Dr. Alaa Al-Deen
Lec. 1
Rabies – Infectious
mononucleosis – CMV
infection
Mon 16 / 3 / 2015
2014 – 2015
مكتب اشور لالستنساخ
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
1
Rabies
Rabies has been around for
centuries; described as early as
2300 B.C.
Transmission is direct,
primarily via inoculation by
bite, with infectious viruses
present in saliva.
The reservoir for rabies is the
animal pool that circulates
rabies virus (diverse species of
mammals each with a specific
strain).
Rabies is >99% fatal once
symptoms occur.
Rabies is caused by a virus …
- Family Rhabdoviridae – ‘bullet’
shaped, contains a single-
stranded RNA genome.
- Genus Lyssavirus.
Picture from Centers for Disease Control and
Prevention
www.cdc.gov/ncidod/dvrd/rabies
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
2
Virulence
Depends on severity of bite.
If treatment is given and when.
Once the disease manifests in CNS ultimate death.
Vehicles of Transmission
Saliva.
Aerosol transmission.
Corneal transplantations.
High Risk Animals
Raccoon.
Skunk.
Groundhog.
Fox.
Bat.
“Free-roaming” cats.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
3
Intermediate Risk Animals
Dogs
Cats – vaccinated or non-
roaming
Livestock – horses, cattle, pigs
Other non-rodent wild animal
species,
i.e. opossum, bear, deer,
coyote… etc.
PATHOGENESIS
Rabies virus is inoculated through the skin, usually via a bite that delivers
virus-laden saliva. Virus replicates within striated muscle cells at the
inoculation site and spreads to peripheral nerves and then to the CNS. The
virus continues to replicate within gray matter and passes along autonomic
nerves to other tissues and from there into saliva, whence it may be
transmitted to another host.
Within the CNS, rabies virus causes nerve cell destruction and microglial
infiltration.
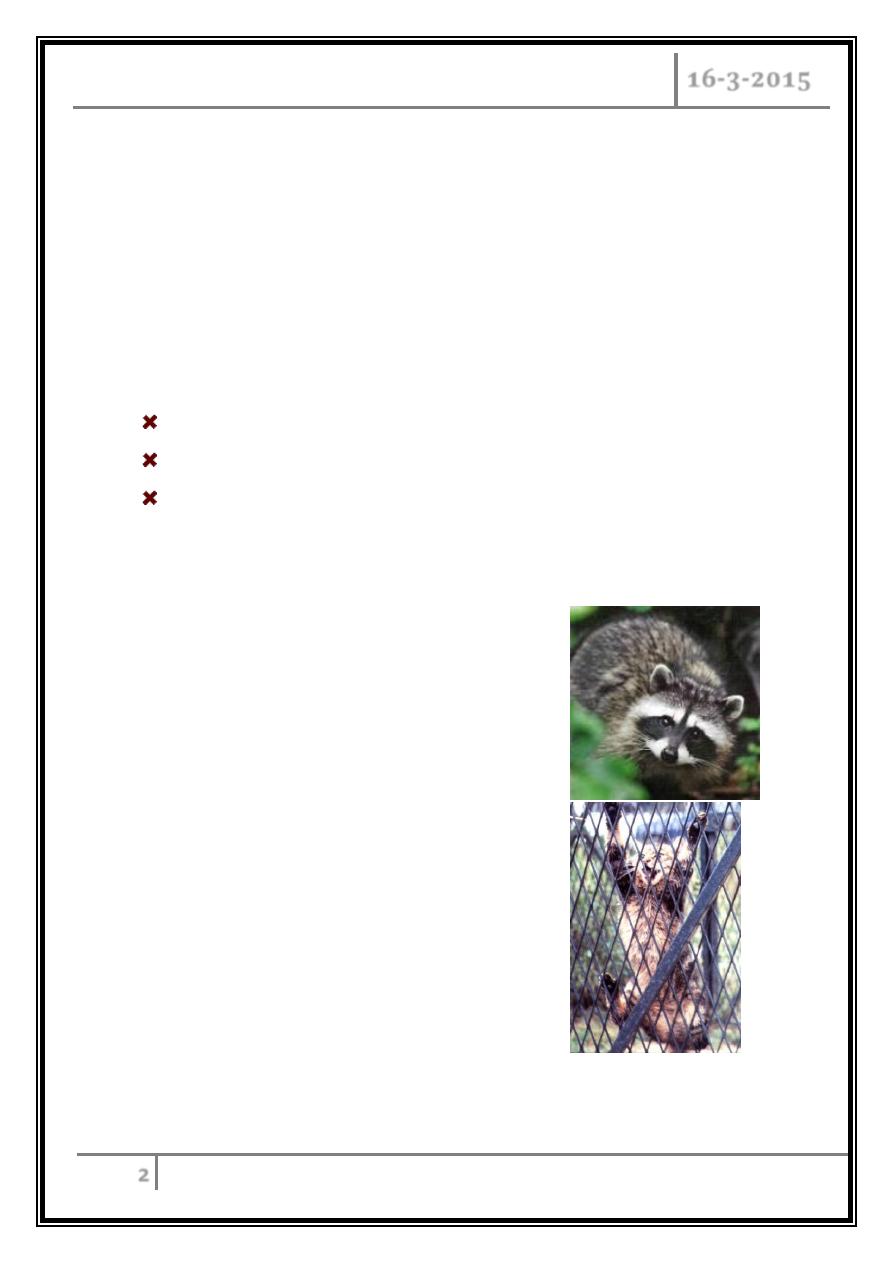
Negri bodies -characteristic eosinophilic cytoplasmic inclusions within
neurons- are made up of a finely fibrillar matrix and rabies virus particles.
