IMMUNOPATHOLOGY
This is concerned with the pathological changes that occur in the tissues as a result of improper immune
response. Body immune responses are normal defense mechanisms designed to combat the effect of invasion by
various environmental factors such as microorganisms & toxic chemicals. It usually works effectively, but
diseases may result from
1. Inadequate immune response.
2. Excessive immune response.
3. Inappropriate immune response.
Inadequate immune responses:
These can result from immuno-deficiency states. There are two classes of immunodeficiency syndromes:
1. Primary; which is present at birth & often the result of a genetic disorder. (Fig. 6-1)
2. Secondary; which is much more common than the primary. It can be secondary to
a. Drugs
b. Diseases
(Fig. 6-2)
Primary immunodeficiency
X-linked agammaglobulinemia (Bruton disease)
This is one of the more common forms of primary immunodeficiency. It is due to failure of pre-B-cells to
differentiate into B-cells that results in the absence of gamma globulin in the blood (agammaglobulinemia). The
disease is seen primarily in males. In most cases, there are recurrent bacterial infections. For obscure reasons,
auto-immune diseases (such as SLE & dermatomyositis) also occur in up to 20% of patients.
Isolated IgA-deficiency
This is the most common of all primary immunodeficiency states. There is marked reduction in the level of
serum IgA but other immunoglobulins are normal. In most cases it is asymptomatic & detected accidentally, but
some patients have recurrent respiratory infections & diarrhea. There is also a significant, unexplained
association with autoimmune diseases.
Hyper-IgM syndrome
In normal immune responses to protein antigens, IgM & IgD antibodies are produced first, followed by the
sequential elaboration of IgG
,
IgA, & IgE antibodies. This orderly appearance of antibody types is called
isotype switching & is important for generating classes of antibodies that can effectively activate complement
&/or opsonize bacterial pathogens. Patients with this syndrome produce normal or even above normal levels of
IgM antibodies to antigens but fail to produce other antibody classes (IgG, IgA, or IgE isotypes).
Thymic hypoplasia (DiGeorge syndrome)
Affected infants show failure of T-cells to form, with hypoplasia of the thymus gland; the result of failure of
development of the third and fourth pharyngeal pouches. The latter structures normally give rise to the thymus,
parathyroid glands, & portions of the face & aortic arch. Thus in addition to the thymic & T-cell defects, there
may be parathyroid gland hypoplasia resulting in hypocalcaemia and tetany, with facial abnormalities that
include cleft lip and palate and congenital cardiac malformations. In 90% of cases there is a deletion affecting
chromosome 22q11. Transplantation of thymic tissue has successfully treated some of these infants.
Severe combined immune deficiency (SCID)
This condition may be inherited as a recessive disorder either autosomal or an X-linked. The condition is due to
failure of development of both B-cell & T-cell precursors from primitive stem cells. Therefore the thymus is
small or absent & lymphoid tissues in lymph nodes & gut are also greatly reduced. Children present early in life
with recurrent infections including candidal thrush, pneumonia & diarrhea. There is a very low blood
lymphocyte count & low blood immunoglobulin levels.
Acquired immunodeficiency syndrome (AIDS)
AIDS is a retroviral disease caused by human immunodeficiency virus (HIV) & is characterized by
1. Profound immuno-suppression leading to opportunistic infections
2. Secondary neoplasms
3. Neurological manifestations.
It is a worldwide disease. About 22 million people have died of AIDS since the epidemic was recognized some
20 years ago; 3 million people died in the year 2000 alone. On the basis of serologic data, an estimated 35
million people are infected with HIV (roughly 1 in every 100), including 1.4 million children & 17 million
women. AIDS represents the fifth most common cause of death in adults (25-44 years of age) in USA.
Epidemiology:
Transmission of HIV occurs under conditions that help the exchange of blood or body fluids containing the
virus or virus-infected cells. Thus, the three major routes are
1. Sexual contact
2. Parenteral inoculation
3. Passage of the virus from infected mothers to their newborns.
Epidemiologic studies have identified five groups at risk for developing AIDS
1. Homosexual or bisexual males (46% of reported cases).
2. Intravenous drug abusers (25% of all patients).
3. Heterosexual contacts of members of other high-risk groups (11% of patients).
4. Recipients of blood & blood components (but not hemophiliacs) who received transfusions of HIV-
infected whole blood or components (e.g., platelets, plasma) (1% of patients).
5. Hemophiliacs, especially those who received large amounts of factor VIII or IX concentrates (less than
1% of all cases).
The epidemiology of HIV infection & AIDS is different in children (<13 years age). About 1% off all AIDS
cases occurs in this population, 90% of them result from transmission of the virus from mother to infant, while
the remaining 10% are hemophiliacs & others who have received blood or blood products.
Sexual Transmission
Sexual transmission is clearly the predominant mode of infection worldwide. The virus is present in semen,
both extra-cellularly & within mononuclear inflammatory cells, & enters the recipient's body through tears or
abrasions in the genital mucosa.
Parenteral Transmission
Parenteral transmission of HIV is seen in three groups:
1. Intravenous drug abusers
2. Hemophiliacs receiving factor VIII or IX concentrates
3. Random recipients of blood transfusion.
Among intravenous drug abusers, transmission occurs through shared needles and syringes contaminated with
HIV-containing blood. This group represents the main line
in the transmission of HIV to other adult population
through heterosexual activity.
Mother-to-infant transmission (vertical transmission)
This is the major cause of pediatric AIDS. Three routes are involved:
1. In utero (transplacental spread)
2. Intra-partum, (during delivery)
3. Via ingestion of HIV-contaminated breast milk.
HIV infection cannot be transmitted by casual personal contact in home, workplace, or school, & there is no
convincing evidence for spread by insect bites.

Etiology
AIDS is caused by HIV. This is a human retrovirus belonging to the lentivirus family. Two genetically different
but antigenically related forms of HIV, called HIV-1 & HIV-2, have been isolated from patients. HIV-1 is the
more common type in USA, Europe & central Africa, whereas HIV-2 is commoner in West Africa. HIV-1
virion is spherical & contains α cone-shaped core surrounded by a lipid envelope derived from the host cell
membrane (Fig. 6-3). The virus core contains:
1- The major capsid protein P
24
.
