Sunday 1 / 3 / 2015
©Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
مكتب اشور لالستنساخ
ANTI-MICROBIAL DRUGS
Lecture 9
Total lectures NO. 41
Dr. Haidar Al-Shakarchi
Pharmacology
Anti-Microbial Drugs 3
1
Dr. Haidar Al-Shakarchi
Lec. 9
(2) Cephalosporins
They're β-lactam antibiotics that are closely related both structurally &
functionally to penicillins. Most cephalosporins are produced semi-synthetically by
the chemical attachment of side chains to 7-aminocephalosporanic acid.
Cephalosporins have the same mode of action as penicillins & they are affected by
the same resistance mechanisms. However, they tend to be more resistant than the
penicillins to β-lactamases.
Antibacterial spectrum:
Cephalosporins have been classified as 1
st
, 2
nd
, 3
rd
or 4
th
generation, based largely
on this bacterial susceptibility patterns & resistance to β-lactamases. They're
ineffective against MRSA, listeria monocytogenes, Clostridium difficile & the
enterococci.
1. First generation:
This group includes cephalexin, cefazolin, cephalothin & cefadroxil. These drugs
are very active against gram +ve cocci, including staphylococci, streptococci &
pneumococci. They're resistant to the staphylococcal penicillinase. Anaerobic
streptococci are usually sensitive. They also have activity against gram –ve rods,
mainly Proteus mirabilis, E.coli & Klebsiella pneumoniae (the acronym PEcK has
been suggested). Cefazolin finds application as a single prophylaxis dose prior to
surgery because of its 1.8hr half-life and its activity against penicillinase producing
S.aureus.Cefazolin is effective for most surgical procedures,including orthopedic
surgery because of its ability to penetrate bone.
2. Second generation:
Members of this group include cefaclor, cefoxitin, cefuroxime, cefamandole &
cefotetan. The 2
nd
generation cephalosporins display greater activity against 3
additional grams –ve organisms: H.influenzae, enterobacter aerogenes & some
Neisseria species (HENPEcK), whereas activity against gram +ve organisms is
weaker.

Pharmacology
Anti-Microbial Drugs 3
2
Dr. Haidar Al-Shakarchi
Lec. 9
The exception to this generalization is cefoxitin which has little activity against
H.influenzae yet is effective against the anaerobe Bacteroides fragilis. Thus
cefoxitin is useful in patients with intra-abdominal sepsis & pelvic inflammatory
disease. Cefuroxime has a longer half-life & crosses the blood brain barrier. It can
be used for community acquired pneumonia.
3. Third generation:
These cephalosporins have assumed an important role in the treatment of
infectious diseases. 3
rd
generation agents include cefotaxime, ceftriaxone,
ceftazidime, cefoperazone, ceftizoxime & cefixime. The major features of these
drugs are their gram –ve coverage & the ability of some to cross the blood brain
barrier. Although inferior to 1
st
generation cephalosporins in regard to their activity
against gram +ve cocci, the 3
rd
generation cephalosporins have enhanced activity
against gram –ve bacilli, including those mentioned above, as well as most other
enteric organisms plus serratia.
Ceftazidime has activity against pseudomonas aeruginosa. Ceftriaxone or
cefotaxime have become agents of choice in the treatment of meningitis.
Ceftriaxone has the largest half-life of any cephalosporin (6-8hrs), which permits
once a day dosing. It is effective against penicillin resistant Neisseria gonorrhoeae.
The drug is excreted in bile &is frequently employed in patients with renal
insufficiency. It has a good penetration into bone. Cefixime is administered orally
once daily.
4.
Fourth generation: cefepime is classified as a 4
th
generation cephalosporin &
must be administered parenterally. Cefepime has a wide antibacterial spectrum,
being active against streptococci & staphylococci. Cefepime is also effective
against aerobic gram –ve organisms, such as enterobacter, P.mirabilis, E.coli,
K.pneumoniae and P.aeruginosa
Pharmacology
Anti-Microbial Drugs 3
3
Dr. Haidar Al-Shakarchi
Lec. 9
Resistance:
Mechanisms of bacterial resistance to the cephalosporins are
essentially the same as those described for the penicillins. Although they're not
susceptible to hydrolysis by the staphylococcal penicillinas; cephalosporins maybe
susceptible to extended-spectrum β-lactamases.
Pharmacokinetics:
1. Administration: most of the cephalosporins must be administered I.V or I.M
because of their poor oral absorption. Cephalexin, cefadroxil, cefaclor, & cefixime
are administered orally.
2. Distribution: Adequate therapeutic levels in the CSF, regardless of
inflammation are achieved only with 3
rd
generation cephalosporins.For
example,ceftriaxone or cefotaxime are effective in the treatment of neonatal and
childhood meningitis caused by H.influenzae. All cephalosporins cross the
placenta.
3. Fate: elimination of cephalosporins occurs through tubular secretion &/or
glomerular filtration. Therefore doses must be adjusted in cases of severe renal
failure. Ceftriaxone is excreted through the bile into the feces.
