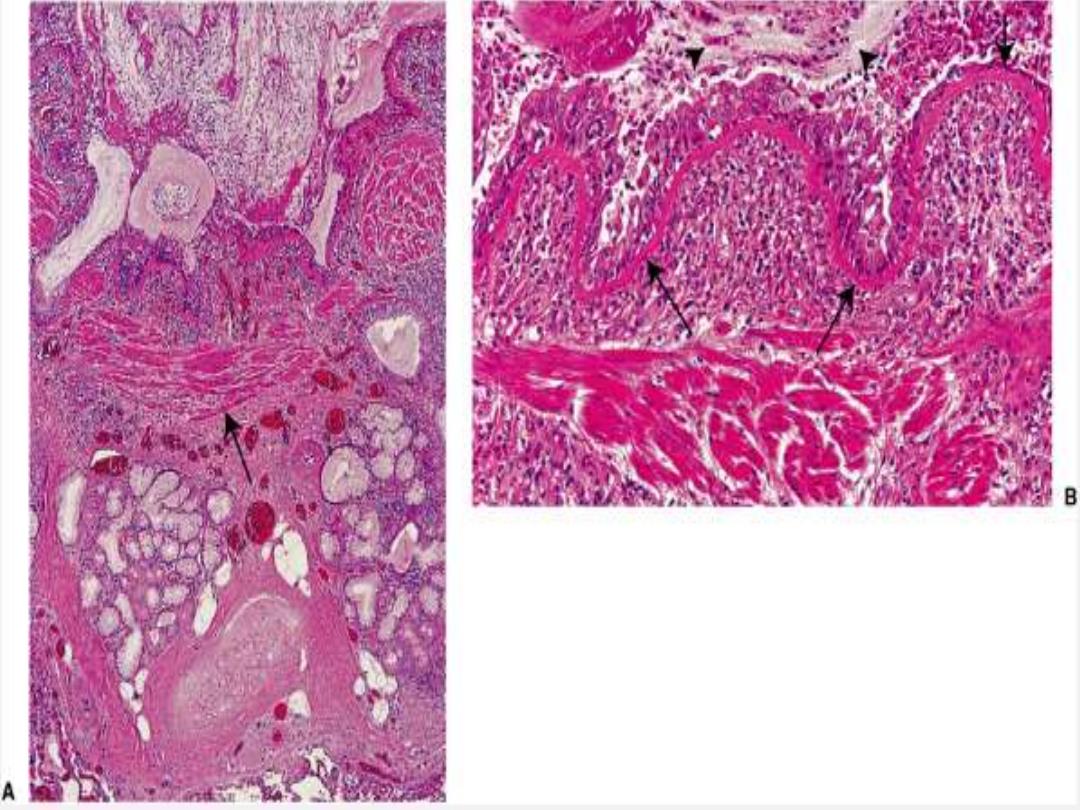
Microscopic features:
There is occlusion of bronchi and bronchioles by thick, tenacious mucous
plugs, which contain numerous eosinophils.
Structural changes of airways include
Thickening of the basement membrane of the bronchial epithelium
Edema and an inflammatory infiltrate in the bronchial walls, with a
prominence of eosinophils and mast cells.
An increase in the size of the submucosal glands.
Hypertrophy of the bronchial muscle cells.

Bronchial asthma
This specimen shows a cross section of a lung from an asthmatic
with obstruction of major airways (bronchi). The lung is collapsed,
due to absorption of air trapped by obstruction of airways (bronchi
and bronchioles). The large and medium-sized bronchioles are
thick-walled and they are filled with greyish-white, jelly-like mucus
plugs. It is these plugs, rather than spasm of airway muscle, that
have caused the partial collapse of the lung, low arterial oxygen and
high carbon dioxide.