2- Nucleocapsid protein P
7
/P
9
.
3- Two copies of genomic RNA
4- The three viral enzymes (protease, reverse transcriptase & integrase).
P
24
is the most readily detectable viral antigen useful in the diagnosis of HIV infection in blood screening. The
viral core is surrounded by a matrix protein called P
17
. The viral envelope is studded by two viral glycoproteins
(gp
120
& gp
41
) critical for HIV infection of cells. The highly effective anti HIV-1 protease inhibitor drugs
prevent viral assembly by inhibiting the formation of mature viral proteins. In addition there are other
regulatory genes, the products of which are important for HIV pahtogenicity, & a number of therapeutic
approaches are being developed to block their actions. Molecular analysis of different viral isolates reveals
considerable variability in many parts of the HIV genome. Most variations cluster in certain regions of the
envelope glycoproteins. Because the immune response against HIV-1 is targeted against its envelope, such
extreme variability in antigen structure poses a barrier for vaccine development.
Pathogenesis
The two major targets of HIV infection are the immune system & the central nervous system.
Immunopathogenesis of HIV disease:
AIDS leads to severe impairment of the cell-mediated immunity system. Infection by HIV leads to destruction
of CD
4
lymphocytes & a decreased helper/suppressor T-cell ratio in the blood. The virus gains entry to T-cells
by attaching to surface CD
4
molecules. It takes over cellular metabolism to synthesize new virus. The CD
4
molecule is a high-affinity receptor for HIV. This explains the selective tropism of the virus for CD
4
+T-cells &
its ability to infect other CD
4
+cells, particularly macrophages & dendritic cells. However binding to CD
4
is not
sufficient for infection; the HIV envelope gp
120
must also bind to other cell surface molecules (co-receptors) to
facilitate cell entry (Fig. 6-4). The virus core containing the HIV genome enters the cytoplasm of the cell. The
viral genome then undergoes reverse transcription, leading to formation of complementary DNA (cDNA). In the
dividing T-cells, the cDNA enters the nucleus & integrates into the host genome. After integration, the provirus
may remain non-transcribed for months or years & the infection becomes latent; alternatively, proviral DNA
may be transcribed to form complete viral particles that bud from the cell membrane, leading to cell death (Fig.
6-5).
HIV colonizes the lymphoid organs (spleen, lymph nodes, and tonsils). Infected T-cells, macrophages, &
dendritic cells represent reservoirs of infection.
Initially, the immune system can vigorously proliferate to replace the dying T-cells, thus masking the massive
cell death occurring primarily in the lymphoid tissues. Due to loss of CD
4
+ cells, patients will have an inversion
of the CD
4-
/CD
8
ratio in the peripheral blood; normally it is about 2, while in AIDS patients the ratio ≤ 0.5.
ADIS patients will also have qualitative defects in T-cell function.
Pathogenesis of central nervous system involvement:
The nervous system is a major target of HIV infection. Macrophages & their equivalents in the CNS; the
microglia, are mainly infected with HIV. The virus is mostly carried into the brain by infected monocytes. The
mechanism of HIV-induced damage of the brain remains obscure. It is believed that neurologic deficit is caused
indirectly by viral products & soluble factors e.g. cytokines produced by macrophages/microglia.
Clinical phases
There are four phases (Fig. 6-6)
1. Primary infection (sero-conversion): after infection, a median time of 2 months elapses before antibodies
to HIV are detected in the blood. Rapid viral replication occurs in all organs (P
24
antigen is detectable in
blood), & an immune response develops, with increased number of virus-specific CD
8
+cytotoxic T-cells.

About 50% of patients develop an influenza-like illness, skin rashes or lymphadenopathy, associated with
transient fall in CD
4
+T-cells. This phase represents the early acute phase.
2. Asymptomatic phase (incubation period): it represents a stage of relative containment of the virus. The
immune system is largely intact, but there is continued HIV replication. The length of this phase is
uncertain, it can last for years. Patients have antibodies to HIV in blood, are infective, can transmit the
disease, & are asymptomatic.
3. AIDS-related complex: the proportion of CD
4
infected cells increases, their function is partially impaired
& their numbers in blood fall to around 400 cells/µliter. It is associated with non-specific general malaise,
fever night sweats, weight loss & diarrhea. Persistent generalized lymphadenopathy is common, with
serological & hematological evidence of impaired cell-mediated immunity & reduced CD
4
+T-cells.
Superficial fungal infections are frequent & infections with pathogens as Salmonella & Haemophilus are
sever. Similarly, gynecological infections such as candidiasis & pelvic inflammatory disease are increased.
2 & 3 phases represent the chronic phase (middle phase), that may last 7 to 10 years. However, sometimes
rapid progression after 2 to 3 years happens.
4. AIDS (crisis phase): it represent the final phase with fully developed immunodeficiency characterized by
fever , fatigue , weight loss , generalized lymphadenopathy & diarrhea ; the CD
4
+cell count is below 500
cells/μL. The patients develop serious opportunistic infections, secondary neoplasms &/or neurologic
manifestations (so called AIDS-defining conditions), & the patient is said to have developed full-blown
AIDS. Also any individual with CD
4
+cell counts less than or equal to 200/ μL is diagnosed as having ADIS.
Opportunistic infections
These are responsible for about 80% of deaths in patients with AIDS.
1. Pneumocystis carinii pneumonia is the presenting feature in many cases.
2. Recurrent mucosal candidiasis
3. Disseminated cytomegalovirus infection (particularly enteritis & retinitis)
4. Herpes simplex; especially sever ulcerating oral & perianal infections
5. Mycobacterium tuberculosis & atypical mycobacteria (mycobacterium ovium-intracellular), usually
disseminated infections
6. Toxoplasmosis, which is the most common secondary infection of the central nervous system
7. Cryptococcal meningitis is also quite frequent.
8. Cryptosporidium or isospora belli infections are often the cause of the so common persistent diarrhea.
However, bacterial pathogens such as Salmonella & Shigella species may also be seen.
