
Hemodynamic Disturbances
Abdulkareem Mohammad Jaafar
MB. ChB. PhD. (Hematopathology)
Department of Pathology
College of Medicine/ University of Baghdad

Edema
refers to:
Increased fluid in the interstitial
tissue spaces.
Mechanisms of edema:
●Increased capillary pressure.
●Diminished colloid osmotic
pressure.
●Lymphatic obstruction.
●Sodium retention.

The edema fluid may be either:
A transudate:
Occurs with:
●Volume or pressure overload.
●Reduced plasma protein.
It is a protein-poor fluid.
An exudate:
Occurs with:
●Increased vascular permeability, due to
inflammation (inflammatory edema).
It is a protein-rich fluid.

Pitting edema
Ankle region
The edema fluid is in the subcutaneous tissue. Finger pressure over edematous
subcutaneous tissue leads to pitted depression hence the name pitting edema.
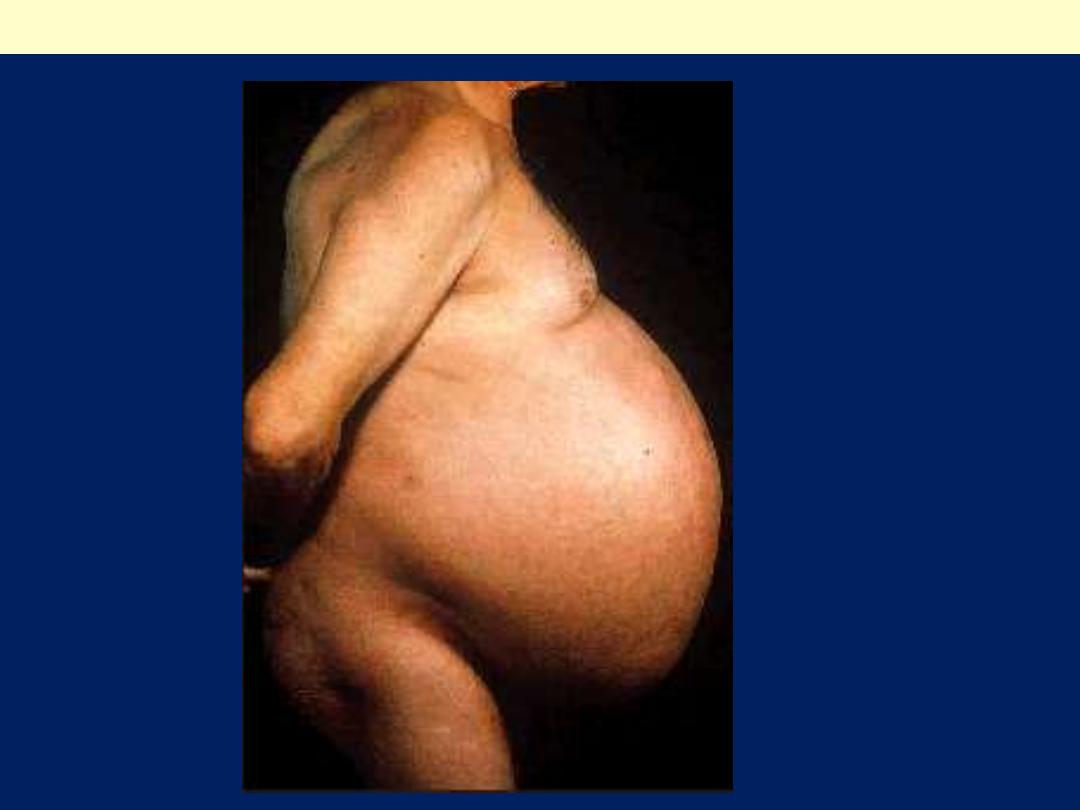
Ascites (severe form) complicating liver cirrhosis

The principal causes of edema are:
●Increased Hydrostatic Pressure
This is either:
►Localized edema:
this is due to
Localized increase in intravascular pressure.
Examples of localized edema are
1. Portal hypertension caused by liver cirrhosis. This produces
ascites.
2. Pressure of gravid uterus on the iliac veins produces edema of
the lower limbs.
3. Acute left ventricular failure causes acute pulmonary edema.
4. Thrombosis of major veins of the lower extremity can cause
edema restricted to the distal portion of the affected leg.
5. Incompetence of venous valves secondary to varicose veins.
►Generalized edema:
this is due to
Generalized increases in intravascular pressure.
Occur most commonly in congestive heart failure, with
involvement of the right ventricular cardiac function.

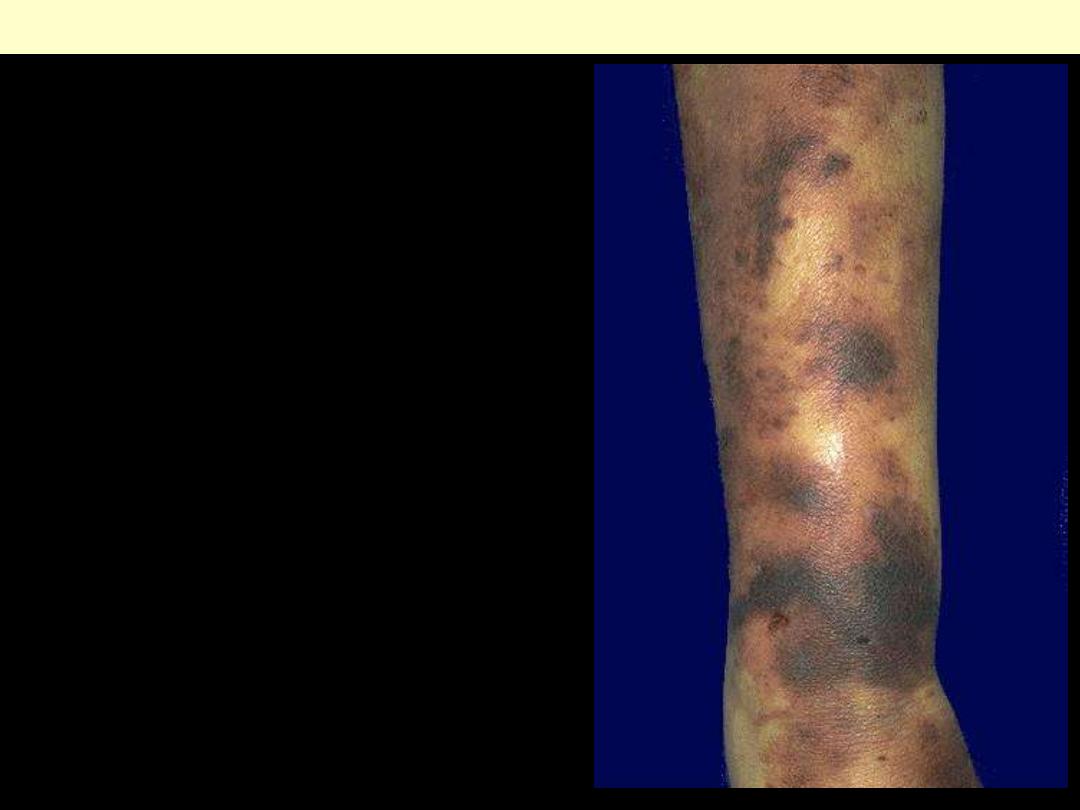
A 35-year-old woman has a
massively swollen Rt. leg.
Deep vein thrombosis (DVT)

The principal causes of edema are:
●Reduced Plasma Osmotic Pressure
Reduced osmotic pressure occurs when there is:
■Reduced synthesis of albumin.
■Increased loss of albumin from the circulation.
Albumin loss is exemplified by:
►The nephrotic syndrome
(glomerular
capillary walls become leaky) that is associated
with generalized edema.
Reduced albumin synthesis occurs in:
►The setting of diffuse liver diseases
(e.g.,
cirrhosis) or protein malnutrition.
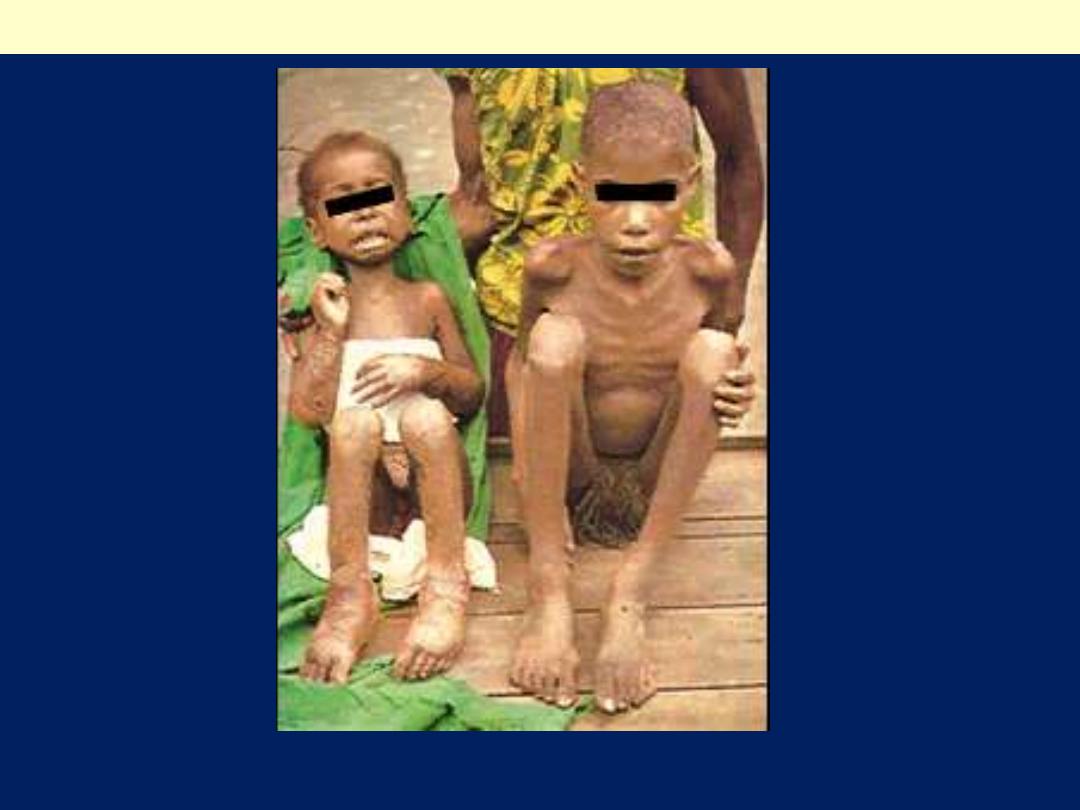
Note edema of the feet in the child on the Lt
Kwashiorkor