The incubation period varies from 7 days to 1 year (mean, 1-2 months).
Bites on the face are associated with the highest rates of infection and
mortality; bites on the legs with the lowest rates.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
4
CLINICAL FEATURES
Prodromal period (1-4 days): patients have fever, headache, malaise, myalgias,
anorexia, nausea, vomiting, sore throat, and non-productive cough.
Paresthesia and/or fasciculations at or near the site of viral inoculation are found
in 50–80% of cases and are suggestive of rabies.
Encephalitic phase:
Patients develop periods of excessive motor activity, excitation, and agitation,
confusion, combativeness, muscle spasms, seizures, focal paralysis, and fever.
These are interspersed with shortening periods of lucidity.
Hyperesthesia is common.
Hydrophobia or aerophobia is seen in approximately two-thirds of patients and
helps in making the diagnosis.
Hyperthermia, autonomic dysfunction, upper motor neuron paralysis, and vocal
cord paralysis can occur.
Brainstem dysfunction:
This stage is characterized by cranial nerve involvement (e.g. diplopia, facial
palsies, optic neuritis, and difficulty with deglutition).
Deglutition problems combined with excessive salivation produce characteristic
foaming at the mouth.
Hydrophobia—painful, violent, involuntary contractions of the diaphragm and of
accessory respiratory, pharyngeal, and laryngeal muscles initiated by swallowing
liquids can occur, as can priapism.
Coma and death:
The median survival period after symptom onset is 4 days; the maximum is 20
days. Even with aggressive supportive measures, recovery is rare.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
5
DIAGNOSIS
CSF examination can show a mild pleocytosis and a slightly increased protein
level.
Rabies virus-specific antibodies in serum and CSF develop late in the clinical
course and, if the patient dies during the acute phase, may remain
undetectable. If no vaccine or rabies immune serum has been given, the
presence of antibody to rabies virus in serum is diagnostic of infection.
Saliva: Reverse-transcription PCR (RT-PCR) can reveal viral shedding in fresh
saliva, which directly precedes the onset of clinical signs and continues
throughout the course.
Skin biopsy: Because the virus spreads centrifugally from the CNS, a skin
biopsy sample from the nape of the neck may be positive in direct fluorescent
antibody (DFA) testing and RT-PCR.
Differential diagnosis
- Other viral encephalitides [e.g. those due to herpes simplex virus (HSV) type 1,
varicella-zoster virus, enteroviruses as well as arboviruses].
- Vasculitis should be considered.
- Clinical diagnosis of rabies is straightforward in developing countries when a
non-immunized patient presents after a bite by a known rabid animal.
- In developed countries, some patients may have an unrecognized exposure
(e.g. to a bat) or are unaware of the risks of exposure and did not receive post-
exposure prophylaxis.
- Rabies should be considered in the differential diagnosis of patients presenting
with acute progressive encephalitis regardless of a history of an animal bite or
known exposure.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
6
PREVENTION
The wound should be thoroughly scrubbed with soap and flushed with water.
Post-exposure prophylaxis (PEP) with a modern cell-culture vaccine should be
administered as appropriate.
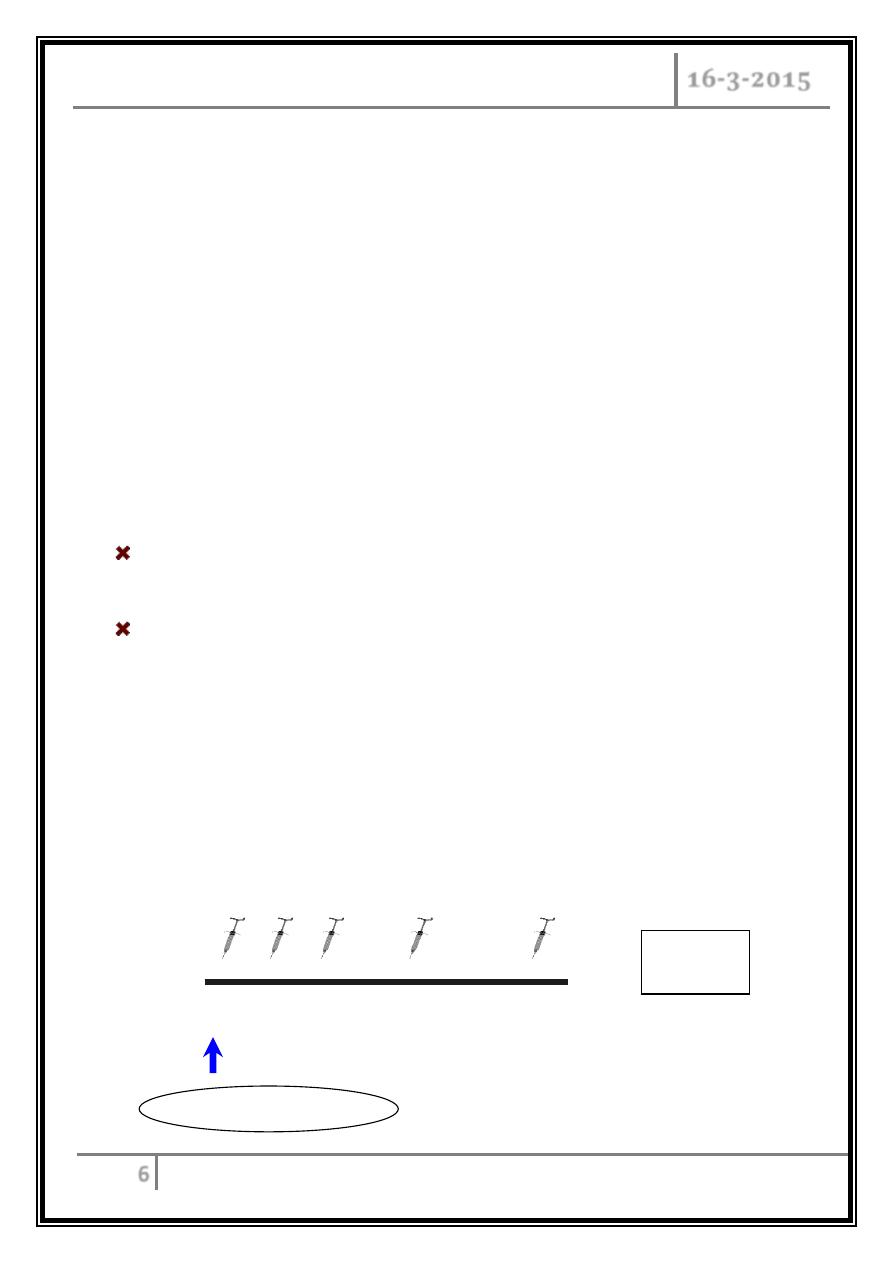
Timing of prophylaxis
Rabies post-exposure prophylaxis is a medical urgency and should begin as
soon as possible after the presumed exposure.