Neoplasms
The basis of increased risk of malignancy is multifactorial and include
1. Profound defects in T-cell immunity
2. Dysregulated B-cell & monocyte functions
3. Infections with known viruses e.g. Human herpes virus type 8, EBV, human papilloma virus & unknown
viruses.
Patients with AIDS have a high incidence of certain tumors as:
1. Kaposi sarcoma (KS): this vascular tumor is the most common neoplasm in AIDS patients. It is more
common among homosexual and heterosexual males than in intravenous drug abusers or other risk groups.
KS in AIDS patients is usually multicentric & tends to be aggressive. It can affect the skin, mucous
membranes, GIT, lymph nodes, & lungs. KS is associated with human herpes virus 8 infections in AIDS
patients. Non-Hodgkin lymphomas: the second most common neoplasm in AIDS patients. These tumors
are highly aggressive, & involve many extra-nodal sites, commonly the brain; so primary lymphoma of the
brain is considered as an AIDS-defining condition. 30%-40% of these lymphomas are associated with EBV
infection.
2. Cervix uteri carcinoma: this due to human papilloma virus infection in ADIS patients. This virus is
intimately associated with squamous cell carcinoma of the cervix & its precursor lesions (cervical dysplasia
& carcinoma in situ); therefore, gynecologic examination should be routinely done for HIV-infected
women.

Central nervous system involvements:
This is common in AIDS patients. 40%-60% of patients have clinically evident neurologic dysfunction. In
addition to opportunistic infection & neoplasms, patients may have a progressive encephalopathy clinically
called AIDS-dementia complex.
Vaccine
Molecular analyses have revealed an alarming degree of polymorphism in viral isolates from different AIDS
patients; this renders vaccine development more difficult. In addition, the nature of the protective immune
response is not yet fully understood. Therefore, at present prevention & effective public health measures remain
the mandatory in the fight against AIDS.
Inappropriate immune response:
Transplant rejection:
Organ transplantation is used increasingly to treat irreversible diseases of the kidney, liver, heart, lung, & bone
marrow. Unfortunately, the action of the immune system of the recipient can lead to destruction of the
transplanted tissue a process termed" transplant rejection". This is a complex immunologic phenomenon
involving both cell -& humoral-mediated hypersensitivity responses of the host, directed against
histocompatibility antigens, human leukocytes antigens (HLA) on the donor allograft. The endothelial cells that
line the blood vessels of the graft are particularly rich in both HLA & blood group antigens, thus blood vessels
are important targets of the host's immune response to a transplanted allograft.
Patterns of transplant rejection:
Rejection reactions have been classified as
1. Hyperacute
2. Acute
3. Chronic
The changes are described in the context of renal transplants; however, similar changes are seen in any other
vascularized organ transplant.
Hyperacute rejection:
This occurs within a very short time from the moment the organ is perfused by the host's blood (minutes to a
few hours). In this form there is a widespread intravascular thrombosis in small vessels, with focal necrosis. It is
the result of pre-formed humoral host antibodies reacting with antigens in the graft. These preformed antibodies
developed due to
1. Previous rejection of a transplant
2. Multiparous women who develop anti-HLA antibodies against paternal antigens shed from the fetus (a
rejection in this instance will affect the transplanted organ donated by the husband and offspring)
3. Prior blood transfusions because platelets and WBCs are rich in HLA antigens and donors and recipients are
usually not HLA-identical.
Since testing recipients for the presence of antibodies to donor lymphocytes become a routine practice,
hyperacute rejection occurs in less than 0.4% of transplants. It is typically recognized grossly by the surgeon
just after the vascular anastomosis is completed. The hyperacutely rejected kidney rapidly becomes cyanotic,
mottled, & flaccid & may excrete only a few drops of blood-stained urine. In contrast to a non-rejected kidney
graft that regains a normal pink coloration & tissue turgor & promptly excretes urine. Histologically the rejected
kidney show acute arteritis & arteriolitis, vessel thrombosis & ischemic necrosis.
Acute rejection:
It occurs within days or weeks of transplantation, but may also appear after cessation of immunosuppressive
therapy that is given to the recipient to prevent rejection. It is mediated by both humoral & cell-mediated
mechanisms. Acute cellular rejection is mediated by T-cells reacting against donor HLA antigens, particularly
class II. It is accompanied by signs of renal failure. Histologically there is extensive interstitial CD
4
+ & CD
8
+T-
cell infiltration. The humoral component of acute rejection is characterized by vasculitis with endothelial
necrosis, neutrophils infiltration of vessel walls, & damage to the intima and elastic lamina of the larger arteries
in the graft.

Chronic rejection:
In recent years, acute rejection has been significantly controlled by immunosuppressive therapy; this has
resulted in the emergence of chronic rejection as an important cause of graft failure. Chronic rejection occurs
slowly & progressively after transplantation (months to years). It is the result of slow breakdown of the host's
tolerance to the graft and may be due to inadequate immune suppression. The condition is manifested by a
progressive rise in serum creatinine levels (which is an index of renal dysfunction), over a period of 4 to 6
months. Histologically, there is intimal fibrosis mainly in arteries & arterioles, leading to secondary ischemic
damage to the parenchyma manifested by hyalinization and loss of glomeuli, interstitial fibrosis, & tubular
atrophy. Chronic rejection does not respond to standard immunosuppressant regimens.
Complication of renal transplantation:
1. Thrombosis of vascular graft
2. Recurrence of original renal disease.
3. Transplant rejections, hyperacute, acute or chronic.
Transplantation of other solid organs
Beside the most frequent kidney transplantation, transplantations of liver, heart, lungs, & pancreas are also
commonly performed. All these organs transplantation, unlike that of the kidney, can be performed with a
disregard to histocompatibility typing. In transplantation of these organs instead we consider
1. ABO blood group typing
2. Absence of preformed circulating antibody
3. Body habitus (e.g. a child cannot receive a heart transplant from an adult).
Autoimmune diseases
Autoimmune diseases are the result of immune reactions against self-antigens i.e. against body tissue or
individual tissue components. Sometimes the immune response is an antibody response (autoantibody), or it is a
cell-mediated immune response. In autoimmune diseases, the normal mechanisms ensuring tolerance for self-
antigens have broken down. (Self-tolerance indicates lack of immune responsiveness to one's own tissue
antigens). Some autoimmune diseases have a genetic component; e.g. certain diseases are associated with
particular HLA histocompatibility types. In other situations, an autoimmune disease can be triggered by a
microbial infection.