The principal causes of edema are:
●Lymphatic Obstruction
Edema due to lymphatic obstruction is usually:
Localized.
It can result from:
■Inflammatory or
■Neoplastic obstruction.
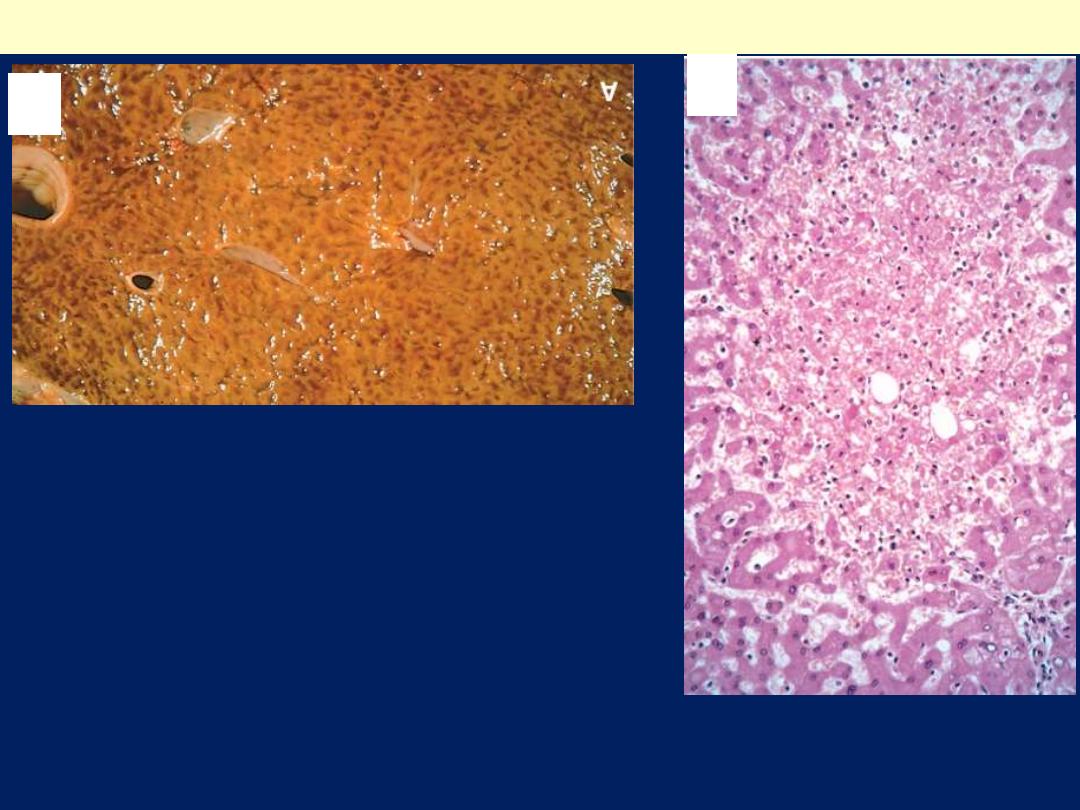
In breast carcinoma
infiltration and obstruction of
superficial lymphatics can cause edema of the
overlying skin, the so-called:
Peau d'orange (orange peel) appearance.
Such a finely pitted surface results from an
accentuation of depressions in the skin at the site of
hair follicles.
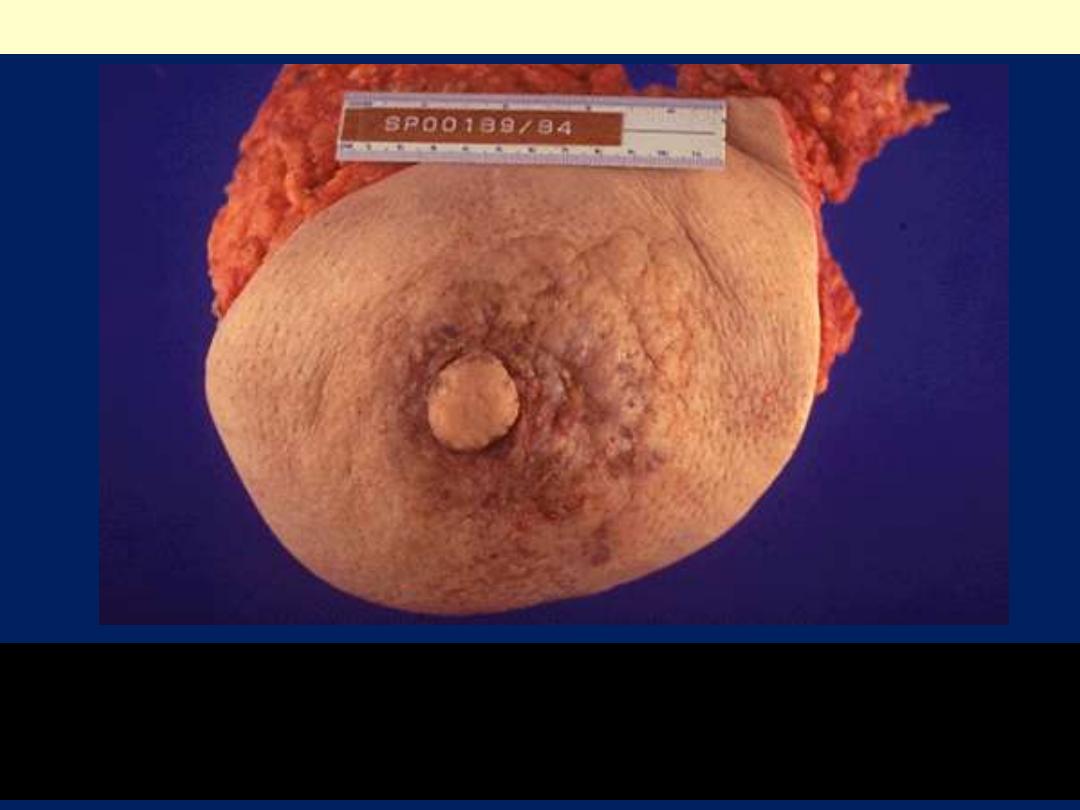
Note the gross cutaneous changes associated with an underlying carcinoma of
breast. These are due to dermal lymphatic invasion by carcinoma that has resulted
in the grossly thickened, erythematous, and rough skin surface with the
appearance of an orange peel ("peau d'orange").
Edema: Lymphatic Obstruction

The principal causes of edema are:
●Sodium and Water Retention
Increased salt-with the obligate
accompanying water-causes:
■Increased hydrostatic pressure.
■Reduced vascular osmotic pressure.
Salt retention can occur with:
■Any impairment of renal function
, as in
poststreptococcal glomerulonephritis and
acute renal failure.
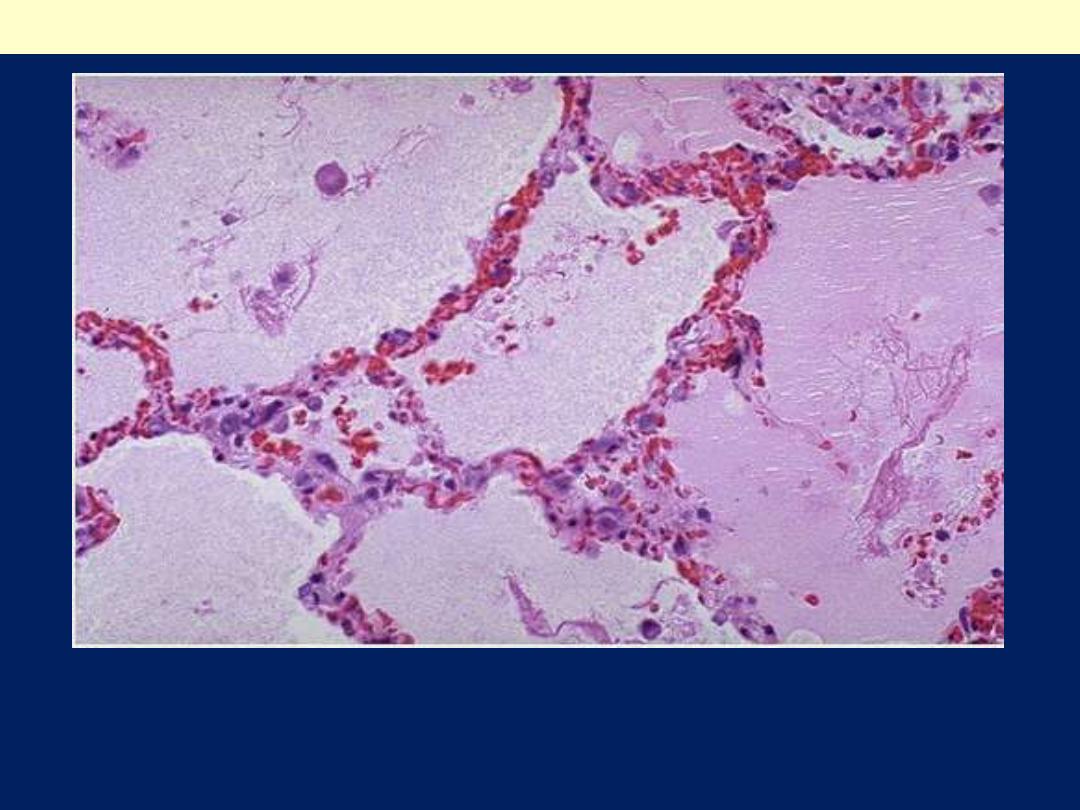
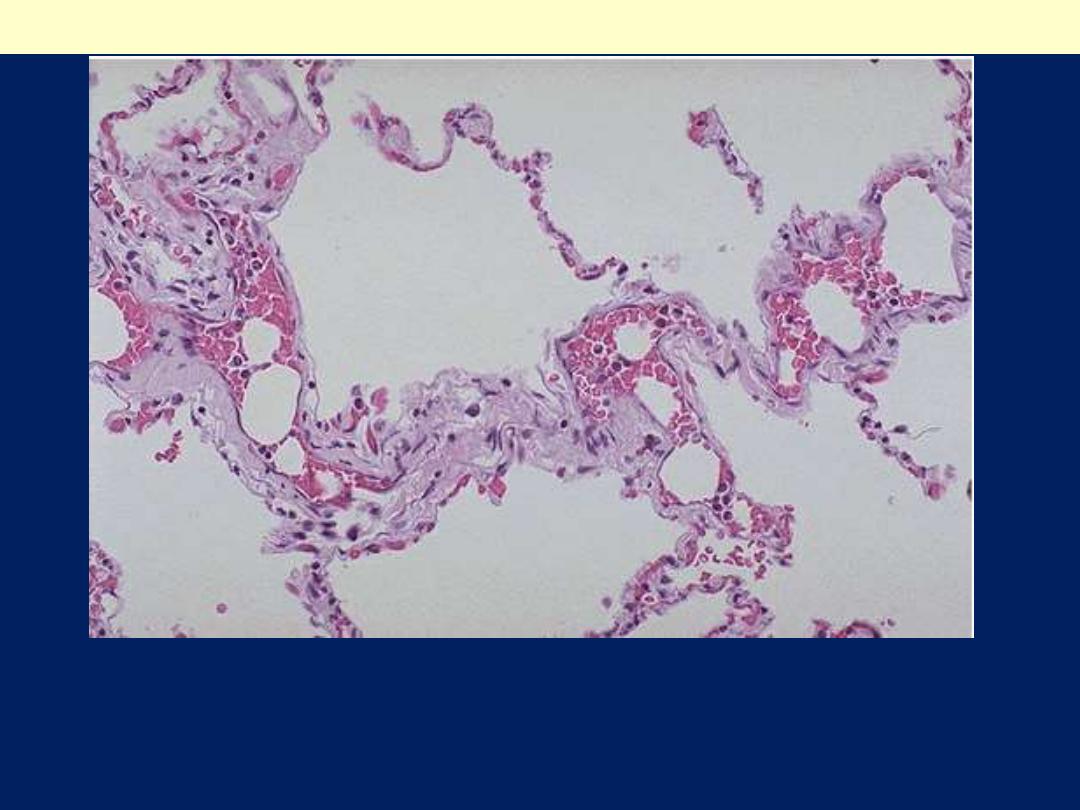
The alveolar spaces are filled with pale pink amorphous fluid. Note
the congested septal capillaries.
Pulmonary edema (a case of Lt heart failure)

?

