Sunday 19 / 4 / 2015
©Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
"Pharmacology
مكتب اشور لالستنساخ
ANTI-CANCER DRUGS
Lecture 10
Total lectures NO. 55
Dr. Samer Matloub

Anticancer Drugs
Page 2
Include:
1) Cytotoxic drugs.
2) Isotopes:
which emit β-irradiation that destroy cancer cells, e.g. I
131
, P
32
, Au
193
3) Hormones:
A- Steroids: prednisolone used in leukemia and lymphoma, it :
Prevents bleeding due to thrombocytopenia.
Prevents hemolysis due to auto Ab.
↓ICP
↓hypercalcemia due to bone metastasis.
B-Sex hormones:
Estrogen : CA breast postmenopausally,CA prostate
Androgen: CA breast premenopausally.
Progesterone: endometrial CA.
Anti-hormones: e.g. tamoxifen.
4) Immunotherapy:
A. Agents that restore, augment, or modify host immunologic mechanisms,
e.g. BCG, interferon α, levamisole (anti-helminthic)
B. Cells or cellular products that have a direct Cytotoxic or cytotactic effects
e.g. T-lymphocytes, bone marrow transplants, IL
2
, monoclonal Ab., anti-
idiotypic Ab.
C. Agents that modify or alter the metastatic potential or affects the initiation
or maintenance of neoplastic transformation e.g. retenoids.
Principles of cancer chemotherapy:
Objectives (goals) of cancer treatment may be:
a) Cure, if not attainable then the goal is
b) Palliation (alleviation of symptoms) prolongation of life but recurrence is an
even present possibility.

Anticancer Drugs
Page 3
The treatment program typically includes a combination of surgery and/or radiation
therapy then followed by chemotherapy and in some cases the use of biological
response modifiers.
Indications for treatment:
A. Indicated when the cancer is disseminated and not amenable to surgery.
B. Used as supplement to surgery and radiation to attack micrometastasis (this is
known as adjuvant chemotherapy) e.g. Ca breast.
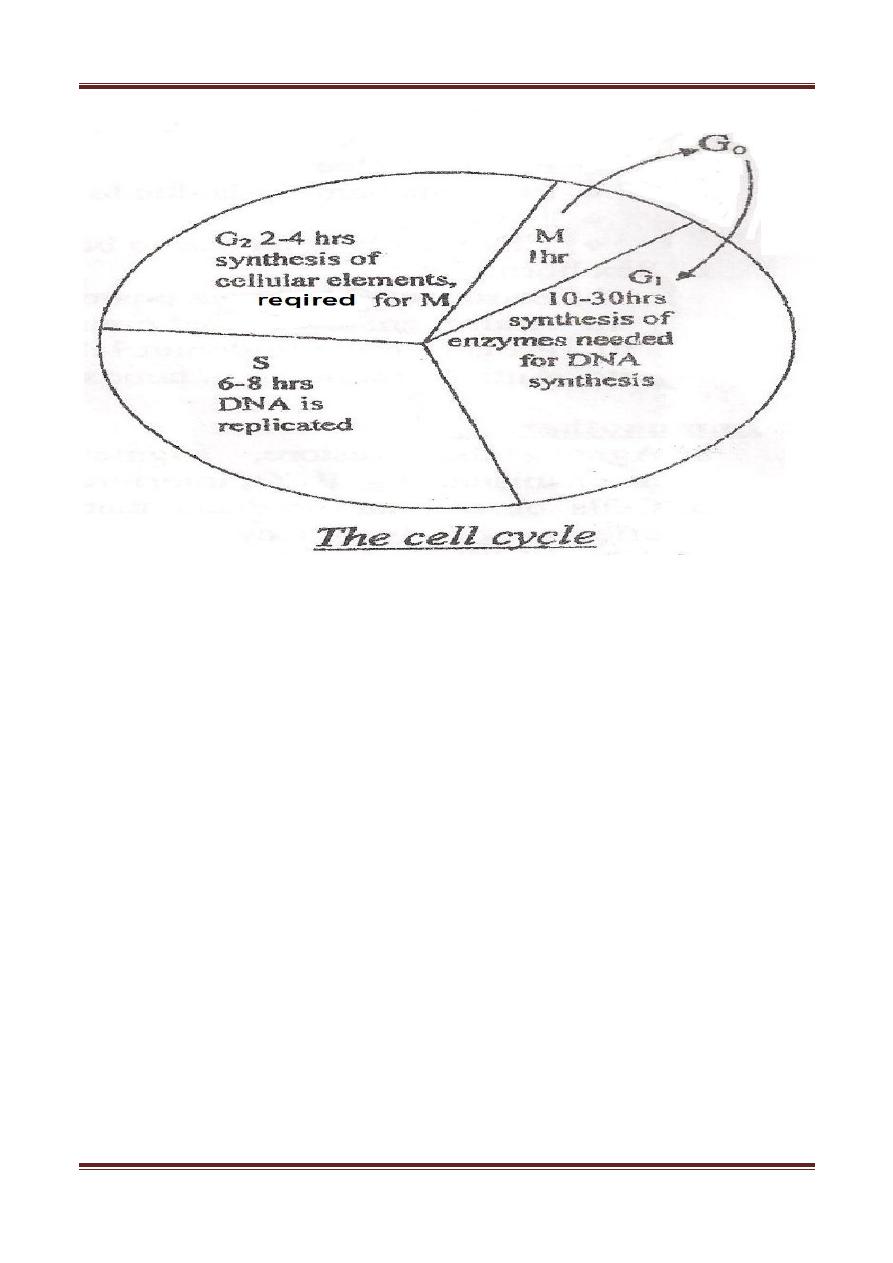
Tumor susceptibility and the growth cycle:
The fraction of the tumor cells that are in the growth cycle (replicative cycle)
influences their susceptibility to chemotherapeutic agents.
