Sunday 22 / 3 / 2015
©Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
مكتب اشور لالستنساخ
ANTI-TB DRUGS
Lecture 4
Total lectures NO. 48
Dr. Huda Al-Qadhi
2 |
P a g e
Mycobacteria are slender, rod shaped bacteria with lipid rich cell wall.
Mycobacterial infections are intracellular. Mycobacterium tuberculosis can
lead to serious infections.
It is currently estimated that about 1/3 of the world is infected with
M.tuberculosis.
Treating tuberculosis (TB) presents therapeutic problems. The organism
grows slowly & resistant organisms readily emerge. Therefore, multi drug
therapy is employed when treating TB in an effort to delay or prevent the
emergence of resistant strains.
Isoniazid, rifampin, ethambutol, streptomycin & pyrazinamide are the
principle or so called 1
st
line drugs because of their efficacy & acceptable
degree of toxicity. Although treatment regimens vary in duration & in the
agent employed, they always include a minimum of 2 drugs, preferably with
both being bactericidal.
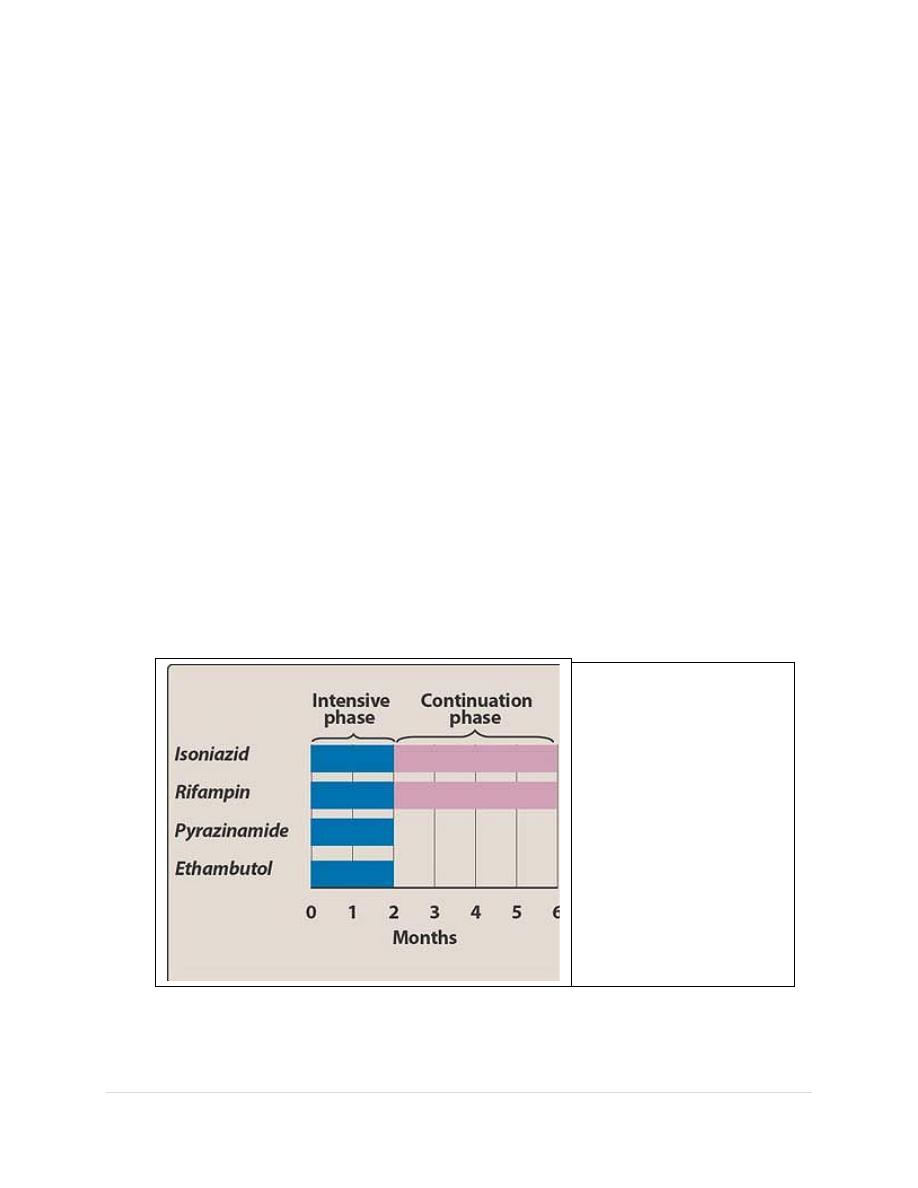
Isoniazid
One of several
recommended
multidrug
schedules for
the treatment
of tuberculosis.