Hyperemia and Congestion
The terms hyperemia and congestion both indicate:
A local
increased volume of blood in a particular
tissue.
●Hyperemia is an:
►Active process
resulting from:
►Augmented blood flow due to arteriolar dilation.
●Congestion is:
►A passive process
resulting from:
►Impaired venous return out of a tissue.
Congestion may occur:
►Systemically
, as in cardiac failure, or
►It may be local
, resulting from an isolated venous
obstruction.
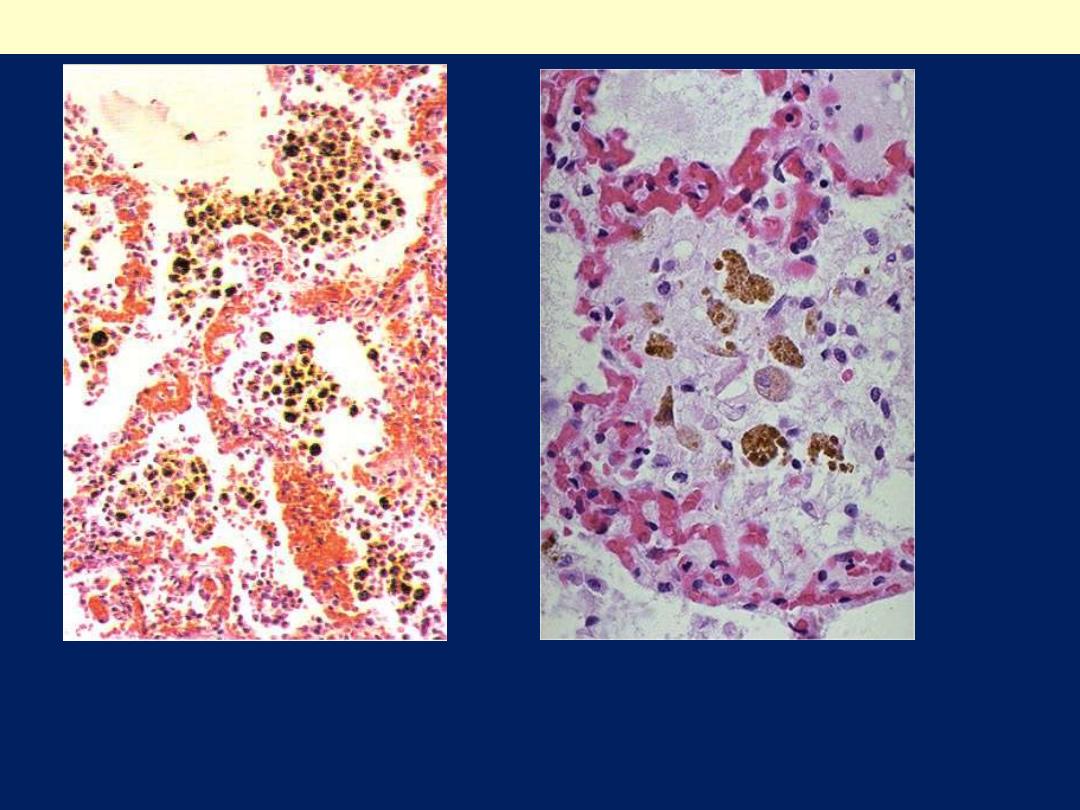
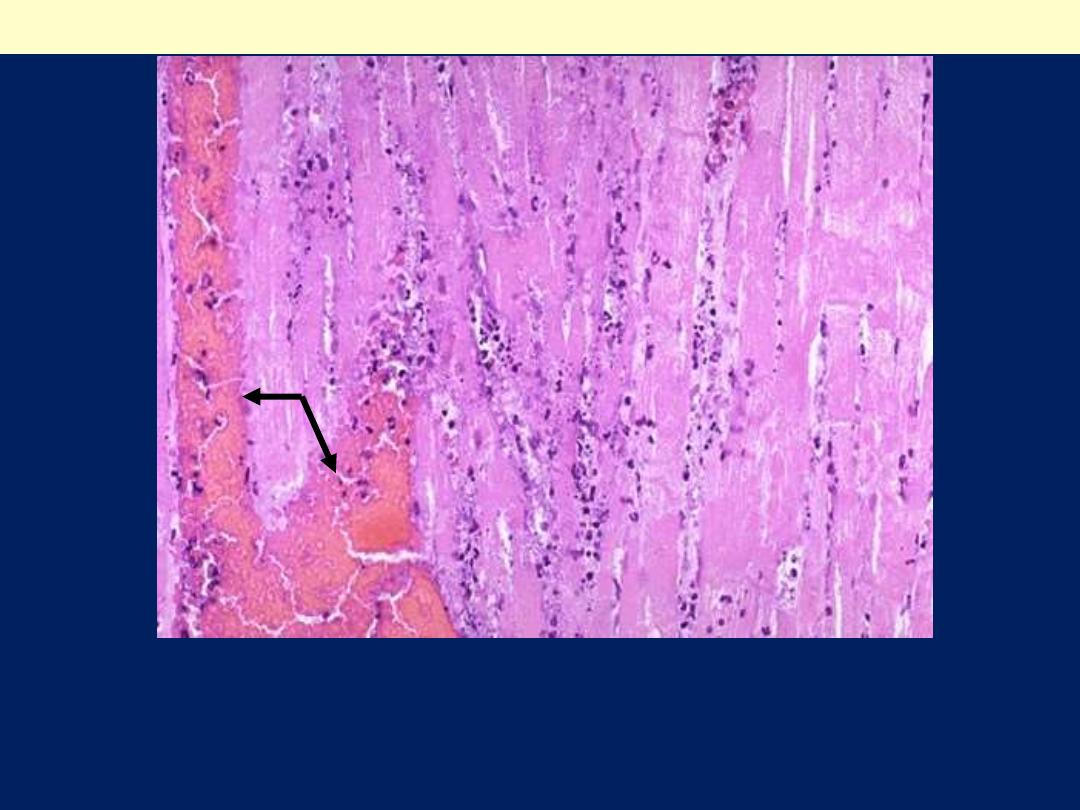
There is engorgement of septal capillaries. Hemosiderin-laden
macrophages (heart failure cells). The hemosiderin granules within
cytoplasm of macrophages appear brownish)
CVC lung
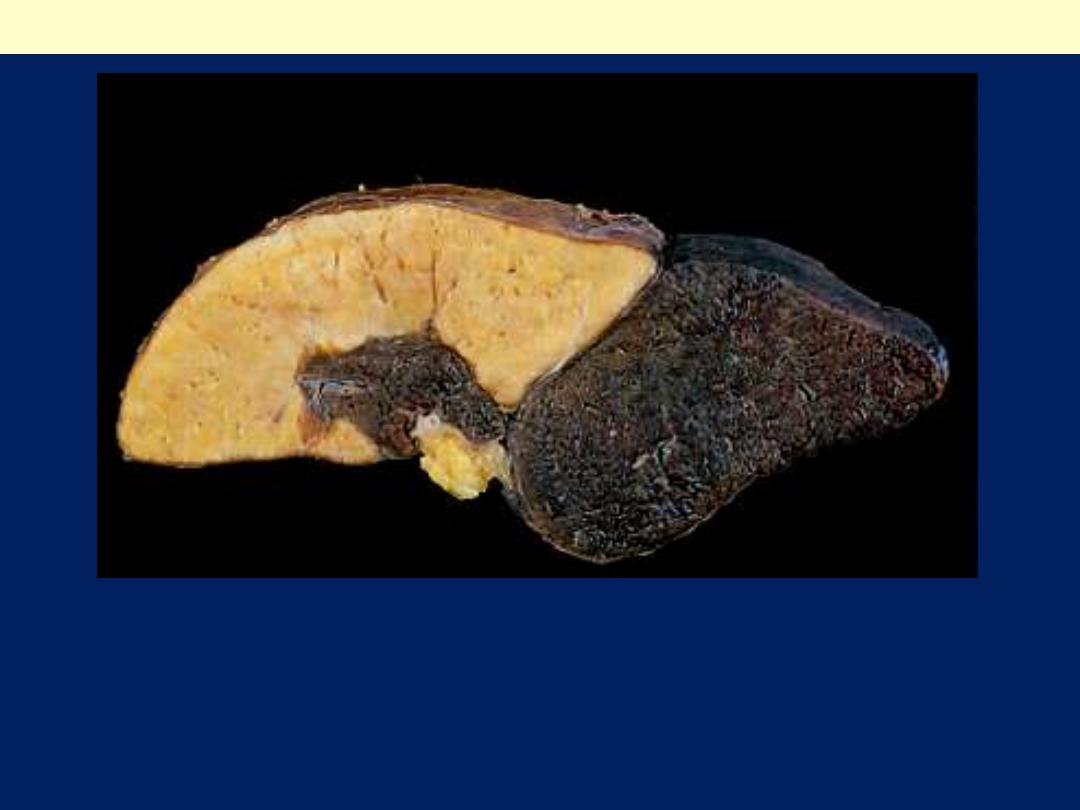
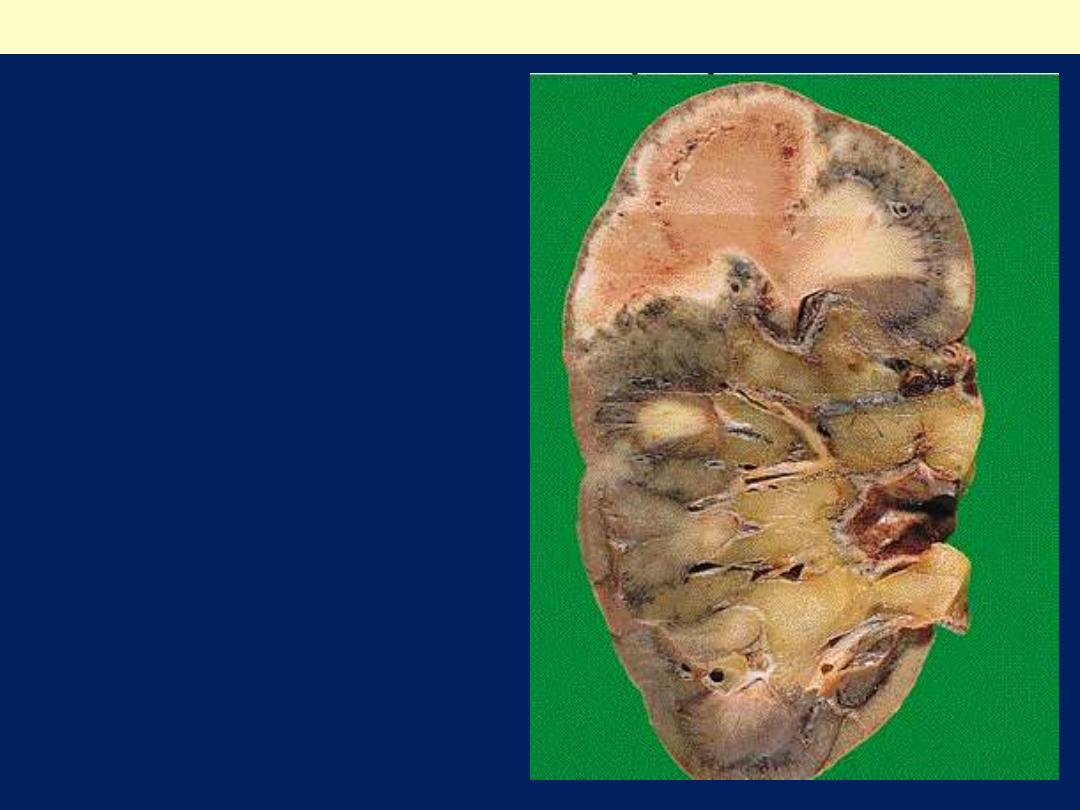
A: Central areas are red and
slightly depressed compared with
the surrounding tan viable
parenchyma.
B: Centrilobular necrosis with
degenerating hepatocytes and
hemorrhage.
Liver with chronic passive congestion and hemorrhagic necrosis
A
B

Hemorrhage:
Hemorrhage is the escape of blood from the vasculature into
surrounding tissues, a hollow organ or body cavity, or to the
outside.
Hemorrhage is most often caused by trauma.
Hematoma:
This localized hemorrhage occurs within a tissue or organ.
Hemothorax, hemopericardium, hemoperitoneum, and
hemarthrosis:
Hemorrhage may occur in the pleural cavity, pericardial sac,
peritoneal cavity, or a synovial space, respectively.
Petechial hemorrhages, petechiae, or purpura:
These small, punctate hemorrhages occur in the skin, mucous
membranes, or serosal surfaces.
Ecchymosis:
This diffuse hemorrhage is usually in skin and subcutaneous
tissue.
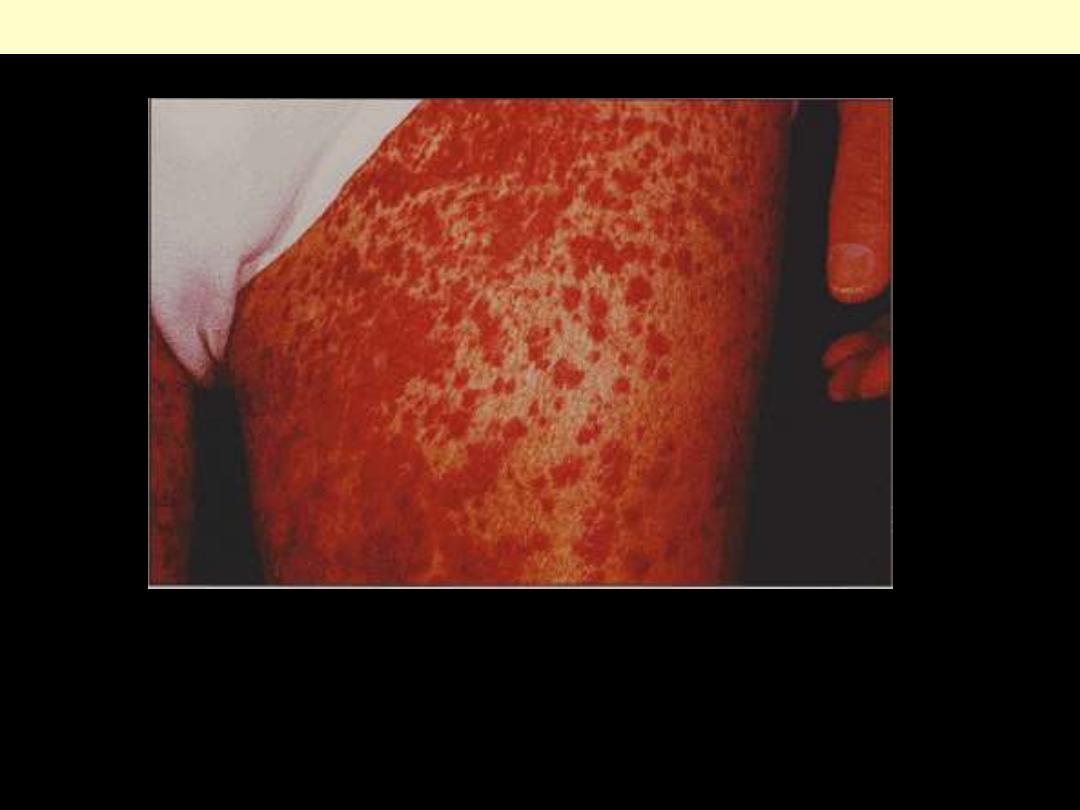
Numerous raised 3- to 5-mm palpable hemorrhages of the skin. In
this case purpura is due to small-vessel vasculitis.
Purpura
Petechiae are classically found
when a coagulopathy is due to a
low platelet count. They can also
appear following sudden hypoxia.
Petechial hemorrhages seen on the epicardium of the heart
The blotchy areas of hemorrhage in
the skin are called ecchymoses
(singular ecchymosis). Ecchymoses
are larger than petechiae. They can
appear with coagulation disorders.
Ecchymoses
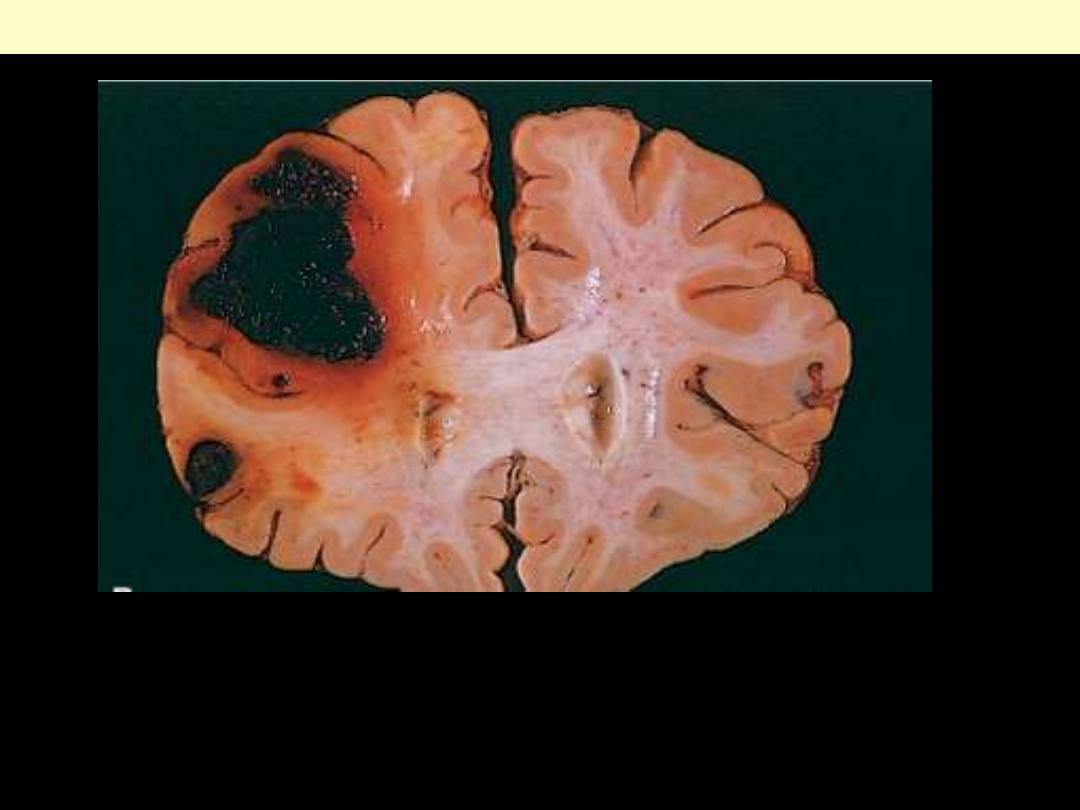
Even relatively inconsequential volumes of hemorrhage in a critical
location, or into a closed space (such as the cranium), can have fatal
outcomes.
Intracerebral hemorrhage
?

