
Objectives ;
-Diagnosis of intestinal amoebiasis.
-- Specimens used for laboratory diagnosis.
-- Different methods used in lab. Diagnosis .
-- Symptoms of intestinal and extra-intestinal
amoebiasis.
- Differential diagnosis of amoebic and bacillary
dysentery.
-
Diagnosis of amoebiasis depend on ;
1-Clinical signs and symptoms .
2- Radiological exam.and different image methods.
3- Sigmoidoscpic or colonoscopic examination.
4- Laboratory diagnosis.

Clinical signs
Clinical signs depend on ;
-Strain of E.histolytica
-Location of infection(intestinal and extraintestinal )
-Immunity of the host
Intestinal amoebiasis
Two types of infection ;
1- Asymptomatic infection
; cyst passing carriers with
vague abdominal discomfort
.

• Symptomatic infection;
• Acute intestinal amoebiasis;
• Dysentery (mucoid bloody diarrhea), 6-8
bowel motion per day .
• localized abdominal pain,flatulens.
• Anemia and weight loss.
• Low grade fever.
Chronic amoebiasis ;
-Constipation alternating with diarrhea
-Anorexia
-Gas of abdomen
-Fatigue
Extra-intestinal amoebiasis
;
Amoebic liver abscess;
Enlarged tender liver,fever,localized abdominal pain
(RLQ),elevation of alkaline phosphatase.
Differential diagnosis include; hepatoma,pyogenic
liver abscess, and hydatid cyst.

Amoebic lung abscess
;
-Chest pain ,tachycardia ,cough ,hamoptesis .
-Differential diagnosis include ,pneumonia, pulmonary
Hydatid cyst, and lung cancer.
-
Amoebic brain abscess ;
Signs of brain tumor and brain hydatid cyst ( epilepsy ,
Headache and blindness).
-
Cutaneous amoebiasis;
Ulceration on wall of abdomen,anal skin,and genitalia
Complicated by bacteria and cause dermatitis.

2-X-ray, U.S., C.T. scan and MRI
are helpful
methods
if
there
is
obstruction
amoeboma,peritonitis,and
extraintestinal
infections .
3-Sigmoidoscopy or colonoscopy.
Diagnosis by sigmoidoscopic image should
always be supplemented by microscopic
examination of aspirated and biopsied
specimens.

4-Laboratory diagnosis:
•Direct demonstration of the parasite
in
stool specimen, liver abscess
aspirate, colonic biopsy and sputum
by
microscopic examination, cultivation,
animal inoculation .
•Indirect demonstration of the parasite
by:
A-Serological tests.
B-Antigen detection test
C-Occult blood test.
D-Blood picture.
E-Liver function test.
Direct demonstration of the parasite;
Stool examination:
Usually more than one specimen is recommended at 3 – 4 days
intervals and almost trophozoites are seen in liquid warm fresh stool,
while cysts are seen in formed and semi -formed stool.
A- General stool exam.;
•Macroscopic examination;
the stool specimen in amoebic dysentery
contains exudates ,mucus and blood.
•Microscopic examination include:
1- Direct wet smear preparation of saline and iodine solutions to look
for the
trophozoites, cysts and charcot-leyden crystals.
2- Indirect concentration method in case of light infection
.
3- Permenante stained smear.
B-Cultivation of the parasite on specific media.
C-Animal inoculation:
experimental infections of
animals to demonstrate the parasite
.
Microscopy is still the most widespread method of
diagnosis around the world .However is not as
sensitive or accurate in diagnosis as the other tests
available.