What to administer
Rabies immunoglobulin is referred to as "passive immunization"; rabies vaccine is
referred to as "active immunization".
Post-exposure rabies prophylaxis, in previously unimmunized persons, should
always include both passive and active immunization.
Standard intramuscular regimen. One dose
into deltoid on each of days:
Essen intramuscular Regimen
WHO Recommended PEP Schedule
5 vials
5 visits
day 0 3
7 14 28
Rabies immunoglobulin
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
7
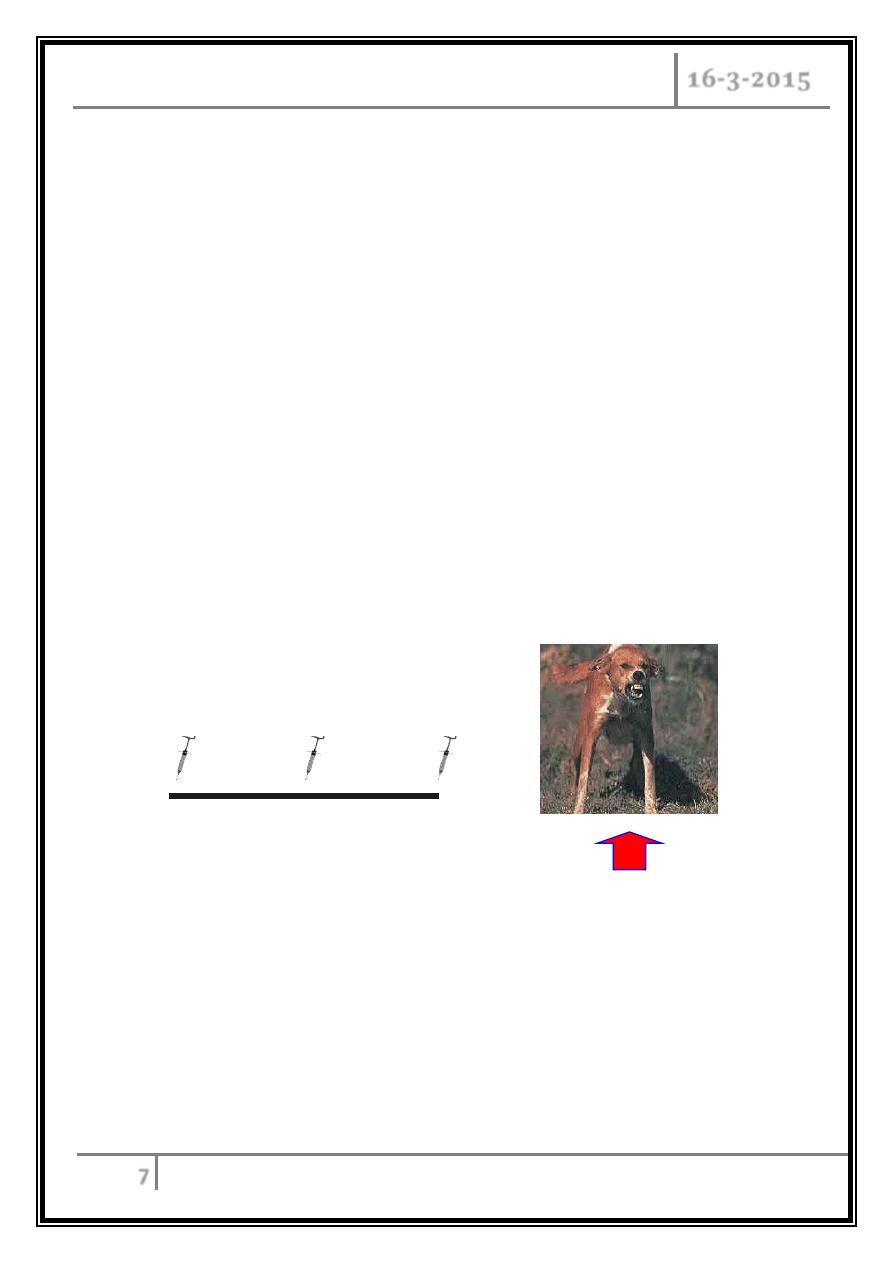
Pre-exposure prophylaxis
Is occasionally given to persons at high risk, after receiving a series of 1-mL doses
of a modern cell-culture vaccine I.M. on days 0, 7, 21, and 28.
High- and moderate-risk patients should have their rabies virus-neutralizing
antibody titers monitored every 6 months and every 2 years, respectively.
