1
Lecture: 4
Parasitology
د. هيفاء
Continuation of lecture 3
Diagnosis of kala-azar
1- Microscopic detection of amastigotes (LD bodies) in Giemsa
stained smear of bone marrow, spleen and s.t lymph node
aspirates. Also, the specimens may be liver biopsy, buffy coat or
thick blood film.
2- Cultivation of aspirates in specific culture medium as NNN
medium → promastigotes seen.
3- Serological method (detection of specific anti-leishmanial
antibodies):
IFAT (indirect immunofluorescent antibody test)
Immunochromatography strip test (rapid test)
DAT (Direct agglutination test)
ELISA (enzyme linked immunosorbent assay)
Immunoblotting (western blotting)
4- Molecular method (PCR polymerase chain reaction) the most
sensitive and specific diagnostic method.
5- Leishmanin skin test (Montenegro test): in kala azar this test is
negative.
6- Aldehyde test : it is non specific test , indicate reversal albumin /
globulin ratio due to hypergammaglobulinaemia in VL.
Treatment
1- Sodium stiboyluconate (pentostam)
2- Pentamidine isothionate
3- Amphotericin B
2
4- Miltefosine
5- Paramomycin
Genus Trypanosoma
1-Trypanosoma cruzi
(American trypanosomiasis, Chagas’ disease)
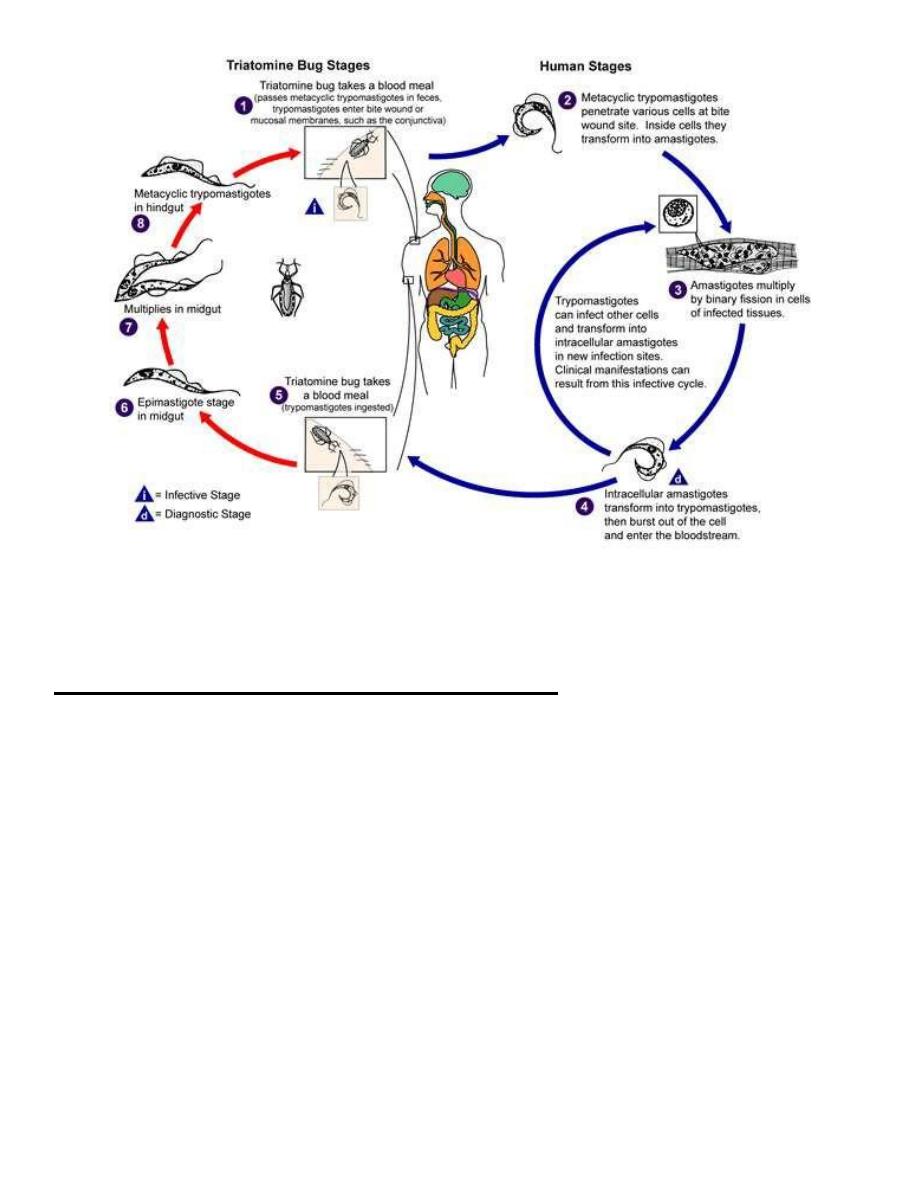
Life cycle of Trypanosoma cruzi
In vector (reduviid bug)
1- Trypomastigotes ingested in blood meal of bug from infected
vertebrate (man).
