Sunday 15 / 2 / 2015
©Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
مكتب اشور لالستنساخ
ANTI-DEPRESSANT AGENTS
Lecture 4
Total lectures NO. 34
Dr. Naseer Al-Harchan
2
Antidepressant Agents
Introduction
Depression is one of the common psychiatric disorders. It has been
found that at every time 5-6% of population is depressed.
Types of depression
1. Reactive depression. (Exogenous).
2. Major depression. (Endogenous).
3. Bipolar depression. (Manic – depressive).
Antidepressants
1. Tricyclic anti-depressants (TCAs).
Imipramine, desipramine, nortriptyline, protryptyline, mytriptiline,
doxepin.
2. Atypical anti-depressants.
New TCAs, amoxapine, bupropion,maprotiline, nomifensine, mianserin.
3. Selective serotonin reuptake inhibitors (SSRIs).
Fluoxetine, sertraline, paroxetine, trazodone.
4. Monoamine oxidase inhibitors (MAOIs).
Isocarboxacid, phenelzine, tranylcypromine.

3
Tricyclic antidepressants(TCA)
• TCA are structurally similar to the phenothiazine antipsychotics
and share many of their pharmacological actions.
• Include imipramine, amitriptyline, desimipramine, nortriptyline,
and protriptyline.
1.Mechanism of Action of TCA
• TCA potentiate the actions of biogenic amines, presumably by
inhibiting reuptake of the amines in the presynaptic neurons.
• TCA have both antihistamine H
1
and alpha-adrenergic blocking
actions.
• TCA possess antimuscarinic action and block the reuptake of
serotonin.
Pharmacokinetics of TCA
• TCA are well absorbed orally. They are lipid soluble and penetrate
all tissues and have long half-lives. They are metabolized by liver
enzymes and many of the metabolites are pharmacologically
active. Excretion is via the kidney.
Pharmacologic Effects of TCA
• 1- Amine uptake blockade: TCA block NE uptake transporters in
the CNS and peripherally in the A.N.S. This increases sympathetic
activity.
• 2- Sedation: is a common effect with TCA. Some may have CNS
stimulant effects.
• 3- Antimuscarinic effects: Atropine-like actions.
4
• 4- C.V. effects: postural hypotension due to alpha-blockade,
arrhythmia due to depression of cardiac conduction.
• 5- Seizures: TCA lowers the convulsive threshold with overdoses
Clinical Uses of TCA
• Major depressive disorders: TCA are considered the treatment of
choice for major depression. The various TCA are equivalent at
appropriate doses with regards to their overall efficacy.
• Nocturnal enuresis: Bed wetting in children with imipramine.

5
• Obsessive-compulsive neurosis: accompanied by depression, and
phobic-anxiety syndromes, chronic pain, and neuralgia may
respond to TCA.
Adverse Effects of TCA
• Resemble those of the phenothiazines.
• 1- Antimuscarinic effects. Occur both centrally and peripherally.
Patients with prostatic hypertrophy and glaucoma are cautioned.
Tolerance develop to this effect.
• 2- Postural hypotension and cardiac arrhythmias
• 3- Manic excitement and delirium occur in patients with bipolar
depression.
• 4- The elderly may suffer from dizziness and muscle tremor.
• 5- Seizures, ventricular arrhythmias and death can result from
overdoses.
• 6- combination of MAO-inhibitors and TCA should be avoided.
Precautions with TCA use
• TCA should be used with caution in manic-depressive patients,
since they may unmask manic behavior
• TCA have narrow therapeutic index. Depressed patients with
suicidal intents should be given limited quantities of these drugs.
