Sunday 2 / 11 / 2014
@Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
"Pharmacology
مكتب اشور لالستنساخ
Adrenergic System
Lec 6
ADRENERGIC SYSTEM
Lecture 6
Total lectures NO. 12
Dr. Haidar Al-Sharkachi
Adrenergic System Lec 6
Page 2
Classification of beta-blockers:
♣ According to the pharmacokinetic properties:
The solubility of beta-blockers varies, some are either lipid soluble or water soluble,
others are intermediate.
1.
Lipid Soluble:
Are extensively metabolized by the liver. They're subject to extensive
hepatic first pass metabolism after oral administration.
Plasma concentrations vary greatly between subjects .
They readily cross cell membranes so have a high apparent volume of
distribution (aVd).
They readily enter the CNS.
They have a shorter t1/2 (about 3 hours).
Examples: propranolol and metoprolol.
2.
Water Soluble:
Excreted unchanged by the kidney.
They're less subject to hepatic first pass metabolism so they show more
predictable plasma concentrations.
These agents are less widely distributed and may have lower incidence
of effects attributed to penetration of the CNS.
They have a longer t1/2 ( about 9 hours).
Examples: atenolol and nadolol
♣ According to selectivity:
Among the beta-receptor blocking drugs, relative affinities for beta
1
and beta
2
receptor varies.
1) Non-selective beta blockers act at both beta
1
and beta
2
receptors.
2) Beta
1
selective ( cardio-selective) beta blockers have a higher affinity (50-100
times) for beta
1
than for beta
2
receptors.
Examples: atenolol, acebutolol and metoprolol.
Note:Butoxamine is a selective beta
2
blocking drug with no obvious clinical
application.
The clinical advantages of selective beta-blockers are:
Adrenergic System Lec 6
Page 3
1) In diabetics: where beta
2
receptors mediate both the symptoms of
hypoglycemia (except sweating) and the counter-regulatory metabolic
responses that reverse the hypoglycemia.
2) In asthma: there's less likelihood of causing bronchoconstriction, however,
none of the available beta
1
blockers is sufficiently selective to be safely
used in asthma.
3) In peripheral vascular disease: and when cold extremities is a troublesome
side effect. Since selective beta-blockers have less effect on peripheral
vascular beta
2
receptors, cold extremities is less frequent.Cold extremeties
is due to decreased cardiac output and reduced peripheral blood flow.
♣ According to other non-blocking effects:
1. Partial agonist action (PAA) [Intrinsic sympathomimetic activity] (ISA)
Most β-blocking drugs are pure antagonists (i.e. cause no activation of the
receptor).However, some are partial agonists (cause partial activation of the
receptor).This is sometimes described as having intrinsic sympathomimetic activity
(ISA). Examples: pindolol and acebutolol.These agents differ from the pure
antagonists in the following:
1) They cause less fall in resting heart rate than do the pure antagonists, and
may be less effective in severe angina pectoris.
2) There is also less fall in cardiac output and possibly fewer patients experience
unpleasantly cold extremities.
3) Abrupt withdrawal may be less likely to lead to a rebound effect if there is
some partial agonist action, since upregulation of receptors, may not have
occurred.
4) They cause minimal disturbance in lipid and carbohydrate metabolism.
5) They are claimed to have increased safety in patients with airway disease.
2. Membrane stabilizing [quinidine-like or local anesthetic] effect or action (MSA):
It is a prominent effect of several β-blockers. This action is the result of typical
local anesthetic blockade of sodium channels. These drugs are not used topically on
the eye for glaucoma, where local anesthesia of the cornea would be highly
undesirable e.g. propranolol and acebutolol.