Mechanisms involved in the pathogenesis of autoimmune diseases
There are regulatory mechanisms that present normally to prevent the occurrence of autoimmune diseases.
Failure of such mechanisms is responsible for the occurrence of such diseases in some 3% of the population that
suffer from such diseases. These will be discussed under the heading of immunological tolerance and its
breakdown.
Immunological tolerance
Both T- and B-cells bear self-reactive molecules (receptors) that can recognized self-antigens and react with
them to produce eventually tissue damage and this is the essence in the production of various autoimmune
diseases. To avoid such incidents T- and B-cells bearing such molecules (receptors) must be either eliminated or
down-regulated so that the immune system is made specifically non-reactive i.e. tolerant to self antigens. Since
T-cells and in particular CD4+ T-cells, have a central role in controlling all immune responses, the process of T-
cell tolerance is much more important than B-cell tolerance in the avoidance of autoimmunity. This is because
not only T-cells may produce tissue damage directly but also self-reacting-B-cells will not be able to produce
auto-antibodies unless they receive appropriate T-cell help.
Processes that induce specific tolerance arise inside the thymus (thymic tolerance) or outside the thymus
(peripheral tolerance.
Thymic tolerance is achieved through eliminating all T-cells capable of recognizing self-proteins. This is not,
however, induced to many tissue-specific proteins.
Peripheral tolerance this involves several mechanisms
1. Immunological ignorance: the self-antigens are invisible to the immune system either because of
sequestration of the antigen e.g. within the vitreous humour of the eye or because the self antigens are presented
to the CD4+ cells in low levels that is not enough to activate such cells. To prevent large amounts of self-
antigen from gaining access to antigen-presenting cells a slow gradual tissue breakdown is achieved through
apoptosis.

2. Anergy: CD4+ T-cells requires two signals to become activated and initiate an immune response: an antigen-
specific signal through the T-cell antigen receptor and a second, nonspecific signal through interaction of CD4+
cells with antigen-presenting dentritic cells. Such an interaction is only likely to occur in secondary lymphoid
tissues such as lymph nodes i.e. the encounter of both cells is very restricted.
If no second signal is available then stimulation through T-cell receptor alone leads to apoptosis or a state of
longstanding unresponsiveness called anergy.
3. Suppression; self-reactive T-cells may be actively suppressed by inhibitory T-cells, which recognize the
same antigen (suppressor T-cells; CD8+). This is achieved through cytokines produced by the suppressor T-
cells to inhibit nearby helper (CD4+) T-cells.
4. B-cell tolerance: this is less complete than T-cell tolerance. The production of self-reactive antibodies by
these B-cells is limited mainly by the lack of T-cell help for cell antigens.
Breakdown of tolerance
For autoimmune diseases to occur, the above mechanisms of immunological tolerance must be broken down.
1. Overcoming peripheral tolerance; resulting from excessive access of self-antigens to antigen presenting
cells, excessive nonspecific signaling, or alterations in which self-antigens are presented to the immune system.
All these are likely to happen when inflammation or tissue damage is present. The structures of the self-
antigen’s peptides (self-peptides) may be altered by viruses, free radicals or ionizing radiation. With such
structural changes the previously established tolerance is bypassed. Tissue damage may release antigens that are
already sequestrated from the immune system e.g. spermatozoa & ocular antigens. Post-traumatic uveitis &
orchitis (after vasectomy) probably result from immune responses against antigens normally sequestered in the
eye & the testis.
2. Molecular mimicry: structural similarity between self-antigens and microbial antigens may trigger an
immune response. In systemic infection, this cross reactivity will cause expansion of the responsive T-cell
population recognizing the self-peptide if local conditions allow. The process is known as molecular mimicry.
For example, rheumatic heart disease sometimes follows Streptococcal infection because antibodies to
Streptococcal M protein cross-react with cardiac glycoprotiens.
Once tolerance has broken down, the resulting immunological mediated inflammation and tissue damage may
allow presentation of further peptides. The immune response broadens and local tissue damage accelerates. This
domino-like process is known as epitope spreading.
(Domino effect: by which one event triggers a succession of other, often similar, events, like a falling domino at
the beginning of a line of up-ended dominoes).
Etiology of autoimmune diseases
The interaction between genetic and environmental factors is important in the pathogenesis of autoimmune
diseases.
Genetic factors
Family studies have confirmed a genetic contribution in all autoimmune diseases. This is supported by the
findings that
1. Different autoimmune diseases may cluster within the same family (such as SLE, autoimmune hemolytic
anemia, & autoimmune thyroiditis).
2. Subclinical autoimmunity is common among family members.
The genetic contribution to autoimmune disease usually involves multiple genes. The strongest associations
between genetic factors and autoimmunity involve alleles of the major histocompatibility complexes (MHC).
This is because of central role of the products of many of these genes in the
1. T-cell function
2. Control of immunity and inflammation.
It is likely that the MHC class II alleles influence the presentation of autoantigenic peptides to T-cells.
An example of such a connection is the well-known strong association of HLA-B
27
with ankylosing spondylitis.
Genetic factors in autoimmunity:

Genetic factors play a significant role in the predisposition to autoimmune diseases. This is supported by the
following
1- There is familial clustering of several human autoimmune diseases Linkage of several autoimmune
diseases with HLA, especially class II antigens.
Environmental factors
These may trigger autoimmune diseases and include
1. Hormones
2. Infections
3. Drugs
4. UV radiation
Hormones
The contribution of hormones in the pathogenesis of autoimmune diseases is supported by the following
1. Most autoimmune diseases affect females much more commonly than males; hormonal factors, besides
genetics, must play a major role in this gender difference.
2. The peak age of onset of most autoimmune diseases is within the reproductive years. Evidences implicate
estrogens as triggering factors.
