
• Learning objectives
• At the end of the lecture you have to Know
• 1-Morphological types of acute
inflammation.
• 2-Chronic inflammatoin.
• 3-clinical significance of acute and chronic
inflammation.

Effects of mediators
• Vasodilatation
-Histamine
- Prostaglandin's (PGE2)
- Nitric oxide
• Increased Vascular Permeability:
-
Histamine
- Complement component (C3a , C5a)
- Bradykinin
- Leukotrienes C4, D4 ,E4
- Platelet activating factor

• Chemotaxis, leukocytes activation
- C5a
- leukotrienes B4
-bacterial products
- chemokines (IL-8)
• Fever
- Il-21, IL-6, TNFα
- prostaglandins
• Pain
- prostaglandins
- bradykinin
• Tissue damage
- neutrophils & macrophage lysosomal enzymes
- oxygen metabolites
-nitric oxide
MORPHOLOGIC PATTERNS OF ACUTE
INFLAMMATION
Many variables may modify the basic inflammatory
response; these include :
1. The nature and intensity of the injury
2. The site and tissues affected
3. The responsiveness of the host

Types of Inflammation
Serous Inflammation
Fibrinous Inflammation
Suppurative Inflammation
Membranous Inflammation
Serous inflammation
• Is characterized by the outpouring of a thin fluid
that is derived from either the plasma or the
secretions of mesothelial cells lining of the
peritoneal, pleural, and pericardial cavities. In
these serous cavities the accumulated fluid is
called
effusion.
• The skin blister resulting from a burn or viral
infection represents a large accumulation of
serous fluid, either within or immediately
beneath the epidermis of the skin.
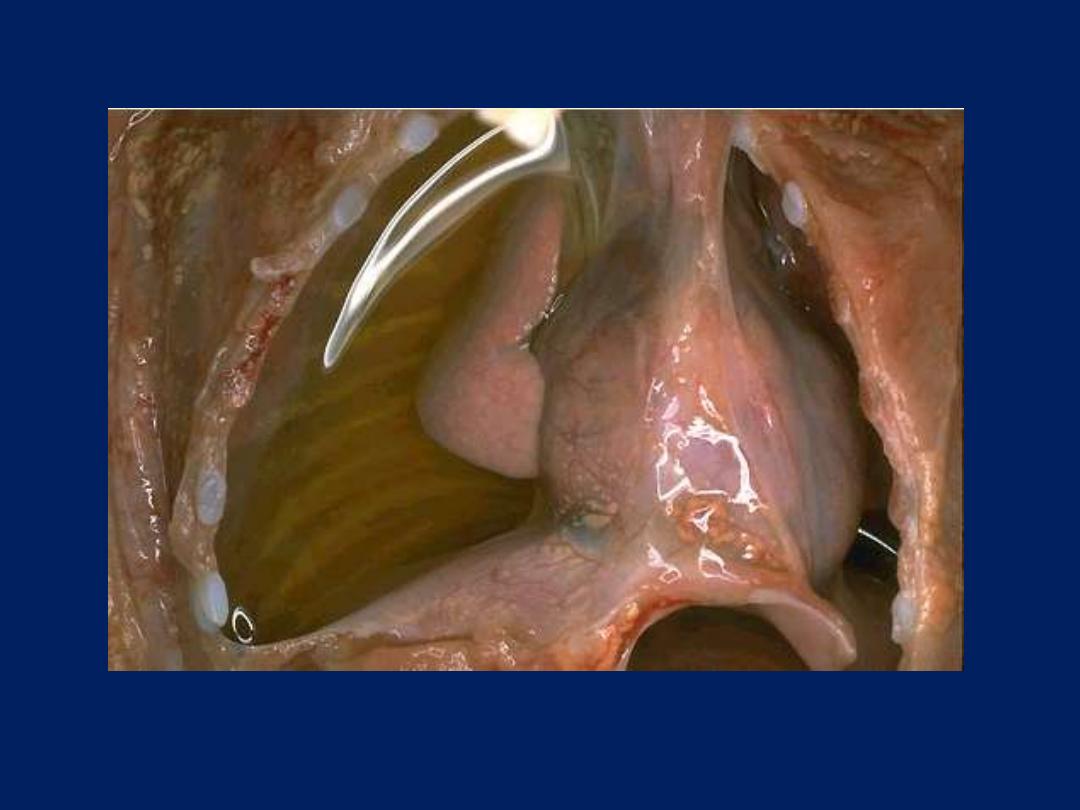
Serous pleural inflammation
Excessive accumulation of clear, thin fluid within pleural cavity. It is transparent but note the
reflection of light in the upper part of the photograph and lung collapse due to pressure
induced by the fluid.
Fibrinous inflammation
With more severe injuries and the resulting
greater vascular permeability, larger molecules
such as fibrinogen pass the vascular barrier, and
fibrin is formed and deposited in the
extracellular space.
A fibrinous exudate develops in such cases. The
latter also occurs when there is a stimulus for
coagulation in the interstitium (e.g., cancer
cells).
A fibrinous exudate is characteristic of
inflammation in the lining of body cavities, such
as the meninges, pericardium, and pleura.
Microscopically,
fibrin appears as an eosinophilic meshwork of threads or
amorphous coagulated mass.
Fibrinous exudates may be removed by fibrinolysis and
clearing of other debris by macrophages. However, when
the fibrin is not removed, it may stimulate the ingrowth
of fibroblasts and blood vessels and thus lead to scarring.
Conversion of the fibrinous exudate to scar tissue is called
organization. When this occurs within the pericardial sac
it leads either to opaque fibrous thickening of the
pericardium or, more often, to the development of
fibrous strands that reduce and may even obliterate the
pericardial space.