Bronchial asthma
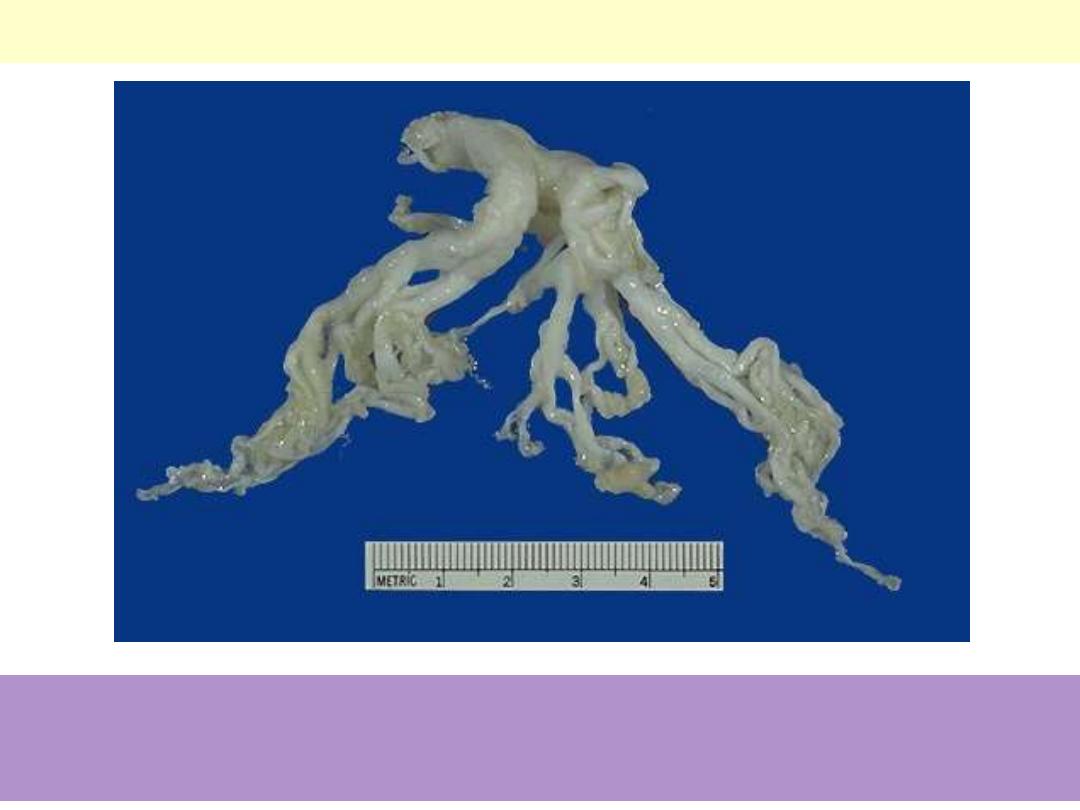
This cast of the bronchial tree is formed of inspissated mucus and was coughed up by a patient during
an asthmatic attack. The outpouring of mucus from hypertrophied bronchial submucosal glands, the
bronchoconstriction, and dehydration all contribute to the formation of mucus plugs that can block
airways in asthmatic patients.