Thrombosis is:
The formation of a blood clot inside a blood
vessel.
Both hemostasis and thrombosis involve
three components:
●Vascular wall.
●Platelets .
●Coagulation cascade.
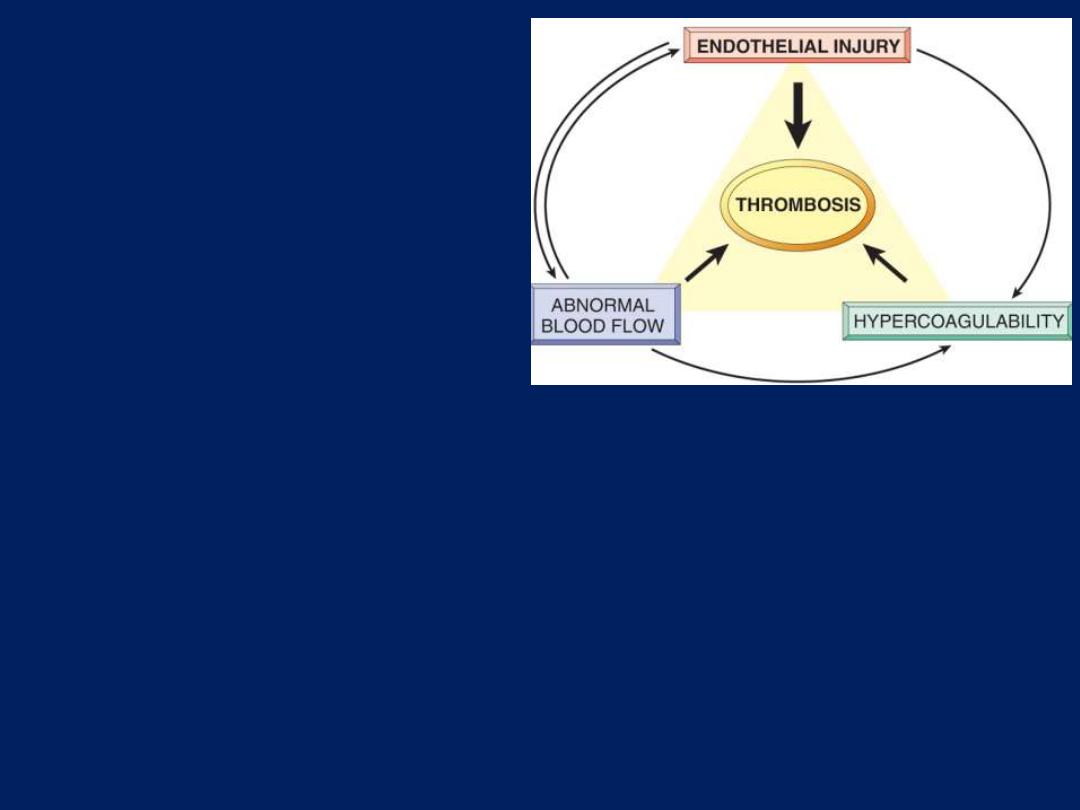
Pathogenesis of Thrombosis:
Three predisposing factors for
thrombus formation
(Virchow's
triad):
1. Endothelium injury:
This is a
dominant predisposing factor,
since endothelial loss by alone
can lead to thrombosis.
It is particularly important for
thrombus formation occurring
in:
The heart or in the arterial
circulation,
where the normally
high flow rates might otherwise
interfere with clotting by
preventing platelet adhesion &
diluting coagulation factors.
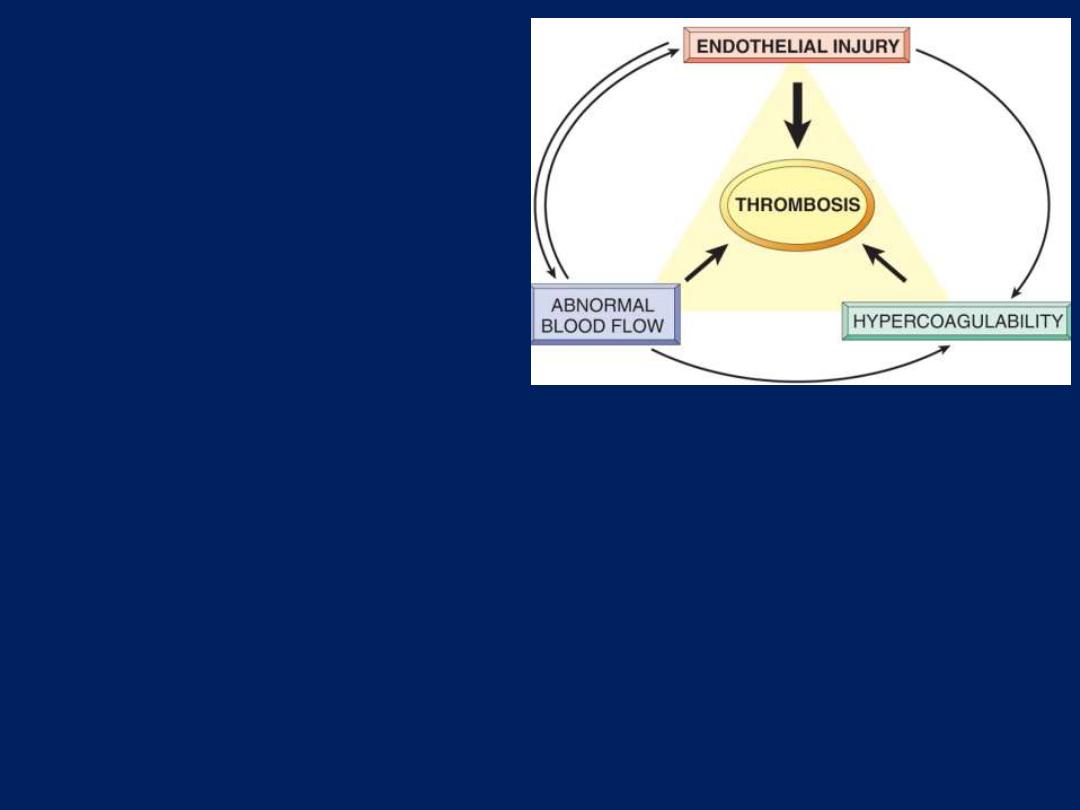
2. Alterations in Normal Blood
Flow:
●Turbulence contributes to:
Arterial and cardiac
thrombosis.
●Stasis is a major contributor to
the development of
venous
thrombi
.
Stasis and turbulence:
1. Disrupt laminar flow and bring
platelets into contact with the
endothelium.
2. Prevent dilution of activated
clotting factors by fresh-flowing
blood.
3. Retard the inflow of clotting
factor inhibitors and permit the
buildup of thrombi.
4. Promote endothelial cell
activation.
3. Hypercoagulability:
Hypercoagulability
generally contributes
less frequently to
thrombosis.
It is defined as:
Any alteration of the
coagulation pathways
that predisposes to
thrombosis.
It is be divided into:
●Primary (Genetic).
●Secondary (Acquired).