Rapidly dividing cells are generally more sensitive to anti-cancer drugs where
as non-proliferating cells (G
0
-phase) usually survive the toxic effects of these agents.
Both normal and tumor cells go through a growth cycle. However, they differ in the
number of cells that are in various stages of the cycle. In cancer cells there is faulty
cell contact signaling processes because of transduction defects (i.e. the normal
feedback mechanism that mediate cell growth are defective).
Anticancer Drugs
Page 4
Cytotoxic drugs
Act against all cells that are multiplying: bone marrow, mucosal surfaces(gut),
hair follicles, RES, germ cells are all dividing rapidly thus they are targets for
cytotoxics (this is shown as side effects of these drugs).
Cell cycle specificity of drugs:
Cycle non-specific: these kill cells whether resting or actively cycling although
they are more toxic to cycling cells, e.g. alkylating agents, anthracyclines,
antitumor ABCs., cisplatin. These are useful in low growth fraction tumors e.g.
solid tumors.
Cycle specific: these kill only cells that are actively cycling often because their
site of action is confined to one part of the cell cycle, e.g. anti-metabolites,
Bleomycin, taxanes, vinca alkaloids, etoposide.
Anticancer Drugs
Page 5
The growth rate of most tumors is initially rapid but it decreases as the tumor size
increases. Thus, reducing the tumor burden through surgery or radiation promotes
recruitment of the remaining cells into active proliferation and ↑their
susceptibility to cytotoxics.
Log kill:
(cell destruction)
Follows a first order kinetics i.e. a given dose of a drug kills a constant fraction
of cells (not a constant number) regardless of the number of the cells present. The
term log kill is used for such phenomenon. Therefore, when there are many cells
(late presentation, macroscopic disease) it is necessary to use several drugs.
E.g. 10
12
tumor cells
cytotoxic drug
99.99% eradication (remaining 0.01%)
Remaining tumor cells= 10
8
i.e. 8 log of tumor cells.