Adrenergic System Lec 6
Page 4
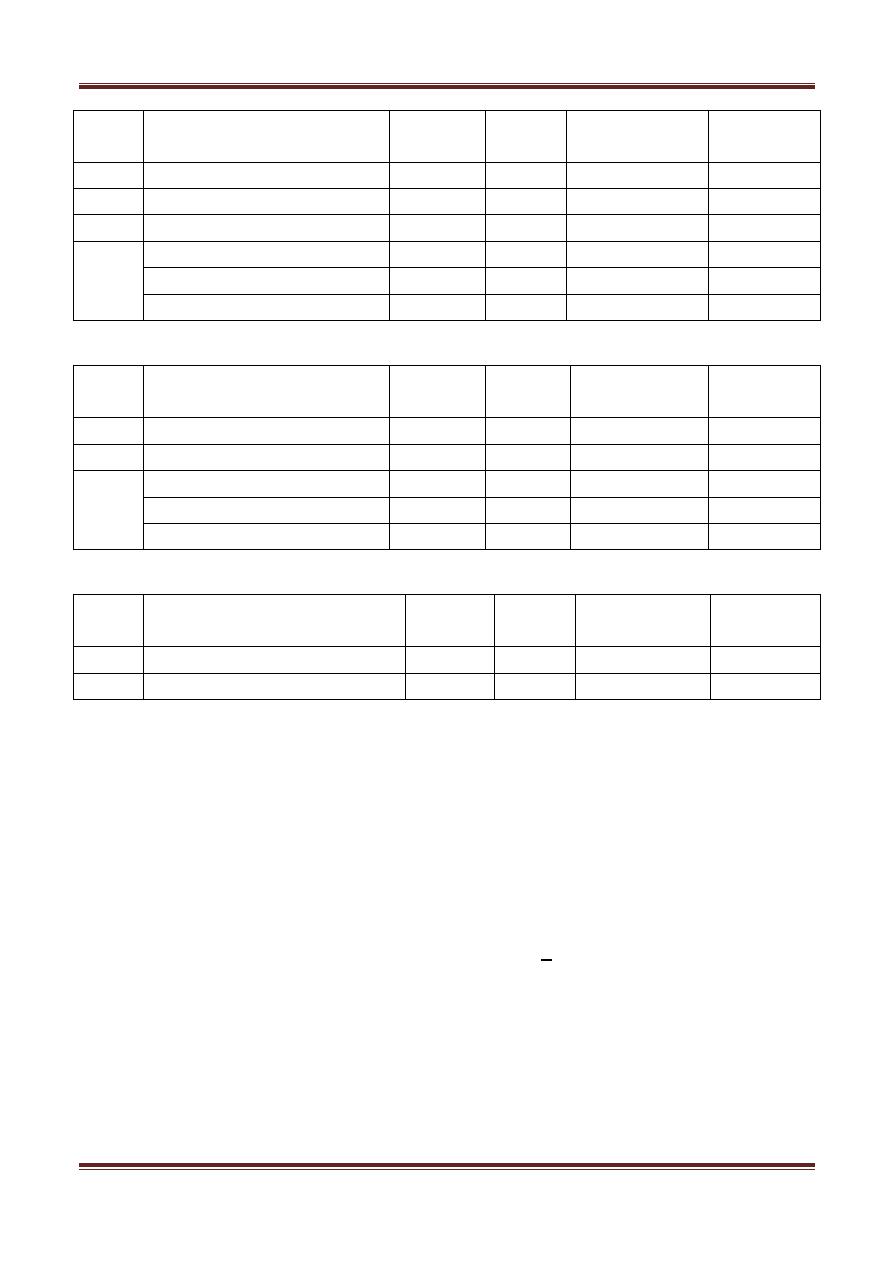
Group Non-selective β-blockers
ISA
MSA
Elimination
half life
Solubility
G I
Oxprenolol
+
+
G II
Propranolol
-
+
4-6 hours
L.S.
G III
Pindolol
+
-
G IV
Sotalol*
-
-
W.S.
Timolol
-
-
Nadolol
-
-
14-24 hours
W.S.
Group β1-selective blockers
ISA
MSA
Elimination
half life
Solublity
G I
Acebutolol
+
+
G III
Esmolol
10 min
G IV
Atenolol, Nebivolol
-
-
W.S.(At.)
Metoprolol, Betaxolol
-
-
L.S.(Me.)
Bisoprolol, Celiprolol
-
-
Group Non-selective β-blockers +
α1-blockers
ISA
MSA
Elimination
half life
solubility
G II
Carvedilol
G IV
Labetalol
L.S.
Notes:
1) Nadolol: has the longest elimination half life.
2) Esmolol: has a very short half life due to metabolism of an ester linkage.It is only
given I.V. if required during surgery or diagnostic procedures.
3)Sotalol: It is a β
1
-selective blocker and is a class III anti-arrhythmic drug(beta
blockers are class II antiarrythmics).
4) Carvedilol: The receptor affinity is beta
1
= beta
2
> alpha
1
> alpha
2
which
means it is a non selective β-blocker that also blocks the α
1
receptors.Carvedilol and
labetalol contrast with the other beta blockers that produce peripheral
vasoconstriction.
- Carvedilol has clinical benefits in congestive heart failure.It also decreases lipid
peroxidation and vascular wall thickening,effects that have benefit in heart failure.
Adrenergic System Lec 6
Page 5
(Clinical trials have shown clinical benefits of carvedilol as well as metoprolol and
bisoprolol in patients with stable chronic heart failure.)
5)Labetalol: May be employed as an alternative to methyldopa in the treatment of
pregnancy induced hypertension.Intravenous labetalol is also used to treat
hypertensive emergencies.
6)Nebivolol: also has vasodilator properties mediated by nitric oxide.
Therapeutic uses of β-receptor blocking drugs:-
A) Cardiovascular uses:
1. Angina pectoris: Beta adrenoceptors blockers reduce the frequency of anginal
episodes and improve exercise tolerance in many patients with angina. These
actions are related to decreased cardiac work and reducion in oxygen demand.
2. Hypertension:
Β-blockers given chronically lower blood pressure in patients with hypertension.
The factors involved may include:
Reduction in cardiac output
Lowering of total peripheral resistance,
Inhibition of rennin release and
CNS effects.