WHO Recommended Pre-exposure
3-dose series intramuscular or
intradermal regimen
Pe-exposure
Exposure: No Rabies immunoglobulin needed
day 0
7 21 or 28
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
8
INFECTIOUS MONONUCLEOSIS
Epstein-Barr virus (EBV)
Virology
Epstein Barr Virus (EBV):
Herpes Family - (linear DNA virus HHV4).
Surrounded by nucleocapsid and glycoprotein envelope.
Most acute EBV infections are asymptomatic.
Symptomatic infectious mononucleosis causes is characterized by a triad of
fever, tonsillar pharyngitis, and lymphadenopathy.
One of the most serious complications of mononucleosis is splenic rupture.
It was initially described as "Drusenfieber" or glandular fever in 1889, but the
term "infectious mononucleosis" was later used in 1920.
Spread by intimate contact between susceptible persons and EBV shedders.
Antibodies to EBV have been demonstrated in all population groups with a
worldwide distribution; approximately 90 to 95 percent of adults are
eventually EBV-seropositive.
Less than 10 percent of children develop clinical infection despite the high
rates of exposure.
The incidence of symptomatic infection begins to rise in adolescent through
adult years.
Traditionally the peak incidence of infection has been described in the 15 to
24-year age range.
IM is relatively uncommon in adults, accounting for less than two percent of
pharyngitis in adults.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
9
TRANSMISSION
Following infectious mononucleosis, virus may be shed in salivary secretions
for many weeks. The virus can persist in the oropharynx of patients with IM for
up to 18 months following clinical recovery.
EBV has also been isolated in both cervical epithelial cells and in male seminal
fluid, suggesting that transmission may also occur sexually.
PATHOGENESIS
Contact of EBV with oropharyngeal epithelial cells allows replication of the
virus, release of EBV into the oropharyngeal secretions, and infection of B cells
in the lymphoid-rich areas of the oropharynx.
EBV-infected B cells are responsible for the dissemination of infection
throughout the lymphoreticular system.
The incubation period prior to the development of symptoms averages four to
eight weeks.
The atypical lymphocytes, that appear in the peripheral blood of patients with
acute IM between one and three weeks after the onset of symptoms, are EBV-
specific cytotoxic T-lymphocytes, and are considered essential in controlling
acute and reactivation infection.
EBV becomes a lifelong infection as it establishes latency with periodic
reactivation with oral shedding of EBV.
increased risks of other conditions, such as increased risks for autoimmune
disorders, such as multiple sclerosis or systemic lupus erythematosus, or:
nasopharyngeal carcinoma.
Burkitt’s lymphoma.
Hodgkin’s disease.
B-cell lymphoma.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
10
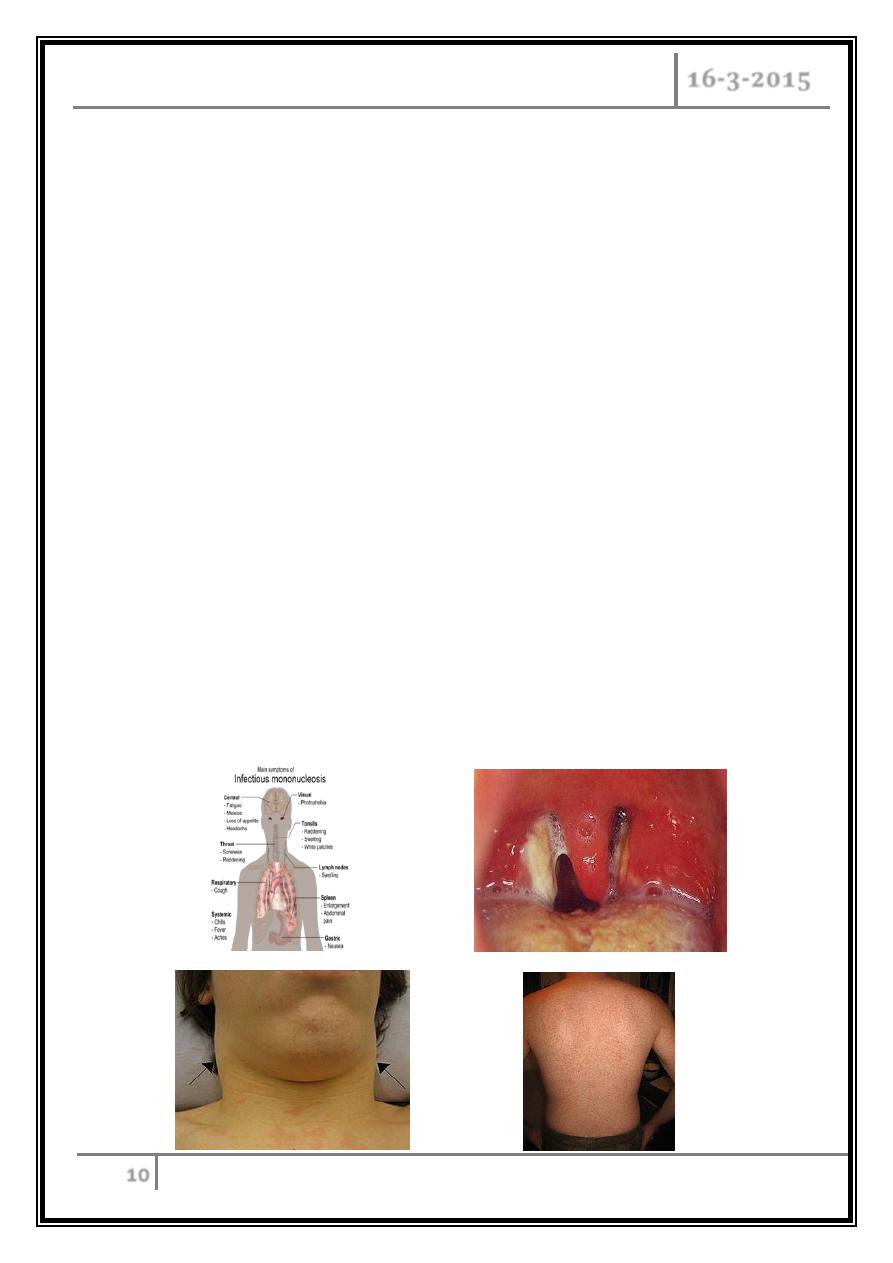
CLINICAL MANIFESTATIONS
Classic IM - typical features of IM include fever, pharyngitis, adenopathy, fatigue,
and atypical lymphocytosis.