Pharmacologic sanctuaries:
Leukemia or other tumor cells find sanctuary in tissues e.g. CNS in which most
cytotoxics cannot enter (these sites require irradiation or intrathecal
administration of drugs to eliminate leukemia cells at that site). Similarly drugs
may not enter certain areas of solid tumors.
Treatment protocols:
Combination chemotherapy is more effective than single drug treatment.
Cytotoxics with quantitavely different toxicities and different mechanisms of
action are usually combined at full doses, this result in a higher response rates and
decreases the chance of resistance. When using drugs with similar dose limiting
toxicities the dose of each must be reduced. Many protocols each is applicable to a
particular neoplastic state.
Common protocols:
لإلطالع
POMP for ALL
6MP, oncovin, MTX, prednisolone.
MOPP for Hodgkin's Mustine, oncovin, procarbazine, prednisolone.
CHOP for lymphoma Cyclophosphamide, adriamycin, oncovin, prednisolone.
CART for AML
Ara-c, asparginase, duanrubicin, 6-thio-guanin.

Anticancer Drugs
Page 6
Other protocols include COP, CMF, ABVD, FAC, FEC, PCV, and VAD.
Therapy is scheduled intermittently (cycles) to allow recovery of the normal
tissues e.g. bone marrow.
Problems associated with chemotherapy:
1. Resistance:
a) Inherent resistance: some neoplastic cells are inherently resistant, e.g.
melanoma cells.
b) Acquired resistance: which develops after prolonged administration of
low drug doses (this can be minimized by using combination drug
therapy).
c) Multidrug resistance: this is now a major problem, it is due to activation
of ATP dependent membrane efflux pump acting via a protein called P-
glycoprotein (it pumps the drug out of the cell), cytotoxics differ in their
capacity to stimulate P-glycoprotein eg.anthracyclines , vinca alkaloids
and some e.g. cisplatin do not induce this type of resistance.
d) Other causes of drug resistance:
Formation of trapping agents (gluthione) e.g. βleomycin, anthracyclines
Abcs.
↑DNA repair e.g. alkylating agents.
Changes in target enzymes sensitivity e.g. methotrexate.
↓activation of prodrugs e.g. purine & pyrimidine analogs.
2. Toxicity: (adverse effects)
a. Bone marrow and RES : pancytopenia and immune suppression (humoral
and cellular immunity) leading to opportunistic microbial infections. BM
depression is the most important limiting factor in using these drugs.
b. GIT: damage to rapidly dividing gut epithelium and other mucosal
surfaces → mucositis which leads to stomatitis, mouth ulcers, vomiting
and diarrhea.
c. Skin: hair follicles →alopecia which recovers after 2-6 months of stopping
therapy. Delayed wound healing and local toxicity if extravasation
occurs.
d. Gonads: (germ cells and reproduction) sterility, mutagenesis,
teratogenisity, and abortion.
Anticancer Drugs
Page 7
e. Hyperuricemia: + gouty nephropathy due to release of nucleoproteins
from destruction of large number of tumor cells →↑uric acid, treated by
alkalinization of urine, fluids, and allopurinol.
f. Oncogenic effects: (second cancers) e.g. non-lymphocytic leukemia or
lymphoma after many years of treatment with alkylating agents.
g. Specific organ toxicity: ,
Hepatic toxicity →6-MP.
Neurotoxicity →vincristine.
Cardiac toxicity →daunarubicin.doxarubicin
Lung toxicity →busulphan.
Bladder toxicity →cyclophosphamide.
Vomiting, alopecia, and stomatitis occur more or less with all neoplastic
agents.
The duration of the adverse effects may be transient, e.g. alopecia, stomatitis,
vomiting or irreversible, e.g. pulmonary, cardiac and bladder toxicity.
Contraindications for the use of cytotoxics:
1) Very advanced disease and debilitated patient,
2) Active infection.
3) Pre-existing bone marrow depression.