2- Trypomastigotes transform to epimastigotes in midgut.
3- Epimastigotes multiply by binary fission in midgut and migrate to
hindgut.
4- Epimastigotes transform to trypomastigotes in hindgut.
5- Slender , infective (metacyclic trypomastigotes) formed in rectum
(posterior station).
In vertebrate (man)
6- Transmission occurs by penetration of trypomastigotes in bug
feces through skin abrasions or mucosa of vertebrate (man).
7- Trypomastigotes do not multiply, they invade tissue cells of
vertebrate.
8- Trypomastigotes transform within tissue cells to amastigotes,
which multiply forming pseudocyst.
9- Amastigotes in pseudocyst transform to epimastigotes and
trypomastigotes, then pseudocyst ruptures to release
trypomastigotes which either re-enter other cells or enter the
blood stream and ingested by the bug.
*Vector: Reduviid (kissing)bug of genera Triatoma and Panstrongylus.
*Final host: Man, dog, Cat and rodent.
3
life cycle of Trypanosoma cruzi
Posterior station transmission in T. cruzi
After multiplication in the midgut of the insect vector, the parasites
pass posteriorly and produce the infective forms (metacyclic
trypomastigotes) in the rectum and the introduction of infective
forms in bug feces to new hosts via skin abrasions or mucous
membrane (especially conjunctiva).
Life cycle in bug need about 8-10 days to excrete infective metacyclic
trypomastigotes in feces.
The amastigote forms are intracellular , within the cells of virtually
every organ or tissue but cells of RES, cardiac, skeletal, smooth
muscles and neuroglia cells are preferentially parasitized, while
trypomastigotes are extracellular (present in peripheral blood).
At night the bugs emerge from the cracks in the walls and painlessly
4
extract a blood meal from the sleeping people. These bugs defecate
during or soon after biting. The bite wound is readily contaminated.
The sleeping victim may also inadvertently scratch or rub the affected
area, thereby helping the entry of the parasite into the body.
Modes of transmission
1- Bite of reduviid bug (commonest mode).
2- Blood transfusion in endemic areas.
3- Congenital transmission.
4- Through contaminated syringes and needles.
The clinical aspect
American trypanosomiasis (Chagas’ disease) is caused by
trypanosoma cruzi.
This disease is distributed in central and south America.
The disease is seen in most commonly and in its most severe form in
children under 5 years, in whom symptoms of CNS involvement may
by prominent, in older children and adults the disease is usually
occurs in a milder subacute or chronic form which generally follows
an acute attack.
Diagnosis of Chagas’ disease
1- Microscopic detection of trypomastigotes in peripheral blood:
a) Wet mount preparation: trypomastigotes are only faintly
visible, but their rapid progressive snake like motion among
erythrocytes make their presence apparent.
b) Fixed preparation by Giemsa stained smear (thick or thin
blood smear): the parasites are typically C or U shaped. In
young children the parasites may be detected in blood with
ease , particularly at acute stage. In older children and adults,
the parasites are frequently very difficult to find.
c) Examination of concentrated blood smear.
2- Culture : such as on NNN medium.
5
3- Xenodiagnosis: at least 6 clean uninfected laboratory bred
reduviid bug are allowed to feed on the suspected patient and
two weeks later the hindgut of the bugs is examined for
epimastigotes.
4- Biopsy examination: lymph node or skeletal muscle biopsy is
examined for amastigotes.
5- Serological diagnosis: IFAT , RIA (radioimmunoassay) , ELISA.
6- PCR (polymerase chain reaction).
7- Animal inoculation.