Palatal petechiae with streaky hemorrhages.
Splenomegaly and splenic rupture.
Fatigue may be persistent and severe.
Rash: a generalized maculopapular, urticarial, or petechial rash is occasionally
seen, while erythema nodosum is rare.
A diffuse macular rash is more common following the administration of ampicillin
or amoxicillin, and has also been described with azithromycin, levofloxacin,
piperacillin/tazobactam, or cephalexin.
Neurologic syndromes, such as Guillain-Barré syndrome:
o Facial and other cranial nerve palsies.
o Meningoencephalitis.
o Transverse myelitis.
o Peripheral neuritis.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
11
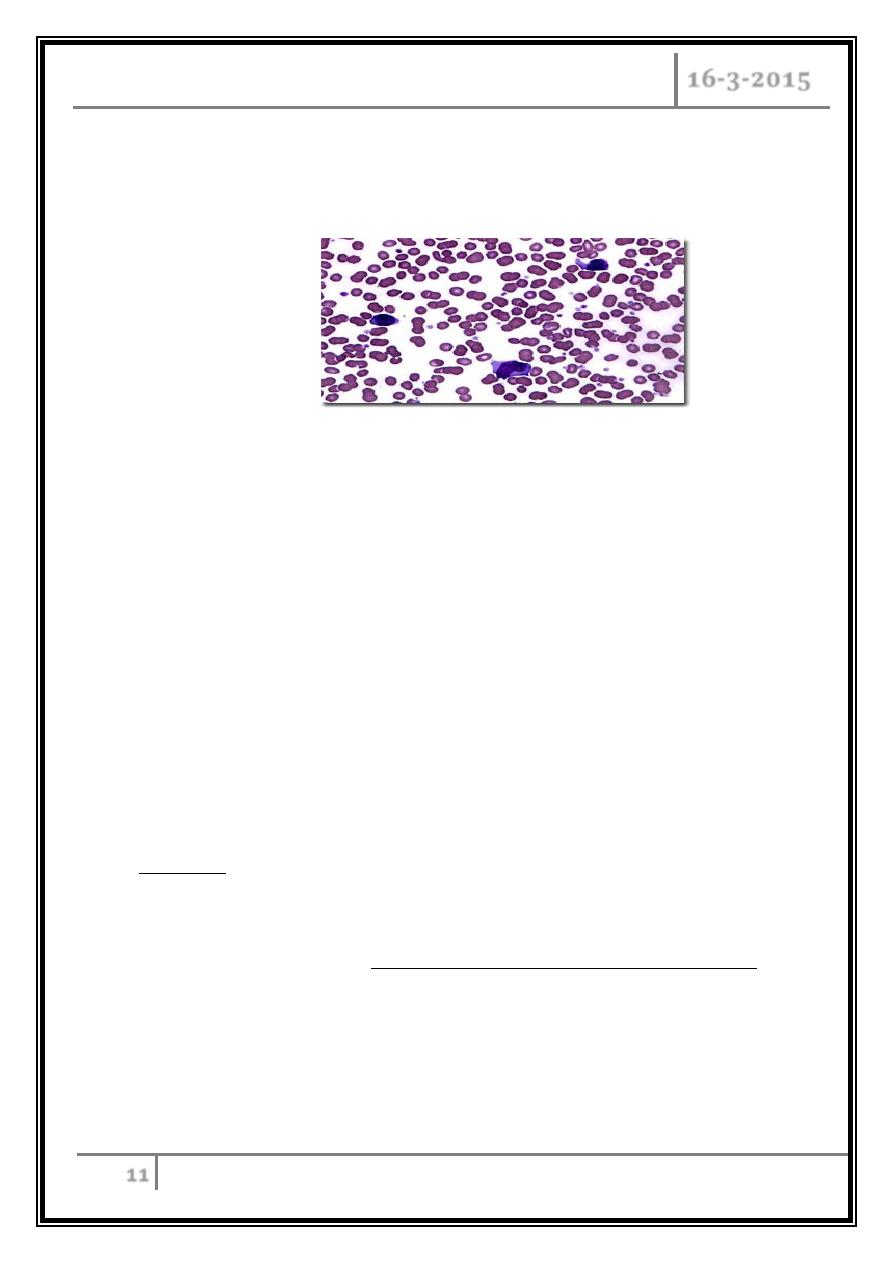
LABORATORY ABNORMALITIES
The most common laboratory finding in association with IM is lymphocytosis with
significant atypical lymphocytosis.
The total white blood cell count may be raised.
Some patients have a mild relative and absolute neutropenia and
thrombocytopenia.
Unusual hematologic manifestations:
- Hemolytic anemia.
- Thrombocytopenia.
- Aplastic anemia.
Liver function tests: elevated aminotransferases are seen in the vast majority of
patients, but are self-limited.
