Sunday 1 / 3 / 2015
©Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
مكتب اشور لالستنساخ
ANTI-MICROBIAL DRUGS
Lecture 8
Total lectures NO. 40
Dr. Haidar Al-Shakarchi
Pharmacology
Anti-Microbial Drugs 2
1
Dr. Haidar Al-Shakarchi
Lec. 8
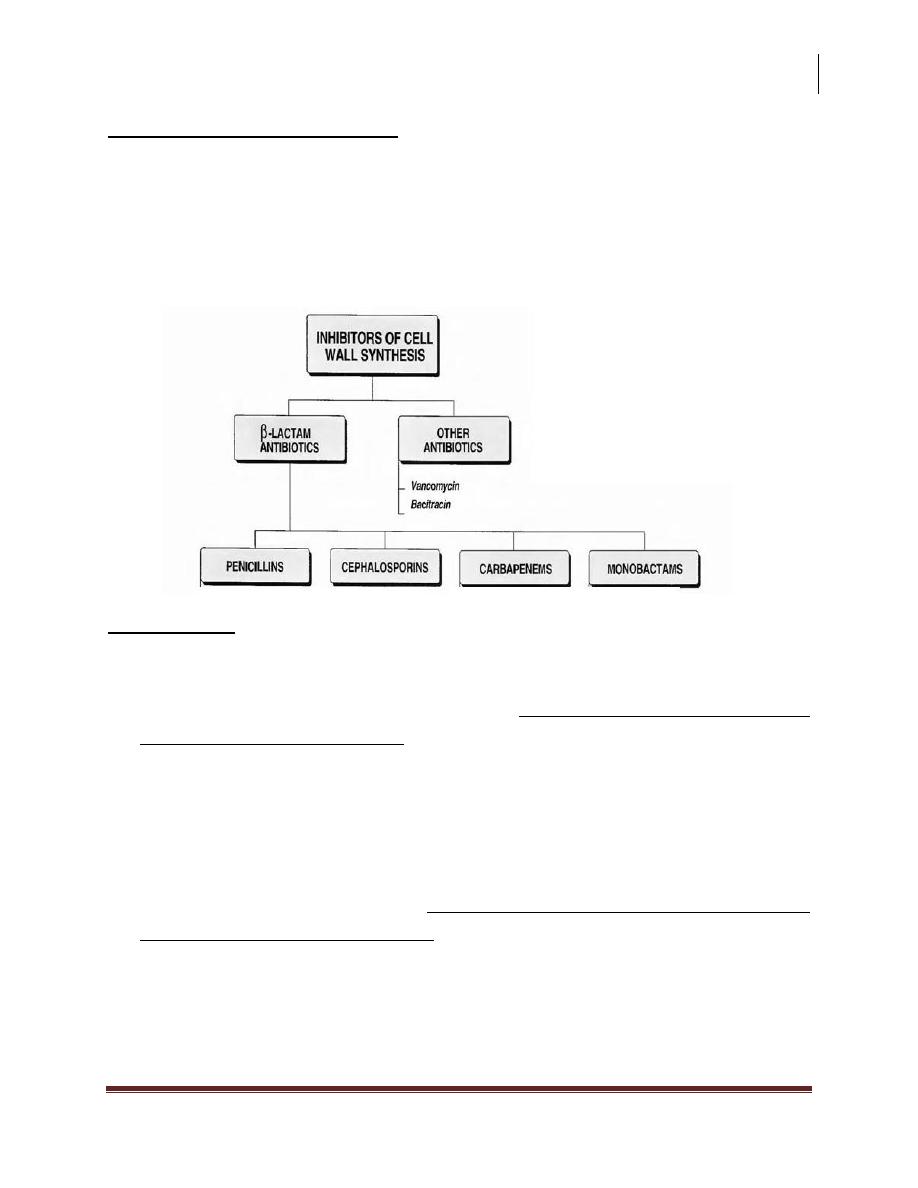
Inhibitors of Cell wall synthesis:
Some antimicrobial drugs interfere with synthesis of bacterial cell wall. The cell
wall is a polymer called peptidoglycan that consists of glycan units joined to each
other by peptide cross-links.
To be maximally effective, inhibitors of cell wall synthesis require actively
proliferating microorganisms.
(1) Penicillins
The penicillins are among the most widely effective antibiotics & also the least
toxic drugs known, but increased resistance has limited their use.
Members differ from one another in the R substituent attached to the 6-
aminopenicillanic acid residue.
The nature of this side chain affects
1
the antimicrobial spectrum,
2
stability to
stomach acid, &
3
susceptibility to bacterial degradative enzymes (β-
lactamases).