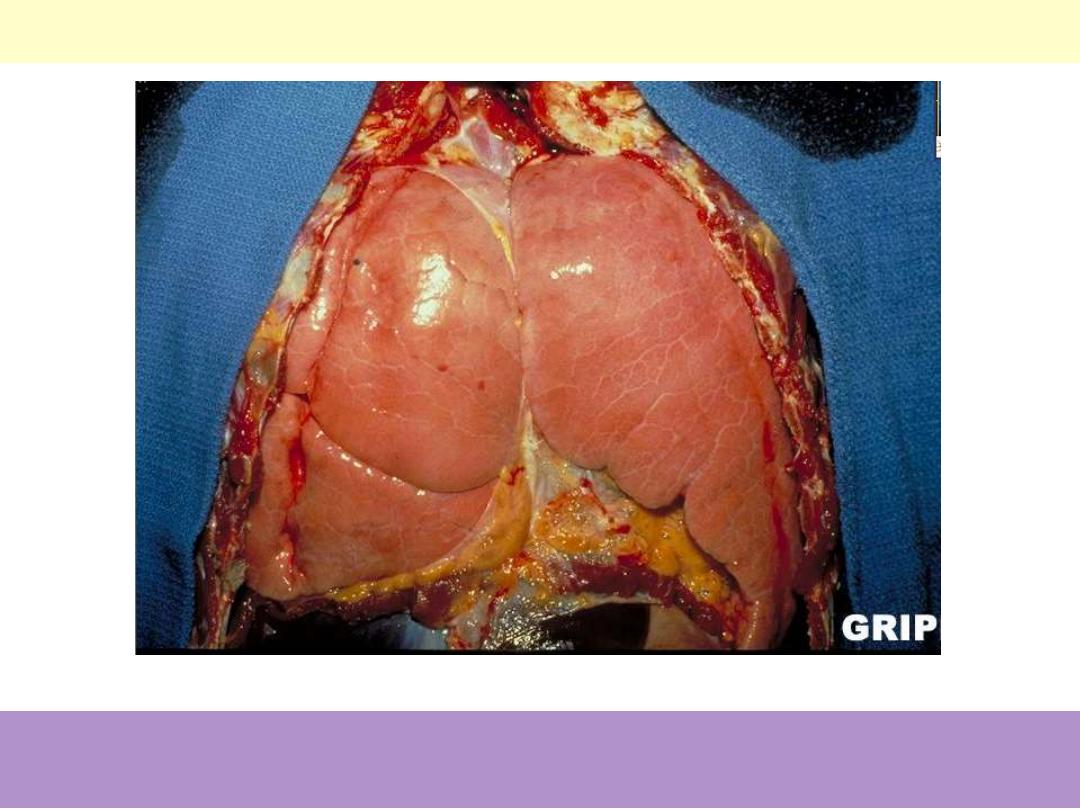
Bronchial asthma: overinflation of the lungs
Status asthmaticus: Note the overinflated lungs secondary to airway
obstruction.
Bronchial asthma
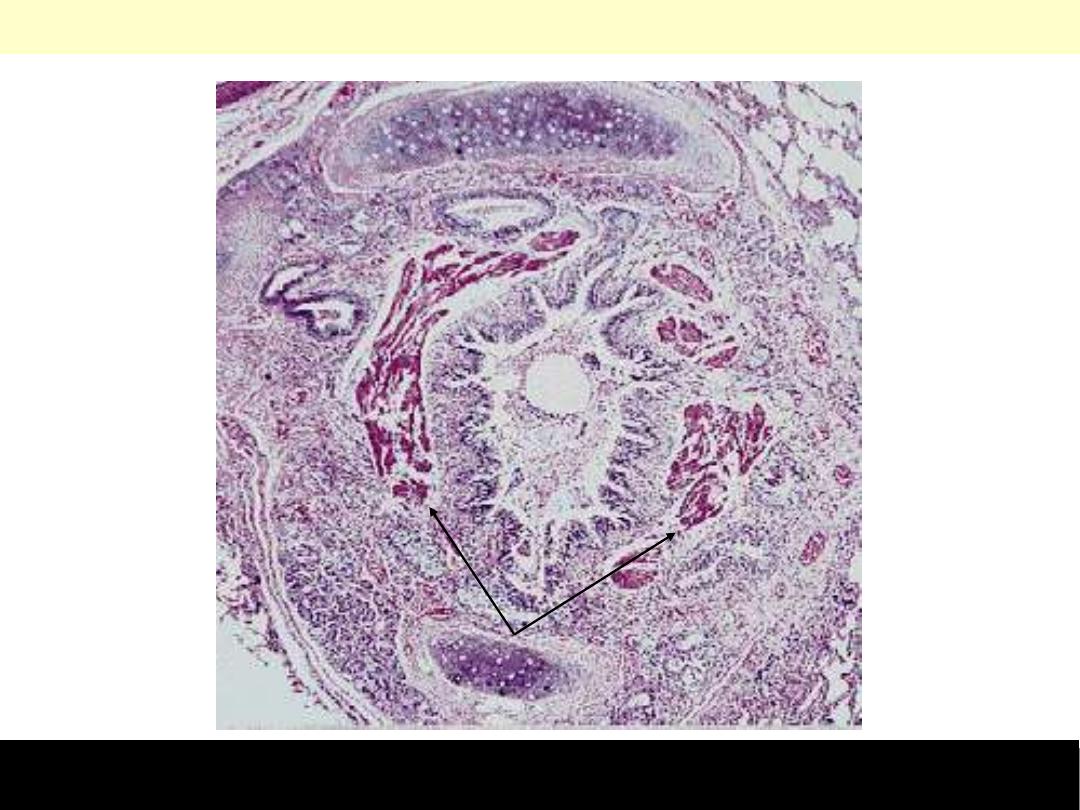
Asthma is characterized by reversible airways obstruction in small airways. The latter is due to a
combination of bronchospasm and mucus plugging. Note mucus plugging of the lumen, smooth muscle
cell prominence (arrow), and the intense inflammatory cell infiltration.