3. In animal models removal of the ovaries inhibits the occurrence of autoimmune diseases (e.g. SLE), while
estrogen administration accelerates the onset of the disease.
Infections
The relationship between infection and autoimmunity is clearest in the situation of molecular mimicry.
Autoimmune diseases tend to be less common in parts of the world with high incidence of parasitic diseases and
other infections. This inverse relationship between the occurrence of autoimmune diseases and the incidence of
various infections is supported by experiments on animal models.
3. Drugs
Drug-induced autoimmunity may involve mechanisms comparable to molecular mimicry, whereby the drug or
drug-self molecule complex has a structural similarity to self that allows bypassing tolerance. Drug-mediated
autoimmunity affects only a small proportion of those treated and is probably genetically determined. For
example, HLA-DR2 is associated with penicillamine-induced myasthenia gravis, whereas DR3 is associated
with penicillamine-induced nephritis. Genetic variation in drug metabolism is also important. Individuals who
are slow metabolizers of the offending drug are more prone to develop the disease (for e.g. drug-induced SLE)
than rapid metabolizers. Slow metabolism of the offending drug may give more time for the formation of
immunogenic conjugates between the drug and self-molecule.
4. Ultraviolet radiation
Exposure to UV radiation, usually in the form of sunlight is a known trigger for skin eruptions
(photosensitivity skin eruption) and sometimes systemic involvement in patients with SLE. UV radiation acts
in this context through two possible mechanisms
a. modifying self-antigens to become immunogenic
b. enhancing apoptosis (cell death) of the cells, which lead to cell surface expression of auto-antigens that are
usually hidden within the cell. Such exposure of the antigens leads to Ag-Ab reaction that triggers tissue
damage.
Autoimmune diseases may be either organ specific (response directed against a single component of a single
tissue) or more often, a non-organ-specific autoimmune disease (response directed against a component that
present in many tissues & organs throughout the body.
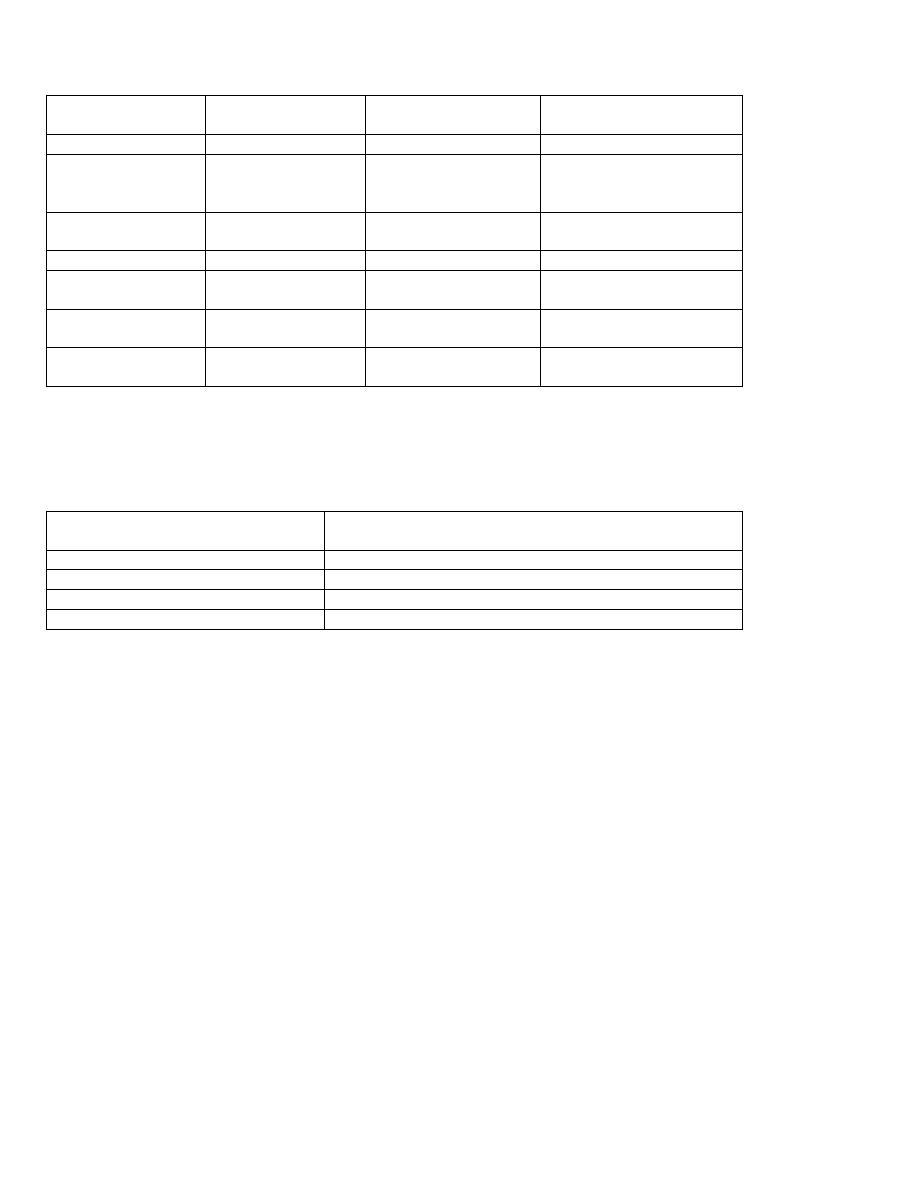
The organ specific autoimmune diseases are listed in following tables:
Organ
Disease
Associated
autoantibody
Comment
Skin
Vitiligo
Antityrosine Ab
Hypopigmentation
Thyroid
Grave's disease
thyroid-stimulating Ab
thyroid
growth-
stimulating Ab
Hyperthyroidism
Thyroid
Hashimoto's disease
Anti-thyroid
specific
Ab
Hypothyroidism
Adrenal cortex
Addison's disease
Anti-adrenal Ab
Hypoadrenocorticalism
Stomach
Autoimmune
(type
A) gastritis
Anti-intrinsic factor &
parietal cell Ab
Pernicious anemia
Pancreatic islet cells
(insulin-producing)
Type
I
diabetes
mellitus
Anti-islet
B-cell
(insulin) Ab
Diabetes mellitus
Skeletal muscle
Myasthenia gravis
Acetylcholine receptors
Ab
Muscle fatigue
Multi-organ involvement is frequently caused by secondary damage due to circulating immune complex. This
group of disorders is often collectively called the ''connective tissue diseases'' or ''collagen vascular
diseases''.