Fibrinous exudate-pericardium (G)
there is a lot of fibrin
the visceral and parietal
surfaces become stuck
together (by fibrin).
Separation of the two
layers imparts rough
irregular appearance (the
so called bread and
butter).
Suppurative (purulent) inflammation:
This is characterized by the production of large
amounts of pus or purulent exudate consisting
of:
neutrophils, necrotic cells, and edema fluid.
Certain bacteria (e.g., staph. aureus, St.
pyogenes, Pneumococci, gonococci,
meningococci and E. coli) produce this localized
suppuration and are therefore called
pyogenic
(pus-producing) bacteria.
A common example of an acute suppurative
inflammation is acute (suppurative) appendicitis.
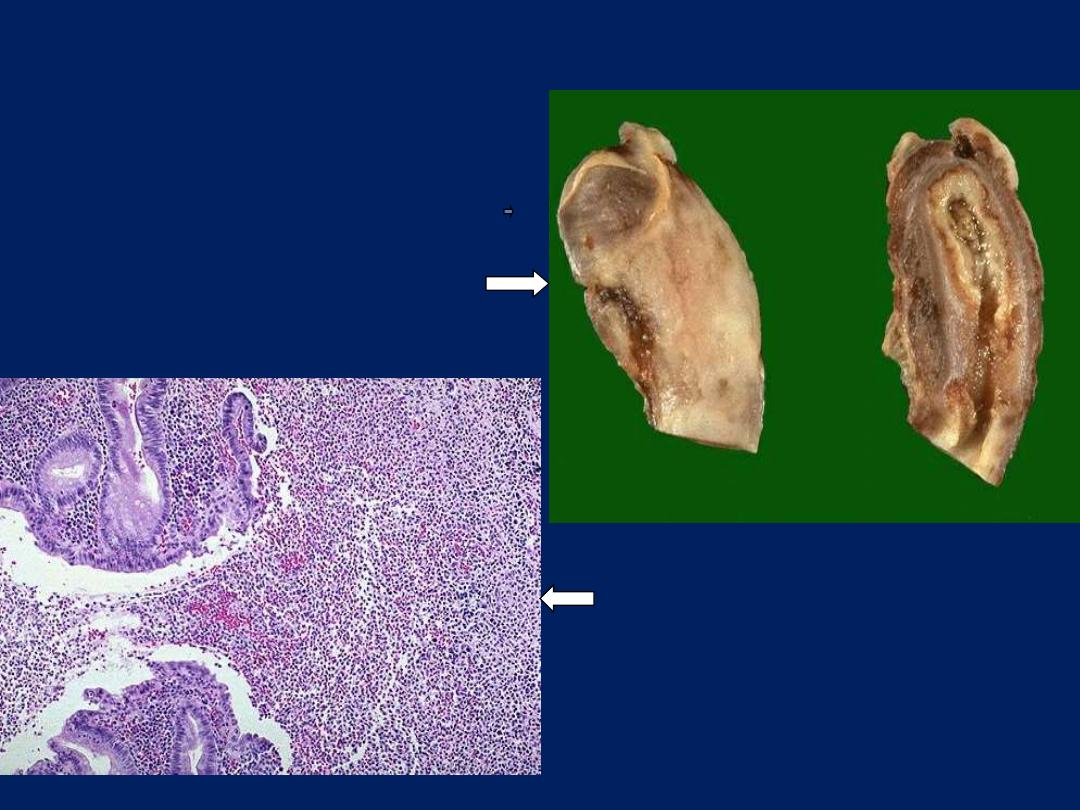
Appendix: acute suppurative inflammation
ulceration and undermining by an
extensive neutrophilic exudate
Upper half of excised appendix.
Lt: fibrino-purulent serosal exudate
Rt: lumen filled with pus
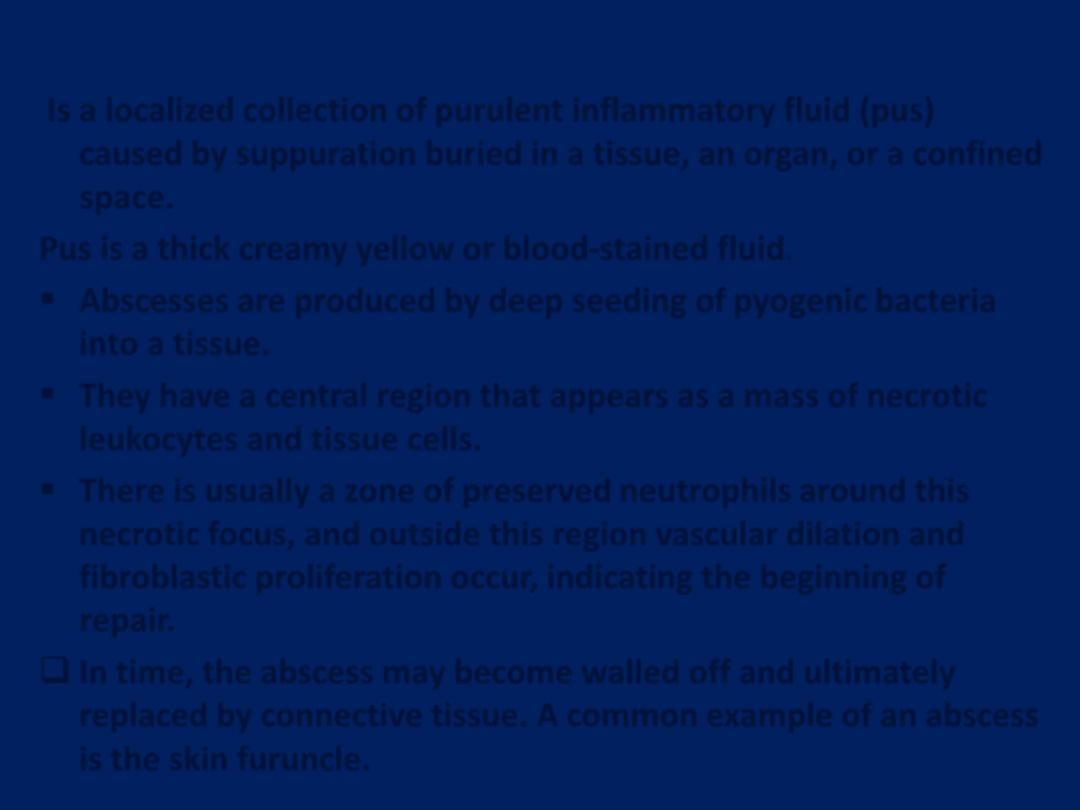
Abscess
Is a localized collection of purulent inflammatory fluid (pus)
caused by suppuration buried in a tissue, an organ, or a confined
space.
Pus is a thick creamy yellow or blood-stained fluid.
Abscesses are produced by deep seeding of pyogenic bacteria
into a tissue.
They have a central region that appears as a mass of necrotic
leukocytes and tissue cells.
There is usually a zone of preserved neutrophils around this
necrotic focus, and outside this region vascular dilation and
fibroblastic proliferation occur, indicating the beginning of
repair.
In time, the abscess may become walled off and ultimately
replaced by connective tissue. A common example of an abscess
is the skin furuncle.
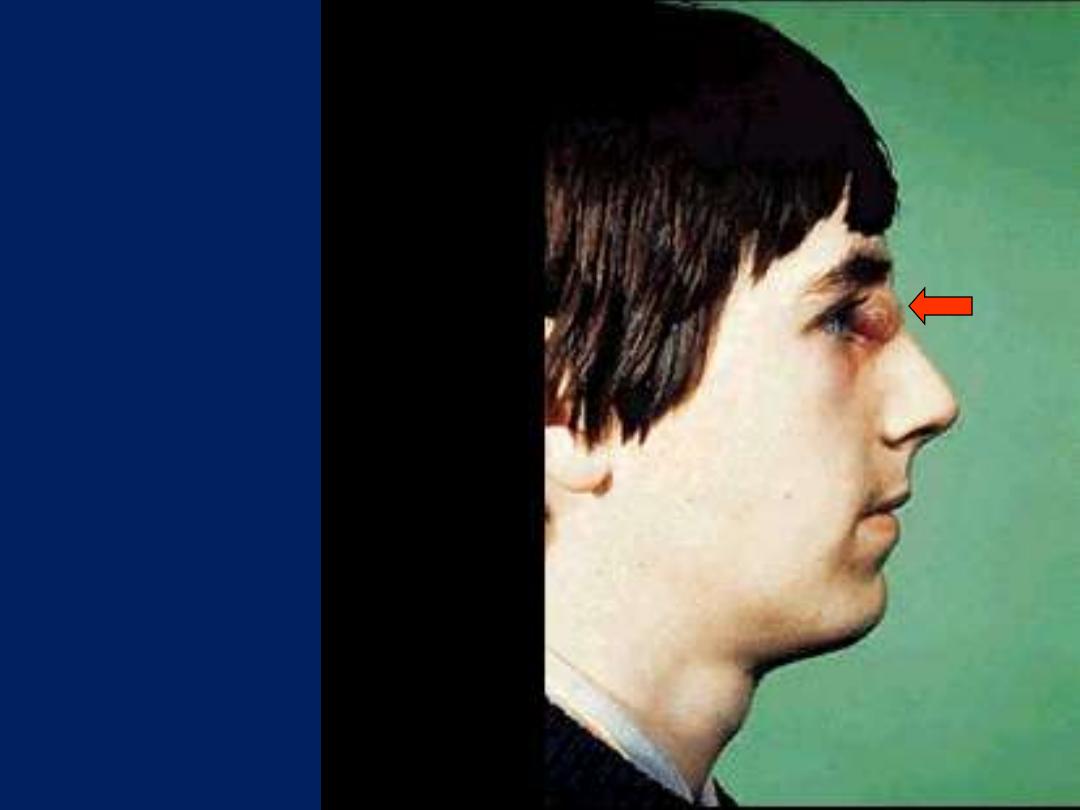
Abscess
Furuncle
(boil)
Abscess that involves the skin is
called “Boil” or “furuncle”.
Pseudomembranous inflammation
of mucous membranes
• Severe injury extensive epithelial necrosis
large shallow ulcers sloughing
• Fibrin, dead epithelium, neutrophils, red cells
and bacteria mix together false (pseudo-)
membrane (white or cream-colored layer)
• Diphtheria and psudomembranous colitis are
typical examples
Ulcers
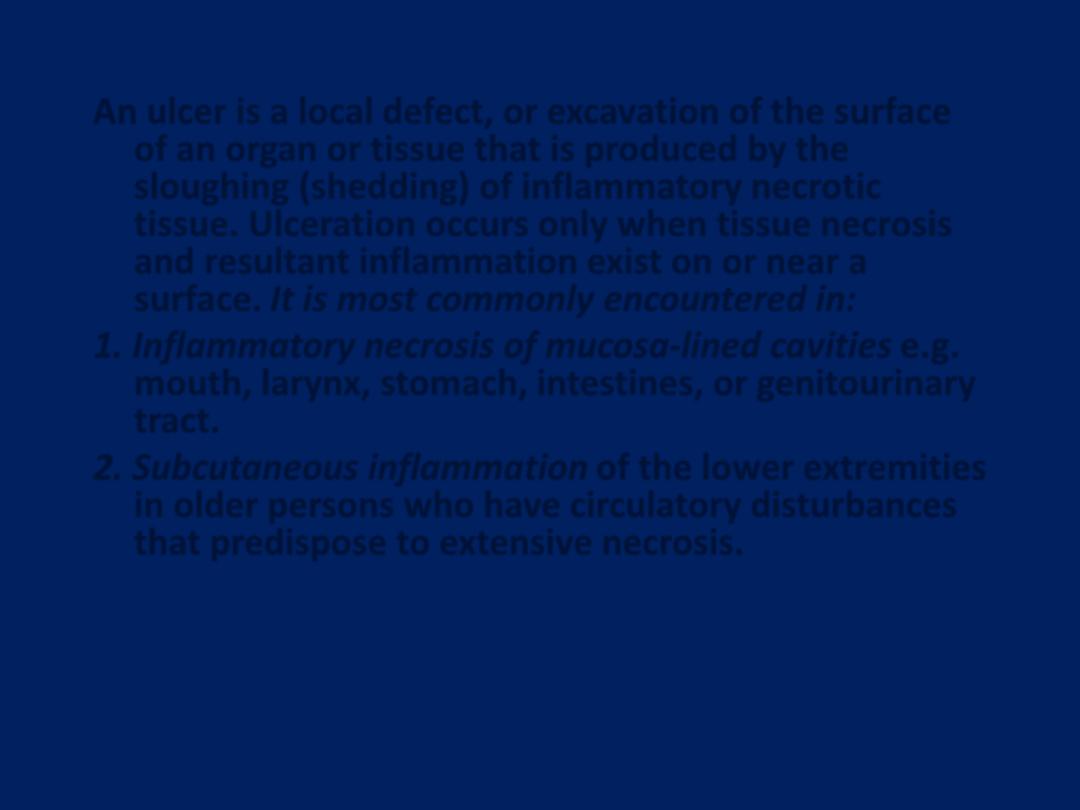
An ulcer is a local defect, or excavation of the surface
of an organ or tissue that is produced by the
sloughing (shedding) of inflammatory necrotic
tissue. Ulceration occurs only when tissue necrosis
and resultant inflammation exist on or near a
surface. It is most commonly encountered in:
1. Inflammatory necrosis of mucosa-lined cavities e.g.
mouth, larynx, stomach, intestines, or genitourinary
tract.
2. Subcutaneous inflammation of the lower extremities
in older persons who have circulatory disturbances
that predispose to extensive necrosis.
Ulcerations are best exemplified by peptic ulcer of the
stomach or duodenum, in which acute and chronic
inflammation coexist.
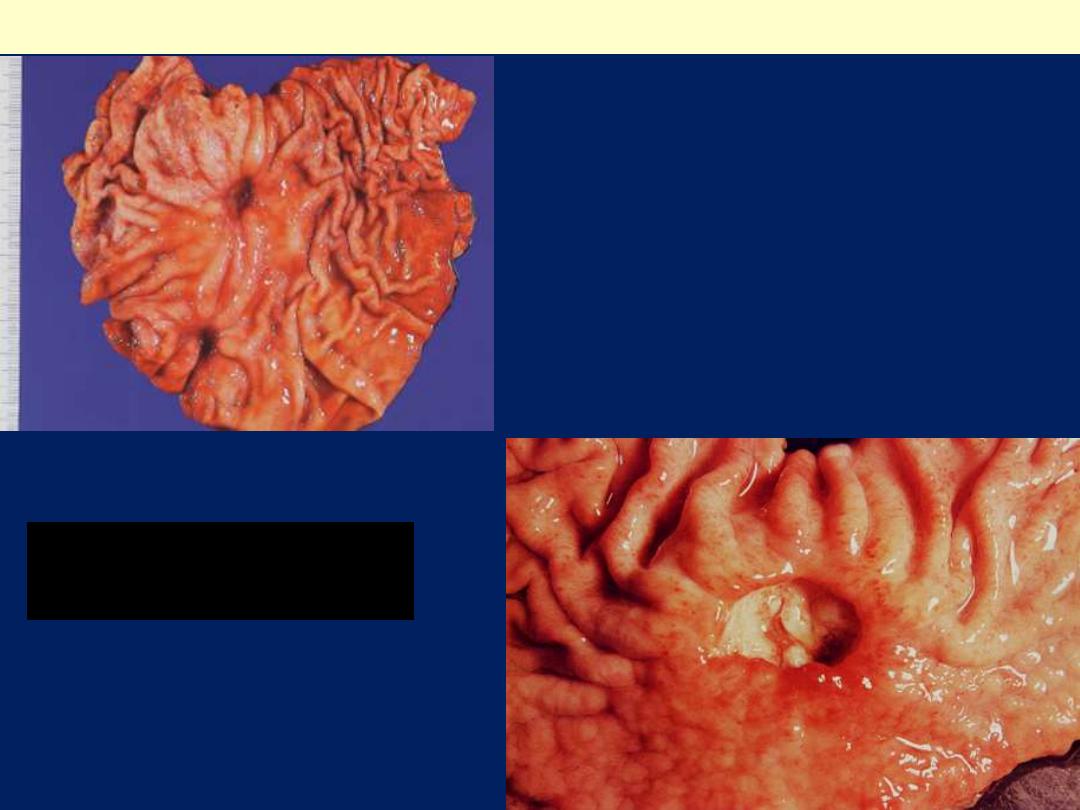
Chronic peptic ulcer stomach
Sharply delimited chronic peptic
ulcer with converging folds of
mucosa in the upper half