Course & prognosis
An attack of asthma is characterized by severe dyspnea with wheezing;
the chief difficulty lies in expiration.
The victim struggles to get air into the lungs and then cannot get it out,
so that there is progressive hyperinflation of the lungs with air trapped
distal to the bronchi, which are constricted and filled with mucus and
debris.
In the usual case, attacks last from 1 to several hours and subside either
spontaneously or with therapy.
Occasionally a severe paroxysm occurs that does not respond to
therapy and persists for days and even weeks
(status asthmaticus)
.
The associated hypercapnia, acidosis, and severe hypoxia may be fatal.
BRONCHIECTASIS
refers to
"the permanent dilation of bronchi and bronchioles
caused by destruction of the musclulo- elastic supporting tissues,
resulting from or associated with chronic necrotizing infections."
The disease is secondary to persisting infection or obstruction
caused by a variety of conditions.
Once developed, it gives rise to symptoms dominated by
cough
and expectoration of copious amounts of purulent, foul
sputum.
Diagnosis depends on an appropriate history along with
radiographic demonstration of bronchial dilation.
The conditions that most commonly predispose to
bronchiectasis include the following:
1.
Bronchial obstruction
e.g. by tumors, foreign bodies. Under these conditions, the
bronchiectasis is localized to the obstructed segment.
Bronchiectasis can also complicate
atopic asthma and
chronic bronchitis through mucus impaction.
In
cystic fibrosis,
widespread severe bronchiectasis results
from obstruction and infection caused by the secretion of
abnormally viscid mucus.
Kartagener syndrome
, an autosomal recessive disorder, is
frequently associated with bronchiectasis and sterility in
males.
Structural abnormalities of the cilia
impair
mucociliary clearance in the airways, leading to persistent
infections, and reduce the mobility of spermatozoa.
2. Necrotizing, or suppurative, pneumonia
,
particularly with virulent organisms such as
Staphylococcus aureus or Klebsiella spp
., may predispose
to bronchiectasis.
In the past, postinfective bronchiectasis was sometimes a
sequel to the childhood pneumonias that complicated
measles, whooping cough, and influenza
, but this has
substantially decreased with the advent of successful
immunization.
Post-tubercculosis bronchiectasis continues to be a
significant cause in endemic areas.
Pathogenesis
Two processes are crucial and tangled in the pathogenesis of
bronchiectasis:
obstruction and chronic persistent infection.
Either of
these two processes may come first.
Normal clearance mechanisms are impaired by obstruction, so
secondary infection soon follows; conversely, chronic infection in time
causes damage to bronchial walls, leading to weakening and dilation.
For example,
obstruction caused by a bronchogenic carcinoma
or a
foreign body impairs clearance of secretions, providing a fertile soil for
superimposed infection.
The resultant inflammatory damage to the bronchial wall and the
accumulating exudate further distend the airways, leading to
irreversible dilation.
A persistent necrotizing inflammation in the bronchi or bronchioles
may cause obstructive secretions, inflammation throughout the wall
(with peribronchial fibrosis and traction on the walls), and eventually
dilation.
Gross features
Usually there is bilateral involvement of the lower lobes
When tumors or aspiration of foreign bodies lead to bronchiectasis, involvement
may be sharply localized to a single segment of the lungs.