Disease
Main organ involved
Systemic lupus erythematosus
Skin , kidney , joints , heart , lung
progressive systemic sclerosis
Skin , gut , lung
Polymyositis- dermatomyositis
Skeletal muscle , skin
Rheumatoid disease
Joints , lungs , systemic vessels
Systemic lupus erythematosus (SLE):
SLE is an autoimmune disease and one of the ''connective tissue disorders''. It is a fairly common disease, with a
prevalence of 1:2500 persons. Like most autoimmune diseases, there is a strong female predominance (9:1) and
is particularly common in young & middle-aged individuals. Clinically, the disease is characterized by
remissions & relapses, with an acute or insidious onset that may involve any organ in the body. Acute flare-ups
are usually controlled by steroids or other immunosuppressive drugs. Renal failure, intercurrent infections, &
diffuse central nervous system involvement are the major causes of death.
Etiology & pathogenesis:
SLE is a complex disease of multifactorial origin including genetic, hormonal, & environmental factors,
resulting in a T-cell & B-cell activation that leads to the production of several autoantibodies. The main defect
in SLE is a failure to maintain self-tolerance. Many types of autoantibodies can be identified in SLE patient
particularly antinuclear antibodies (ANAs), which are directed against several nuclear antigens. ANAs can be
identified using the indirect immunofluorescence test, which is positive in virtually every patient with SLE, so
that the test is quite sensitive. However, it is not specific. However, the presence of autoantibodies against
double stranded DNA is diagnostic to SLE. Antibodies against blood cells, including red cells, platelets, &
lymphocytes, are found in many patients. Antiphospholipid antibodies are found in 40% to 50% of SLE
patients. Because phospholipids are required for blood clotting, SLE patients with antiphospholipid antibody
tend to have venous and arterial thrombosis, thrombocytopenia & recurrent spontaneous miscarriages
(antiphospholipid syndrome).
Genetic factors:
There is much evidence supporting the genetic predisposition for SLE:
1. There is a higher rate of concordance in monozygotic twins (25%) than in dizygotic twins (1%-3%).
2. Family members have an increased risk of developing SLE, & up to 20% of clinically unaffected first-
degree relatives may have autoantibodies.
3. There is a positive association between SLE & class II HLA genes.
4. About 6% of SLE patients have inherited deficiencies of complement components. Lack of complement
may impair removal of immune complexes from the circulation & favor tissue deposition, resulting in
tissue injury.
Nongenetic factors:
1. The clearest example of environmental factors in initiating SLE is the occurrence of a lupus-like
syndrome in patients receiving certain drugs, including procainamide & hydralazine. Thus, most
patients treated with procainamide for more than 6 months develop ANAs, with clinical features
of SLE appearing in 15%-20% of them.
2. Sex hormones; the female predominance of SLE, reflects the important influence of sex
hormones in the development of the disease, due to the helpful effects of estrogens on antibody
synthesis.
3. Exposure to ultraviolet light exacerbates the disease in many individuals. Ultraviolet light may
damage DNA & promote cell injury that will release cellular contents & augment the formation
of DNA/antiDNA immune complexes.
Mechanism of tissue injury:
Most of the visceral lesions are caused by immune complexes (type III hypersensitivity). For example,
DNA/anti-DNA complexes can be detected in the glomeruli. In addition, autoantibodies against red cells, white
cells, & platelets causing effect by type II hypersensitivity. The denaturated nucleus of an injured cell will be
engulfed by a neutrophil or macrophage producing the LE cell. LE cell test is positive in about 70% of patients
with SLE.
Clinical manifestations:
The clinical presentation of SLE is so variable & with similarities to other autoimmune connective tissue
diseases (rheumatoid arthritis, polymyositis & others) so that it has been necessary to develop diagnostic
criteria. If a patient has four or more of the criteria, serially or simultaneously, during any interval of
observation, the diagnosis of SLE is established. The range of features that can occur in SLE is shown by the
American Rheumatism Association
List of Diagnostic Criteria for SLE
1. Discoid skin rash.
2. Malar rash.
3. Photosensitivity.
4. Oral ulcers.
5. Arthritis.
6. Serositis.
7. Renal disorder.
8. Neurologic disorder.
9. Hematologic disorder.
10. Immunologic disorder.
11. Presence of antinuclear antibody.
Skin rashes of various types occur in about 80% of all patients with SLE. One of the most common tissues
affected in SLE is the skin. The most common patterns of skin rash are:
1. Chronic discoid LE: round (discoid), red scaly telangiectatic plaques, usually on the face & scalp,
2. Malar skin rash: a symmetrical, slightly raised red erythematous rash on the cheeks & across the bridge of
the nose (butterfly rash). This is seen in 50% of the patients.
3. Photosensitivity reactions: exposure to sunlight (ultraviolet light) exacerbates the erythema, & the rash will
be seen on the face & sun-exposed areas mainly. Direct immunofluorescence microscopy reveals deposition
of immunoglobulins (IgG, IgM) & complement at the dermo-epidermal junction. Histologically: there is

characteristic liquefactive degeneration of the basal layer of epidermis, edema at the dermo-epidermal
junction & mononuclear infiltrates around blood vessels & skin appendages. (Fig. 6-7)
4. An acute necrotizing vasculitis: clinically, producing slightly raised erythematous patches.
5. Oral mucosal lesions in SLE produce superficial erosions & ulcers.
6. Musculoskeletal symptoms may be the earliest presenting feature of SLE. Joint pain and swelling occurs in
about 90% of patients.