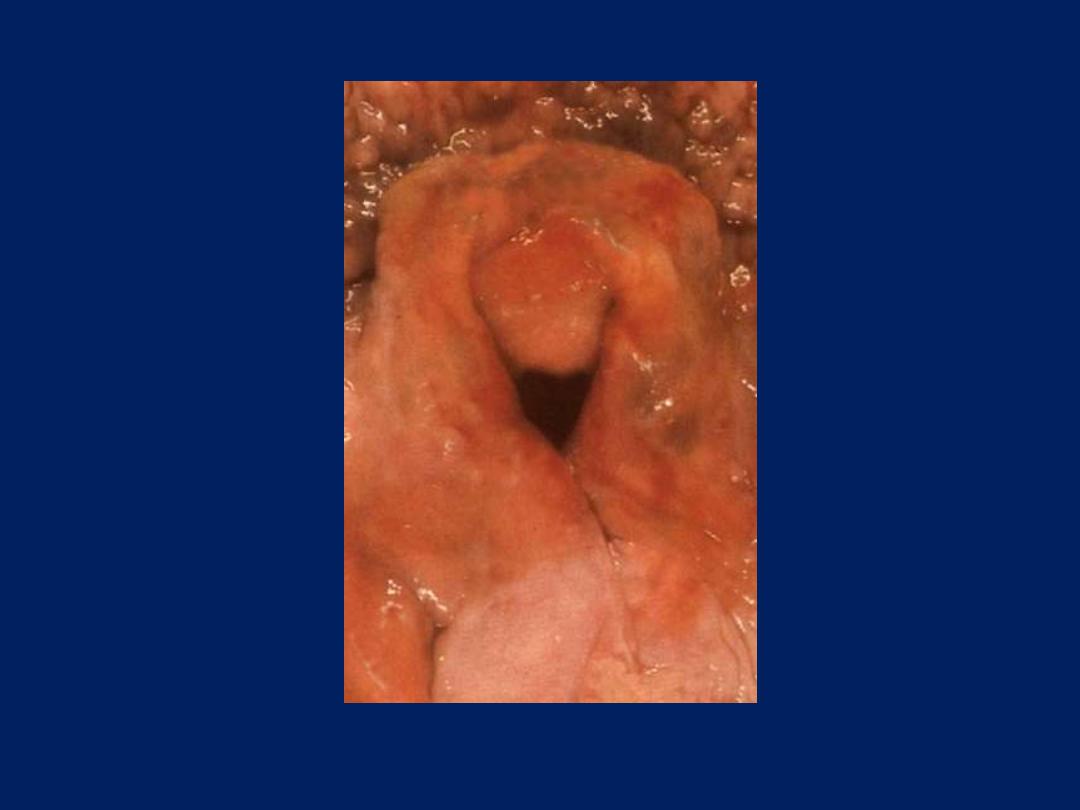
Ulceration, larynx, gross
Below the vocal cords in this
larynx are large ulcerations.
Such subglottic ulcers are
produced with prolonged
endotracheal intubation in
which the cuff of the
endotracheal tube fits too
tight. Thus, ulcerations can
be produce by mechanical
forces. In fact, so-called
"pressure ulcers" or
"decubitus ulcers" can form
in the skin over bony
prominences in persons who
are bedridden for an
extended time.
Pseudomembranous inflammation of mucous
membranes
Severe injury may be associated with extensive
epithelial necrosis with sloughing.
This creates large shallow ulcers. Fibrin, dead
epithelium, neutrophils, red cells and bacteria
mix together to produce a white or cream-
colored false (pseudo-) membrane covering the
affected mucosa.
Diphtheria and pseudomembranous colitis are
typical examples.
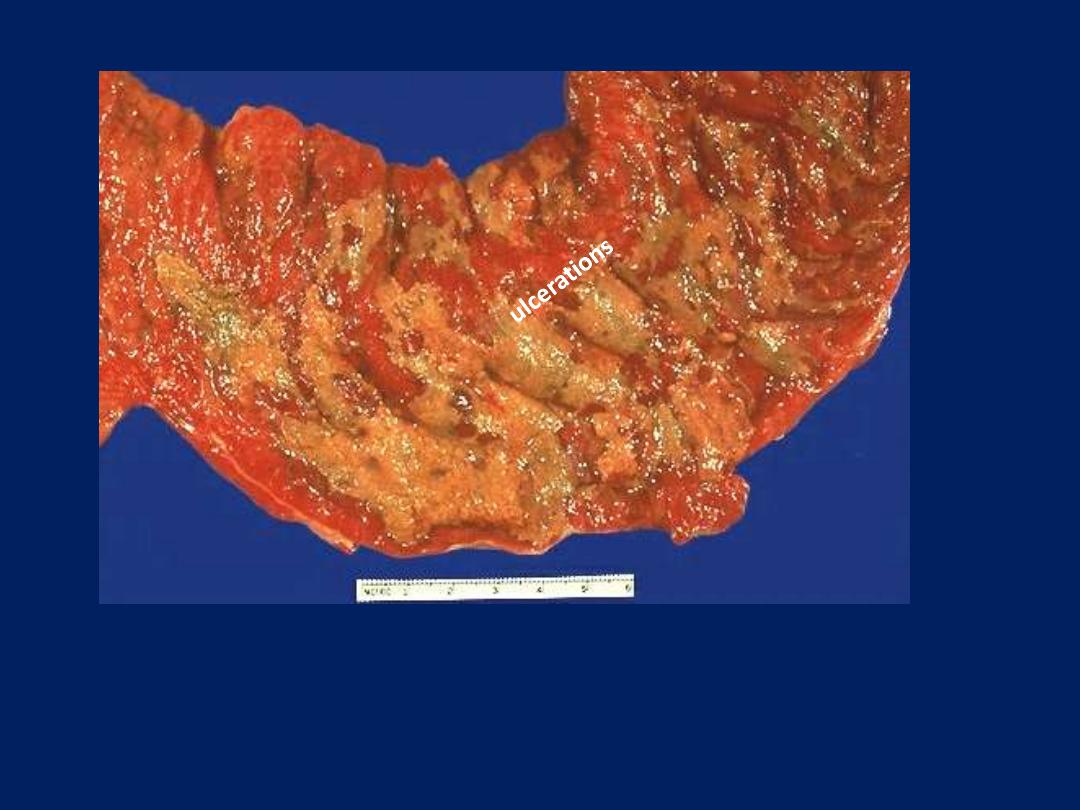
pseudomembrane
Pseudomembranous entercolitis (G)
This yellow-green exudate on the surface of an inflamed, hyperemic
(erythematous) bowel mucosa consists of many neutrophils along with
fibrin and amorphous debris from dying cells.

EFFECTS OF INFLAMMATION
Beneficial Effects
1. Dilution of Toxins
2. Protective Antibodies.
3. Fibrin Formation
4. Promotion of immunity.
5. Cell Nutrition.