Mechanism of action:
The penicillins interfere with last step of bacterial cell wall synthesis
(transpeptidation or cross linkage), resulting in exposure of the osmotically less
stable membrane. Cell lysis can then occur, either through osmotic pressure or
through the activation of autolysis. These drugs are thus bactericidal.
Penicillins are only effective against rapidly growing organisms that synthesize
a peptidoglycan.
Pharmacology
Anti-Microbial Drugs 2
2
Dr. Haidar Al-Shakarchi
Lec. 8
1. Penicillin binding proteins (PBP
s
): penicillins inactivate numerous proteins
on the bacterial cell membrane. These PBP
s
are bacterial enzymes involved in
the synthesis of the cell wall and in the maintenance of the morphologic
features of the bacterium. Alterations in some of these target molecules provide
the organism with resistance to the penicillins e.g. methicillin resistant
staphylococcus aureus (MRSA).
2. Inhibition of transpeptidase: some PBP
s
catalyse formation of the cross-
linkages between peptidoglycan chains. Penicillins inhibit this transpeptidase-
catalyzed reaction, thus hindering the formation of cross links essential for cell
wall integrity.
3. Production of autolysins: many bacteria particularly the gram +ve cocci
produce degradative enzymes (autolysins) that participate in the normal
remodeling of the bacterial cell wall. In the presence of penicillin, the
degradative action of the autolysins proceeds in the absence of cell wall
synthesis.
Antibacterial Spectrum
In general, gram +ve microorganisms have peptidoglycan cell walls that are easily
traversed by penicillins to reach the PBP
s
in the periplasmic space.
Gram –ve microorganisms have an outer lipoploysaccharide membrane
surrounding the cell wall that presents a barrier to the water soluble penicillins.
However, they've proteins inserted in the lipopolysaccharide layer that act as water
filled channels (called porins) that permit transmembrane entry.
(Note: Pseudomonas aeruginosa lacks porins).
1.
Natural penicillins:
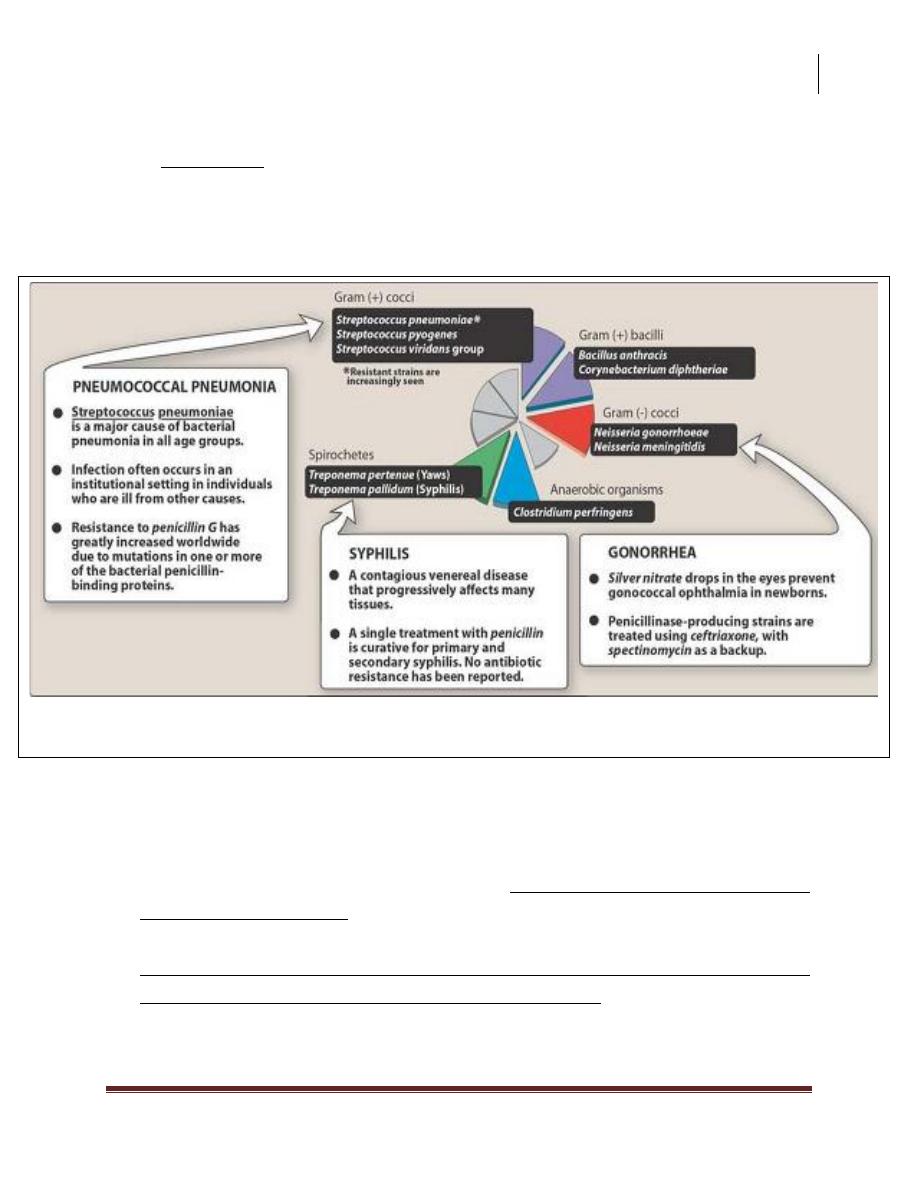
Penicillin G (benzyl penicillin) is the cornerstone of therapy for infections
caused by a number of
Gram +ve cocci (Streptococcus pyogenes, Streptococcus viridans),
Gram +ve bacilli (Bacillus anthracis, Corynebacterium diphetheriae),
Gram –ve cocci (Neisseria gonorrhoeae, Neisseria meningitidis),
Anaerobic organisms (Clostridium perfringens), & Spirochetes (Treponema
pallidum).
Pharmacology
Anti-Microbial Drugs 2
3
Dr. Haidar Al-Shakarchi
Lec. 8
Penicillin G is susceptible to inactivation by β-lactamase (penicillinases).
Penicillin V has a spectrum similar to that of penicillin G, but it's not used
for treatment of bacteremia because of its higher MBC. It is more acid stable