3 |
P a g e
Isoniazid
Isoniazid, often referred to as INH, the hydrazide of isonicotinic acid, is a synthetic
analog of pyridoxine. It’s the most potent of the antitubercular drugs.
Mechanism of action:
INH is a prodrug that is activated by a mycobacterial catalase peroxidase (KatG).
There are at least 2 different target enzymes for INH within the unique type II
fatty acid synthase system involved in the production of mycolic acids. The
activated drug covalently binds to & inhibits these enzymes, which are essential for
the synthesis of mycolic acid. Mycolic acid is a β-hyroxylated fatty acid found in
the mycobacterial cell walls.
Antimicrobial spectrum:
For bacilli in the stationary phase, INH is bacteriostatic, but for rapidly dividing
organisms, it is bactericidal. It is effective against intracellular bacteria. Isoniazid
is specific for treatment of M.tuberculosis (mycobacterium kansasi may be
susceptible at higher drug levels).
Resistance: This is associated with several chromosomal mutations. When it is
used alone,resistant organisms rapidly emerge.
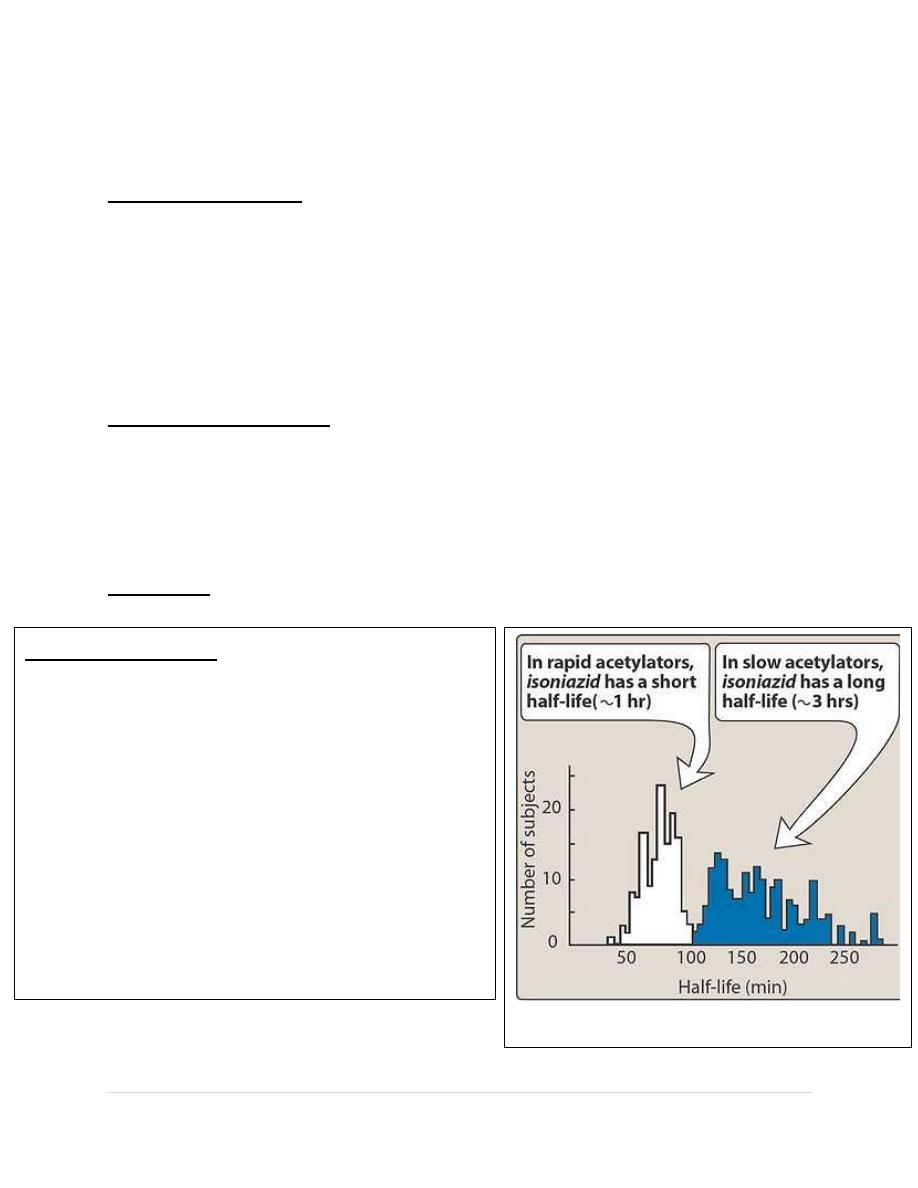
Bimodal distribution of isoniazid half-lives caused by
rapid and slow acetylation of the drug.
Pharmacokinetics:
Orally administrated INH is readily absorbed.
Absorption is impaired if INH is taken with food.
The drug diffuses into all body fluids, cells &