EFFECTS OF INFLAMMATION
Harmful Effects
1. Swelling &Edema.
2. Rise in tissue pressure.
3. Severe Allergic Reaction.
Acute laryngeal edema
Note congestion and the marked narrowing of laryngeal orifice

Fate Of Acute Inflammation
Resolution
Healing By Fibrosis.
Suppuration & Abscess Formation.
Progression To Chronic Inflammation.
OUTCOMES OF ACUTE
INFLAMMATION
1. Complete resolution
The battle between the injurious agent and the
host may end with restoration of the site of
acute inflammation to normal. This is called
resolution and is the usual outcome when
a. the injury is limited or short-lived .
b. there has been little tissue destruction
c. the damaged parenchymal cells can regenerate
2. Healing by fibrosis
a. After extensive tissue destruction
b. When the inflammatory injury involves tissues
that are incapable of regeneration
c. When there is abundant fibrin exudation.
When the fibrinous exudate in tissue or serous
cavities (pleural, peritoneal, synovial) cannot be
adequately cleared, connective tissue grows
into the area of exudate, converting it into a
mass of fibrous tissue—a process also called
organization.
3. Progression to chronic inflammation
Acute to chronic transition occurs when the
acute inflammatory response persists,
owing either to:
• the perseverance of the injurious agent .
• failure of acute bacterial pneumonia to
resolve may lead to extensive tissue
destruction and formation of a cavity in
which the inflammation continues to
smolder, leading eventually to chronic
lung abscess.
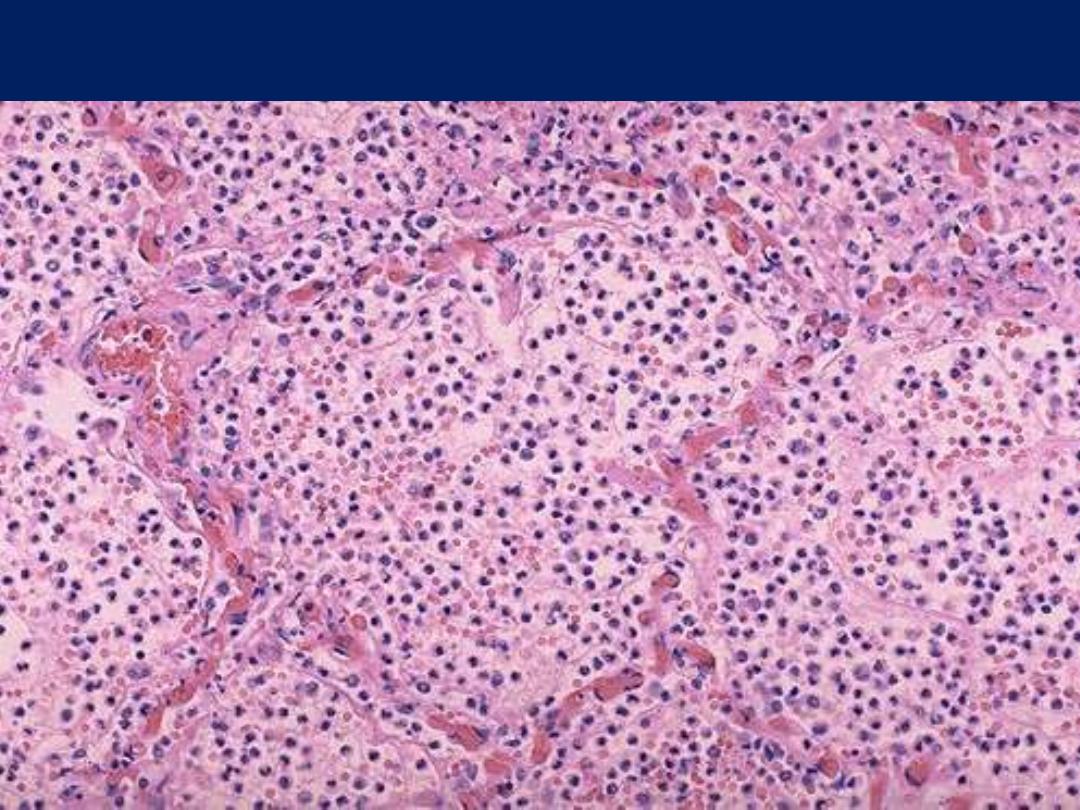
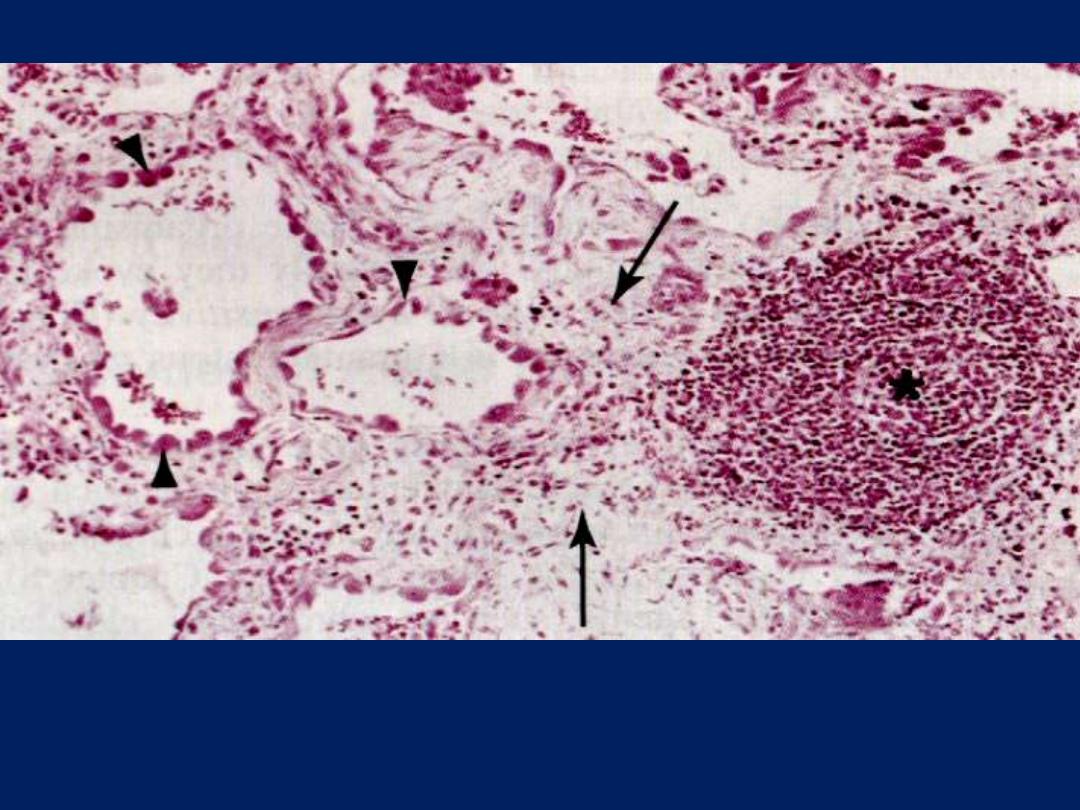
Acute pneumonia, microscopic
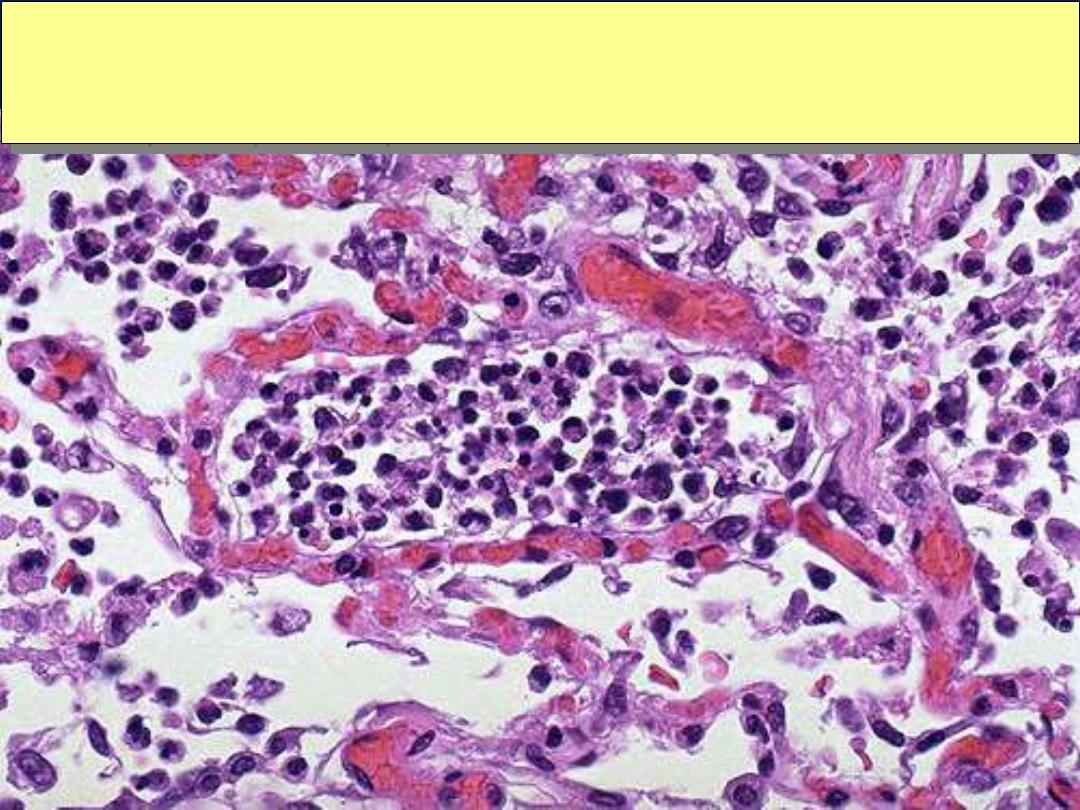
Acute pneumonia, microscopic
Acute bronchopneumonia, microscopic
The PMN's seen here are in alveoli, indicative of an acute bronchopneumonia of the lung. The
PMN's form an exudate in the alveoli. This patient had a "productive
“ cough because large
amounts of purulent sputum were produced. The source is seen here.