Methods of indirect demonstration of the parasite:
A- Serological tests:
to detect specific antibodies against E.
histolytica. Antibodies will be detectable within 5 – 7 days
of acute infection and may persist for years.
Serological tests are positive in 90 – 95% of patients with
extra-intestinal infection. Several serological tests are used
e.g. Indirect haemagglutination, ELISA and Indirect
fluorescent antibody test. The levels of antibodies are
much higher in individual with liver abscess
.
B-Antigen detection test
:
it gives indication that the
parasite is still present.It is more sensitive method
than microscopy and it is specific for
E.histolytica
infection
.
C-Occult blood test
usually positive in acute bloody
diarrhea.
D-Blood picture:
leucocytosis with eosinophilia is
observed in 80% of cases and mild anemia also
observed
.
E-Liver function test
:
In amoebic liver abscess, alkaline
phosphatase shows slight elevation
.
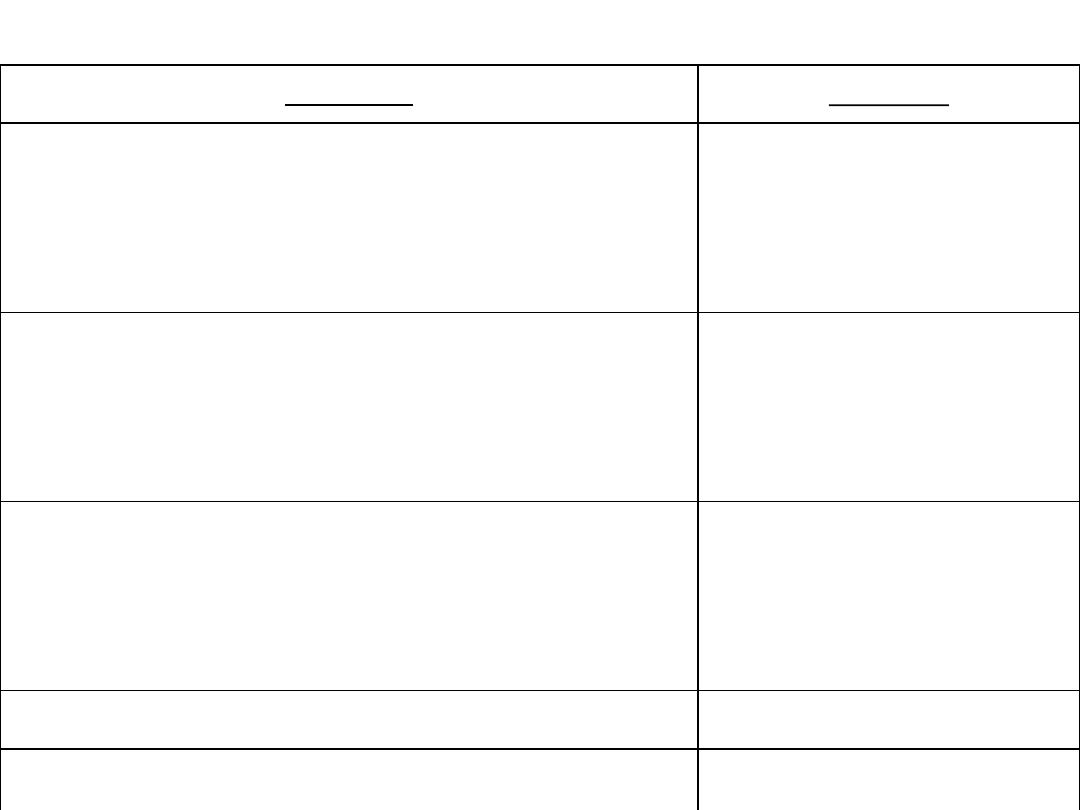
Amoebiasis
Shigellosis
-
Chronic disease may persist from 1 – 14 weeks or even
years.
-
Acute disease with short
incubation period
-
Flask – shaped ulcer involving all coats of intestine.
-
Superficial infection with
necrosis
of
mucous
membrane
-
Stool consisting of blood, mucus and fecal materials but
with few leukocyts.
-
Stool filled with cellular
exudates,
numerous
pus
cells.
-
RBCs may be agglutinated.
-
RBCs not agglutinate
-
Charcot – leyden crystals usually present.
-
Not present.
Differential diagnosis of amoebic and bacillary dysentery:
- E. histolytica troph. may
have ingested RBCs.
- No E. histolytica troph.
- Localized abdominal pain
over cecum.
- Generalized
abdominal pain.
- No fever
- Fever usually present.
- Response to antiamoebic
drug.
- Response to antibiotic.