Heterophile antibodies: they agglutinate sheep red blood cells (the classic Paul-
Bunnell test), horse red blood cells (used in the "Monospot" test), and ox and
goat erythrocytes.
Reactive heterophile antibodies in a patient with a compatible syndrome are
diagnostic of EBV infection and are therefore the diagnostic test of choice in most
clinical settings.
EBV-specific antibodies: measurement of EBV-specific antibodies may be
warranted in patients with suspected IM and a negative heterophile test.
IgM and IgG antibodies directed against viral capsid antigen have high sensitivity
and specificity for the diagnosis of IM.
Polymerase chain reaction assays: EBV’s DNA quantification can be accomplished
through polymerase chain reaction assays on blood or plasma.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
12
DIFFERENTIAL DIAGNOSIS
Patients with fever, pharyngitis, and lymphadenopathy may have:
Streptococcal infection.
Cytomegalovirus pharyngitis associated with CMV tends to be extremely mild,
if present at all, but may cause liver function test elevations, as does acute
EBV.
Rarely, toxoplasma infection rubella, roseola, viral hepatitis, mumps, CMV,
acute HIV infection.
A mononucleosis syndrome with atypical lymphocytosis can also be induced
by several drugs, particularly anticonvulsants such as phenytoin,
carbamazepine, and antibiotics, such as isoniazid or minocycline.
Lymphoma.
TREATMENT
Primary EBV infections rarely require more than supportive therapy.
Symptomatic treatment: acetaminophen or nonsteroidal anti-inflammatory
drugs are recommended for the treatment of fever, throat discomfort, and
malaise.
Provision of adequate fluids and nutrition is also important. It is prudent to get
adequate rest, although complete bed rest is unnecessary.
With complications including airway obstruction, we use corticosteroids, as
well as emergent consultation with an otolaryngologist.
Corticosteroid therapy :
Severe overwhelming life-threatening.
Infection (e.g. fulminant liver failure).
Severe hemolytic.
Acute airway obstruction.
Aplastic anemia.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
13
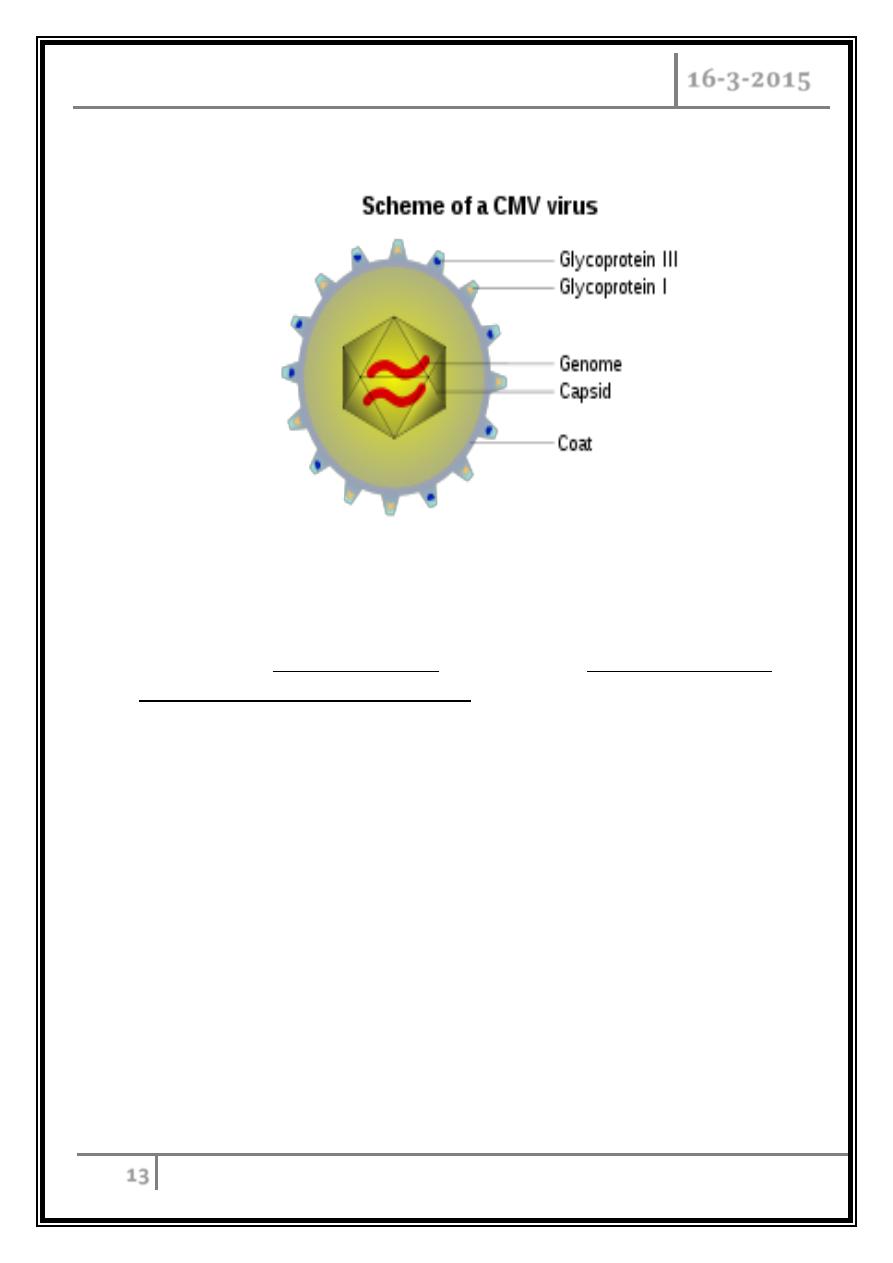
Cytomegalovirus (CMV) infection
CMV infections in immunocompromised patients cause substantial morbidity and
mortality, especially among transplant recipients and those infected with the
human immunodeficiency virus (HIV).