6
Heterocyclics
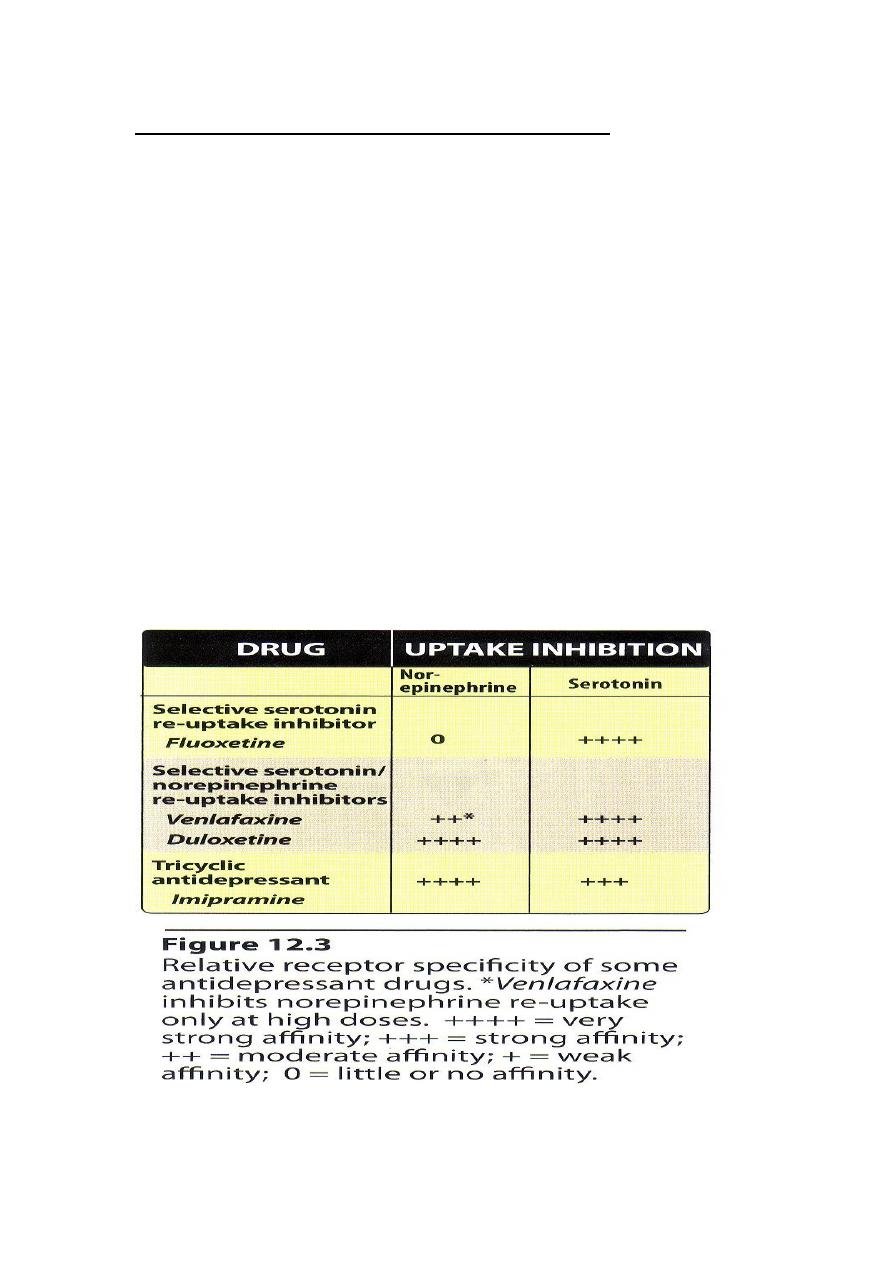
• Venlafaxine:
• Inhibits serotonin and at higher doses inhibits NE and dopamine
reuptake. Has fewer adverse effects than TCA.
• Duloxetine:
• Not indicated in patients with end stage renal diseases. Can cause
nausea, vomiting, diarrhea, dizziness and somnolence, sweating
and sexual dysfunctions. It can be used for depression
accompanied by neuropathic pain.
Atypical Antidepressants
• Have actions at several sites. Include Bupropion, Mirtazapine
nafazodone and Trazodone. They are not better than TCA or SSRIs
but their adverse effects are different.
1. Bupropion
• Mechanism of action unknown. It decreases the craving for
nicotine in tobacco abusers. May produce dry mouth, sweating,
tremor, and seizures
2. Mirtazapine
• It can block 5-HT
2
and α
2
receptors. It is sedative due to its
antihistaminic activity, but has no atropine-like actions. It does not
interfer with sexual activity. Increased appetite and weight gain
can occur.