Adverse effect:
1. Allergic manifestation: the cephalosporins should be avoided or used with
caution in individuals who are allergic to penicillins (5-15% show cross
sensitivity). In contrast, the incidence of allergic reactions to cephalosporin is 1-2%
in patients without history of an allergy to penicillins.
2. Disulfiram-like effect: when cefamandole, cefotetan or cefoperazone is ingested
with alcohol, a disulfiram-like effect is seen. This occurs because they block the
second step in alcohol oxidation, which results in the accumulation of
acetaldehyde.The toxicity is due to the presence of the methyl thio tetrazol (MTT)
group.
3. Bleeding: bleeding also associated with agents that contain the MTT group
because of anti-vitamin K effects.
Pharmacology
Anti-Microbial Drugs 3
4
Dr. Haidar Al-Shakarchi
Lec. 9
(3) Carbapenems:
Carbapenems are synthetic β-lactam antibiotics. Imipenem , meropenem and
ertapenem are the only drugs of this group currently available. Imipenem is
compounded with cilastatin to protect it from metabolism by renal
dehydropeptidase.
Antibacterial spectrum:
Imipenem/cilastatin & meropenem are the broadest- spectrum β-lactam antibiotics
preparations currently available. Imipenem resists hydrolysis by most β-
lactamases, but not the metallo- β-lactamases. The drug plays a role in empiric
therapy, because it is active against penicillinase-producing gram +ve & -ve
organisms, anaerobes & P. aeruginosa. Meropenem has antibacterial activity
similar to that of imipenem.Ertapenem is not an alternative for P.aeruginosa.
Pharmacokinetics:
Imipenem & meropenem are administered I.V & penetrate well into body tissue
& fluids, including the CSF when the meninges are inflamed. They're excreted by
glomerular filtration.
Imipenem undergoes cleavage by a dehydropeptidase found in the brush border
of the proximal renal tubule. This enzyme forms an inactive metabolite that is
potentially nephrotoxic. Compounding the imipenem with cilastatin protects the
parent drug & thus prevents the formation of the toxic metabolite. This allows the
drug to be used in the treatment of UTIs.Meropenem doesn't undergo metabolism.
Adverse effects:
imipenem/cilastatin can cause vomiting & diarrhea.
Eosinophilia & neutropenia are less common. High levels of imipenem may
provoke seizures.
Pharmacology
Anti-Microbial Drugs 3
5
Dr. Haidar Al-Shakarchi
Lec. 9
(4) Monobactams:
These drugs are with a monocyclic β-lactam ring. Aztreonam, which is the only
commercially available monobactam, is resistant to the action of β-lactamases.
Aztreonam is active against gram –ve rods primarily the enterobacteriaceae . It has
no activity against gram +ve bacteria or anaerobes.
This narrow antimicrobial spectrum precludes its use alone in empiric therapy.
Aztreonam is administered either I.V or I.M & is excreted in the urine. This drug
is relatively nontoxic & has a low immunogenic potential. Thus, it may offer a safe
alternative for treating patients who are allergic to penicillins &/or cephalosporins.
ß-lactamase inhibitors:
β-lactamase inhibitors such as clavulanic acid, sulbactam & tazobactam contain
a β-lactam ring, but by themselves don't have significant antibacterial activity.
Instead, they bind to & inactivate β-lactamases, thereby protecting the antibiotics
that are normally substrates for these enzymes.
They're potent inhibitors of many but not all bacterial β-lactamases. Β-lactamase
inhibitors are most active against β-lactamases produced by staph., H.influenzae,
gonococci, salmonella, shigella, E.coli & K.pneumoniae. They're not good
inhibitors of β-lactamases produced by pseudomonas & enterobacter.