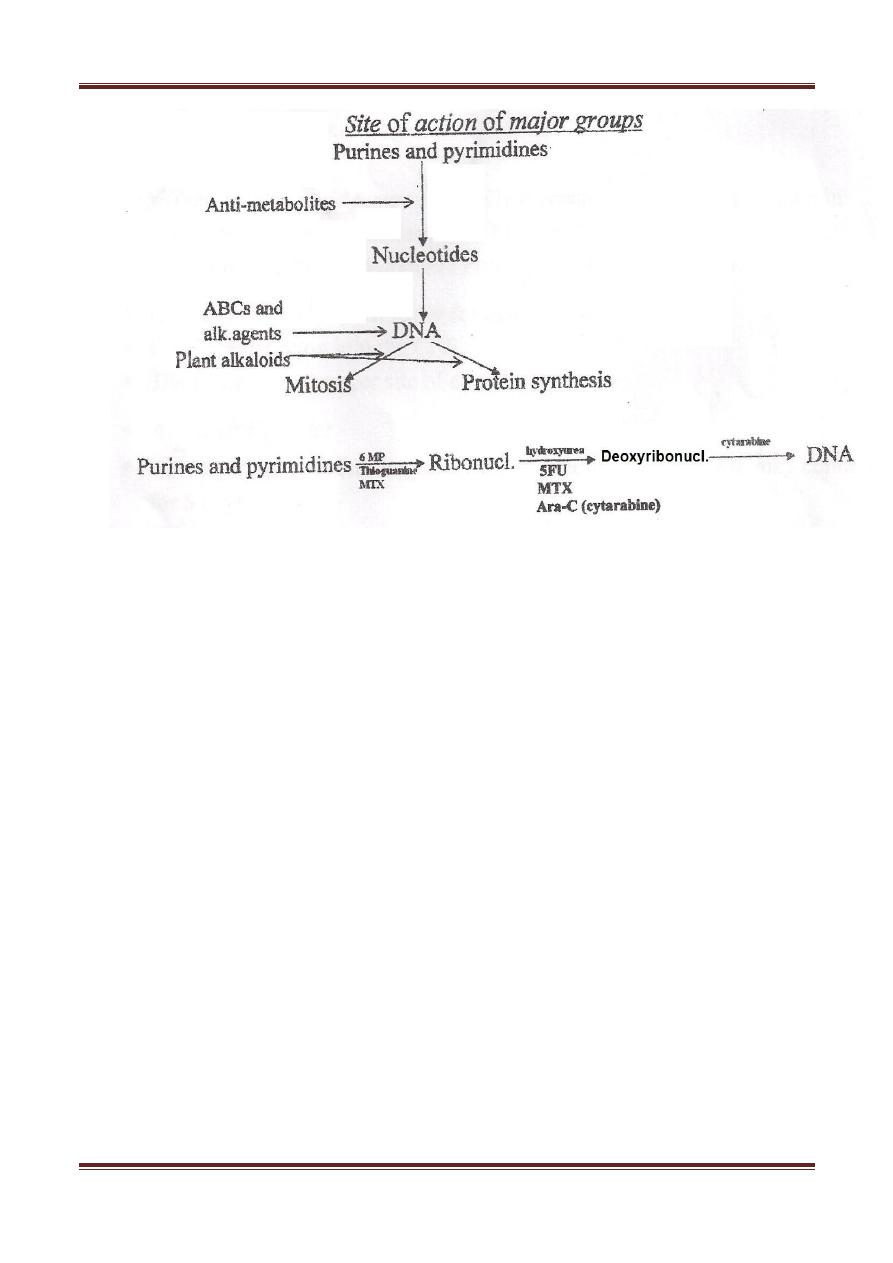
Classes of cytotoxic agents:
a. Alkylating agents.
b. Spindle poisons( microtubular inhibitors)(plant alkaloids)
c. Antibiotics.
d. Anti-metabolites.
e. Miscellaneous.