Chronic Inflammation
• Inflammation of slow progress lasting for weeks ,
months or years
• Marked by formation of new connective tissue
• Characterized by infiltration with mononuclear cells
including lymphocytes, plasma cells and macrophages
• Type of inflammatory process in which active
inflammation ,tissue injury and healing proceed
simultaneously

Features of chronic
inflammation
1. Long duration: persists for weeks, months or years
2. Tissue destruction: frequently greater than in acute
inflammation.
3. The inflammatory infiltrate is a mixture of
macrophages, lymphocytes and plasma cells
4. Productive rather than exudative: production of fibrous
tissue through formation of granulation tissue.
Features of chronic inflammation
The three characteristic features of chronic inflammation (in the lung)
1. Chronic inflammatory cells infiltration* 2. destruction of the normal tissue
(normal alveoli are replaced by spaces lined by cuboidal cells (arrow heads)
3. Replacement by fibrosis (arrows)

A. Chronic Inflammation may supervene on acute
inflammation
• Almost always a suppurative type of inflammation
• Presents as a purulent discharge (pus) as seen in abscess.
• The cause is either
- delay in the evacuation of an abscess, or
- presence of foreign-body within inflamed area
(dirt ,wood, metal or a sequestrated bone)

Chronic cholecystitis with
cholelithiasis

B. Chronic inflammation ab Initio
Usually follows injuries caused by
1. Chemical or physical agents (talc powder,
asbestos .silica)
2. Due to poor local circulation (Varicose veins)
3. Certain micro organisms (Leprosy ,Tuberculosis
and Syphilis).
4. Certain diseases (Rheumatoid Arthritis, Crohn's
disease).
5. Auto-immune diseases.
Mediators of chronic inflammation
Agent
Action
Source
Migration inhibition
factor (MIF)
Aggregation of
macrophages at site
of injury
Activated T
lymphocytes
Macrophage
activating
factor (MAF)
Increased
phagocytosis by
macrophages
Activated T
lymphocytes
Complement C5a
Chemotatic for
macrophages
Complement system
Eosinophil
chemotactic
factor of
anaphylaxis (ECF A)
Chemotactic for
eosinophils in
metazone infection
Mast cells and
basophils
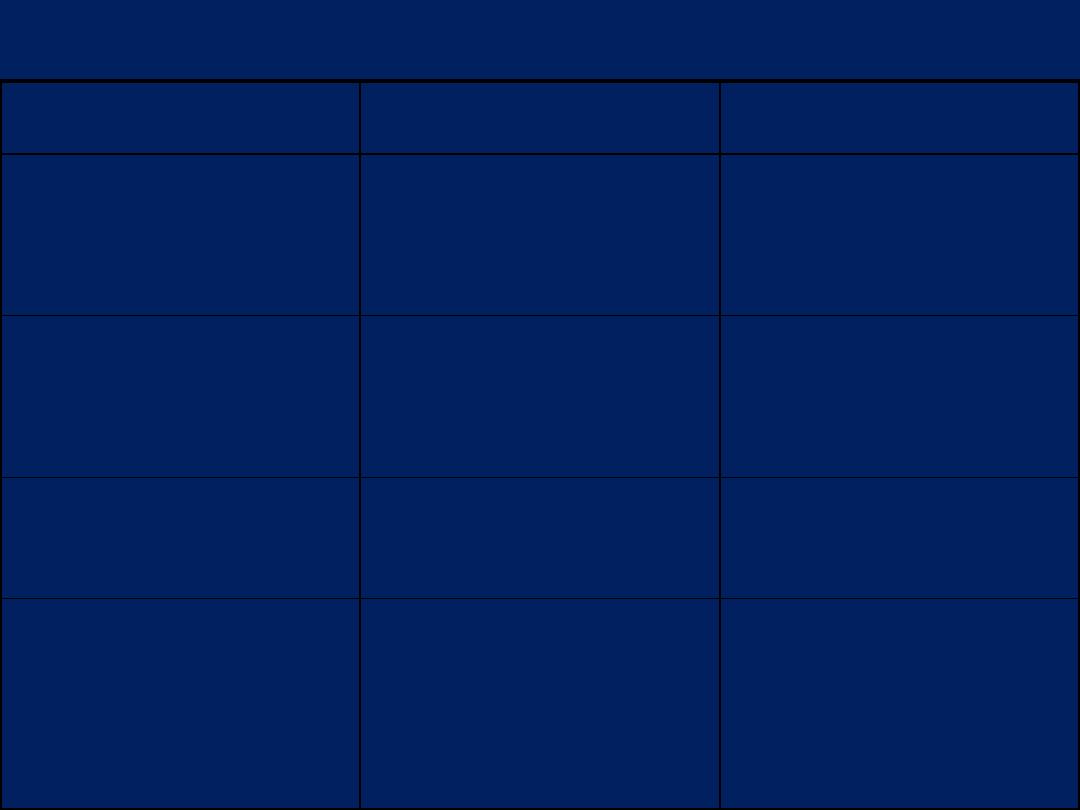
Silicotic nodule mic
A silicotic nodule in lung is seen here. It is composed mainly of bundles of interlacing pink
collagen. The silica particles are colorless and so not visible with this ordinary H & E stain
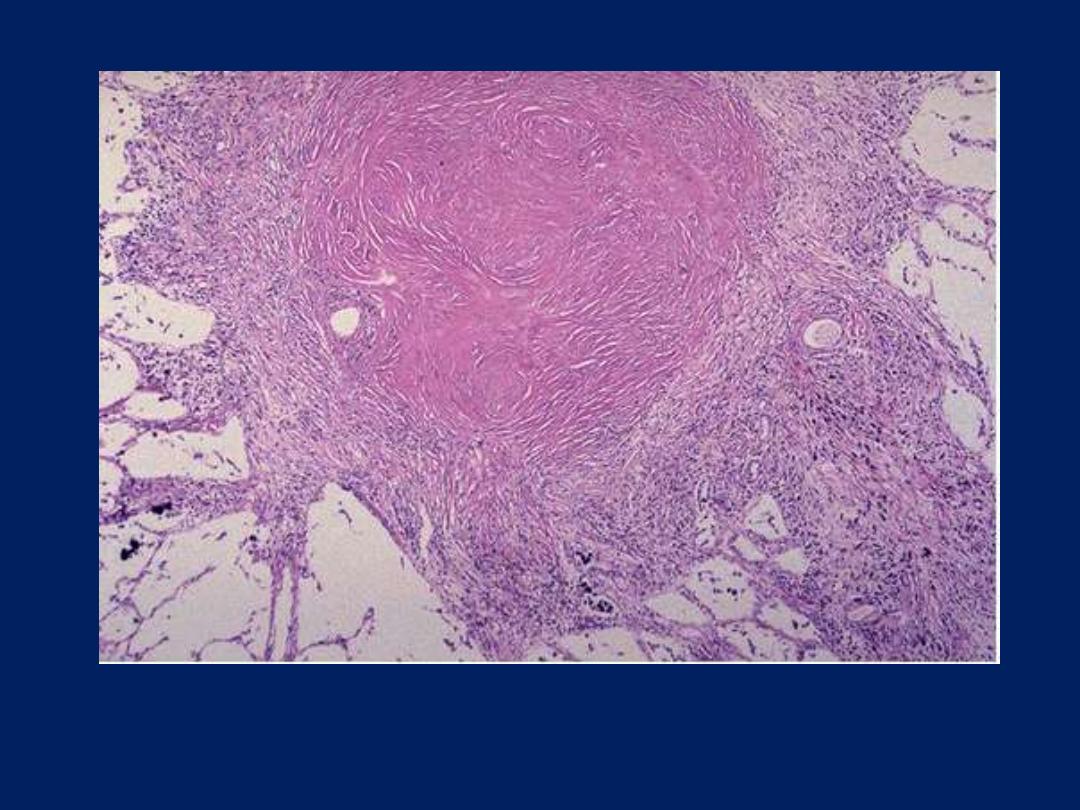
Rheumatoid arthritis
This deformity of the hand is due
to rheumatoid arthritis (RA).
This autoimmune disease leads
to synovial proliferation and
joint destruction, typically in a
symmetrical pattern involving
small joints of hands and feet,
followed by wrists, ankles,
elbows, and knees.
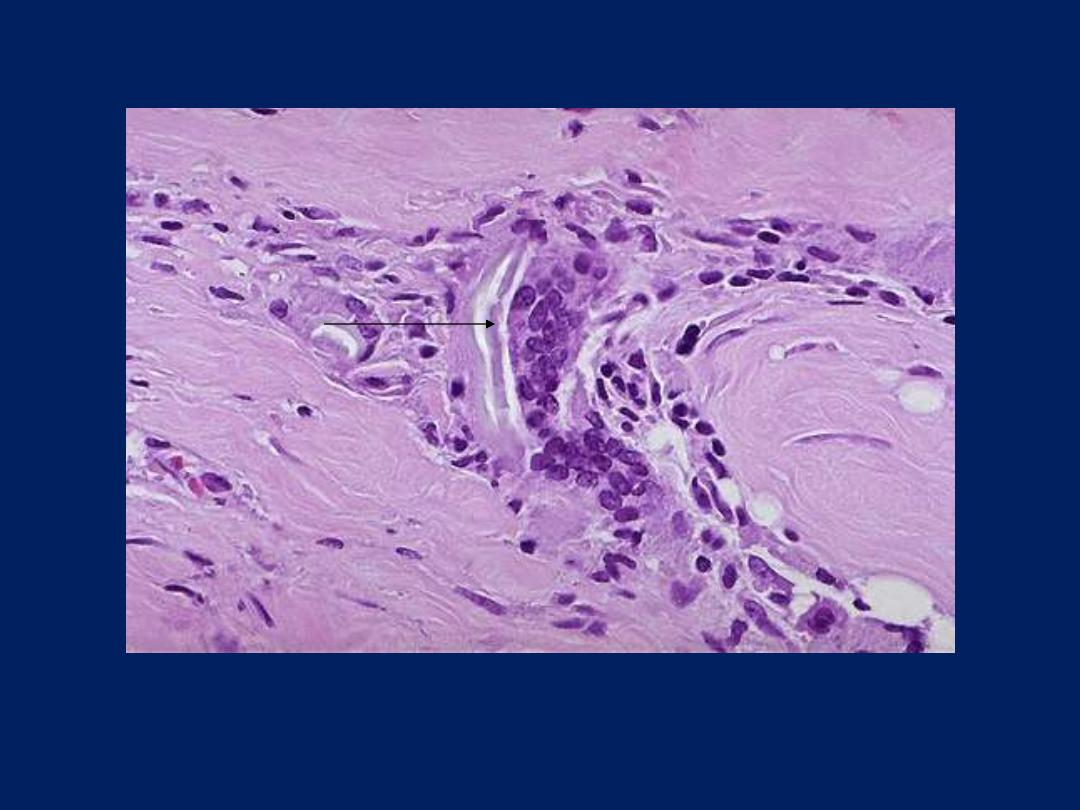
Chronic inflammation can go on for a long
time. Seen here in the synovium of a
patient with rheumatoid arthritis are
collections of dark blue lymphocytes.