caseous material. INH undergoes N-acetyaltion &
hydrolysis ,resulting in inactive products.
Acetylation is genetically regulated ,with the fast
acetylator trait being autosomally dominant. A
bimodal distribution of fast & slow acetylators
exists. Slow acetylators excrete more of the parent
compound.
4 |
P a g e
Adverse effects:
1. Peripheral neuritis: peripheral neuritis (manifesting as parasthesia), which is
the most common adverse effect, appears to be due to a relative pyridoxine
(vitamin B6) deficiency.
2. Hepatitis & idiosyncratic hepatotoxicity: potential fatal hepatitis is the most
severe side effect of INH. It is caused by a toxic metabolite during the
metabolism of INH.
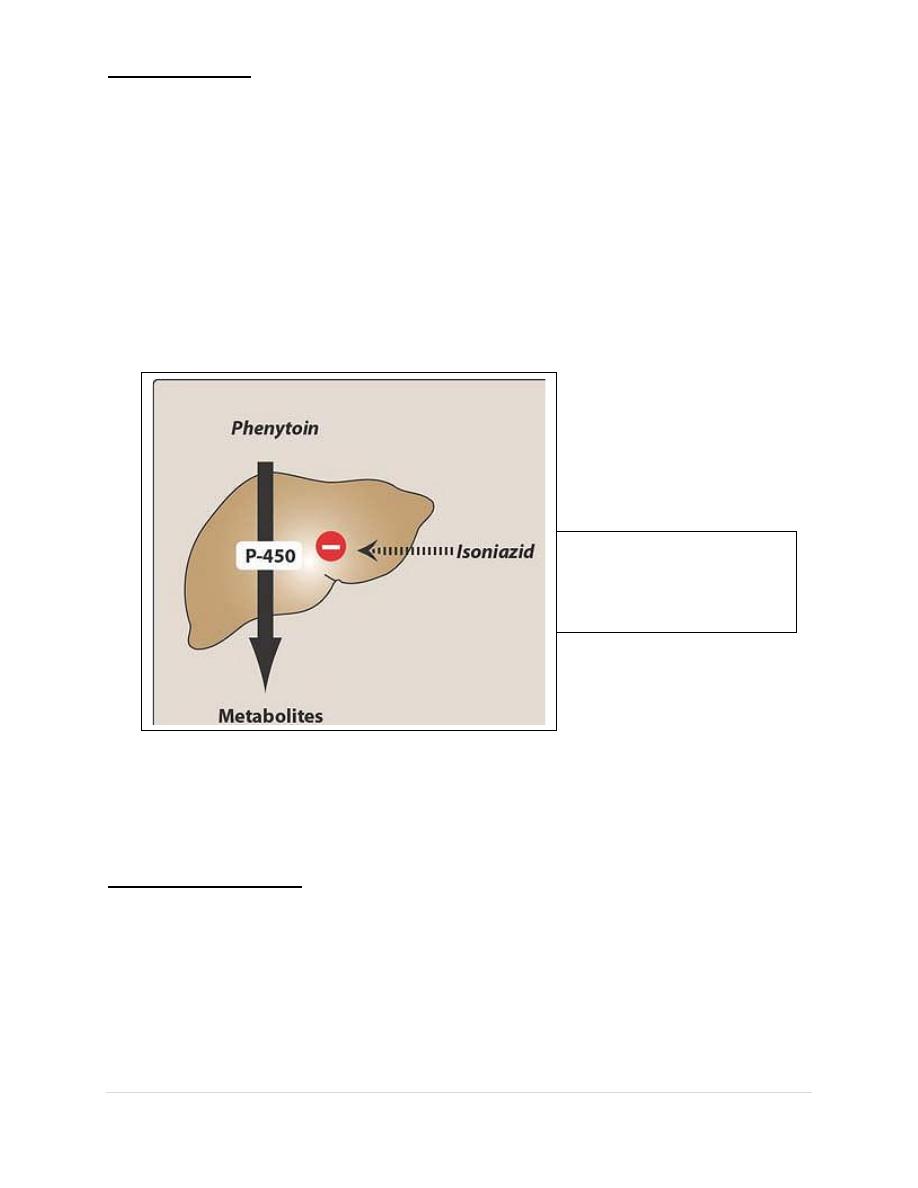
3. Drug interactions: because INH inhibits metabolism of phenytoin, INH can
potentiate the adverse effect of that drug (e.g. nystagmus, ataxia)
4. Other adverse effects: mental abnormalities, convulsions, optic neuritis &
hyper sensitivity reactions have been observed.
Rifampin
Rifampin has a broader antimicrobial activity than INH & has found application in
the treatment of a number of different bacterial infections.
Mechanism of action: Rifampin blocks transcription by interacting with β-subunit
of bacterial but not human DNA dependant RNA polymerase. Rifampin inhibits
RNA synthesis by suppressing the initiation step.
Antimicrobial spectrum: Rifampin is bactericidal for both intracellular &
extracellular mycobacteria including M.tuberculosis & atypical mycobacteria(e.g
M.kansasii). It is effective against many gram –ve & gram +ve organisms and is
frequently used prophylactically for individuals exposed to meningitis caused by
Isoniazid potentiates the
adverse effects of
phenytoin.
5 |
P a g e
meningococci or H.influenza. Rifampin is the most active antileprosy drug present.
It is usually given in combination with other drugs. .Rifabutin, an analog of
rifampin,has some activity against Mycobacterium avium-intracellulare complex,
but it is less active against TB.
Resistance: resistance to rifampin can be caused by mutation in the affinity of the
bacterial DNA-dependant RNA polymerase for the drug or by decreased
permeability.
Pharmacokinetics: absorption is adequate after oral administration & distribution
occurs to all body fluids. Adequate levels are attained in the CSF even in the
absence of inflammation. The drug is taken up by the liver and undergoes
enterohepatic cycling. Rifampin itself can induce the hepatic mixed function
oxidases, leading to a shortened t1/2. Elimination of metabolites & the parent drug
is via the bile into the feces or via the urine (urine,feces and other secretions have
orange-red color).