The airways may be dilated up to 4 times their usual diameter and can be
followed almost to the pleural surfaces
Microscopic features
There is intense acute and chronic inflammatory exudate within the walls of the
bronchi and bronchioles.
The desquamation of lining epithelium causes extensive areas of ulceration.
When healing occurs, the lining epithelium may regenerate completely.
In chronic cases there is fibrosis of the bronchial and bronchiolar walls and
peribronchiolar areas.
In some instances, the necrotizing inflammation destroys the bronchial or
bronchiolar walls and forms a
lung abscess.
In cases of severe, widespread bronchiectasis
hypoxemia, hypercapnia,
pulmonary hypertension, and (rarely) cor pulmonale occur.
Metastatic brain abscesses and reactive amyloidosis are other, less frequent
complications.
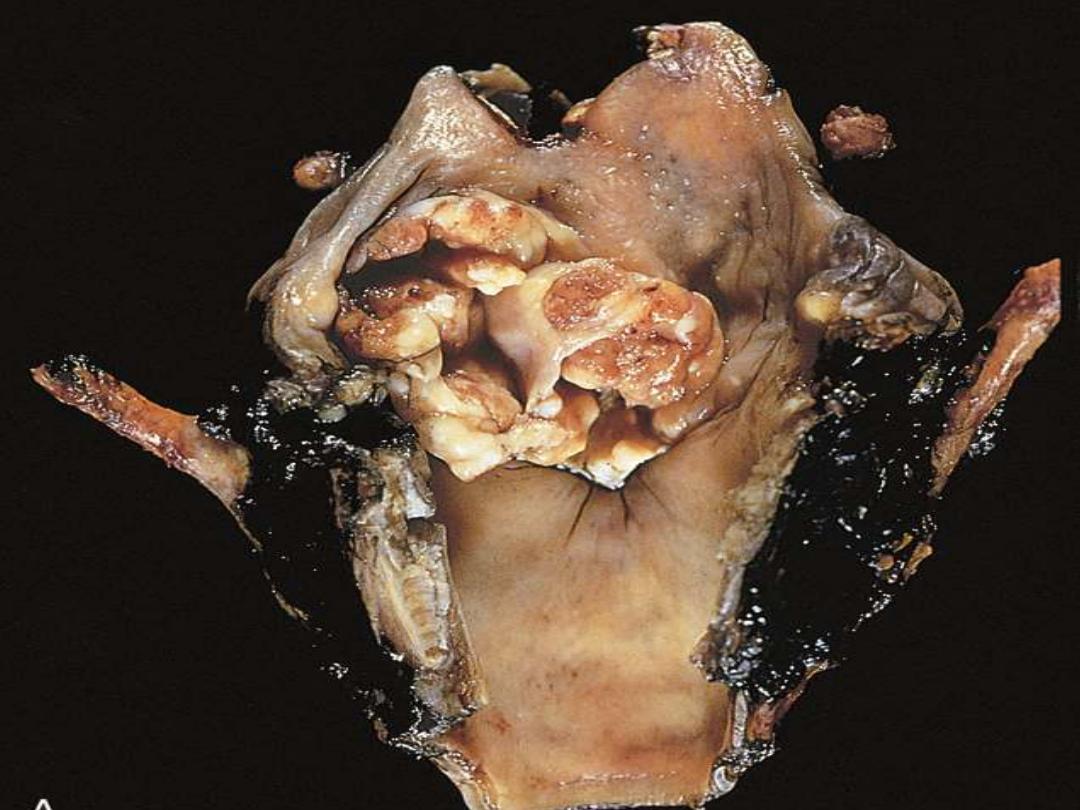
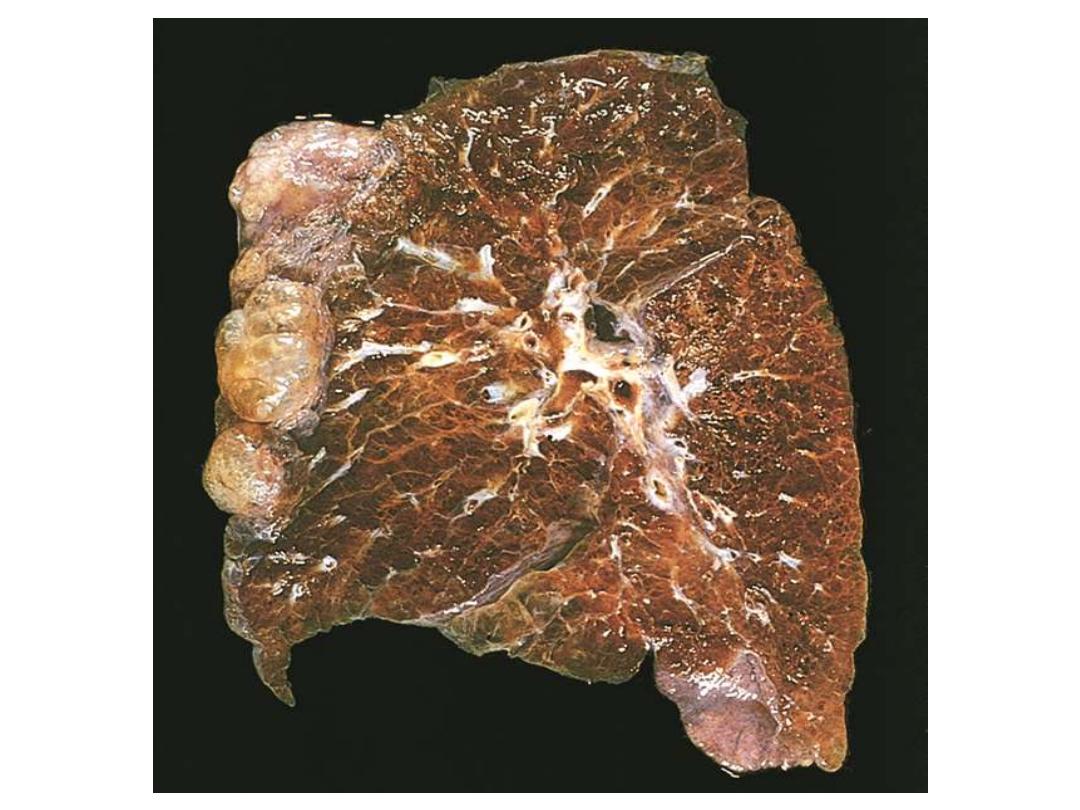
Bronchiectasis
Extensive bilateral bronchiectasis; the massively dilated bronchi extend almost to the pleura. Widespread
bronchiectasis is typical for patients with cystic fibrosis who have recurrent infections and obstruction of
airways by mucus throughout the lungs.
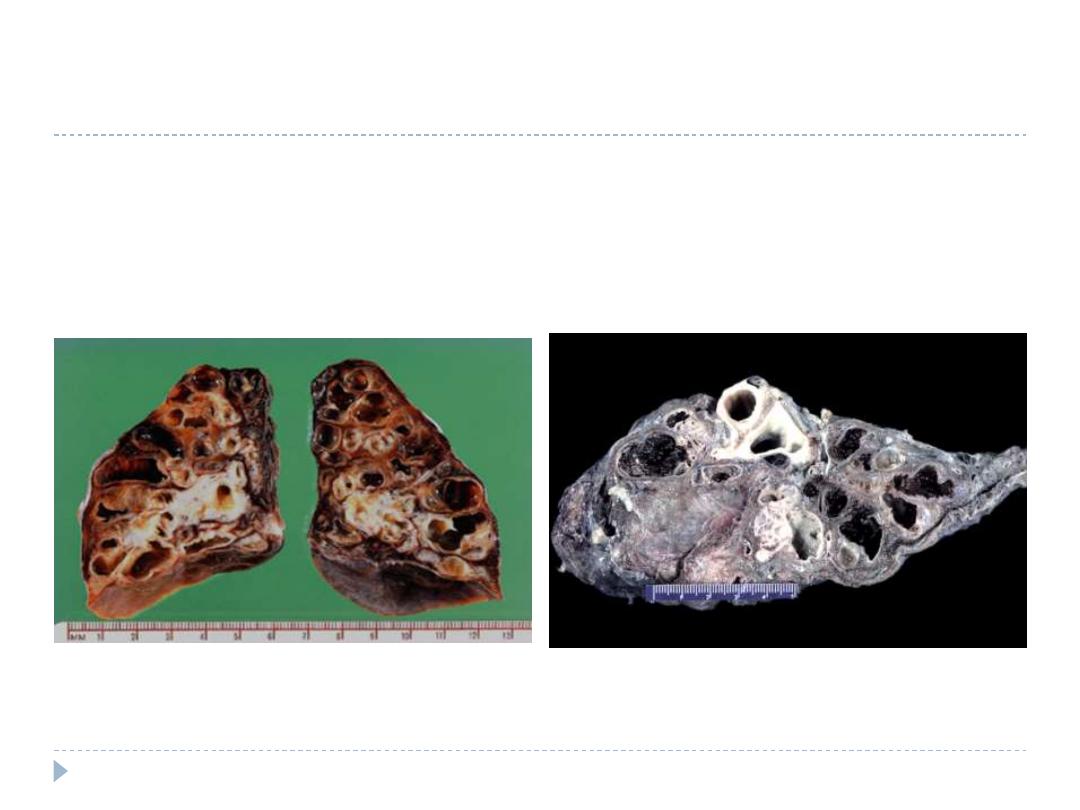
Extensive bilateral bronchiectasis; the massively