3. Nefazodone and 4.Trazodone
• Weak inhibitors of 5-HT reuptake. They block 5-HT
1
presynaptic
autoreceptors, and so increase 5-HT release. They are sedating
due to antihistamine effect. Trazodone causes priapism.
7
Selective Serotonin Re-uptake Inhibitors (SSRIs)
• specifically inhibit serotonin re-uptake having 300- to 3000-fold
greater selectivity for 5-HT transporter as compared to NE
transporter. SSRIs have little ability to block DA transporter. In
addition they have little blocking activity at muscarinic, α-
adrenergic, and histamine H
1
receptors. Therefore common
adverse effects associated with TCA such as orthostatic
hypotension, sedation, dry mouth and blurred vision, are not seen
with SSRIs
• SSRIs because of their relative safety and fewer AR have largely
replaced TCA and MAOI as the drug of choice in treating
depression.
• They include fluoxetine, citalopram, escitalopram, fluvoxamine,
paroxetine and sertraline

8
Actions of SSRIs
• Inhibit reuptake of 5-HT leading to increased concentration of
serotonin in the synaptic cleft and increased postsynaptic
neuronal activity.
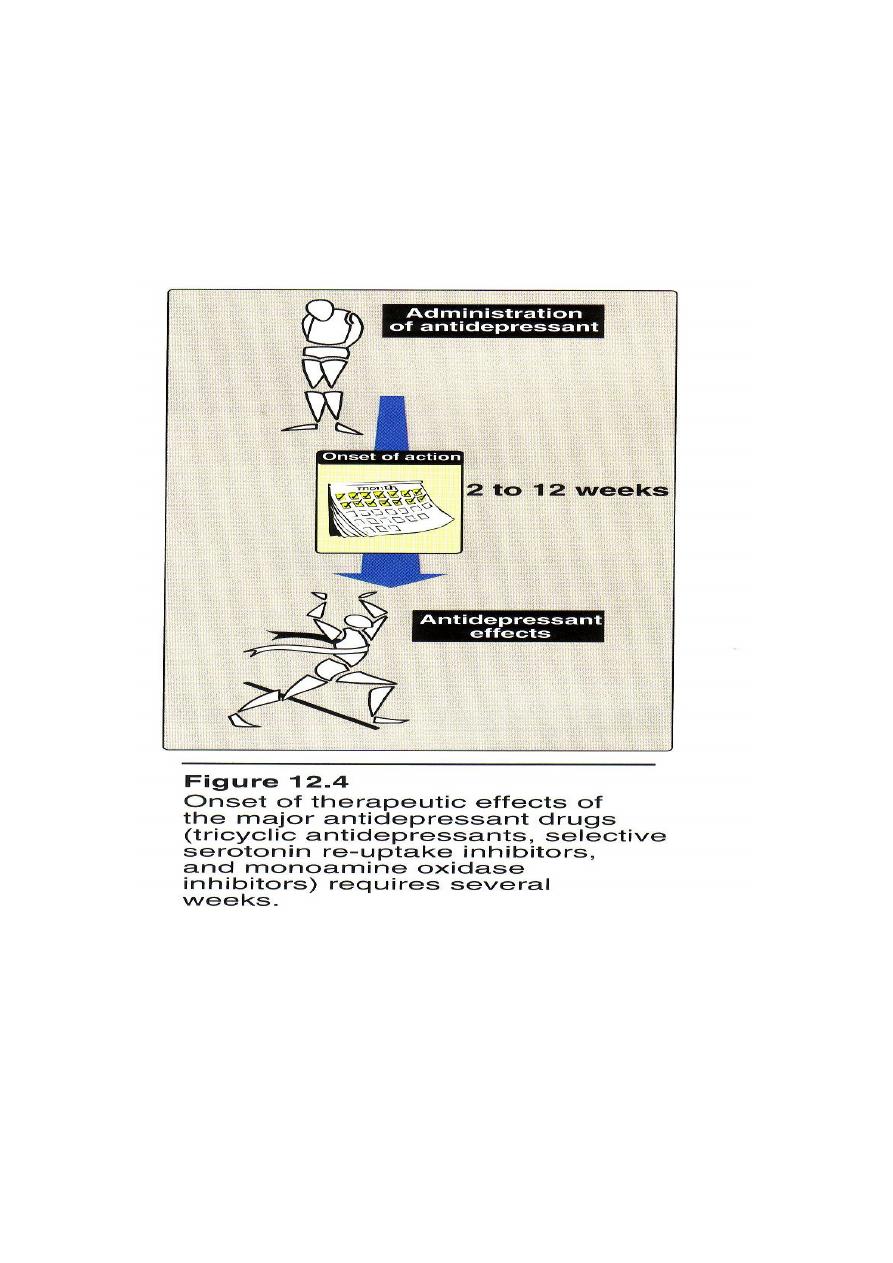
• Antidepressants, including SSRIs typically take 2 weeks to produce
improvement in mood and may require 12 weeks or more.