The main leg veins are filled with fresh thrombosis, from an elderly
man who died of a massive pulmonary embolus.
Deep vein thrombosis: leg veins
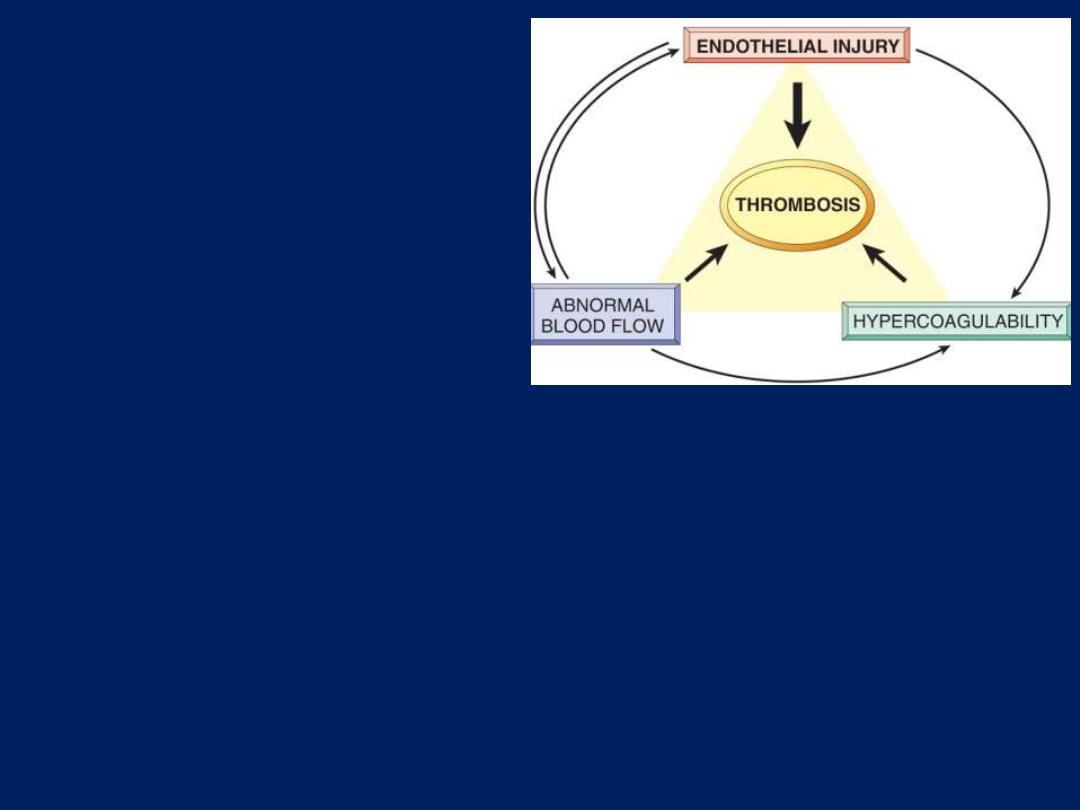
Cardiac auricle thrombus
showing lines of Zahn
Thrombi can have grossly (and
microscopically) apparent
laminations called lines of Zahn;
these represent pale platelet and
fibrin layers alternating with
darker erythrocyte-rich layers.
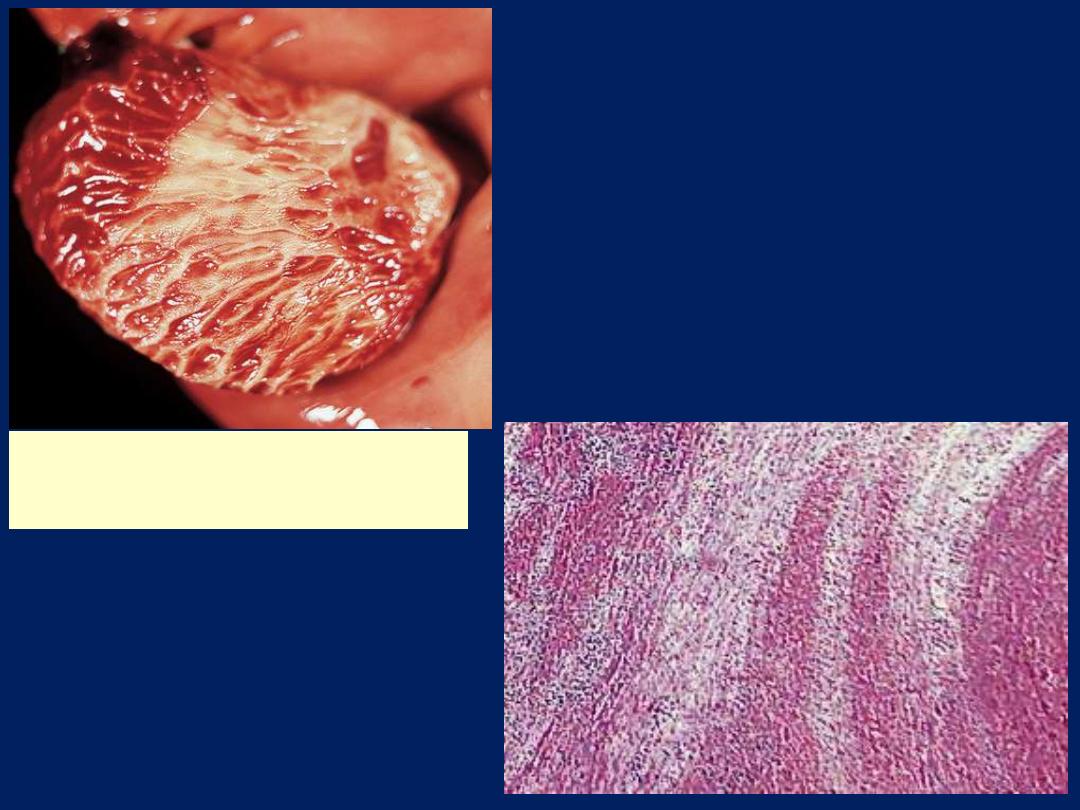
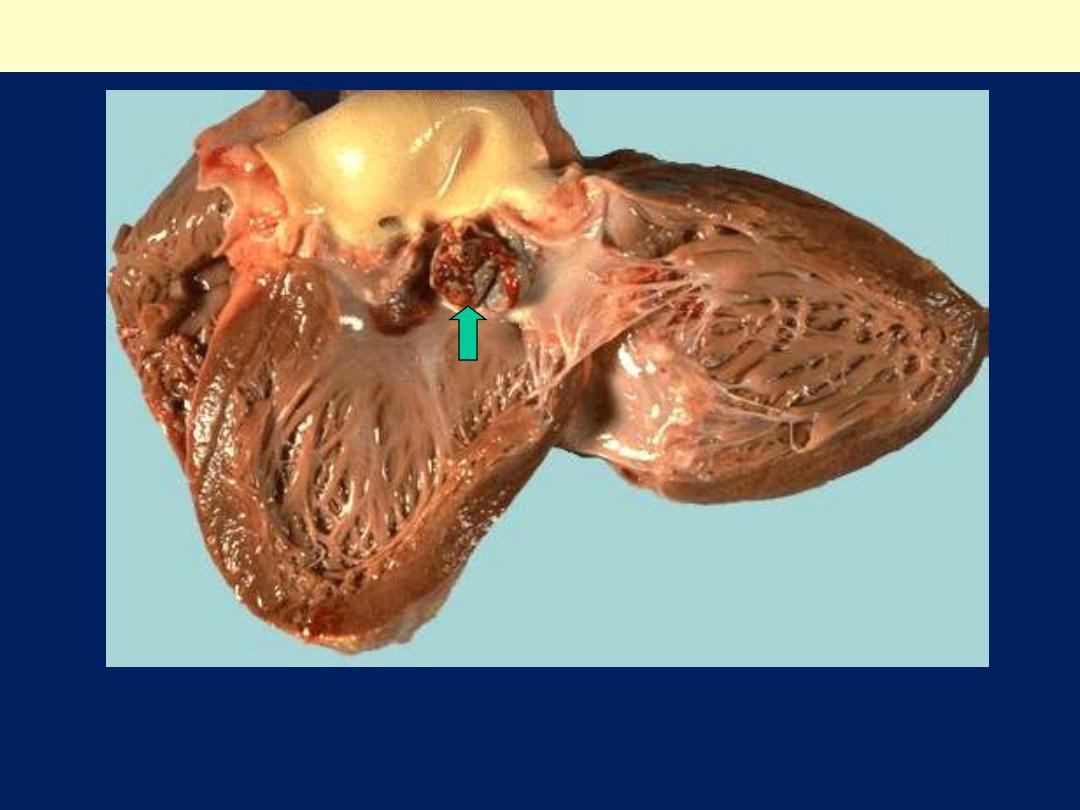
Thrombus in the left and right ventricular apices, overlying white
fibrous scar.
Mural thrombi

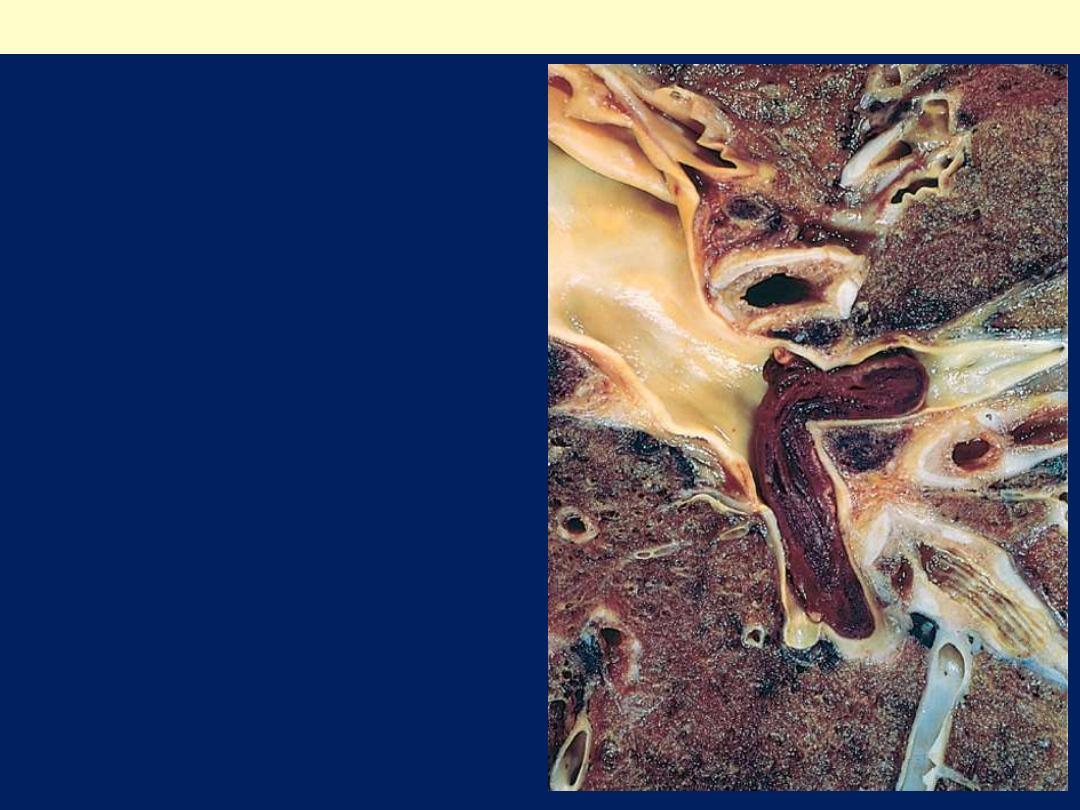
Laminated thrombus
in a dilated abdominal
aortic aneurysm
(arrow).
Mural thrombi
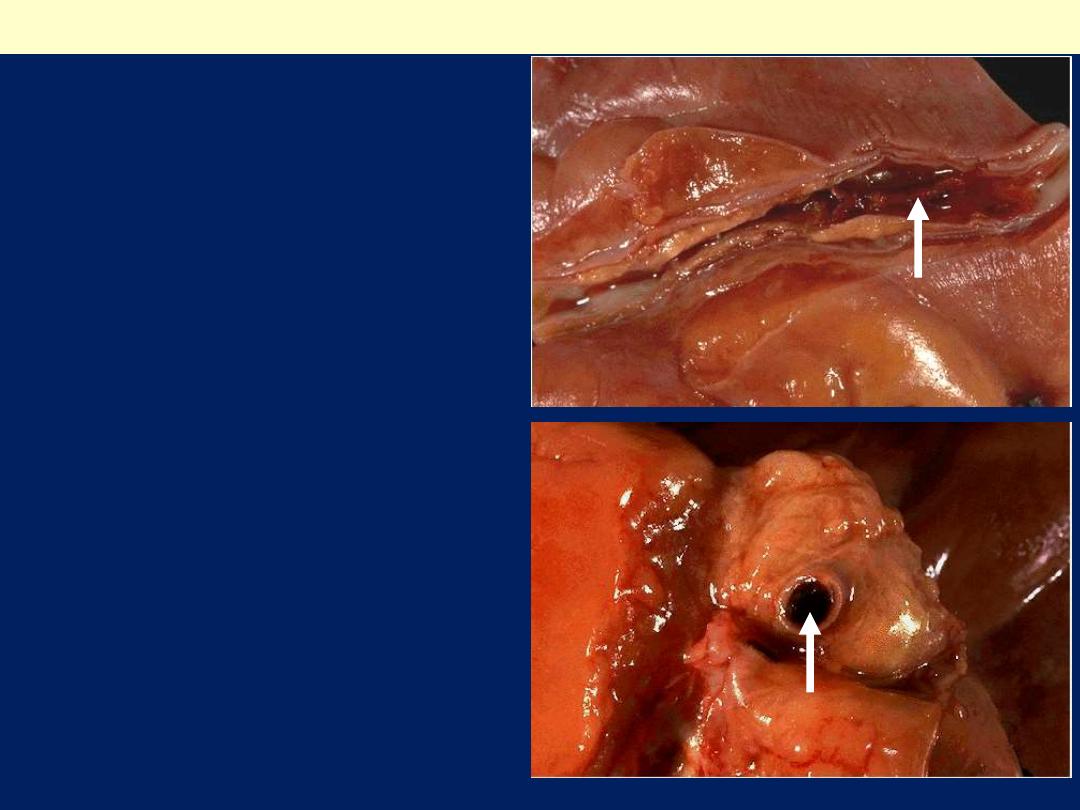
An occlusive
thrombus within the
anterior descending
branch of the Lt.
coronary artery.
Coronary atherosclerosis + superadded thrombosis
Coronary atherosclerosis + superadded thrombosis
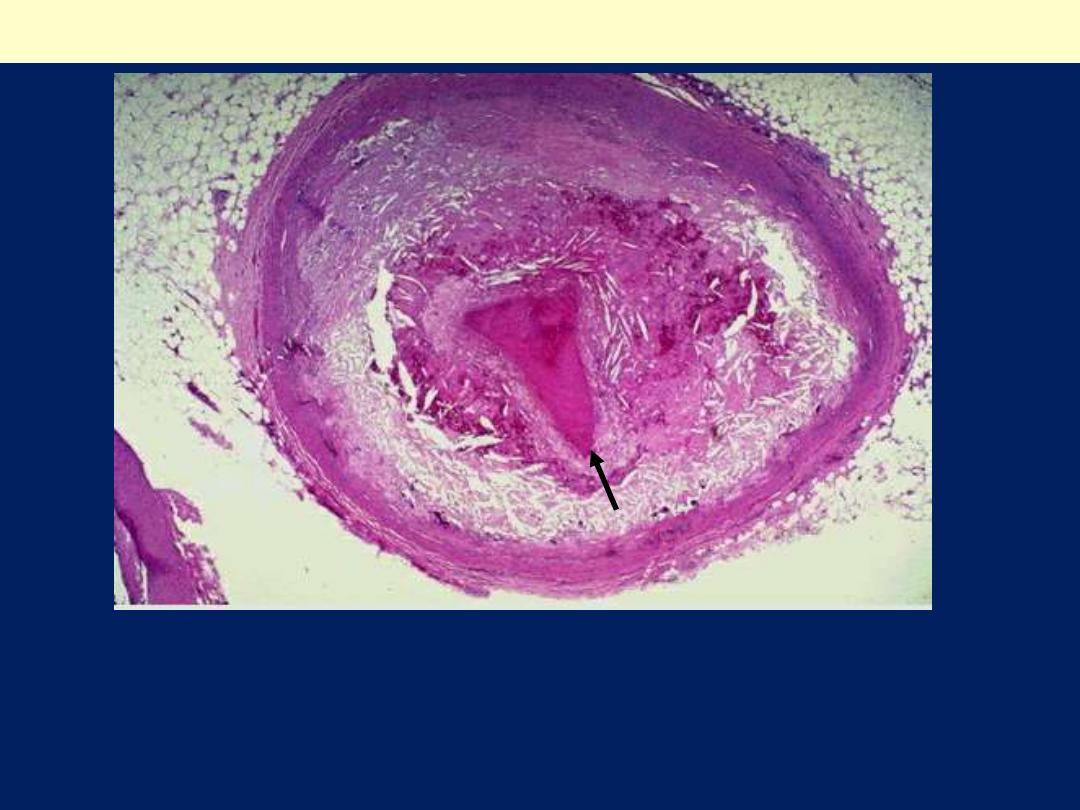
4
The narrowed lumen is occupied by an occlusive thrombus
(arrow). The narrowing is due to atheroslcerosis. Note that the
intimal atheroma display cholesterol clefts (whitish needle-like
spaces). There is atrophy of the media.
Infective endocarditis (aortic valve)
Note the relatively bulky vegetation causing destruction of the aortic
valve cusps.
?