than penicillin G. It is often employed for the treatment of oral infections,
where it is effective against some anaerobic organisms.
2.
Anti-staphylococcal penicillins: Methicillin, nafcillin, oxacillin, cloxacillin
& dicloxacillin are penicillinase-resistant penicillins.
Their use is restricted to the treatment of infections caused by penicillinase-
producing staphylococci.
Because of its toxicity, methicillin is not used.
A serious source of hospital-acquired infection, MRSA are usually susceptible
to vancomycin and rarely to ciprofloxacin or rifampin.
Typical therapeutic applications of penicillin G
Pharmacology
Anti-Microbial Drugs 2
4
Dr. Haidar Al-Shakarchi
Lec. 8
3.
Extended spectrum penicillins:
Ampicillin and amoxicillin have an antimicrobial spectrum similar to that
penicillin G, but are more effective against gram –ve bacilli.
They are therefore referred to as extended spectrum penicillins. The
antimicrobial spectrum of ampicillin includes gram +ve bacilli (listeria
monocytogenes) and gram –ve rods (Proteus mirabilis & Salmonella typhi
while Escherichia coli and Haemophilus influenzae are frequently resistant).
Amoxicillin is employed prophytically by dentists for patients with
abnormal heart values who are to undergo extensive oral surgery.
Resistance to these antibiotics is now a major clinical problem because of
inactivation by plasmid-mediated penicillinase. Formulation with a β lactamase
inhibitor, such as clavulanic acid or sulbactam, protects amoxicillin or
ampicillin, respectively from enzymatic hydrolysis & extends their
antimicrobial spectrum.
4. Anti-pseudomonal penicillins: Carbenicillin,ticarcillin,and piperacillin are
called antipseudomonal penicillin because of their activity against
Pseudomonas aeruginosa. Piperacillin is the most potent of these antibiotics.
They're effective against many gram –ve bacilli including Enterobacter,
Escherichia coli, Proteus, Haemophilus influenzae & Pseudomonas aeruginosa,
but not against Klebsiella, because of its constitutive penicillinase.
Formulation of ticarcillin or piperacillin with clavulanic acid or tazobactam,
respectively, extends their antimicrobial spectrum to include penicillinase
producing organisms.
Penicillins & aminoglycosides: The antibacterial effects of all β-lactam
antibiotics are synergistic with the aminoglycosides. Because cell wall
synthesis inhibitors alter the permeability of bacterial cells, these drugs can
facilitate the entry of aminoglycosides that might not ordinarily gain access to
intracellular target sites.
Pharmacology
Anti-Microbial Drugs 2
5
Dr. Haidar Al-Shakarchi
Lec. 8
Resistance
Natural resistance to the penicillins occurs in organisms that either lack a
peptidoglycan cell wall e.g. mycoplasma or have cell wall that are impermeable to
the drugs.