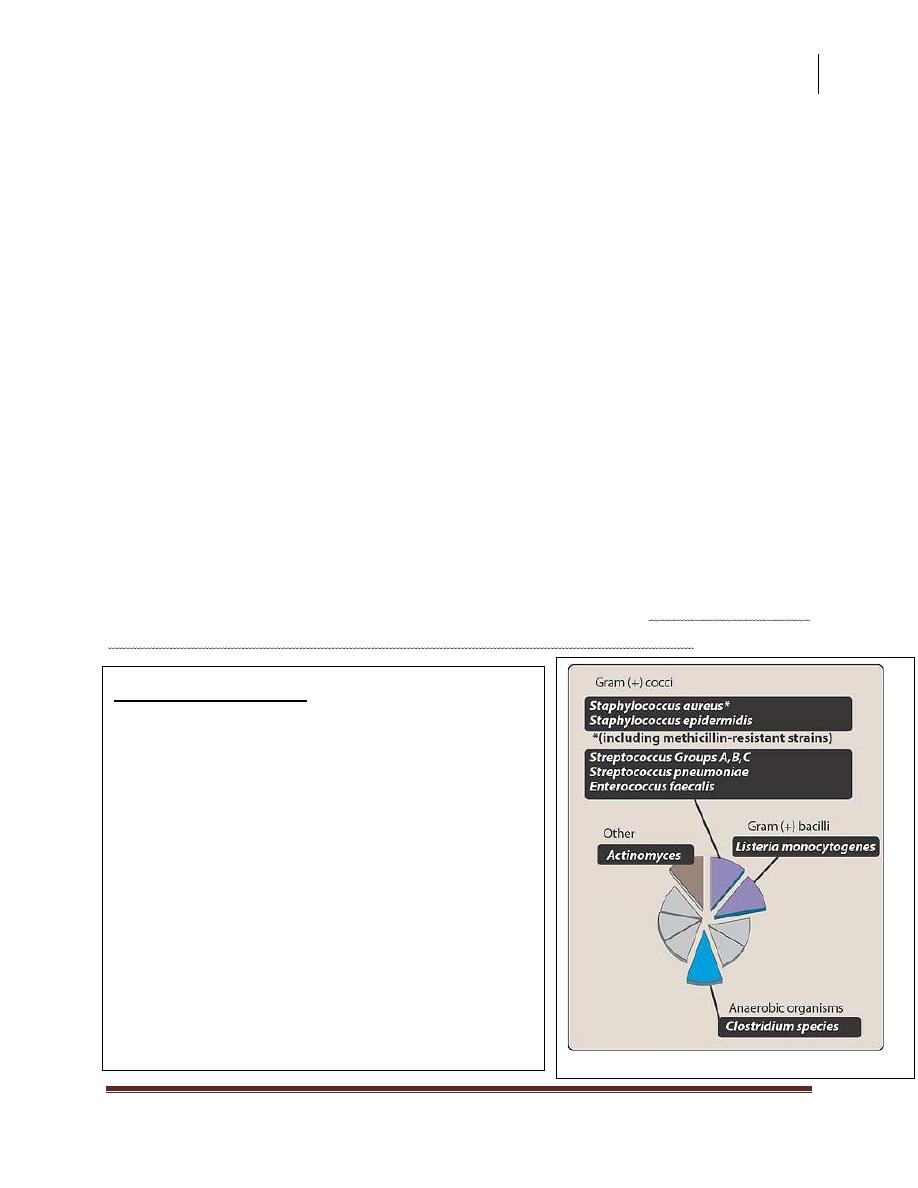
Antimicrobial spectrum of vancomycin.
VANCOMYCIN
Vancomycin is a tricyclic glycopeptides
that has become increasingly important.
Bacitracin is a mixture of glycopeptides
that also inhibits bacterial cell wall
synthesis; however, its use is limited to
topical application because of its potential
for nephrotoxicity. Vancomycin inhibits
synthesis of bacterial cell wall
phospholipids as well as peptidoglycan
polymerization.
Pharmacology
Anti-Microbial Drugs 3
6
Dr. Haidar Al-Shakarchi
Lec. 9
Antibacterial spectrum:
Vancomycin is effective primarily against gram +ve organisms. It's been
lifesaving in the treatment of methicillin-resistant staph aureus (MRSA) &
methicillin-resistant staph epidermidis (MRSE) infections, as well as enterococcal
infections. Vancomycin is used in the treatment of serious infections caused by β-
lactam resistant gram +ve microorganisms & in patients with gram +ve infections
who have a serious allergy to the β-lactams.
Oral vancomycin is limited to treatment for potentially life threatening
antibiotic associated colitis due to C.difficile or staph. Vancomycin is used in
individuals with prosthetic heart valves & in patients undergoing implantation
with prosthetic devices. Vancomycin acts synergistically with aminoglycosides
& this combination can be used in the treatment of enterococcal endocarditis.
Resistance:
vancomycin resistance can be caused by plasmid-mediated changes
in the permeability to the drug or by decreased binding of vancomycin to receptor
molecules.
Pharmacokinetics:
Slow I.V infusion is employed for treatment of systemic
infections or prophylaxis. Because vancomycin is not absorbed after oral
administration, this route is only employed for the treatment of antibiotic induced
colitis due to c. difficile when metronidazole has proven ineffective. Inflammation
allows penetration into the meninges. However, it is often necessary to combine
vancomycin with other antibiotics, such as ceftriaxone. Metabolism of the drug is
minimal & 90-100% is excreted by glomerular filtration.
Adverse effect:
Side effects are a serious problem & include fever, chills &
phlebitis at the infusion site. Flushing (red man syndrome) & shock results from
histamine release. Dose related hearing loss has occurred in patients with renal
failure. Ototoxicity & nephrotoxicity are more common when vancomycin is
administered with another drug that can also produce these effects.
Pharmacology
Anti-Microbial Drugs 3
7
Dr. Haidar Al-Shakarchi
Lec. 9
Daptomycin
Is a cyclic lipopeptide antibiotic that is an alternative to other agents such as
linezolid and quinupristin – dalfopristin , for treating infections caused by resistant
gram –positive organisms, including MRSA and vancomycin -resistant
enterococci(VRE) .
Done by
Ali Kareem