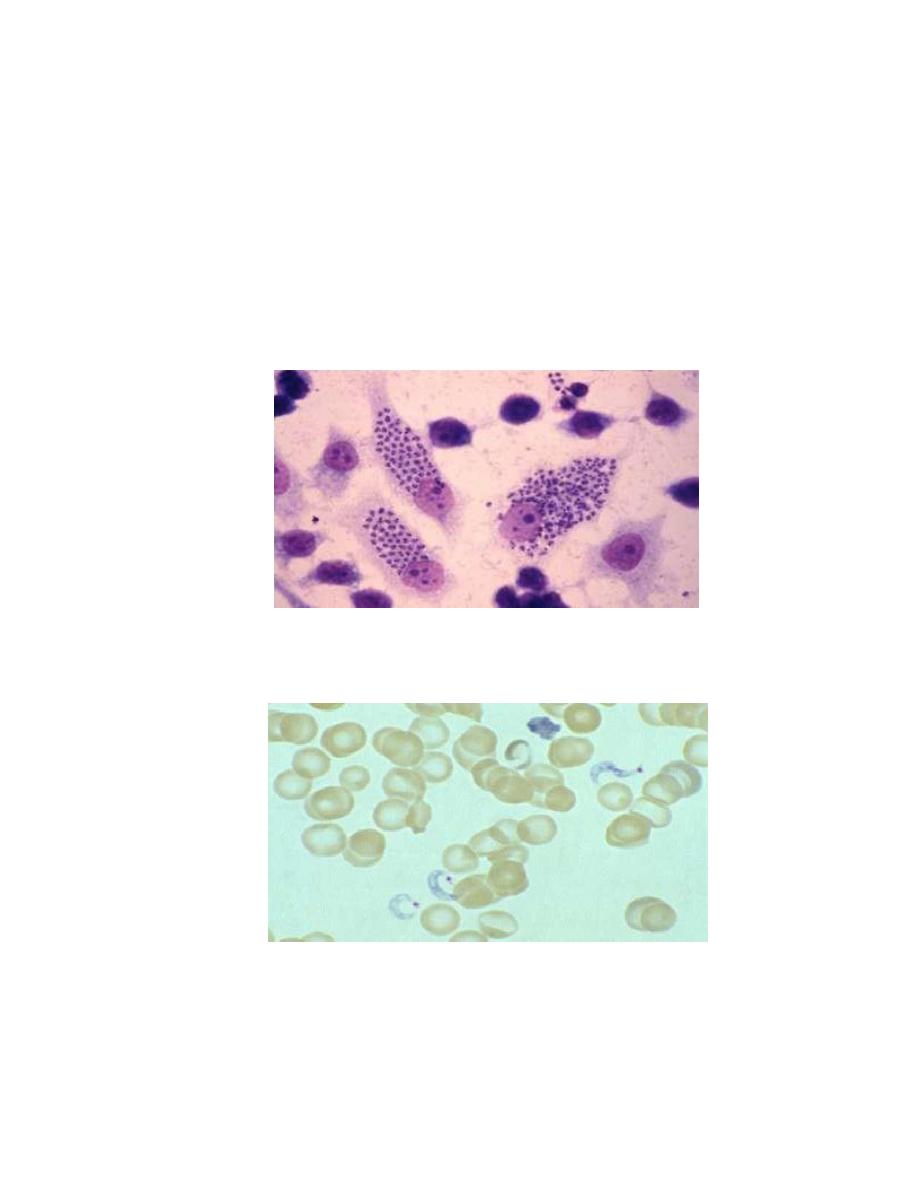
Amastigotes from biopsy of cardiac muscle
C – shape trypomastigotes in blood smear
6
2-Trypanosoma brucie
(African Trypanosomiasis,Sleeping sickness)
Trypanosoma brucie
T. gambiense
T. rhodesiense
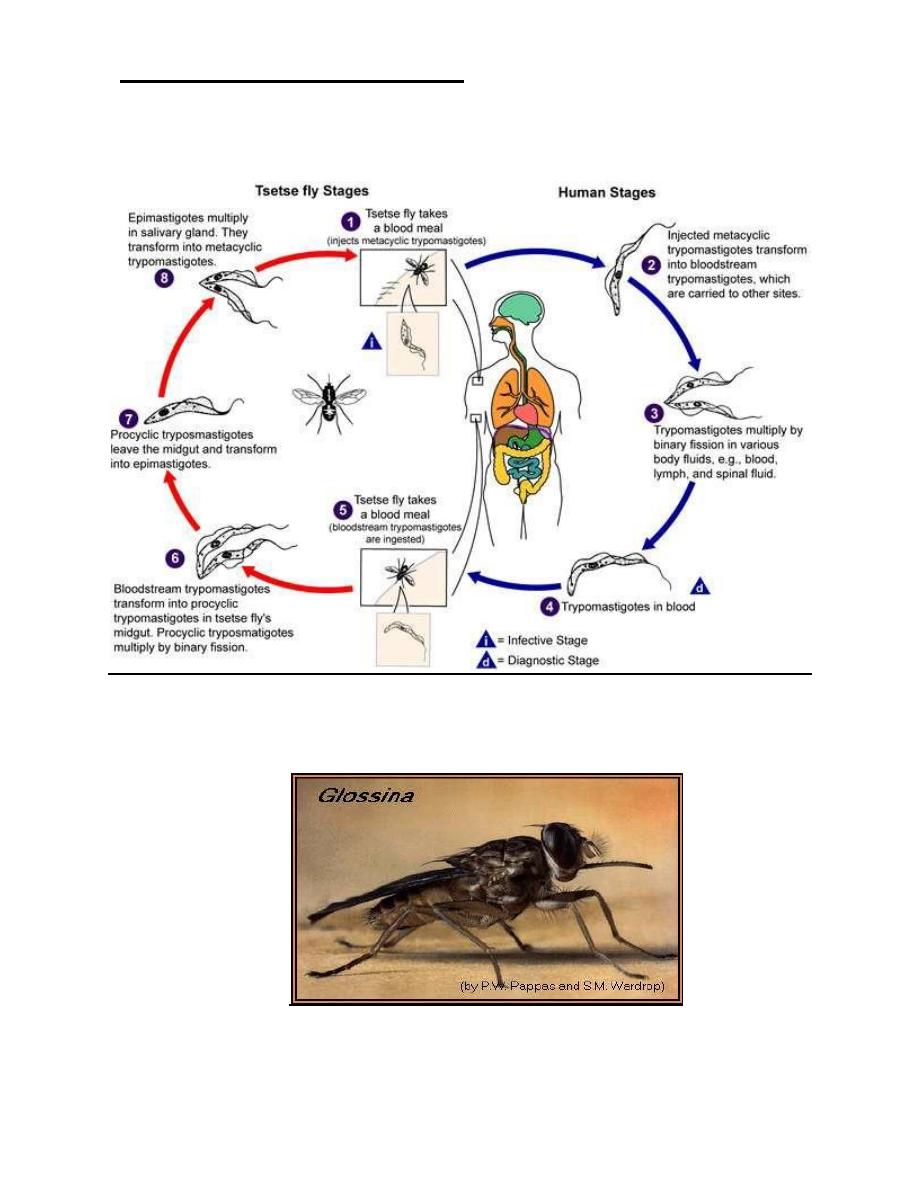
Life cycle of T. brucie
A- In vector (Tsetse fly)
1-Short stumby and long trypomastigotes ingested by tsetse fly
during blood meal by proboscis and go to midgut of the fly.
2-The trypomastigotes transform to procyclic trypomastigote
and multiply in midgut.
3-Then procyclic trypomastigotes migrate forward to the
oesophagus → proboscis → to reach the salivary gland.
4-In fly’s salivary gland, procyclic trypomastigotes transform into
epimastigotes and multiply.
5-Epimastigotes in salivary gland transform to infective
metacyclic trypomastigotes.
B- In vertebrate (man).
6-The infective metacyclic trypomastigotes pass from fly’s
salivary ducts and injected into the bite wound of the vertebrate
(man) at the time of blood meal and transform to blood
trypomastigotes.
7-Trypomastigotes multiply inside bite asexually for 1-2 days
before entering the blood circulation by lymphatics.
8-Trypomastigotes multiply extracellulary in blood at the site of
the bite and/or in other tissue fluids (lymph and CSF) and the
cycle repeated.
*Final host: man, antelope and other domestic and wild cattle.
7
*Vector (intermediate host): Tsetse fly (genus Glossinia),
Glossinia morsitans for T. rhodesiense and Glossinia pallipidis for T.
gambiense.
Life cycle of T. Brucie (T. gambiense and T. Rhodesiense)
Tsetse fly, vector of sleeping sickness
8
Antigenic variation of T. brucie
Parasitaemia in African trypanosomal infection persists inspite of
strong antibody response because the parasite shows antigenic
variation every week to 10 days. This phenomena occurs because
the parasites shed thier outer varient surface glycoprotien (VSG)
coat and replace it with another one. Each VSG is immunogenic
but antigenically different from the previous sheded VSG → Thus
the parasite escapes the host immune response.