7. Serositis: the pericardium & pleura are usually affected. In the acute phase they may lead to serous effusion.
8. Renal disorder: kidney involvement in SLE is common, & is an important cause of morbidity & mortality.
The severity of involvement can vary from minor abnormalities (such as asymptomatic albuminuria) to
sever glomerular disease leading to renal failure. The basis of the glomerular damage is the deposition of
immune complexes within glomeruli. (Fig. 6-8)
9. Neurological & psychiatric disorders are common in SLE.
10. Hematological abnormalities are common in SLE, some having an unknown cause, & others having an
autoimmune mechanism:
a. Normocytic, hypochromic anemia.
b. Autoimmune hemolytic anemia
c. Leucopenia usually due to disproportionate reduction of lymphocytes (lymphopenia).
d. Thrombocytopenia
The spleen may be moderately enlarged. Involvement of the heart showing mainly pericarditis, myocarditis &
vascular lesions called Libman-Sacks endocarditis, which represent a nonbacterial verrucous endocarditis. (Fig.
6-9)
Systemic sclerosis (SS):
It is one of the connective tissue diseases, & affects many systems & organs. It is three times more common in
women than in men, & occurs mainly in middle-aged or elderly individuals. The main abnormality is an excess
formation of fibrous tissue, which leads to rigidity of the affected organ. Vessel wall thickening & perivascular
fibrosis are characteristic features in SS, & are responsible for slowly progressive ischemic damage in a wide
range of tissues. The skin is the most commonly affected organ (scleroderma), but the alimentary tract, lung,
kidney & heart may also be involved.
There is usually affection of the skin of the fingers & distal regions of the upper extremities. Extending to the
upper arms, shoulders, neck & face may occur. There is dermal thickening due to fibrous replacement of the
normal dermal structures.
Rheumatoid disease (rheumatoid arthritis) (RA)
RA is a multi-system connective tissue disease in which the dominant effects are on the joints. It is
characterized by the presence of a circulating autoantibody, ''rheumatoid factors'' (seropositive arthritis). RA
is a very common condition, with a prevalence of about 1%. It is three to five times more common in women
than in men, & the usual age of onset is between 35 to 45 years. The disease is not limited to joints but also
affects, among others, the skin, lungs, blood vessels, eyes & the hemopoietic system.
Pathologic changes:
RA typically presents as symmetric polyarthritis, mainly affecting the small joints of the hands & feet.
However, larger joints may also be involved e.g. ankles, knees, wrists, elbows & shoulders. Classically, the
proximal interphalangeal & metacarpophalangeal joints are affected. The affected joints become swollen,
painful & warm, often with redness of the overlying skin. There are three main pathological changes
1. In the early stage there will be rheumatoid synovitis. The synovium is swollen with prominent villous
pattern. There is a great increase in chronic inflammatory cells mainly lymphocytes, plasma cells &
macrophages with formation of lymphoid follicles. There is marked synovial hypertrophy & hyperplasia,
often with increased vascularity due to angiogenesis. There is often fibrinous effusion in the joint space; the
fibrin gets deposited on the synovial surfaces.
2. With time there is articular cartilage destruction with replacement by vascular granulation tissue (pannus).
The latter grows across the surface of the articular cartilage from the edge of the joint.

3. The inflammatory pannus causes focal destruction of the subjacent bone; this is manifested as ''erosions'' on
radiographs. Following destruction of the articular cartilage & erosion of the subarticular bone, the pannus
fills the joints space. Subsequent fibrosis & classification may cause permanent ankylosis of the affected
joint. The loss of articualr cartilage can lead to secondary osteoarthritis (a degenerative joint disease),
especially in the weight-bearing joints such as the knee. Destruction of tendons, ligaments, & joint capsules
produces deformities of the joints; that of the hand are characteristic, which include radial deviation of the
wrist, ulnar deviation of the fingers, & flexion-hyperextension abnormalities of the fingers (swan-neck
deformity).
Rheumatoid subcutaneous nodules develop in about 25% of the patients. They occur along the extensor
surface of the forearm or other areas subjected to mechanical pressure. Rheumatoid nodules are firm, nontender,
oval or rounded masses up to 2 cm in diameter. Microscopically there is central focus of fibrinoid necrosis
surrounded by a palisade of macrophages which is rimmed by granulation tissue.
Pulmonary involvement in RA takes the form of interstitial pneumonitis & fibrosing alveolitis, which leads
eventually to a pattern of interstitial fibrosis called ''honeycomb lung''. The latter is also caused by other
diseases such as systemic sclerosis.
Anemia is very common in rheumatoid disease as is increased susceptibility to infections, & sepses, which are
important & common causes of death.
Pathogenesis of RA:
There is a genetic predisposition to RA which is suggested by
1. The increased frequency of this disease among first-degree relatives.
2. The strong association of the disease with HLA-DR
4
&/or HLA-DR
1
.
About 80% of the patients have rheumatoid factors (RF) in their serum & synovial fluid. RF represents an
autoantibody mainly of IgM class directed against the Fc portion of IgG. RF & IgG form immune complex that
fix complement, attract neutrophils, & lead to injury by a type III hypersensitivity reaction.
It is proposed that the disease is initiated in a genetically predisposed individual, by activation of helper T-cells
possibly by microbial agent, the activated CD
4
+cells produce cytokines that will:
a. Activate macrophages & other cells in joint space to release degrading (proteolytic) enzymes & other
factors that initiate inflammation and cause tissue destruction.
b. Activate B-cells, which produce RF (autoantibody). These will form immune complexes with IgG that
often get deposited on the synovial membrane with subsequent joint injury.
c. It has been found that activated T-cells will also induce osteoclast cell differentiation & activation that
leads to bone resorption.
Juvenile rheumatoid arthritis (JRA):
It is a chronic idiopathic arthritis that occurs in children. Like the adult form of (RA) it is a destructive arthritis
but differs from it by the following points
1. It affects large joints
2. There is absence of RF
3. There are no rheumatoid nodules.
4. Some cases of JRA are associated with HLA-B
27
.
SjÖgren syndrome:
This autoimmune disease is characterized by dry eyes (keratoconjunctivitis sicca) & dry mouth (xerostomia)
resulting from immune-mediated destruction of the lacrimal & salivary glands. It occurs in two forms a primary
form i.e. an isolated disorder, and as a secondary form associated with other autoimmune disorder such as, RA,
SLE, polymyositis, systemic sclerosis, vasculitis and thyroiditis.