Infection in the immunocompetent host is generally asymptomatic or may
present as a mononucleosis syndrome.
TRANSMISSION
The virus is generally passed from infected people to others through direct
contact with body fluids, such as urine, saliva, vaginal secretions, and semen or
probably exposed to virus shed from the upper respiratory tract and urine.
Transfusion of blood products.
Sexual modes of transmission are supported by evidence that seroprevalence
rates are higher among patients with multiple sexual partners.
Transplantation of organs from seropositive donors.
Perinatal
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
14
CMV MONONUCLEOSIS
A syndrome resembling infectious mononucleosis.
It is the most common presentation of symptomatic CMV infection in
immunocompetent adults.
CMV can cause fever of unknown origin in healthy adults, especially in those
with day-care-aged children.
Classic mononucleosis is an illness characterized by significant, often
protracted fevers, and lassitude in the setting of absolute lymphocytosis and
atypical lymphocytes.
Heterophile-negative.
CMV-related disease in immunocompetent hosts is related to primary
infection.
In immunocompetent hosts, T cells play an important role in controlling viral
replication and disease, but do not eliminate the virus completely.
With seroprevalence rates ranging between 40 to 100 percent of the adult
population the prevalence of CMV-specific antibody increases with age.
Like other members of the Herpesvirus family, CMV establishes latent
infection after the resolution of acute infection.
CMV mononucleosis can be accompanied by dermatologic manifestations in
approximately one-third of patients including macular, papular,
maculopapular, rubelliform, morbilliform, and scarlatiniform eruptions.
Exposure to ampicillin or related beta-lactam antibiotics has also been
associated with the development of a characteristic generalized
maculopapular rash in patients with CMV mononucleosis, analogous to that
seen with EBV.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
15
Pregnant women
o Infection of pregnant women, even if asymptomatic, is occasionally associated
with the syndrome of congenital CMV in newborns with 15% chance.
o For pregnant women, the two most common exposures to CMV are through
sexual contact and through contact with the urine of young children with CMV
infection.
Diagnosis
Most often is established by isolation of CMV from blood by serologic testing.
Culture.
Histopathologic evidence of CMV infection in involved tissues (such as liver, lung,
gastrointestinal tract).
From clinical findings alone (CMV retinitis).
Differences between EBV and CMV mononucleosis
The mononucleosis syndrome associated with CMV infection has been described
as "typhoidal" in presentation, since systemic symptoms and fever predominate and
signs of enlarged cervical nodes and splenomegaly are not as commonly seen as they
are in EBV.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
16
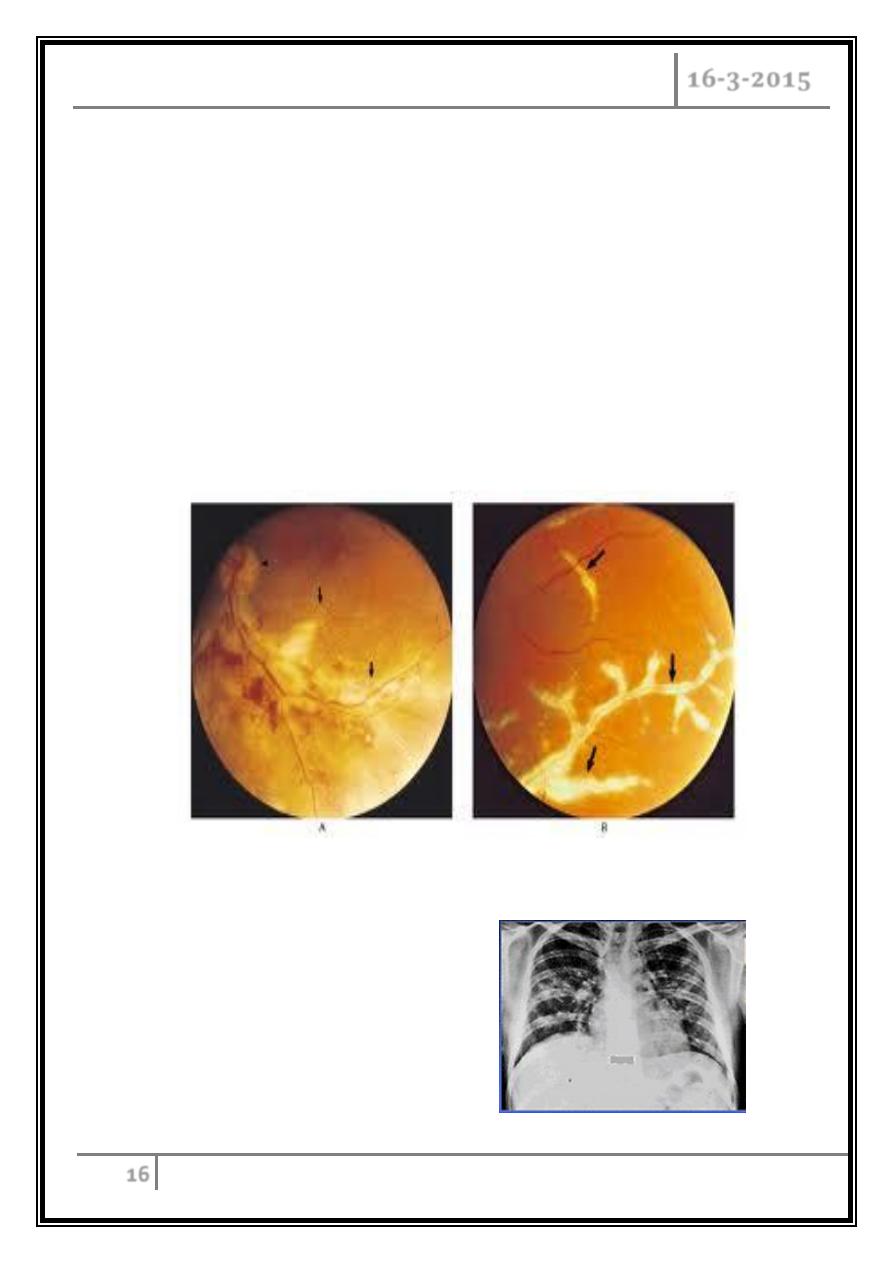
ORGAN-SPECIFIC cOMPLICATIONS
In persons with impaired cellular immunity (such as those with AIDS or organ
and bone marrow transplant recipients), CMV causes serious infections:
CMV syndrome:
Retinitis.