Diagnosis of African trypanosomiasis
1-Microscopic detection of trypomastigotes in:
a-Trypanosomal chancre. b-Peripheral blood. c-Bone marrow. d-
Lymph node aspiration. e-CSF, by:
1)Wet preparation: direct microscopical examination of
unstained film.
2)Fixed preparation by Giemsa stained smear.
3)Concentrated method.
2-Serological diagnosis:
-IFAT (indirect fluorescent antibody test).
-IHT (indirect haemoagglutination test).
-ELISA.
-CFT (complement fixation test).
-Card indirect agglutination test.
3-Aldehyde test: positive due to reverse albumin/globulin ratio.
4-Serum and spinal fluid IgM measurement: are of diagnostic
value, because in many cases the total serum IgM exceeds eight
(8) times the normal amount.
5-Animal inoculation.

9
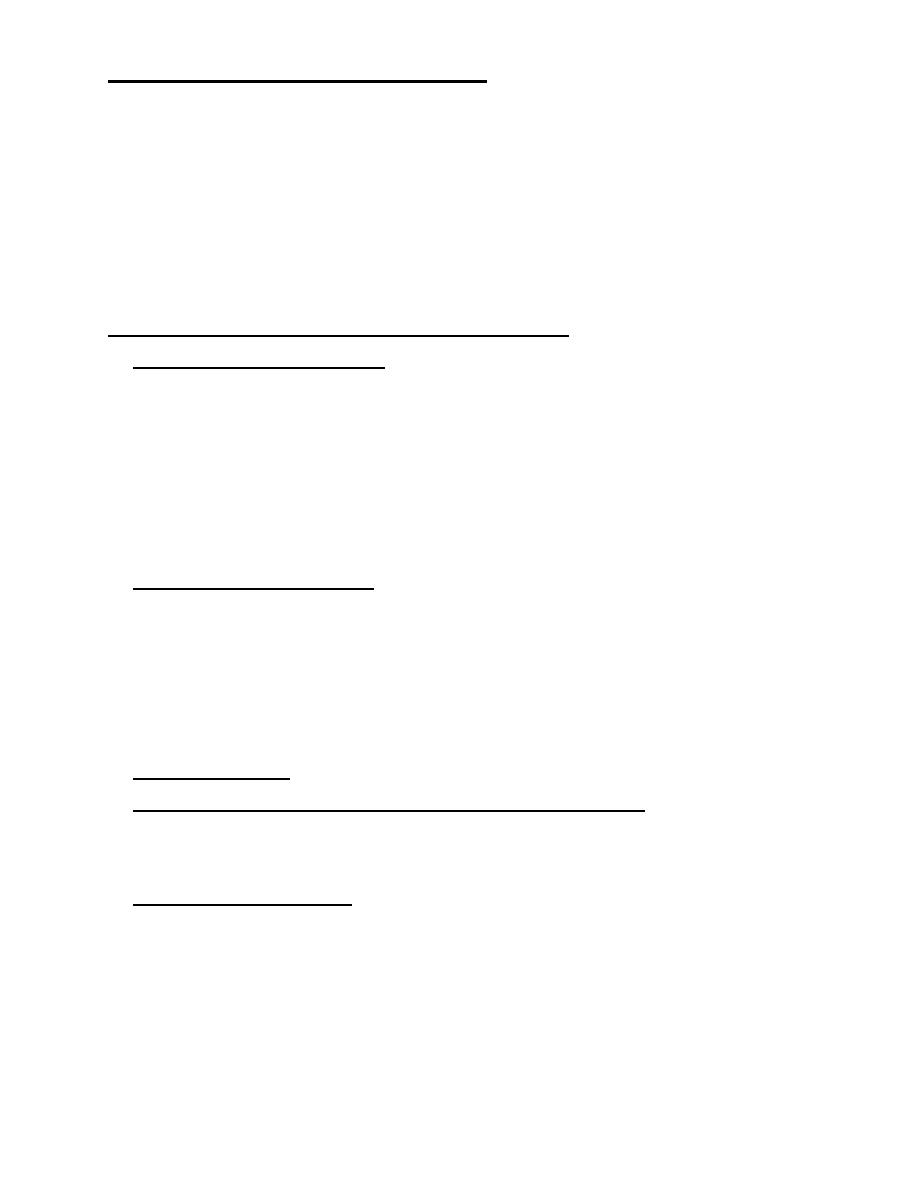
Trypanosoma gambiense or rhodesiense trypomastigote forms in
blood smear