Granulomatous Inflammation
• Distinctive pattern of chronic inflammation
characterized by
- aggregation of activated macrophages (epithelioid)
- multinucleated giant cells .
• Examples
- Tuberculosis
- Foreign-body granuloma
- Syphilis.
- Sarcoidosis
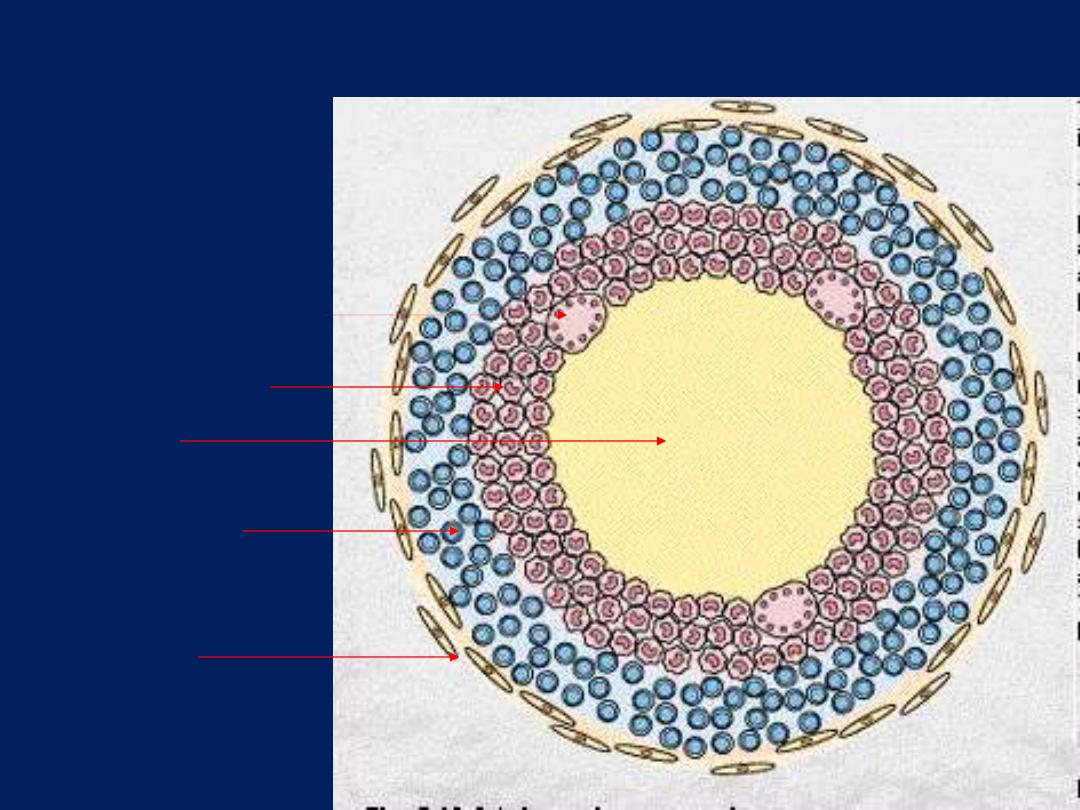
Diagram of typical TB granuloma
Caseation
Epithelioid cells
Multinucleated GC
Lymphocytes
fibroblasts
Langhan’s Vs FB giant cells
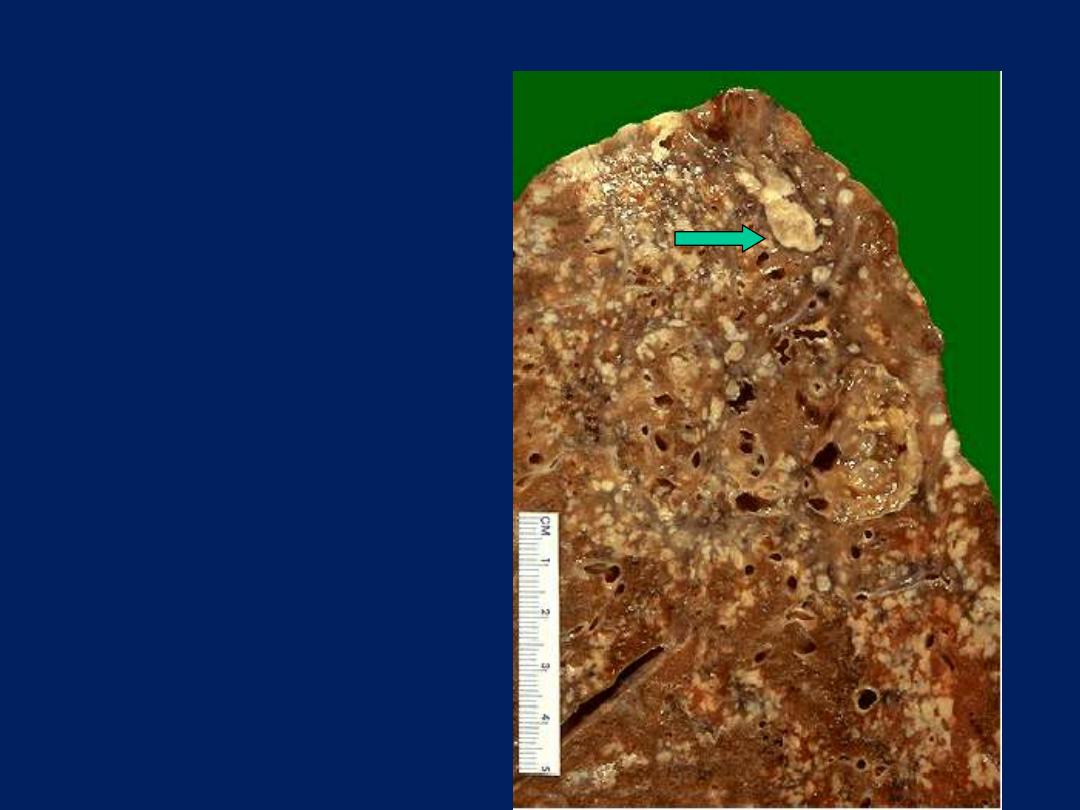
Lung, granulomatous inflammation with caseation
Note the yellowish mottling of lung
tissue. These small, yellow nodules
are caseating TB granulomas. Some
have fused together to form larger
areas of yellow caeation (arrow)
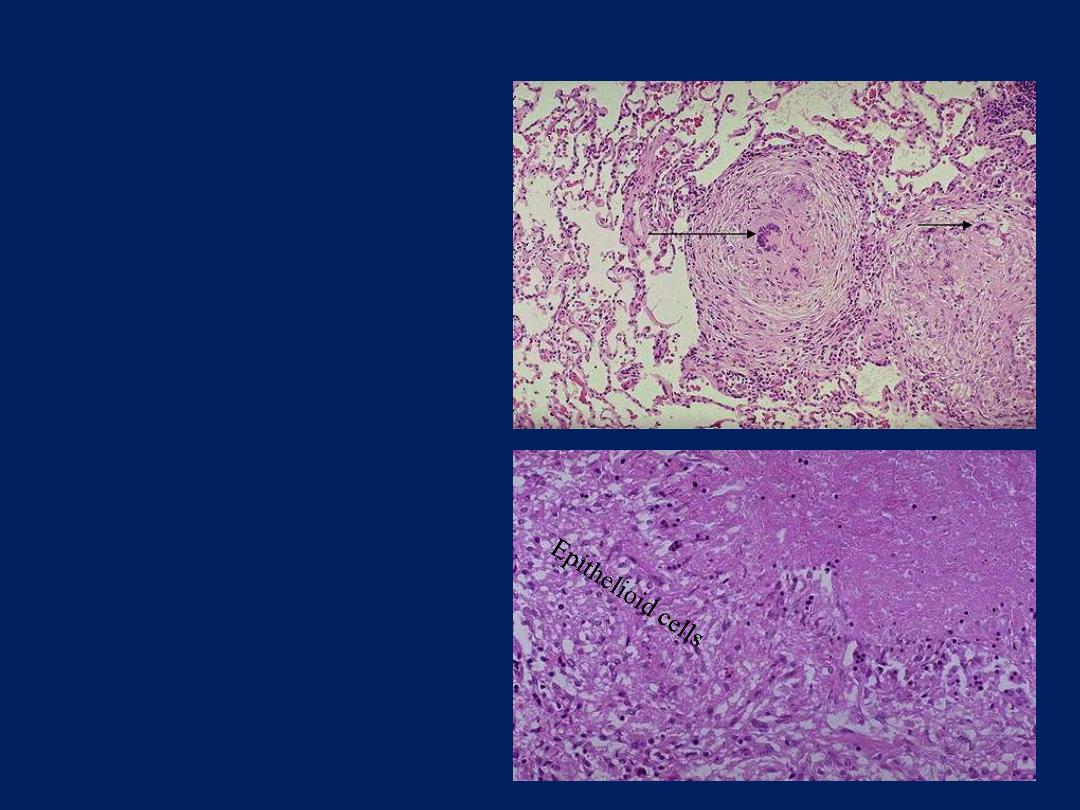
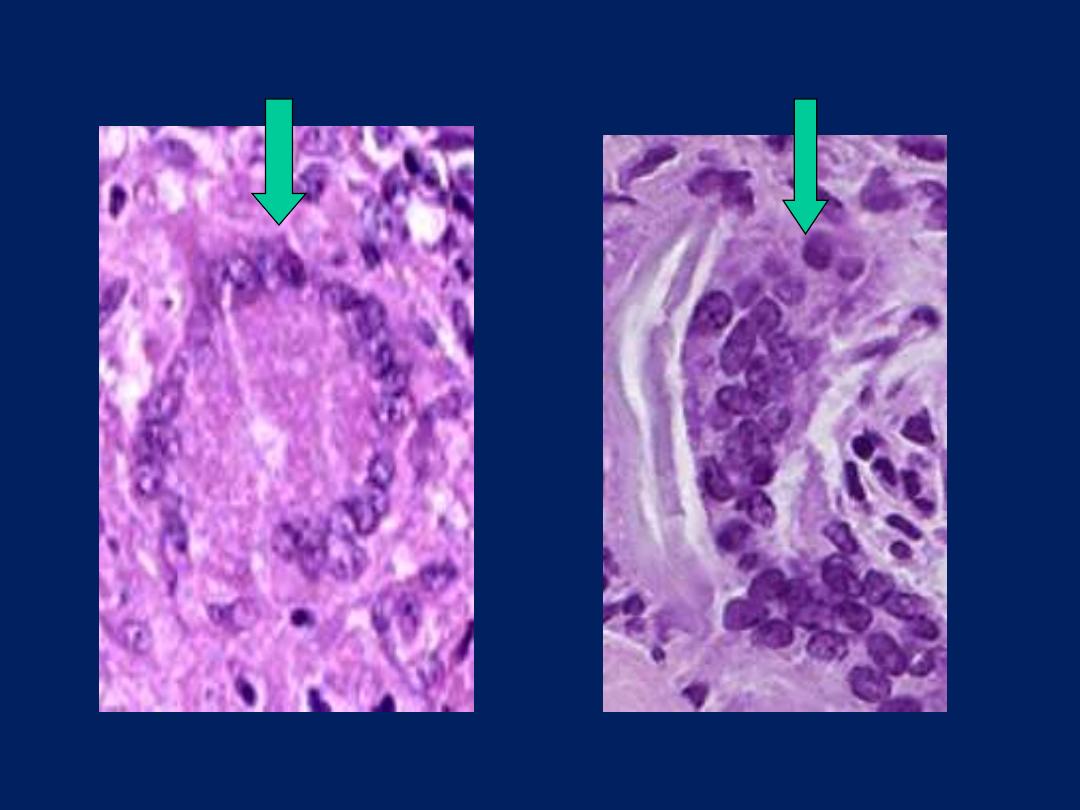
TB granulomas lung
This is a low power view
showing
two,
adjacent,
well-defined,
rounded
granulomas . From this
power the presence of
multinucleated giant cells
is obvious (arrow).
This is a high power view
showing
a
portion
of
typical
TB
granuloma.
Note
the
amorphous,
pinkish central caseation,
which is surrounded by a
rim of epithelioid cells.
caseation
Foreign body giant cells in suture granuloma
Two foreign body giant cells are seen, where there is a bluish
strand of suture material (arrow) from a previous operation
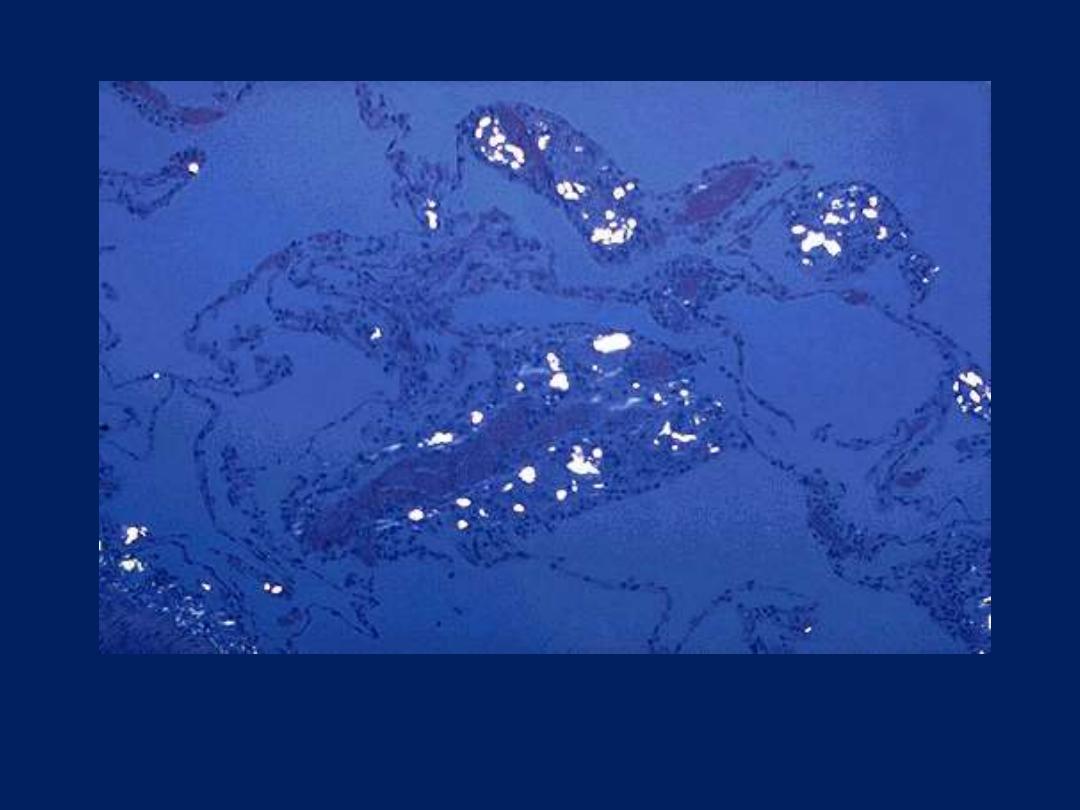
Talc granulomatosis, pulmonary, polarized light mic
Seen under polarized light are numerous bright white crystals of talc in a patient who was an
intravenous drug user. The injected drug was diluted with the talc. Such foreign material can
produce a granulomatous reaction.
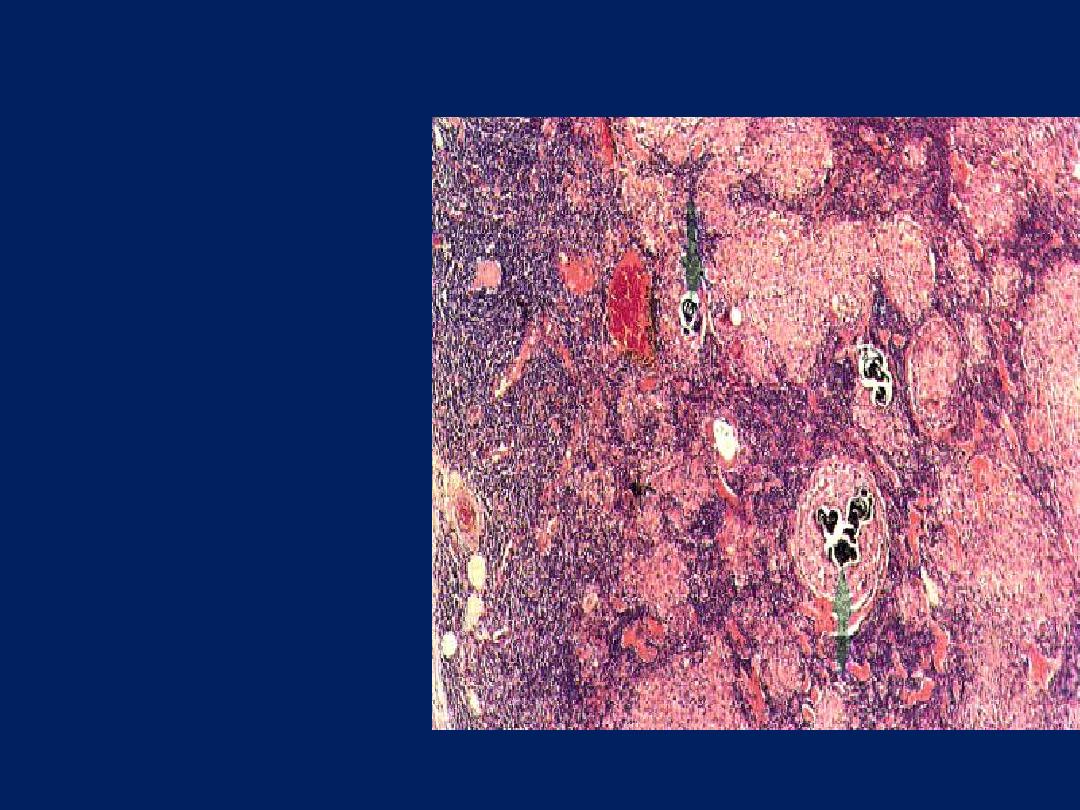
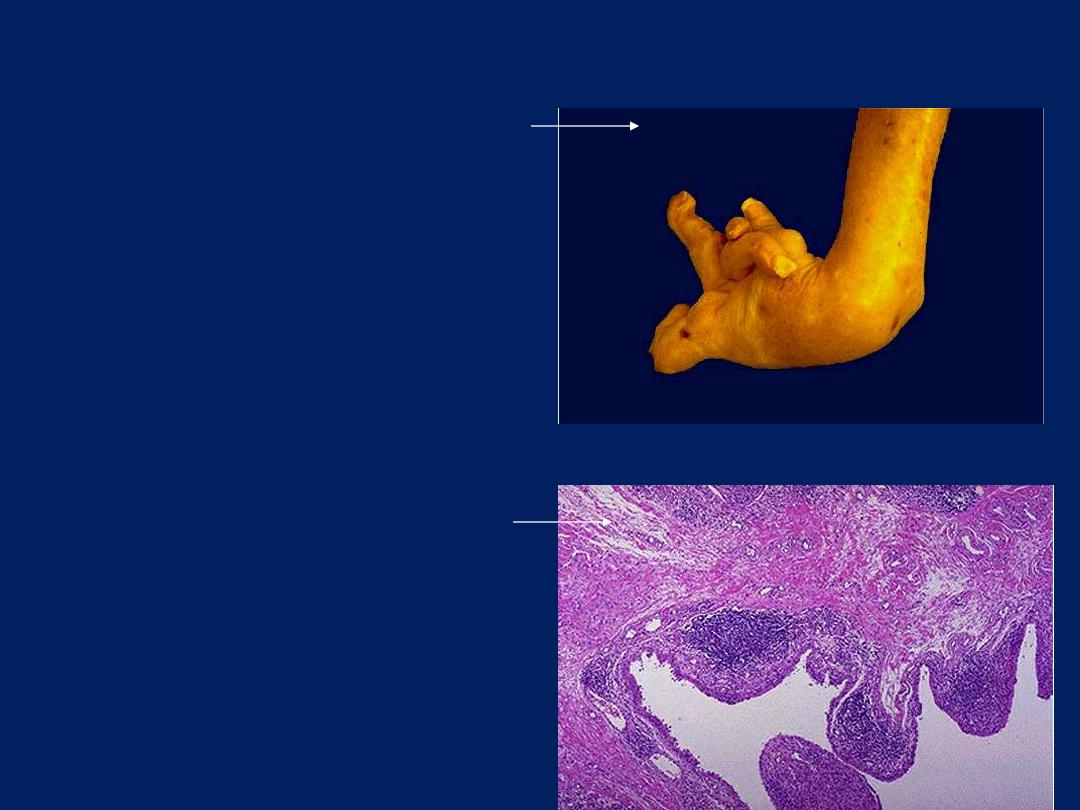
Sarcoidosis lymph node
Sarcoidosis is a granulomatous
inflammatory
disease
which affects many tissues,
including lymphoid tissue.
The capsule of the node is
on the left. The normal
architecture of the node has
been
largely
destroyed,
with some blue-staining
lymphoid tissue surviving
beneath the capsule and
between the round sarcoid
granulomas. The latter vary
widely in size, from a few
cells
to
very
large
collections (right) several
mm in diameter. They
consist
of
epithelioid
histiocytes. There is no
caseation,
but
some
contain calcified laminated
Schaumann
bodies
(arrows).
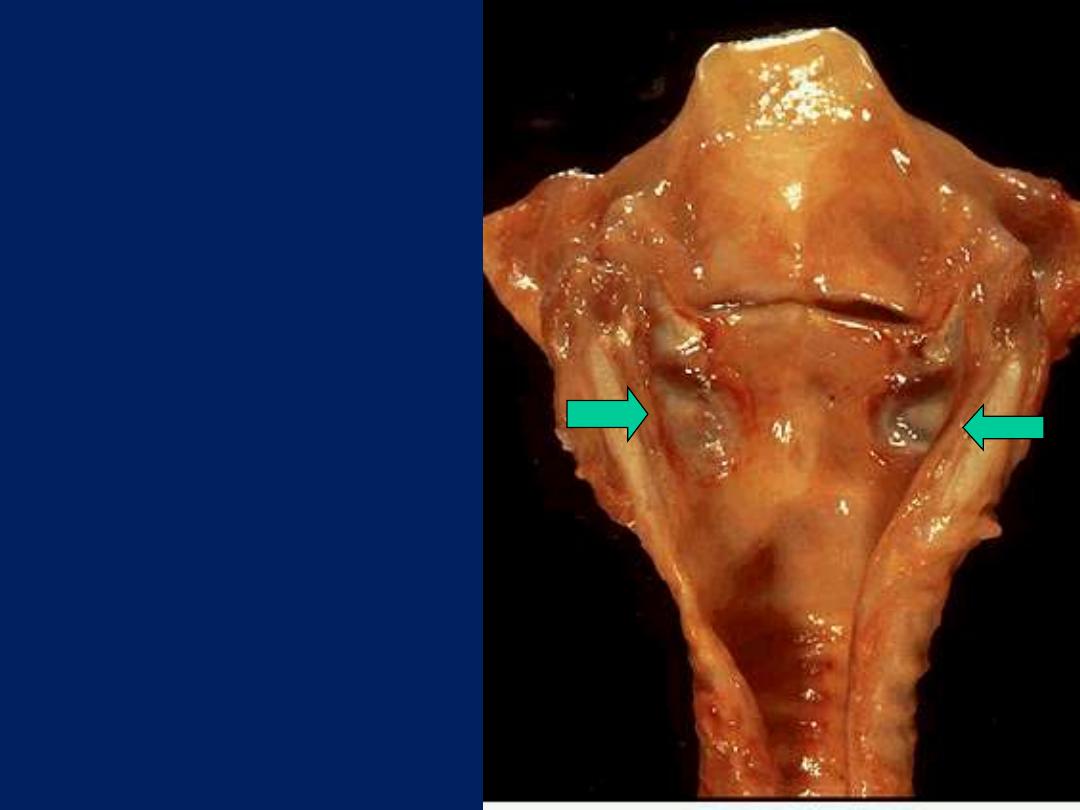
Ulceration, larynx, gross
Below the vocal cords in this larynx
are large ulcerations. Such subglottic