Acquired resistance to the penicillins by plasmid transfer has become a significant
clinical problem because an organism may become resistant to several antibiotics
at the same time.
1.
β-lactamase activity: this family of enzymes hydrolyzes the cyclic amide
bond of the β-lactam ring, which results in loss of bactericidal activity.
Β-lactamases are either constitutive, or more commonly, are acquired by the
transfer of plasmids. Some of the β-lactam antibiotics are poor substrates for
β lactamases & resist cleavage. Gram +ve organisms secrete β lactamases
extracellularly, whereas gram –ve bacteria have the enzymes in the
periplasmic space between the inner & outer membranes.
2.
Decreased permeability to the drug: decreased penetration of the antibiotic
through the outer cell membrane prevents the drug from reaching the target
PBP
s
..The presence of an efflux pump can also reduce the amount of
intracellular drug.
3.
Altered PBP
s
: modified PBP have lower affinity for β-lactam antibiotics,
requiring clinically unattainable concentrations of the drug to effect
inhibition of bacterial growth. This mechanism may explain MRSA.
Pharmacokinetics
1. Administration: the route of administration of a β-lactam antibiotic is
determined by the stability of the drug to gastric acid and by the severity of the
infection. Ticarcillin, piperacillin, ampicillin + sulbactam, ticarcillin +
clavulanic acid and piperacillin + tazobactam must be administrated IV or IM.
Penicillin V, amoxicillin and amoxicillin + clavulanic acid are available as oral
preprations.
Others are effective by the oral, IV or IM routes. Procaine penicillin G &
benzathine penicillin G are administrated IM and serve as depot forms. They're
slowly absorbed into the circulation and persist at low levels over a long period
of time.
Pharmacology
Anti-Microbial Drugs 2
6
Dr. Haidar Al-Shakarchi
Lec. 8
2. Absorption: most of the penicillins are incompletely absorbed after oral
administration & they reach the intestine in sufficient amount to affect the
composition of the intestinal flora. However, amoxicillin is almost completely
absorbed. Consequently is not appropriate therapy for the treatment of shigella
& salmonella derived enteritis, because therapeutically effective levels don't
reach the organisms in the intestinal crypts. Oral penicillins, except for
amoxicillin, shouldn't be given at meal times, to minimize binding to food
proteins & acid inactivation.
3. Distribution: distribution of the β-lactam antibiotics throughout the body is
good. All the penicillins cross the placental barrier, but none has been shown to
be teratogenic. However, penetration into certain sites, such as bone or CSF, is
insufficient in therapy unless these sites are inflamed.
4. Excretion: the primary route of excretion is through the organic acid (tubular)
secretory system of the kidney as well as by glomerular filtration. Patients with
impaired renal function must have dosage regimens adjusted. Probenecid
inhibits the secretion of penicillins and thus, can increase blood levels.
Adverse Reactions
1. Hypersensitivity: This is most important adverse effect. The major antigenic
determinants of penicillin hypersensitivity are its metabolite, penicilloic acid,
which reacts with proteins and serve as a hapten to cause an immune reaction.
Approximately 5% of patients have some kinds of reactions, ranging from
maculo-papular rash (the most common rash seen with ampicilllin
hypersensitivity) to angioedema (marked swelling of the lips, tongue and
periorbital area) and anaphylaxis. Among patients with infectious
mononucleosis who are treated with ampicillins, the incidence of
maculopapular rash approaches 100%. Cross allergic reactions do occur among
the β-lactam antibiotics.
2. Diarrhoea: this effect which is caused by disruption of the normal balance of
intestinal microorganisms is a common problem. It occurs to a greater extent
with those agents that are incompletely absorbed & have an extended
antibacterial spectrum. Diarrhea appears to be less frequent with amoxicillin
Pharmacology
Anti-Microbial Drugs 2
7
Dr. Haidar Al-Shakarchi
Lec. 8
than ampicillin. As with some other antibiotics, pseudomembranous colitis may
occur.
3. Nephritis: all penicillins, but particularly methicillin, have the potential to
cause acute interstitial nephritis.
4. Neurotoxicity: the penicillins are irritating to neuronal tissue, & they can
provoke seizures if injected intrathecally or if very high blood levels are
reached. Epileptic patients are particularly at risk.
5. Hematologic toxicities: decreased agglutination maybe observed with the
antipseudomonal penicillins (ticarcillin & carbenicillin) &, to some extent, with
penicillin G. Additional toxicities include eosinophilia.
6. Cation toxicity: Penicillins are generally administered as the sodium or
potassium salts. Toxicities maybe caused by the large quantities of sodium or
potassium that accompany the penicillin.
Done by
Ali Kareem