However none of the antidepressants is uniformly beneficial.
About 40% of patients respond well to treatment. Patients who do
not respond to one drug may respond to another drug, and
approximately 80% or more will respond to at least one
antidepressant drug. Antidepressants do not elevate mood in
normal subjects
Therapeutic Uses of SSRIs
• Used in depression,
• Obsessive compulsive disorders (fluvoxamine)
• Panic disorders
• Generalized anxiety
• Premenestrual dysphoric disorders
• Bulimia nervosa
Pharmacokinetics
• All SSRIs are well absorbed from GIT. Food has little effect on
absorption. All are well distributed with large V
d.
Most have long
plasma half-life. Metabolized by liver and excreted in urine.
• Fluoxetine: Has longer half-life about 50 hours and available as
sustained release preparations allowing once-weekly dosing. Also

9
it is metabolized to norfluoxetine which is active having a half-life
of 10 days.
• Fluoxetine and paroxetine: are potent enzyme inhibitors
• Paroxetine and sertraline are partly excreted in bile
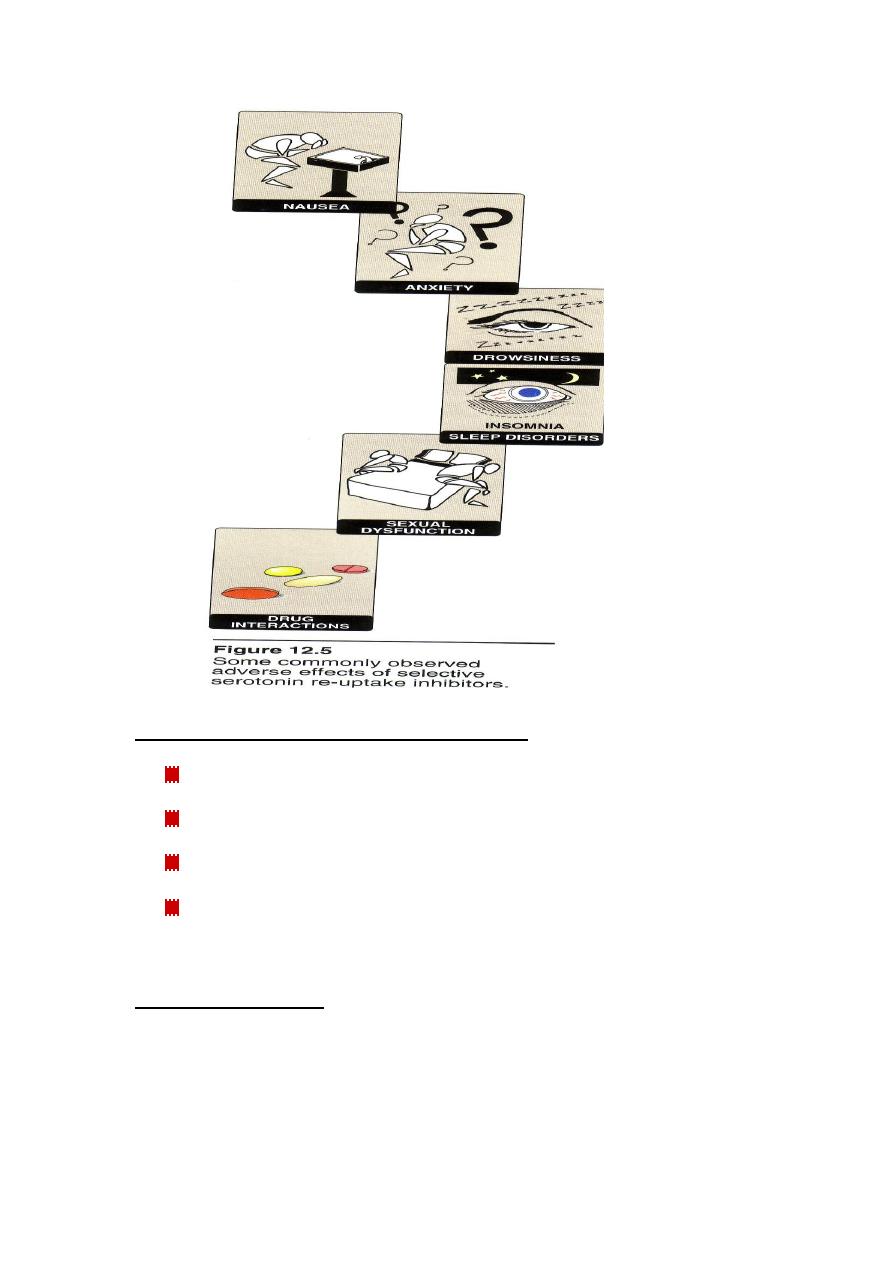
Adverse effects of SSRIs
• Sleep disturbance: Paroxetine and fluvoxamine are sedating, while
fluoxetine is activating causing insomnia
• Sexual dysfunction: Loss of libido, delayed ejaculation, anorgasmia
• Uses in children and teenagers: one out of 50 children becomes
suicidal as a result of use of SSRIs
• Overdose: fluoxetine may cause seizures. They cause “serotonin
syndrome” characterized by hyperthemia,muscle rigidity, clonic
muscle twitching and changes in mental status in the presence of
MAOIs
01
Monoamine oxidase inhibitors (MAOIs)
Phenelzine (Nardil)