ulcers are produced with prolonged
endotracheal intubation in which the
cuff of the endotracheal tube fits too
tight. Thus, ulcerations can be
produce by mechanical forces. In fact,
so-called "pressure ulcers" or
"decubitus ulcers" can form in the
skin over bony prominences in
persons who are bedridden for an
extended time.
SYSTEMIC EFFECTS OF INFLAMMATION
Acute phase response (Systemic inflammatory
response syndrome [SIRS]).
These changes are reactions to cytokines
produced in response to bacterial
infections and other inflammatory
stimuli.
The acute phase response consists of several
clinical and pathologic changes:
1. Fever
is a prominent manifestation; it is
produced in response to pyrogens that act by
stimulating PG synthesis in the vascular and
perivascular cells of the hypothalamus.
2. Acute-phase proteins
are plasma proteins,
mostly synthesized in the liver, and whose
plasma concentrations may increase several
hundred times in inflammation:
a. C-reactive protein (CRP)
b. Fibrinogen
c. Serum amyloid A protein (SAA).
CRP and SAA, bind to microbial cell walls acting as
opsonins and fixing complement.
The rise in fibrinogen causes erythrocytes to form stacks
(rouleaux) that sediment more rapidly than individual
erythrocytes. This is the basis for the elevation of the
ESR.
Prolonged production of SAA causes secondary amyloidosis in
destructive chronic inflammations (e.g. rheumatoid arthritis).
Elevated serum levels of CRP are now used as a marker for increased
risk of myocardial infarction in patients with atherosclerotic
coronary artery disease.
The inflammation involving atherosclerotic plaques in the coronary
arteries may predispose to thrombosis and subsequent infarction,
and CRP is produced during inflammation. On this basis, anti-
inflammatory agents are being tested in patients to reduce the risk
of myocardial infarction.
3. Leukocytosis
is a common feature of the acute phase response, especially those induced
by bacterial infection.
The leukocyte count usually rises to 15,000 or 20,000 cells/µl, but
sometimes it may reach very high levels of 40,000 to 100,000 cells/µl.
These extreme elevations are referred to as
leukemoid reactions
because they are similar to the white cell counts obtained in leukemia.
The leukocytosis occurs initially because of accelerated release of cells
from the bone marrow reserve pool (induced by cytokines, including IL-1