Adverse effects: GIT upset, rashes, fever ,hepatitis, and a flu-like syndrome
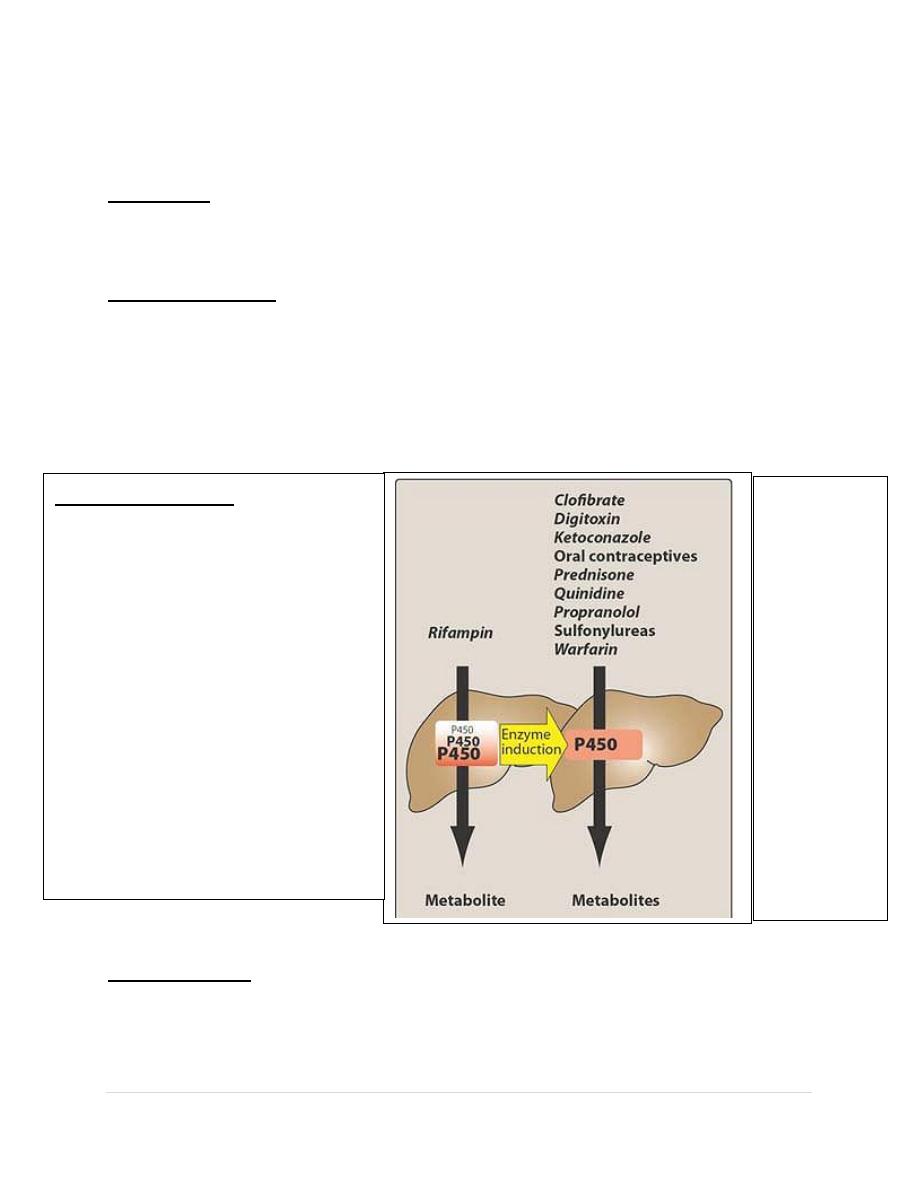
Drug interaction:
because rifampin can induce a
number of cytochrome p450
enzymes, it can decrease the t1/2
of the other drugs that are
coadministered & metabolized
by this system. Rifabutin, an
analog of rifampin, doesn’t
increase the metabolism of other
drugs.