Anticancer Drugs
Page 8
Alkylating agents :( cycle non-specific)
Mechanism of action:
they react strongly with nucleophilic substances and
form covalent linkage. Their toxic effects are due to free radical formation and
alkylation of the components of DNA, RNA, and cellular proteins. These reactions
have profound effects on DNA replication and transcription and may cause
mutagenesis and carcinogenesis.
Nitrogen Mustards and ethylenimine: act by transferring alkyl groups to DNA in N-
7 position of guanine during cell division leading either to DNA strand breakage or
cross linking of the 2 strands, so that the normal synthesis is prevented.
Platinum analogs: also complex with DNA at the N-7 guanine position forming
intrastrand cross links, they also in addition bind to nuclear and cytoplasmic proteins
behaving therefore as bifunctional alkylating agent.
Uses:
Treatment of wide varity of lymphatic and solid tumors in combination with
other agents.
Adverse effects:
Particularly nausea and vomiting, alopecia, BM suppression(delayed with carmustine
and lomustine)

Anticancer Drugs
Page 9
Hemorrhagic cystitis with cyclophamide and ifosamide.
Pulmonary fibriosis with busulphan
Male infertility and premature menopause may occur
Individual members:
Meclorethamine (Mustine):
is a bifunctional agent (can bind and react at 2 separate sites) it forms a reactive
intermediate that alkylates the N
7
position and guanine leading to DNA cross linkage
and/or depurination that facilitate DNA strand breakage.
It is used primarly for Hodgkin's disease as a part of the MOPP regimen and also in
solid tumors. It is powerful blistering agent.
It is given I.V. only, it is very unstable in solution.
Cyclophosphamide & Ifosfamide:
Very closely related mustard agents they share most of the same toxicities. They are
unique in that:
1- They can be taken orally.
2- They have to be transformed to hydroxylated intermediates by cytochrome
P450 to become cytotoxic and hydroxylated intermediate under go breakdown
to form the active compounds phosphoramide mustard and acrolein.
The reaction of phosphoramide mustard with the DNA is considered the cytotoxic
step.
Uses:
1- Neoplastic conditions, part of regimens of wide variety of neoplasms:
Hodgkin's disease, lymphoma, CLL, myloma, breast and lung CA.
2- Non-neoplastic nephritic syndrome and intractable rheumatoid arthritis.

Anticancer Drugs
Page 10
Adverse effects:
GIT, alopecia, BM suppression, infertility, hemorrhagic cystitis, fibrosis of the
bladder due to acrolein toxicity in case of cyclophosphamide, treated by good
hydration + MESNA (IV) (sodium 2-mercaptoethane sulfonate) which inactivates
the toxic compound. These drugs are preferentially given orally. Minimal amount
of the parent drug is excreted in urine or feces.
Nitroso Ureas:
Carmustine and Lomustine are closely related.
Streptozocin is especially toxic to the Beta cells of pancreas, useful in
insulinoma, it causes diabetes and reversible renal damage.
Nitroso Ureas are useful primarily in treatment of brain tumors because of
their ability to pass to the CNS.
Carmustine is given IV.
Lomustine is given orally (it is metabolized to the active product).
The kidney is the major excretory route.
Cisplatin & carboplatin
Cisplatin: severely toxic, carboplatin less toxic.
therapeutic effectiveness is similar.
Cisplatin has synergestic cytotoxicity with radiation and other chemotherapeutic
agents.
Uses:
a- Treatment of solid tumors especially metastatic testicular carcinoma in
combination with vinblastine and bleomycin.
b- Also is used in the treatment of ovarian and bladder cancer.
Given I.V. ,also intraperitonially for ovarian CA.
Poorly penetrate into CNS.
The kidney is the major site of excretion.
Adverse effects:

Anticancer Drugs
Page 11
Severe persistant vomiting after one hour of administration, and may continue for 5
days.
Major toxicity:
nephrotoxicity& ototoxicity, also it may cause neurotoxicty but
cause mild mylosuppression.
Carboplatin
:
cause little nausea and vomiting it is not nephrotoxic or neurotoxic.
Major toxicity:
mylosuppression.