Fate of the Thrombus
Thrombi undergo some combination of the following four events:
●Propagation:
Thrombi accumulate additional platelets and fibrin, eventually
causing vessel obstruction.
●Embolization:
Thrombi dislodge or fragment and are transported elsewhere in
the vasculature.
●Dissolution:
Is the result of fibrinolytic activation, which leads to rapid
shrinkage and even total lysis of recent thrombi.
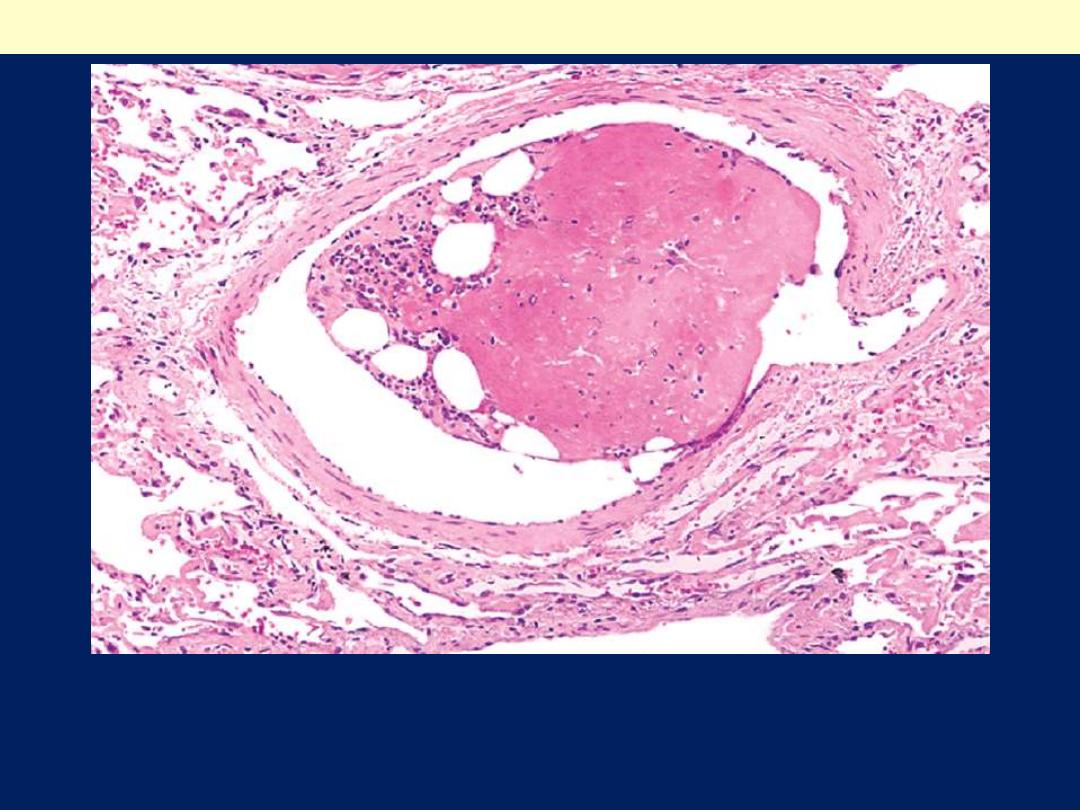
●Organization and recanalization:
Older thrombi become organized by the ingrowth of endothelial
cells, smooth muscle cells, and fibroblasts into the fibrin-rich clot.
Capillary channels are eventually formed that, to can create
conduits along the length of the thrombus and thereby re-establish
the continuity of the original lumen.
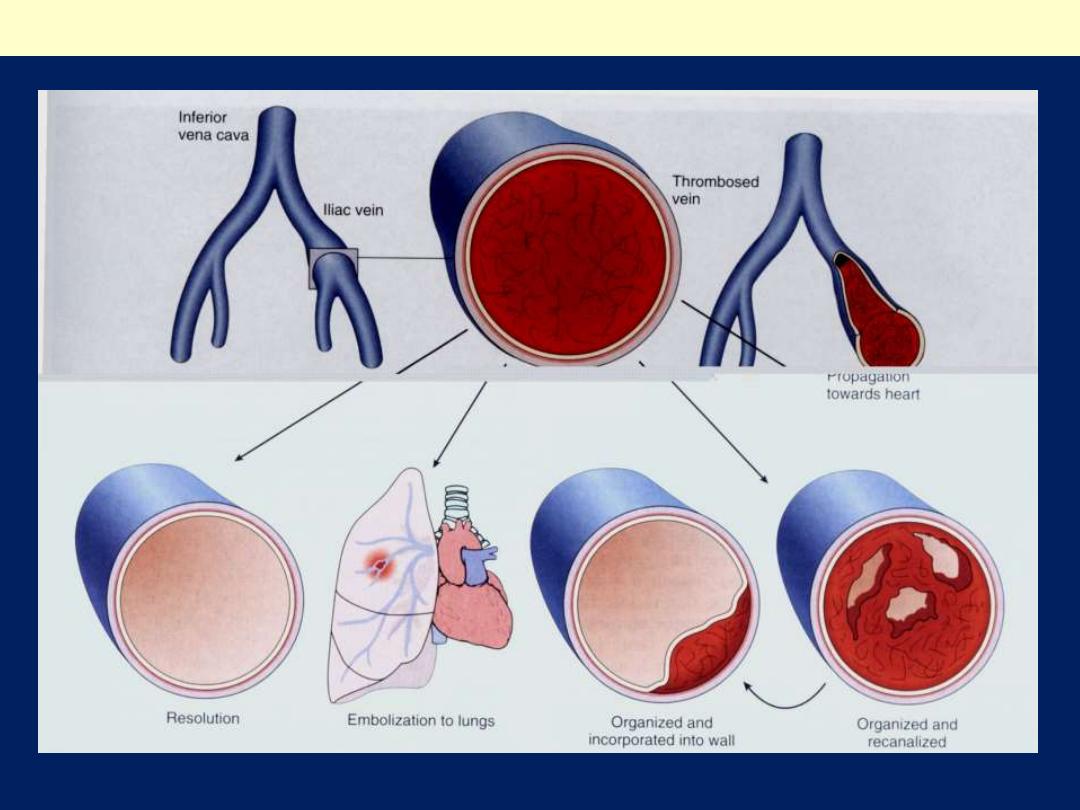
Potential outcomes of venous thrombosis
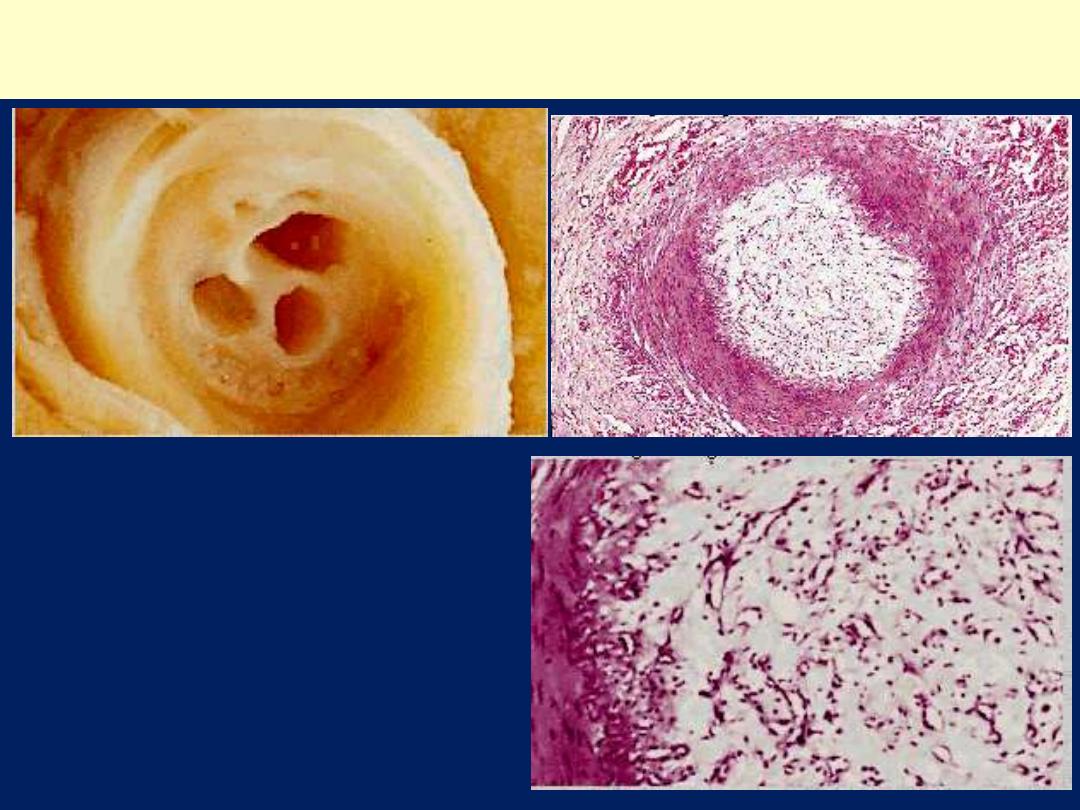
Coronary thrombosis showing organization and re-canalization

Deep venous thrombosis can complicate:
1. Advanced age, bed rest, and immobilization increase the risk
of deep venous thrombosis because reduced physical activity:
●Diminishes the milking action of muscles in the lower leg and
so slows venous return.
2. Cardiac failure causes:
●Stasis in the venous circulation.
3. Trauma, surgery, and burns result in:
●Reduced physical activity. ●Injury to vessels. ●Release of
procoagulant substances from tissues. ●Reduced t-PA activity.
4. Peripartum and postpartum states:
●Amniotic fluid infusion into the circulation.
●Hypercoagulability.
5. Hypercoagulable states.
6. Disseminated cancers:
●Tumor-associated procoagulant release.