Rifampin
induces
cytochrome
P450 which
can decrease
the half-lives
of
coadminister
ed drugs
that are
metabolized
by this
system

6 |
P a g e
Pyrazinamide
Pyrazinamide is a synthetic, orally effective, bactericidal, antitubercular
agent used in combination with isoniazid & rifampin. Pyrazinamide must be
enzymatically hydrolyzed to pyrazinoic acid, which is the active form of the
drug. Some resistant strains lack the pyrazinamidase. Pyrazinamide is active
against tubercle bacilli in the acidic environment of lysosomes as well as in
macrophages.
Pyrazinamide distributes throughout the body, penetrating the CSF. About 1-
5% of patients taking isoniazid, rifampin & pyrazinamide may experience
liver dysfunction. Urate retention can also occur & may precipitate a gouty
attack.
Ethambutol
Ethambutol is bacteriostatic and specific for most strains of M.tuberculosis
and M.kansasii. It inhibits arabinosyl transferase-an enzyme that is
important for the synthesis of mycobacterial arabinogalactan cell wall.
Ethambutol can be used in combination with pyrazinamide, isoniazid &
rifampin to treat TB.
Absorbed on oral administration, ethambutol is well distributed. Penetration
into the CSF is therapeutically adequate in tuberculous meningitis. Both
parent drug & metabolites are excreted by glomerular filtration & tubular
secretion.
The most important adverse effect is optic neuritis, which results in
diminished visual activity & loss of ability to discriminate between red &
green.Visual acuity should be periodically examined. Discontinuation of the
drug results in reversal of the toxic symptoms. In addition, urate excretion is
decreased by the drug; thus gout may be exacerbated.
Therapeutic margin of 1
st
line drugs
As with any drug, antitubercular drugs have a therapeutic margin-that is the
difference between the minimum drug concentration required to inhibit the growth
of M.tuberculosis & the maximum concentration that can be given without
provoking drug toxicity. The therapeutic margin is large for isoniazid & rifampin
but narrow for pyrazinamide, ethambutol & streptomycin.

7 |
P a g e
Alternate 2
nd
line drugs
A number of drugs are considered to be second-line drugs, either because they’re
no more effective than the 1
st
line agents & their toxicities are often more serious
or they’re particularly active against atypical strains of mycobacteria.
a)
Aminosalicyclic acid: It is bacteriostatic agent that acts as a competitive
inhibitor for P-amonobenzoic acid (PABA) in folate biosynthesis.
b)
Capreomycin: It is a peptide that inhibits protein synthesis. Capreomycin is
primarily reserved for the treatment of multi drug resistant tuberculosis.It is
administered pareterally.
c)
Cycloserine: It is tuberculostatic agent that antagonizes bacterial cell wall
synthesis. It distributes well throughout body fluids, including the CSF.
Adverse effects involve CNS disturbances,exacerbation of epileptic seizures
& peripheral neuropathies.
d)
Ethionamide: It is a structural analog of isoniazid. It’s widely distributed
throughout the body fluids, including the CSF. Adverse effects include
gastric irritation, hepatotoxicity, peripheral neuropathies & optic neuritis.
e)
Fluoroquinolones: They have an important role in the treatment of multi-
drug resistant tuberculosis. An example is moxifloxacin & levofloxacin.
f)
Macrolide: Macrolides such as azithromycin & clarithromycin are part of
the regimen that includes ethambutol & rifabutin used for the treatment of
infections by M.avium-intracellular complex. Azithromycin is preferred for
HIV-infected patients, because it’s least likely to interfere with the
metabolism of antiviral drugs.
g)
Streptomycin : Its action is directed against extracellular organisms
.Infections due to streptomycin-resistant organisms may be treated with
kanamycin or amikacin, to which these bacilli remain sensitive.
Done by
Ali Kareem