Spindle Poisons: (Plant alkaloids)(Microtubular inhibitors)
The mitotic spindle (consists of Chromatin and a system of Microtubules composed
of protein tubulin) is essential for internal movements occurring in the cytoplasm of
all eukaryotes and for equal positioning of DNA into the daughter cells formed when
the cell divides.
Plant alkaloids cause cytotoxicity by disrupting this process by affecting the
equilibrium between the polymerized and de-polymerized forms of the microtubules
(block Mitosis).
1. Vinca alkaloids: Vincristine, Vinblastine, Navelbine.
2. Taxoids:paclitaxel (taxol),docetaxel`
3. Podophyllotoxins: Etoposide (VP-16), Teniposide (VM-26)
4. Comptothecins: Topotecan, Irinotecan.
Adverse Effects:
They in particular cause Bone Marrow depression, peripheral neuropathy
(Vincristine) and Alopecia.
Individual Members:

Anticancer Drugs
Page 12
Vincristine and Vinblastine:
They're cycle-specific, M phase specific, block mitosis in metaphase (M phase) by
blocking the ability of Tubulin to polymerize to form microtubules (prevent Tubulin
assembly)
Vincristine is administrated as the (O) in MOPP for Hodgkin's.
Vinblastine is combined with Bleomycin and Cisplatin for the treatment of Metastatic
testicular CA, administrated IV, metabolized in the Liver, excreted in bile and feces, it
causes Hyperurecemia.
Adverse Effects:
GIT, Alopecia, Phelbitis, Cellulitis.
Unique toxicity: Vinblastine
Bone marrow depression.
Vincristine
Neurotoxicity.
Paclitaxel (Taxol):
Binds reversibly to Tubulin but unlike Vince Alkaloids, It promotes polymerization and
stabilization of the Polymer rather than dis-assembly, the cell therefore remains
frozen in Metaphase
death of the cell (it prevents microtubular dis-assembly)
Uses:
1. Advanced Ovarian Cancer.

Anticancer Drugs
Page 13
2. Metastatic Breast Cancer.
3. Small –cell lung CA.
4. CA of head and Neck.
It's given IV over 3-4 hours.
It's metabolized by the liver
excreted in Bile.
Adverse Effects:
1. Severe Hyper-sensitivity reactions.
2. Neutropenia (Dose limiting toxicity)
3. Alopecia, Neuropathy and Bradycardia.
Etopside (VP-16) (Late S and early G2 phase)
It causes metaphase arrest. Their major target is topo-isomerase II (binding of the
drug to the enzyme-DNA complex leading to persistent cleavable complex). The result
will be irreversible double-strands breaks.
USES:
1. Oat-cell CA of the lung.
2. Ref. testicular CA.
It's given IV or orally
Low penetration to the CNS.
High-binding to Plasma proteins.
Metabolized to Sulphate and Glucoronide.
It's excreted in Urine.
Leucopenia is dose-limiting toxicity, others: nausea and vomiting, alopecia and
Anaphylactic reaction.
VM-26: It's similar to VP-16 but its use is limited to Acute Lymphoblastic Leukemia
(ALL)

Anticancer Drugs
Page 14
Camptothecins:
these drugs inhibit topoisomerase I (responsible for cutting and
religating single DNA strand) resulting in DNA damage.
Topotecan:
used for 1- Advanced ovarian CA.
2- Small cell lung cancer (2
nd
line)
The drug is excreted by the kidney.
Irinotecan:
converted in the liver to (SN-38)metahabite which inhibit the
topoisomerase I.
Drug excreted in bile & feces.
It is used in:
1) 2
nd
line monotherapy for metastatic colorectal CA who have failed 5-Fu.
2) 1
st
line drug when used in combination with 5-Fu and leucovorin.
Main toxicity of comptothecin is bone marrow suppression and diarrhea.
Diarrhea is either: 1- early after 24hrs →stopped by atropine like drugs.
2- late after 3-10 days
Done by
Ali Kareem