Cardiac and Arterial Thrombosis:
The major initiator of arterial thromboses is:
Atherosclerosis.
Because it is associated with:
●Loss of endothelial integrity. ●Abnormal vascular flow.
The major initiator of cardiac mural thrombi is:
Myocardial infarction.
Because it is associated with:
●Dyskinetic myocardial contraction. ●Damage to the adjacent
endocardium.
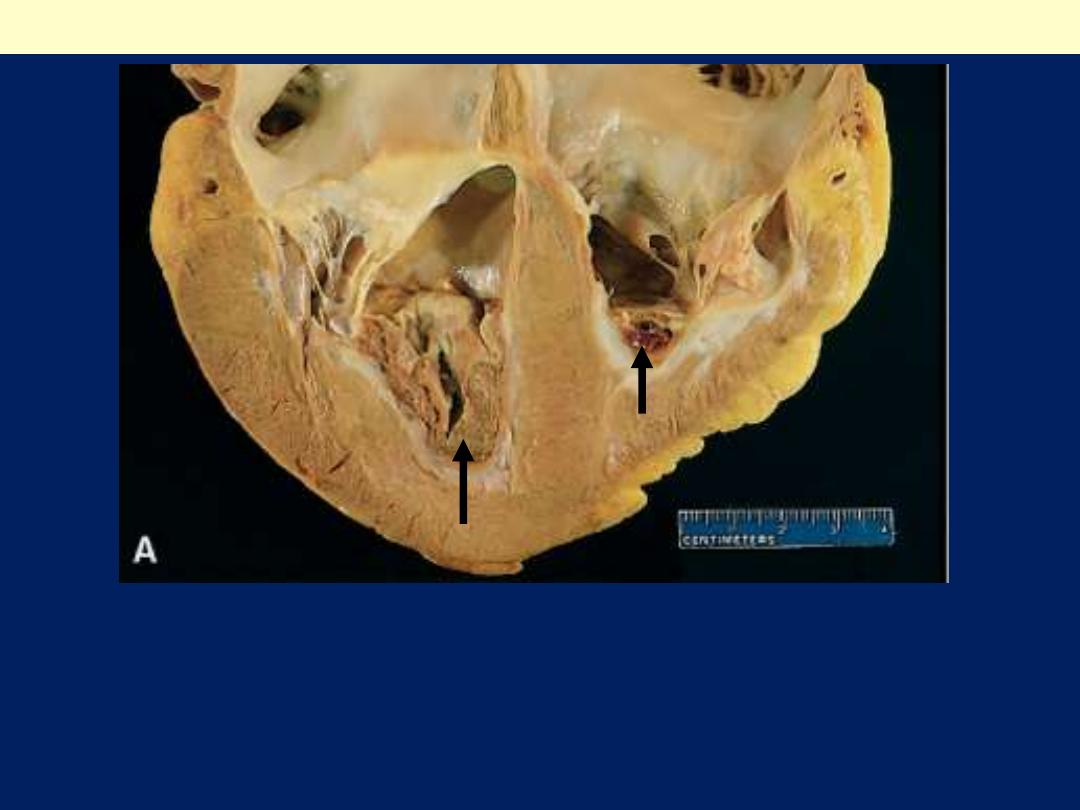
Rheumatic heart disease can cause:
Atrial mural thrombi due to:
●Mitral valve stenosis
, followed by
●Left Atrial Dilation
and
concurrent
●Atrial Fibrillation.
Arterial aneurysms (e.g. aortic) are frequently filled by thrombi.
Cardiac and Aortic mural thrombi can embolize peripherally.
Virtually any tissue can be affected, but brain, kidneys, and
spleen are prime targets because of their large volume of blood
flow.

Embolism
An embolus is:
A detached intravascular solid, liquid, or gaseous mass that
is carried by the blood to a site distant from its point of
origin.
Forms of emboli
1. Thromboemboli:
representing a dislodged thrombus or
part of it.
Rare forms of emboli include
2. Fat emboli:
consisting of fat droplets.
3. Air emboli:
consisting of bubbles of air or nitrogen.
4. Atherosclerotic emboli:
(cholesterol emboli) consisting of
athermatous debris.
5. Tumor emboli:
made up of fragments of a tumor.
6. Bone marrow emboli
:
consisting of bits of bone marrow.
7. Foreign body emboli:
as
bullets or shrapnel.
Embolus
Derived
From:
A Lower Extremity
Deep Venous
Thrombosis
and now:
Impacted astride the
bifurcation of the main
pulmonary artery.
Pulmonary thromboembolism

Large embolus occluding main pulmonary A
A pulmonary thrombo-embolus.
Such thrombi embolize from large
veins in the legs and pelvis.
This pulmonary thrombo-embolus is
occluding the main pulmonary artery.
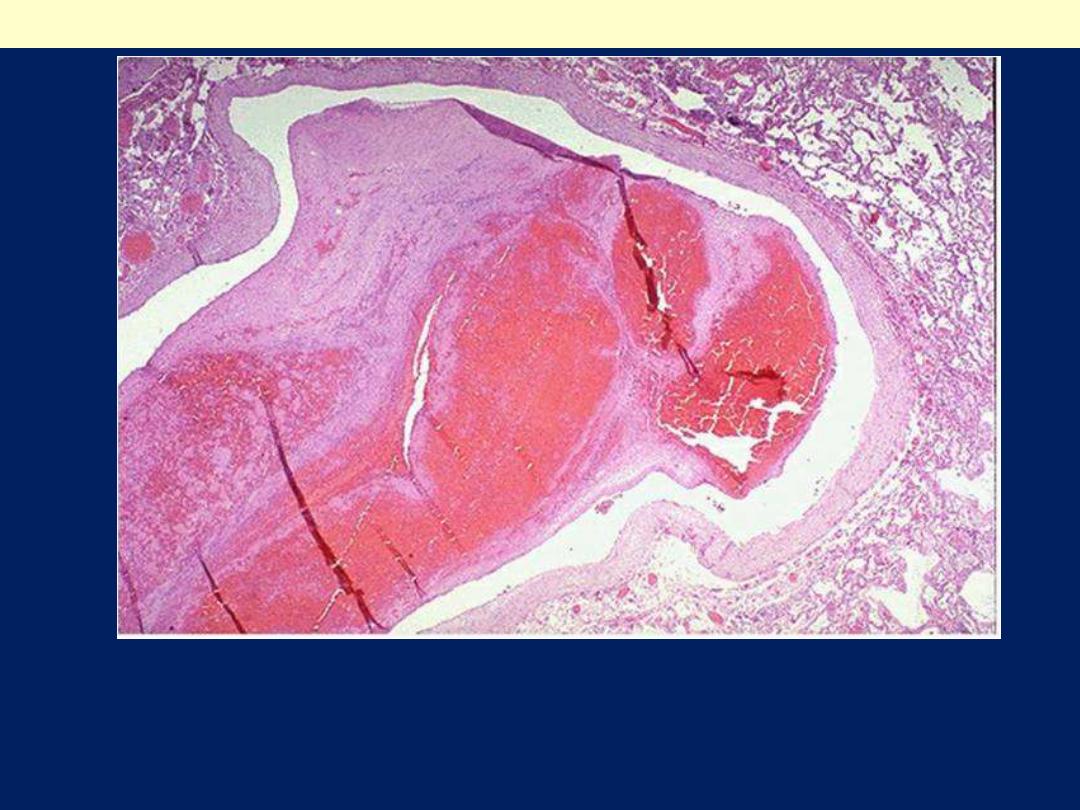
Pulmonary thrombo-embolus
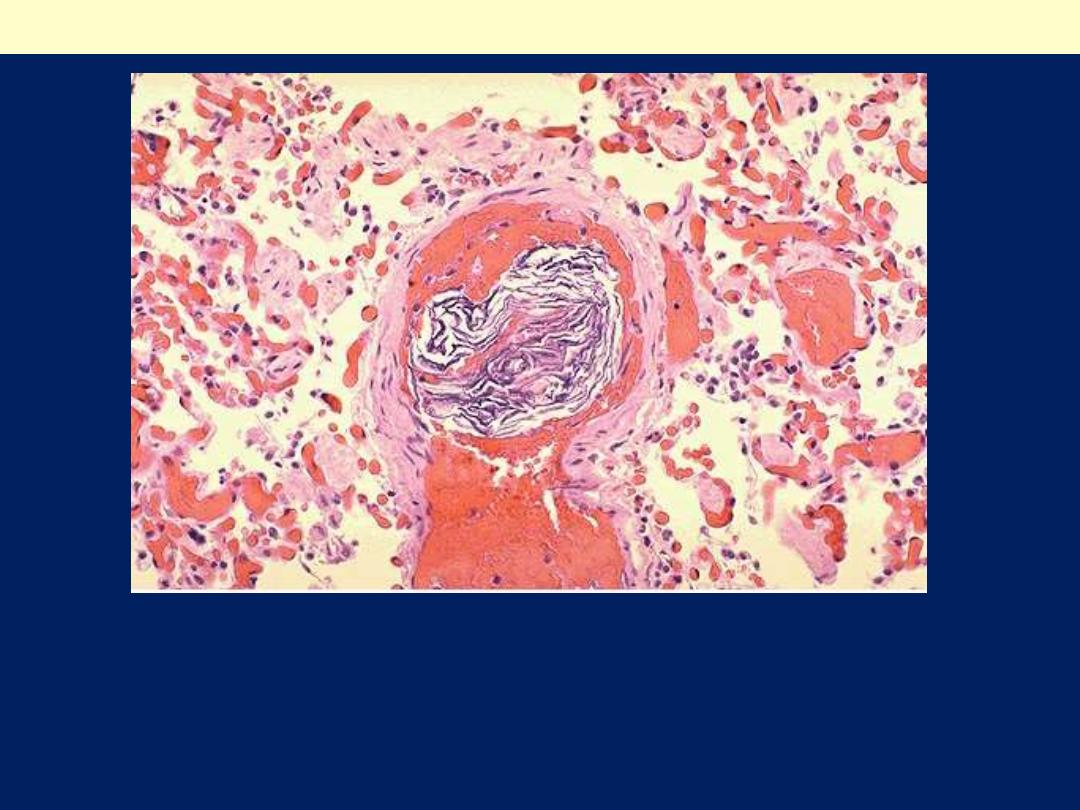
This is the microscopic appearance of a pulmonary thrombo-
embolus in a major pulmonary artery branch. Note its laminated
appearance (lines pf Zahn)

Systemic Thromboembolism
This refers to emboli in:
The arterial circulation.
Sources include:
1. Intracardiac mural thrombi
(80%) that complicate:
A. Infarction of the left ventricular wall (70%).
B. Dilated left atria (e.g., secondary to mitral valve disease)
(25%).
The remainder (5%) originates from thrombi complicating:
2. Aortic aneurysms.
3. Ulcerated atherosclerotic plaques.
4. Valvular vegetations.
A very small fraction of systemic emboli appear to
arise in
veins but end up in the arterial circulation, through
interventricular defects.
These are called:
5. Paradoxical emboli.

The major sites for arteriolar
embolization are:
1. The lower extremities (75%).
2. The brain (10%).
3. The intestines (mesenteric), kidneys,
and spleen.
4. The upper limbs are the least
common sites.
?
The rounded holes that appear in the vascular spaces here in the lung are fat
emboli. Fat embolization syndrome occurs most often following trauma with
fracture of long bones that releases fat globules into the circulation which are
trapped in pulmonary capillaries.
Fat embolism lung
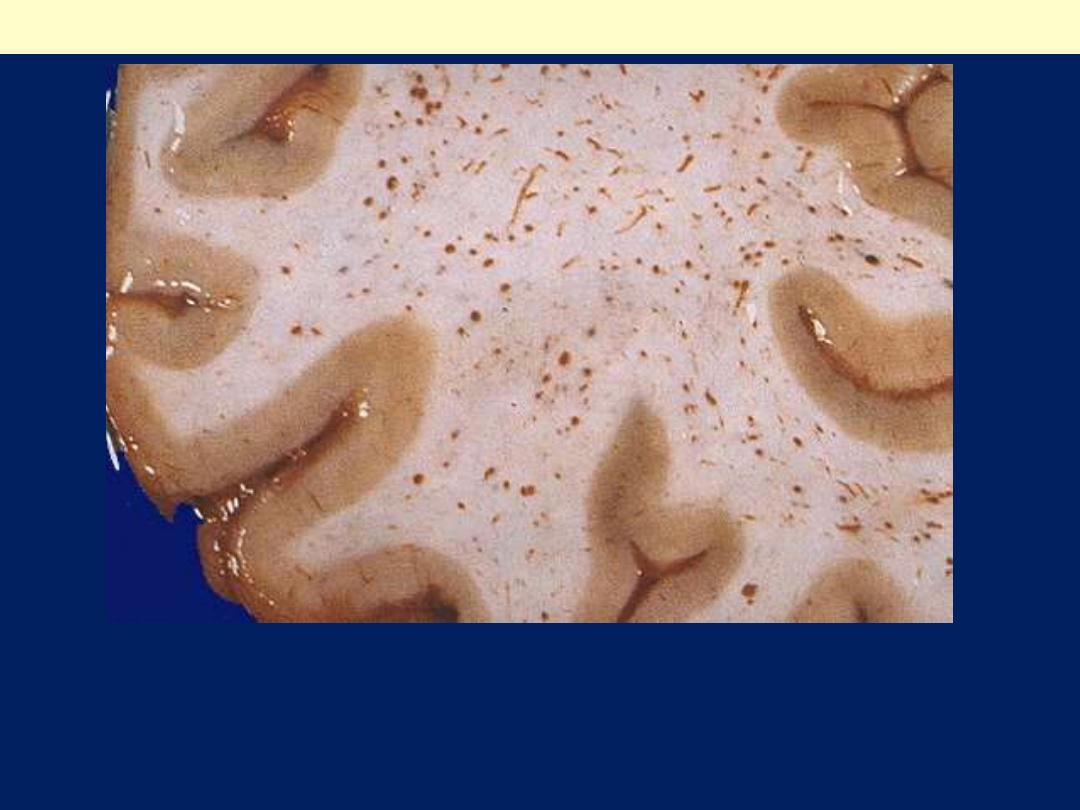
Sometimes about a week following the event initiating fat embolism syndrome,
there is loss of consciousness because of "brain purpura" as shown here.
Numerous petechial hemorrhages are produced by fat emboli to the brain,
particularly in white matter.
Fat embolism syndrome brain
The cellular elements on the left side of the embolus are hematopoietic precursors,
while the cleared vacuoles represent marrow fat. The relatively uniform red area
on the right of the embolus is an early organizing thrombus.
Bone marrow embolus in the pulmonary circulation.
This is a rare finding that may complicate a term pregnancy at delivery.
Seen here in a pulmonary artery branch is an amniotic fluid embolus that
has layers of fetal squames. Amniotic fluid embolization can have the same
outcome as a large saddle pulmonary embolus.
Amniotic fluid embolism lung

Fat & bone marrow embolism:
Microscopic fat globules can be
found in the circulation
after fractures of long bones (which contain
fatty marrow) or after soft-tissue trauma.
Fat enters the circulation by rupture of the marrow vascular
sinusoids or rupture of venules in injured tissues.
Air Embolism:
Gas bubbles within the circulation can obstruct
vascular flow and cause ischemic injury.
Air may enter the
circulation during obstetric procedures or as a consequence of chest
wall injury.
Generally, more than 100 ml of air are required to produce a
clinical effect;
bubbles can coalesce to form frothy masses
sufficiently large to occlude major vessels.
Amniotic Fluid Embolism:
The underlying cause is entry of
amniotic fluid into the maternal circulation via a tear in the
placental membranes with the fluid gaining access into ruptured
uterine veins.
Classically, there is marked pulmonary edema and diffuse alveolar
damage.