Isocarboxazid (Marplan)
Tranylcypromine (Parnate)
Selegiline (Deprenyl)
MAO INHIBITORS
Mechanism of action:
Inhibit MAO enzymes (non-selective):
1) Irreversible MAO inhibitors
Phenelzine and isocarboxazid => hydrazides.
00
2) Reversible MAO Inhibitors. RIMA (reversible inhibitor of monoamine
oxidase A)
Tranylcypromine => non-hydrazide,
prolonged blockade, but reversible within 4hr.
Decrease metabolism of most biogenic amines (NE, 5HT, DA, tyramine,
octopamine).
Acute administration causes:
NE and 5-HT in synaptic terminals in brain but
NE in PNS.
NE synthesis.
Acute euphoria
Suppressed REM sleep.
Chronic administration causes:
NE-stimulated cAMP in brain.
Down regulation of
receptors.
Down regulation of 5-HT
2
receptors.
MAO-A NE, 5-HT, Tyramine
MAO-B DA
Selective MAOIs:
Inhibitors MAO-A
Moclobemide, Clorgyline
Inhibitors of MAO-B.
Deprenyl, Selegiline
02
Wine-and-Cheese Reaction
- Fatal interaction with tyramine-containing foods (fermented foods in
particular, such as wine and cheese).
-
MAO-A =>
Tyramine in the body =>
NE in circulation => induces
hypertensive crisis => can lead to intracranial bleeding and other organ
damage.
Negative drug interactions with:
Any drug metabolized by MAOs* including SSRIs, TCAs and meperidine,
alcohol, CNS depressants, sympathomimetics, phenylephrine (O/C nasal
decongestants), ampetamines, and other indirect-acting adrenergic
drugs.
* Interaction with drugs metabolized by MAOs (e.g. Meperidine (opioid
analgesics) => hyperpyrexia or “hyperexcitation syndrome” involving
high fever, delirium and hypertension).
Other side effects:
Hypotension
Hepatotoxicity.
Sedation.
Done by
Ali Kareem