For acute or emergency treatment of hypertension β-blockers are not used (may
increase diastolic pressure). Labetalol, a competitive α and β antagonist, is
effective.
3.Cardiac tachyarrhythmias:
Β-blockers are class II anti-arrhythmics. They depress automaticity and increase the
AV nodal refractory period. They are especially effective for treatment of
supraventricular arrhythmias.Sotalol is a non selective β-receptor antagonist that
has marked class III anti arrhythmic effect reflecting potassium channel blockade. It
causes lengthening of the refractory period of the cardiac cells.
Adrenergic System Lec 6
Page 6
4.Myocardial infarction:
Β-blocker has a cardioprotective effect in:
a. Early use within 6-12 hours of infarction and for 3-4 weeks results in the
reduction in the infracted size and protection against cardiac rupture.
b. Late use between 4 days-4 weeks after onset of infraction and is continued for
at least 2 years. Useful for secondary prevention from another M.I.
5. Hypertrophic obstructive cardiomyopathy or (hypertrophic subaortic stenosis)
and tetralogy of Fallot (TOF): β-blockers decrease outflow resistance and increase
stroke volume.
6. Hepatic portal hypertension & esophageal variceal bleeding:
Βeta-blockers cause reduction of portal pressure.
7. Aortic dissection & after subarachnoid hemorrhage:
Βeta-blockers reduce force and speed of systolic ejection (contractility) and blood
pressure.
B) Endocrine uses:
1. Hyperthyroidism:
Beta-blockers reduce the unpleasant symptoms of sympathetic over-activity; there
may also be an effect on the metabolism of thyroxine.
2. Pheochromocytoma:
Beta-blockers may be required after α receptor blockade has been instituted to
reverse the cardiac effects of excessive catecholamines.Beta-antagonists should
NOT be employed PRIOR to establishing effective α receptor blockade,since
unopposed beta receptor blockade could cause blood pressure elevation from
increased vasoconstriction.
C) CNS uses:
1. Anxiety with somatic symptoms.
Adrenergic System Lec 6
Page 7
2. Essential tremor: The tremor may respond to standard doses of selective or
non-selective blockers. Dysfunction of β1 receptor has been implicated in some
cases.
3. Migraine headache prophylaxis: Ssome β-blockers e.g. propranolol show a
beneficial effect in reducing the frequency and intensity of migraine headache. The
mechanism is not known.
4. Alcohol and opioids acute withdrawl symptoms.
D) Eye uses:
Glaucoma: Topical administration of a β-blocking drug with no MSA e.g. timolol
reduces intraocular pressure (IOP). The mechanism appears to involve reduced
production of aqueous humor by the ciliary body.
Adverse effects of β-receptor blocking drugs:
A. Adverse reactions due to beta-adrenoceptor block:
1. Cardiac failure:
B-receptor blockade depresses myocardial contractility. In patients with
abnormal myocardial function, cardiac output may be dependent on
sympathetic derive. If this stimulus is removed, cardiac decompensation
may result.
2. Bronchoconstriction:
B2- receptor blockade associated with the use of non selective agents
commonly causes worsening of pre existing asthma and other forms of
airway obstruction.While B
1
- selective drugs may have less effect on
airways,they are not totally selective and may precipitate asthma.
3. Hypotension: When the drug is given after myocardial infarction.
4. Bradycardia and heart block:
5. Hypoglycemia: It occurs especially with non selective members in
diabetes, due to impairment of the normal sympathetic- mediated
homeostatic mechanisms for maintaining blood glucose. i.e: the recovery
from hypoglycemia is delayed.
In addition symptoms of hypoglycemia will not occur.
Adrenergic System Lec 6
Page 8
6. Cold extremities: it’s due to reduced peripheral blood flow especially with
non- selective drugs.
*B-blockers (1) reduce cardiac output.
(2) block peripheral vascular B2 receptors.
7. Withdrawal phenomenon:
Abrupt withdrawal of therapy can be dangerous in angina pectoris and
after myocardial infarction.It probably occurs due to upregulation of B-
receptors and appears to be least common with partial agonists.
8. Intrauterine growth retardation:
B-blockers administered during pregnancy decrease placental blood flow
and may retard growth of the fetus. They also produce neonatal
bradycardia and neonatal hypoglycemia.
9. Hyperlipidemia:
B-blockers cause decrease of HDL/ LDL ratio which is in a direction adverse
for coronary heart disease. These changes are minimal with parial
agonists.
10. Impotence:
Interference of sexual function is unusual .
B. Adverse reactions not certainly due to beta-receptor blockade:
1. CNS side effects: include sedation, fatigue, nightmares and depression. B-
blockers with low lipid solubility are associated with a lower incidence of
CNS adverse effects.
2. Hyper sensitivity reactions: skin rash.
3. Oculomuco cutaneous syndrome:
It occured with chronic use of practolol (now obsolete).
Contraindications:
1. Heart failure.
2. Asthma.
3. Sick sinus syndrome or heart block.
4. Bradycardia & hypotension.
5. Diabetes.
6. Peripheral vascular disease.