and TNF) and is therefore associated with a rise in the number of more
immature neutrophils in the blood (shift to the left).
Prolonged infection also induces proliferation of precursors in
the bone marrow, caused by increased production of colony
stimulating factors (CSFs).
Neutrophilia
Refers to an increase in the blood neutrophil count. Most
bacterial infections induce neutrophilia.
Viral infections such as infectious mononucleosis, mumps, and
German measles produce a leukocytosis due to absolute
lymphocytosis
.
In bronchial asthma, hay fever, and parasitic infestations, there is an
absolute increase in the number of eosinophils, creating an
eosinophilia
.
Certain infections (typhoid fever and infections caused by viruses,
rickettsiae, and certain protozoa) are associated with a decreased
number of circulating white cells (leukopenia).
Leukopenia
is also encountered in infections that overwhelm
patients debilitated by disseminated cancer or uncontrolled
tuberculosis.
4. Other manifestations of the acute phase response include increased
pulse and blood pressure; decreased sweating; rigors, and
anorexia.
5. Disseminated intravascular coagulation (DIC)& septic shock: in
severe bacterial infections (sepsis), the large amounts of organisms
and lipopolysaccharides (LPS) in the blood stimulate the
production of enormous quantities of TNF and IL-1. High levels of
TNF cause DIC.
LPS and TNF induce tissue factor (TF) expression on endothelial
cells, which initiates coagulation; the same agents inhibit natural
anticoagulation mechanisms.
Cytokines cause liver injury and impaired liver function, resulting in
a failure to maintain normal blood glucose levels due to a lack of
gluconeogenesis from stored glycogen
.
Overproduction of NO by cytokine-activated cardiac myocytes and
vascular smooth muscle cells leads to heart failure and loss of
perfusion pressure, respectively, resulting in
cardiogenic shock
.
The clinical triad of DIC, hypoglycemia, and
cardiovascular failure is described as
septic shock.
•
Multiple organs show inflammation and intravascular
thrombosis, which can produce organ failure.
• Lung damage (adult respiratory distress syndrome
[ARDS]) results when neutrophil-mediated endothelial
injury allows fluid to escape from the blood into the
airspaces.
• The kidney and the bowel are also injured, largely due
to reduced perfusion. Septic shock is often fatal.

END