dilated bronchi extend almost to the pleura.
Widespread bronchiectasis is typical for patients
with cystic fibrosis who have recurrent infections
and obstruction of airways by mucus throughout the
lungs.
Cross-section of lung demonstrating
dilated bronchi extending almost to the
pleura.
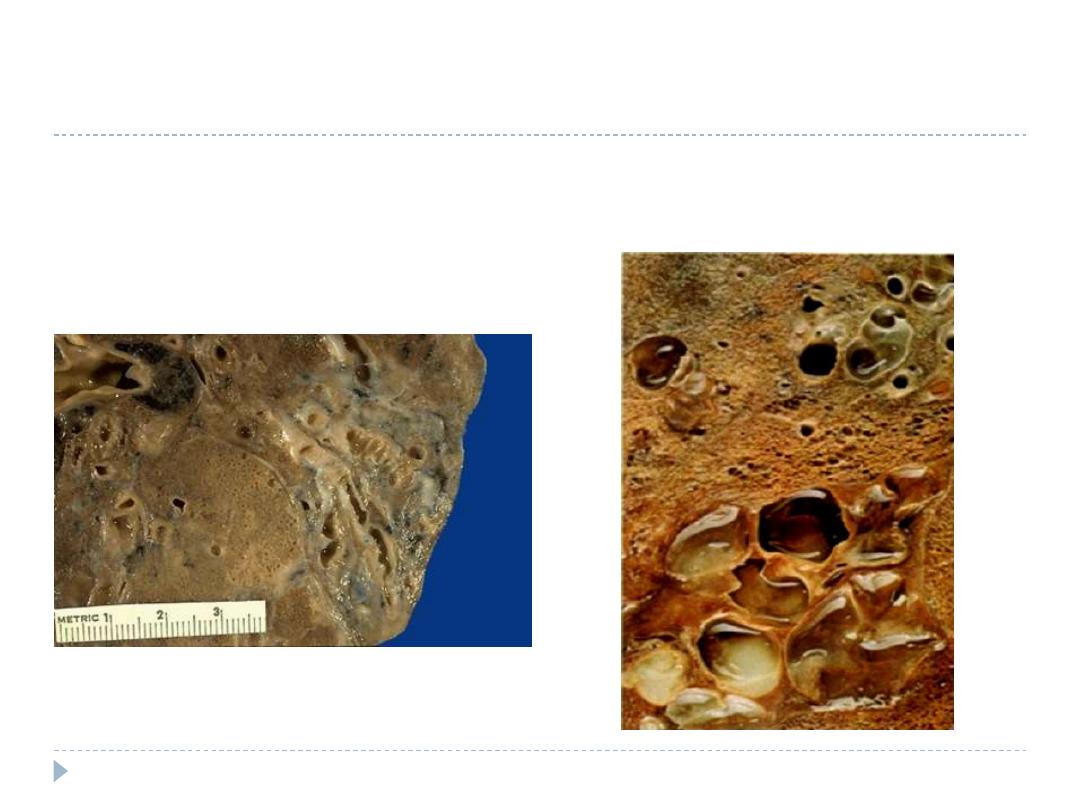
A closer view demonstrates the focal area of dilated bronchi with
bronchiectasis. Bronchiectasis tends to be localized with disease
processes such as neoplasms and aspirated foreign bodies that block a
portion of the airways. Note that the dilated bronchi can be traced down
to the pleura.