Inflammatory myopathies:
These are heterogeneous group of rare disorders characterized by immune mediated muscle injury &
inflammation. Under this heading are three disorders
1. Polymyositis
2. Dermatomyositis ,

3. Inclusion body myositis.
They may occur alone or with other autoimmune disease as systemic sclerosis.
Clinically, they present with symmetric muscle weakness initially affecting large muscles of the trunk, neck &
limbs, with difficulty in getting up from a chair. In dermatomyositis, there is associated skin rash that involves
the upper eyelids together with & periorbital edema. Histologically, there is infiltration of lymphocytes with
degeneration of muscle fibers.
Mixed connective tissue disease:
Patients present with multiple features suggestive of SLE, polymyositis, & systemic sclerosis. They also have
high titer of antibodies to ribonucleoprotein antigen. Two distinctive features of this disease
1. The kidneys are rarely involved
2. An extremely good response to corticosteroids.
Polyarteritis nodosa (PAN):
It is a systemic disease characterized by inflammatory necrosis of the wall of small-& medium-sized arteries.
The clinical effects are the result of vessel occlusion leading to small areas of infarction. The tissues most
seriously affected are the kidneys, heart, alimentary tract, liver, CNS, peripheral nerves, skeletal muscle & skin.
The cause of the disease is unknown, but it is likely to be immune-complex-mediated. There is an association
with chronic hepatitis B virus antigenemia.
AMYLOIDOSIS
Amyloid is the generic term for a variety of proteinaceous materials that are abnormally deposited in tissue
interstitium causing clinical disorders.
Morphology
The diagnosis depends on identification by light microscopy of the material in biopsy. H & E stain shows
amyloid as an amorphous, eosinophilic hyaline extracellular substance.
It also takes up certain special stains; the most widely known of these is congo red stain, which gives pink to
red color under ordinary light microscopy but characteristically green birefringence under polarizing
microscopy. (Fig. 6-10)
Electron microscopy of amyloid shows that it is composed of fibrils in a ß- pleated sheet. (Fig. 6-11)
Effects
Progressive accumulation causes pressure atrophy at adjacent cells.
Composition
Amyloid is not a single chemical entity, thee major & several minor biochemical forms could be found.
Physical nature of amyloid
95% of amyloid component is nonbranching fibrils, 7.5-10 nm in width, with characteristic crossed β-pleated
sheet conformation.
The minor component is a nonfibrillar pentagonal glycoprotein (P-component) & proteoglycans, which form the
remaining 5%.
Chemical nature of amyloid:
1. AL (amyloid light chain) derived from plasma cell & contains Ig light chain. It is encountered with
some forms of monoclonal B-cell proliferation.
2. AA (amyloid- associated): derived from serum precursor protein synthesized by the liver (serum
amyloid associated) (SAA). It is non-immunoglobulin protein and deposited in the setting of chronic
inflammatory states.
3. Aβ: found in the cerebral lesions of Alzheimer disease.
4. Transthyretin (TTR), this is a normal serum protein that binds & transports thyroxin & retinol. It is
deposited in the heart of aged patients. A mutant form of TTR is deposited in some genetic disorders and
is called familial amyloid polyneuropathies.
5. ß
2
– microglobulin, this is a component of the MHC class I molecules & a normal serum protein.
Amyloidosis may be systemic (generalized) or may be localized to a single organ. Systemic amyloidosis may
be
1. Primary which is associated with immunocyte dyscrasia
2. Secondary as a complication at chronic diseases.
Primary amyloidosis
1. AL type, usually systemic. Examples include amyloidosis which is associated with multiple myeloma (a
malignant neoplasm of plasma cells). In this neoplasm two forms of AL are synthesized
a. Abnormal amount of specific immunoglobulin producing M (myeloma) protein spike on serum
electrophoresis.
b. λ & κ light chains known as Bence Jones protein which is excreted in urine.
2. Reactive systemic amyloidosis (AA): the distribution of the amyloid deposition in this pattern is
systemic. Previously this from was considered to be secondary because it is associated with chronic
infectious diseases like TB, bronchiectasis, chronic osteomyelitis. With the use of antibiotics to control
such infections, currently it tends to be associated with chronic inflammation caused by autoimmune
states such as rheumatoid arthritis and inflammatory bowel disease.
3. Heredofamilial amyloidosis (AA)
Examples include familial Mediterranean fever, which is an autosomal recessive febrile illness of
unknown cause, associated with serosal inflammation such as the peritoneum, pleura & synovium.
4. Localized amyloidosis (AL) limited to one organ or tissue that may produce detectable nodular masses
or be evident only through microscope examination.
5. Endocrine amyloid (TTR) this form is found in medullary carcinoma of the thyroid, islet cell tumor of
pancreas and pheochromocytoma.
6. Amyloid of aging (TTR) usually occurs in the age group 70-80 years and is called senile systemic
amyloidosis. The heart is predominantly involved.
Pathogenesis:
Long standing tissue injury & inflammation cause macrophage activation & lead to elevated SAA levels
through the influence of cytokines (IL
1
, IL
6
) on liver cells. Elevation of SAA levels alone does not lead to
amyloidosis. It is believed that SAA is normally degraded to soluble end products by action of monocyte-
derived enzymes. So individuals who develop amyloidosis have an enzyme defect that results in the incomplete
breakdown of SAA, thus generating insoluble AA molecules.
Morphological effects on various organs
Kidneys become large, pale, gray and firm.
Amyloid is deposited in the glomeruli, peritubular tissue and in the wall of blood vessels. (Fig. 6-12)
Spleen becomes firm, enlarged, pale and waxy on cut section (Sago spleen).
Liver is enlarged, pale and waxy. The deposition occurs in the space of Disse and surrounding blood vessels.
Clinical correlation
S &S depend on site, amount & duration of the deposition.
Weakness, fatigue, & weight loss are the most common initial symptoms. Later the manifestations may be
present as renal disease (nephrotic syndrome) which is often the major cause of symptoms in reactive systemic
amyloidosis. Liver involvement is associated with hepatomegaly. Heart involvement may lead to
cardiomyopathy that is associated with arrhythmias.