Infarction
This is defined as:
Localized area of
ischemic cell necrosis
in a living organ or
tissue, resulting most often from:
Sudden reduction or cessation of its blood supply.
Causes of vascular obstruction:
1. Nearly 99% of all infarcts result from thrombotic or
embolic events, and almost all result from arterial occlusion.
Uncommon causes include:
2. Expansion of atheromatous plaques by intraplaque
hemorrhage.
3. Spasm of coronary arteries.
4. Pressure on a vessel from outside: ●Tumor. ●Fibrous
adhesions. ●Narrow hernial sac.
5. Twisting (torsion) of the pedicle of mobile organ
e.g. loop of
small intestine (volvulus), ovary and testis.
?

A pulmonary infarct is
hemorrhagic
because of :
1. The spongy nature of the
lung tissue.
2. The dual blood supply from
the non-occluded bronchial
arteries which continue to
supply blood, but do not
prevent the infarction.
Pulmonary infarction
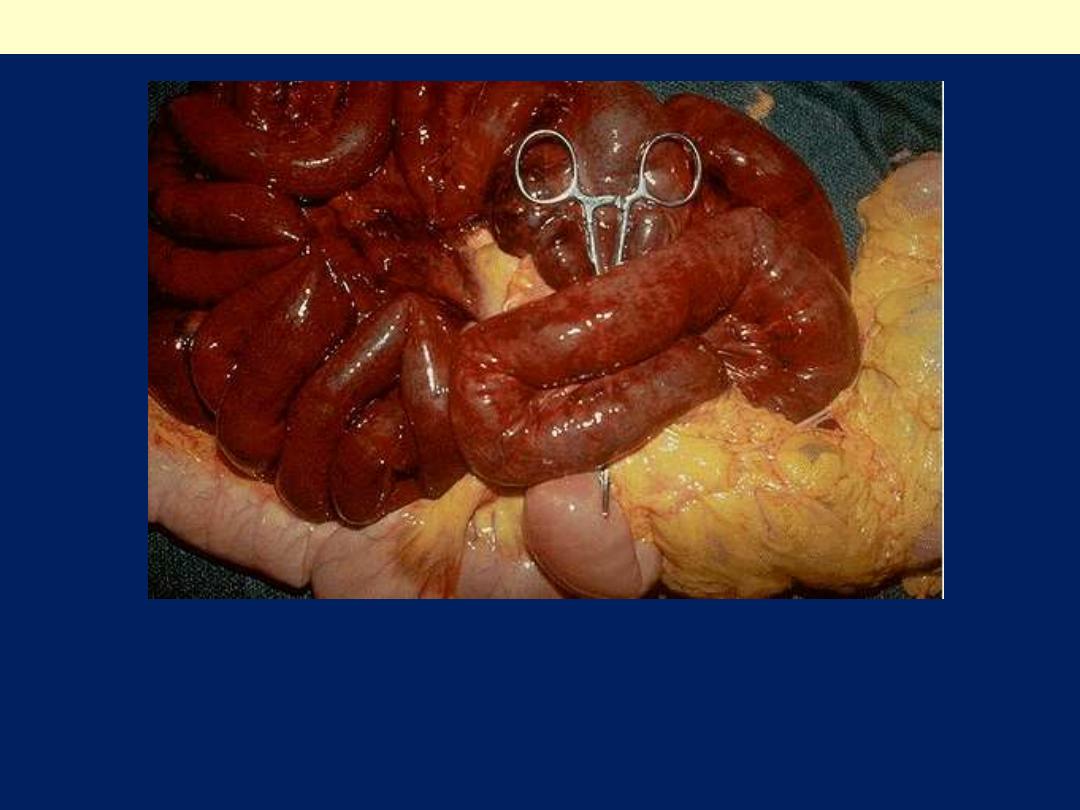
The dark red infarcted small intestine contrasts with the light pink
viable bowel. This is one complication of adhesions from previous
surgery. The trapped bowel has lost its blood supply because of
fibrous adhesions
Intestinal infarction (Hemorrhagic-red)
Sharply demarcated pale infarct in the spleen (white infarct). Note
the wedge shape of the infarct.
Splenic infarction
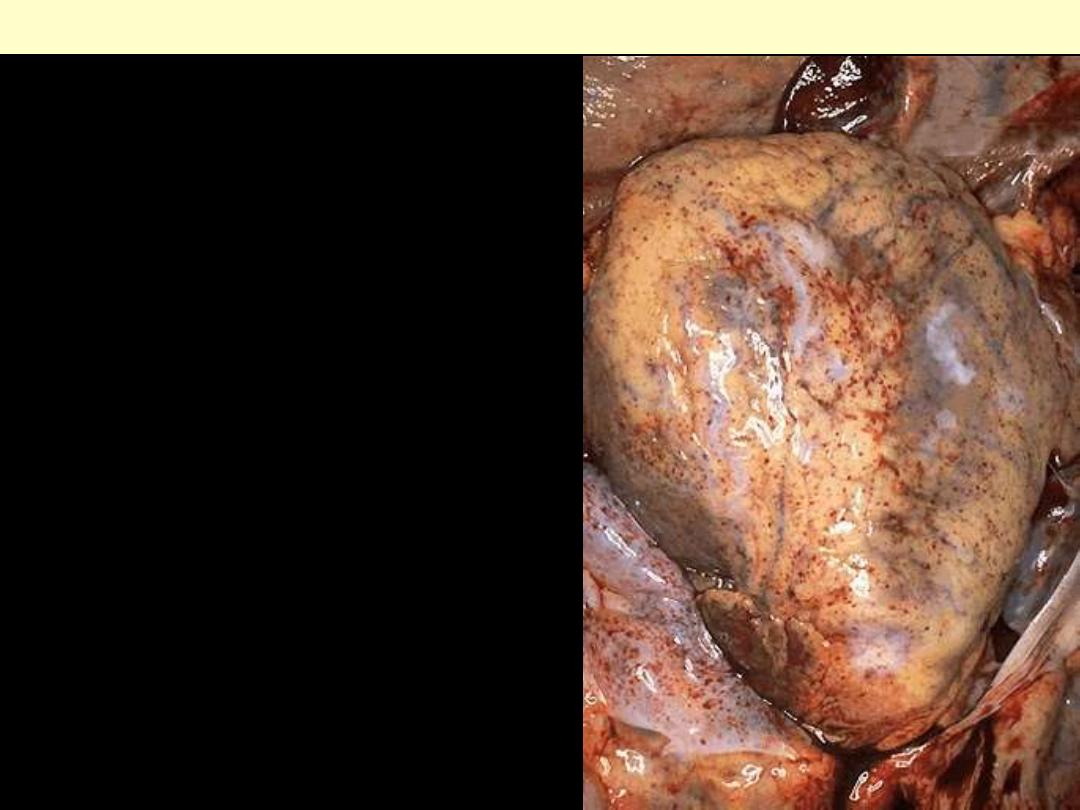
A recent infarct of the kidney
shows a pale area of infarction,
with an adjacent hyperemic
border separating it from
normal kidney. Note the wedge
shape of the infarct.
Renal infarction
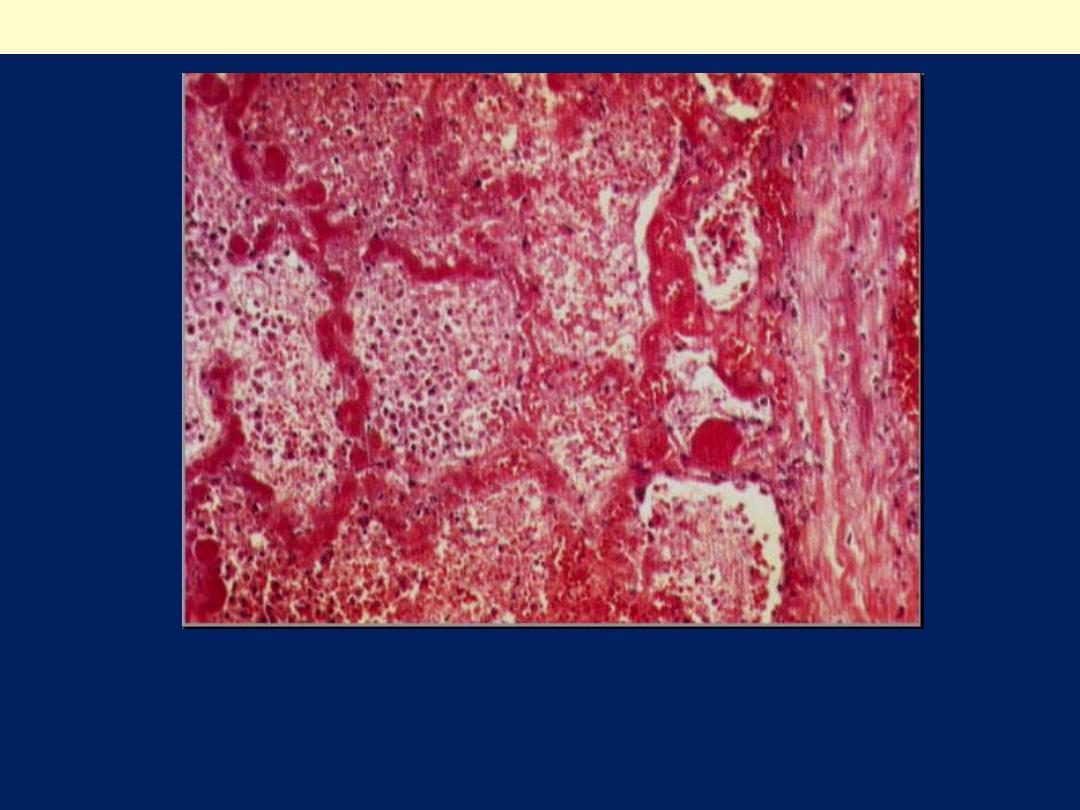
Myocardial infarction of about 1 to 2 days in duration. The myocardial cell
nuclei and cross striations have almost all disappeared. There is beginning acute
inflammation (neutrophils with their dark blue segmented nuclei, infiltrate
between necrotic myocardial fibers. An area of hemorrhage is present (arrows)
Myocardial infarction-Recent
The walls of the alveoli are necrotic. The capillaries are full of blood but
endothelial and alveolar epithelial cells can not be distinguished. The alveolar
spaces contain necrotic cells and cell debris, much of it derived from red cells.
There is also abundant fibrin
Pulmonary infarction

Factors That Influence Development of an Infarct:
Nature of the Vascular Supply:
The presence or absence of an alternative blood supply.
For example, lungs have a dual pulmonary and bronchial artery
blood supply; thus, obstruction of small pulmonary artery or
arterioles does not cause.
2. Rate of Development of Occlusion:
Slowly developing occlusions are less likely to cause infarction
because they provide time for the development of alternative
perfusion pathways i.e. collateral vessels.
3. Vulnerability to Hypoxia:
The susceptibility of a tissue to hypoxia influences the likelihood of
infarction.
4. Oxygen Content of Blood:
Partial flow obstruction of a small vessel in an anemic or cyanotic
patient might lead to tissue infarction, whereas it would be without
effect under conditions of normal oxygen tension.
?

END