Pneumonia.
Gastrointestinal ulcerations.
Encephalitis.
Adrenalitis.
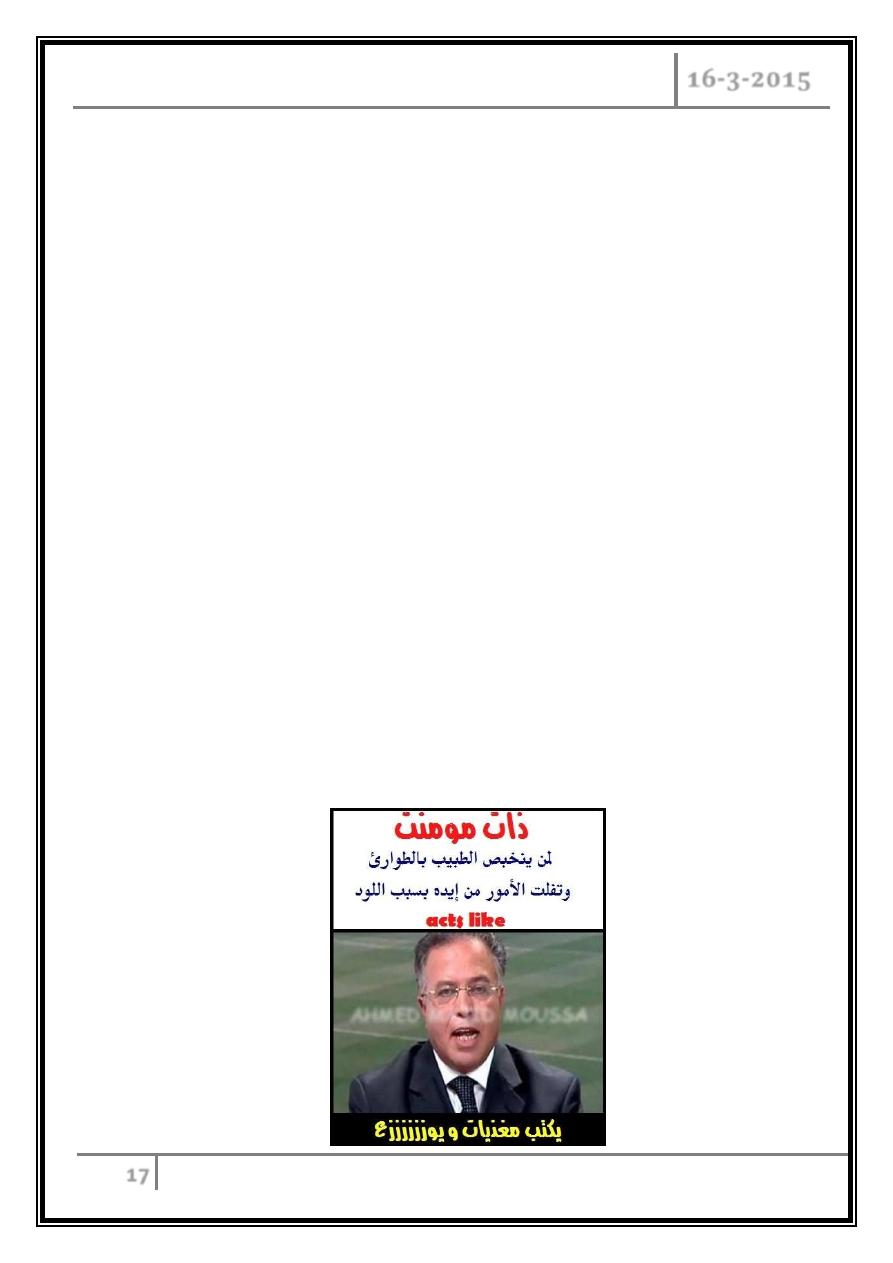
CMV pneumonitits
Median onset 50 days.
Causes of half of interstitial
pneumonitis cases
Case fatality rate = 85%
Leading cause of infection
deaths.
RABIES - INFECTIOUS MONONUCLEOSIS - Dr. Alaa Al-Deen
CMV INFECTION
16-3-2015
17
Hepatic manifestations :
Liver function abnormalities are frequently encountered in patients with
symptomatic CMV infection.
Subclinical transaminitis is the most common finding in immunocompetent
patients.
CMV should also be included in the differential diagnosis of granulomatous
hepatitis.
THERAPY
Most cases of primary CMV infection in immunocompetent hosts are
associated with minimal or no symptoms.
Among patients with symptomatic CMV infection, especially the
mononucleosis syndrome, the illness is generally self-limited, with complete
recovery over a period of days to weeks. Antiviral therapy is not usually
indicated.
Several agents available for the systemic therapy of CMV infection in
compromised host, including ganciclovir, valganciclovir, foscarnet, and
cidofovir.
… The end …