Segmental distribution of bronchiectasis. The bronchi
are dilated into cavities. The dilated bronchi are filled
with gelatinous inspissated mucus.
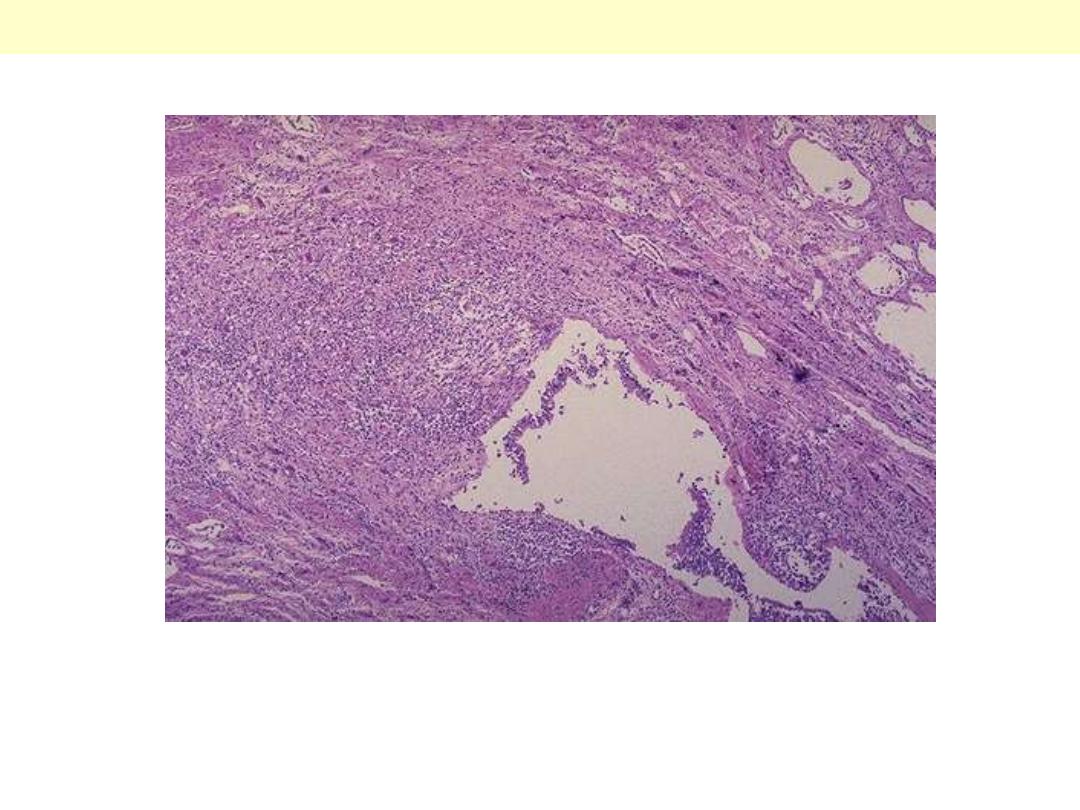
The mid lower portion of this photomicrograph demonstrates a dilated bronchus in which the mucosa
and wall is not clearly seen because of the necrotizing inflammation with destruction.
Bronchiectasis